Abstract
Objective:
To examine the prevalence of depression and serious psychological distress (SPD) among adult United States (US) immigrants and US-born; and to investigate trends in depression and SPD.
Methods:
National Health Interview Survey data (2010 – 2016) was analyzed. Chi-square tests were used to measure differences in prevalence of SPD between US-born and immigrants, and differences in prevalence of depression. Logistic regression models were used to measure the association between mental health outcomes (depression, SPD) and predictors (nativity, length of residence). General linear models were used to investigate depression and SPD trends.
Results:
101,142 US adults were included in the analysis. Immigrants were found to be 11% (OR 0.89, 95% CI [0.85,0.95]) less likely to suffer from depression compared to US-born. US-born (p<0.0001) had a higher prevalence of depression compared to immigrants, and prevalence of depression decreased overtime (p=0.011) for immigrants and US-born individuals. Immigrants who lived in the US 15+ years were 17% (OR 1.17, 95% CI [1.00,1.36]) more likely to have SPD compared to those who were born in the US. Among immigrants, as length of residence increased the prevalence of SPD (p=0.002) and depression (p<0.0001) increased.
Limitations:
This study examines immigrants as an entire population, not accounting for differences in immigrant status or immigrant ethnicity.
Conclusions:
While the prevalence of depression is lower in immigrants compared to US-born, being an immigrant in the US for more than 15 years increases risk of SPD to the point of surpassing that of US-born individuals and increases risk of depression.
Keywords: Immigrant, Mental Health, Serious Psychological Distress, Depression, Trends
Introduction
Mental illness is a highly prevalent disease impacting approximately 18 percent of adults in the United States (US)1. Major depressive disorder and serious psychological distress (SPD) are two prevalent and costly forms of mental illness2,3. Many studies have estimated the prevalence of major depression to be 4.6 to 9.3 percent2,3, additionally, individuals with major depressive disorder spent approximately 98.9 billion dollars on medical treatment in 20104. Serious psychological distress (SPD) impacts approximately 3.3 percent of the population, and is associated with comorbidities such as heart disease and disability5,6. Mental and neurological disorders are considered a leading disability in the US due to years of life lost and premature mortality; these conditions led to 258 million absolute disability-adjusted life years (DALYs) globally in 20107,8. Adults who have a serious mental illness are less likely to be employed, and more likely to fall below the poverty line9. While research shows that new immigrants tend to have a better mental health profile than the native-born population10,11, it is unclear if there are differences in mental illness trends by nativity.
In 2016 there were approximately 43.7 million immigrants in the US, totaling about 13.5 percent of the total population12. Immigrants make up a large proportion of the US population and it is predicted that the vast majority of population growth between now and 2050 will be due to immigration13. In general, past research has shown that immigrant health is better than native-born health upon arrival to US, but this health deteriorates over time14–16. As seen in physical health, Black Caribbean and Latino male immigrants have been evaluated as having better mental health profiles than non-immigrants when they first arrive in the US, but also a higher risk of psychiatric disorders, the longer they stay in the US17,18. Although mental health conditions can impact US-born regardless of their income, race, or geographical location, the US immigrant population has unique characteristics that are important to understand. Prior research has shown that immigrant and refugee populations have significant mental health issues, such as an increase in suicidality as length of residence in the US increases19. Immigrants are known to be exposed to factors pre-migration, during migration, and post-migration that contribute to negative health outcomes that the native-born population do not face20,21. With such a large proportion of the US population being made up of immigrants, it is important to understand immigrant mental health and its unique aspects.
The concept of examining trends to explain the prevalence of mental health conditions has been used before. In the United States, work has been done to explore trends in depressive episodes, finding that the percentage of individuals reporting poor mental health has increased approximately two percent22. While previous research projects have examined the changes in prevalence of mental health disorders like depression over time23, as far as we know, there are no studies on trends in mental health that compare rates among immigrants and US-born adults. Therefore, the aim of this study was to examine the prevalence of depression and serious psychological distress (SPD) among adult United States (US) immigrants and US-born individuals; and to investigate trends in depression and SPD.
Methods
Data Source:
This study used seven years of National Health Interview Survey (NHIS) data, 2010–2016, and utilized the sample adult, person, family, and functionality and disability files24. Everyone that had data in each of the four files was included in the study.
Outcomes
Depression: Participants were asked “How often do you feel depressed?” Respondents who answered “never” were categorized as “not depressed”, while respondents who gave any other answer (daily, weekly, or monthly) were categorized as “depressed”.
Serious Psychological Distress (SPD): This variable utilized the Kessler 6 (K6) nonspecific distress scale. The K6 asks about how often in the past thirty days you experienced each of six symptoms. The symptoms included feeling sad, nervous, restless, hopeless, worthless, and that everything was an effort25. Each question had responses of none of the time, a little of the time, some of the time, most of the time, and all of the time that were scored from 0 to 4, respectively. The six symptom frequencies were then summed, and SPD was categorized as present (score ≥ 13) and not present (score < 13). The K6 questionnaire has been shown to be an accurate indicator of psychological distress in large samples26.
Main Predictors
Immigration Status – Participants were asked “Was X Born in the United States?” This variable was coded as Immigrant (No) and Non-Immigrant (Yes).
Years in the US – Participants were further categorized based upon how many years they had spent as a resident of the United States. Participants were asked „Years that X has been in the United States?” Years in the US was categorized in to less than 5, 5 to less than 10, 10 to less than 15, 15 + years, and born in the United States. Previous studies that used length of US residence as a variable to explore health trends have separated individuals into similar categories27.
Demographic Variables
Age – Age was obtained from participants’ age in years item, and was categorized into four groups: 18–34, 35–49, 50–64, and 65 +.
Sex – Participants’ sex (male, female).
Race/Ethnicity – Participants’ race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic other).
Region – Participants’ region of the United States (Northeast, Midwest, South, West).
Education – Participants’ education level (less than high school, high school graduate/GED, some college, college degree).
Employment – Participants’ employment status as of last week (employed for pay, not employed for pay/unemployed).
Federal Poverty Line Ratio – Ratio of the families’ income to the federal poverty level (under 1.00, 1.00–1.99, 2.00–2.99, 3.00 or over).
Comorbidities – The total number of comorbidities that the participant reported. Participants were asked “Ever been told you have …?” for fourteen conditions. The conditions included hypertension, coronary heart disease, angina pectoris, heart attack, heart condition, stroke, emphysema, asthma, chronic bronchitis (past 12 months), cancer, diabetes, weak/failing kidneys (past 12 months), liver condition (past 12 months) and any kind of chronic/long-term liver condition. These fourteen were further divided in to eight categories: hypertension, heart conditions (coronary heart disease, angina pectoris, heart attack, heart condition), stroke, pulmonary conditions (emphysema, asthma, chronic bronchitis), cancer, diabetes, weak/failing kidneys, and liver conditions (liver condition, any kind of chronic/long-term liver condition). A binary variable was created for each of the eight categories, not present or present, and were then summed to get the total number of comorbidities present.
Statistical Analysis
The statistical analysis was performed using SAS 9.4 (SAS Institute) with the purpose of investigating the relationship between mental health conditions and immigration characteristics as well as their trends over time. Analyses were conducted to examine differences in demographic and socioeconomic characteristics by length of residence in the US using chi-square tests. Differences in SPD and depression were also assessed using chi-square tests. Logistic regression models were utilized to determine the relationship between two mental health outcomes (depression, SPD) and two main predictors (nativity, length of residence). Each of the logistic models were run unadjusted then adjusted by demographic variables. General linear models were used to assess whether the relationship between immigration and SPD changed over time, and to investigate if depression changed over time among both immigrants and non-immigrants and among immigrants (< 5 years, 5 − <10 years, 10 − <15 years, 15+ years). Survey commands were applied to account for the complex study design and weights were used to generalize this information to the US civilian non-institutionalized population who are at least eighteen years old.
Results
The unweighted sample size was 101,142 adults (18 years or older) and represented a weighted sample of 44,718,335 within the US population. Table 1 shows the sample characteristics stratified by the number of years the participant has lived in the United States. Immigrants who have lived in the US less than 5 years had the youngest population with 68.02% (p <0.0001) being between the ages of 18–34 and had a mean age of 32.7 years (p<0.0001), while US-born had a mean age of 49.4 years of age and 28% between the ages of 18–34. US-born were made up of 54.4% females while immigrants with less than 5 years of residence were 47.2% female, 52.7% female for those with 5 to less than 10 years of residence and steadily increased up to 54.6% female for those with 15+ years of residence (p<0.0001). The immigrant population had at minimum 4.5 times as many Hispanic participants as their US-born counterparts. All length of residence groups had the highest percentage of people with a college degree; however, immigrants had higher percentages within groups of individuals with less than high school education from 11.9% for less than 5 years residence, 17.9% of 5 to less than 10 years residence, 22.6% of those with 10 to less than 15 years of residence, and 18.2% (p<0.0001) for 15+ years of residence compared to 6.9% of US-born. Those in the US less than 5 years had 37.67% whose income ratio to the federal poverty line was less than 1.00, while 5 to less than 10 years, 10 to less than 15 years, 15+ years, and born in the US had 25.62%, 26.11%, 19.31% and 14.91% (p<0.0001), respectively. The highest percentage of those with serious psychological distress (SPD), 3.99%, occurred in the immigrant population who have been in the United States for 15+ years compared to 3.68% of US-born and 2.27% (p=0.0002) of those with <5 years residence, while those born in the US had the highest percentage of depression at 39.94% compared to 30.75% (p<0.0001) of those with less than 5 years of residence in the US.
Table 1:
Sample characteristics for all participants, 2010–2016
| Characteristics, % (SE) | US - Born n = 82,648 N = 37,618,133 |
NUSB <5 years n = 1,739 N = 682,281 |
NUSB 5 – < 10 years n = 2,020 N = 750,542 |
NUSB 10 – < 15 years n = 2,600 N = 973,422 |
NUSB 15 + years n = 11,899 N = 4,606,170 |
p- value |
|---|---|---|---|---|---|---|
| Age in years, mean | 49.37 (0.15) | 32.73 (0.38) | 35.59 (0.29) | 38.39 (0.33) | 52.49 (0.25) | < 0.0001 |
| Age Group | < 0.0001 | |||||
| 18–34 | 28.05 (0.33) | 68.02 (1.41) | 56.29 (1.30) | 42.59 (1.13) | 14.53 (0.42) | |
| 35–49 | 22.61 (0.21) | 23.24 (1.24) | 32.47 (1.27) | 41.65 (1.05) | 32.11 (0.58) | |
| 50–64 | 26.62 (0.22) | 5.59 (0.62) | 8.00 (0.64) | 11.47 (0.73) | 29.51 (0.52) | |
| 65 + | 22.72 (0.26) | 3.16 (0.50) | 3.23 (0.46) | 4.30 (0.56) | 23.85 (0.66) | |
| Gender | < 0.0001 | |||||
| Male | 45.62 (0.21) | 52.83 (1.28) | 47.28 (1.10) | 46.62 (1.18) | 45.37 (0.55) | |
| Female | 54.38 (0.21) | 47.17 (1.28) | 52.72 (1.10) | 53.38 (1.18) | 54.63 (0.55) | |
| Race/Ethnicity | < 0.0001 | |||||
| Non-Hispanic White | 78.01 (0.40) | 23.34 (1.33) | 16.67 (1.13) | 15.70 (0.98) | 25.47 (0.69) | |
| Non-Hispanic Black | 13.26 (0.34) | 9.02 (0.94) | 10.07 (0.78) | 9.25 (0.61) | 7.84 (0.35) | |
| Hispanic | 6.43 (0.16) | 30.05 (1.48) | 43.21 (1.36) | 54.71 (1.31) | 46.35 (0.96) | |
| Non-Hispanic Other | 2.30 (0.08) | 37.59 (1.53) | 30.04 (1.33) | 20.35 (0.94) | 20.33 (0.54) | |
| Region | < 0.0001 | |||||
| Northeast | 16.63 (0.40) | 21.90 (1.07) | 20.32 (1.07) | 20.74 (0.90) | 23.06 (0.79) | |
| Midwest | 25.84 (0.88) | 18.35 (1.42) | 13.47 (1.10) | 12.84 (0.73) | 11.00 (0.54) | |
| South | 37.51 (0.84) | 35.80 (1.70) | 36.51 (1.53) | 37.21 (1.49) | 31.48 (1.27) | |
| West | 20.02 (0.43) | 23.95 (1.19) | 29.70 (1.18) | 29.21 (1.12) | 34.47 (0.91) | |
| Education | < 0.0001 | |||||
| Less than high school | 6.88 (0.14) | 11.85 (0.82) | 17.85 (0.94) | 22.59 (0.94) | 18.16 (0.51) | |
| High school/GED | 20.99 (0.25) | 12.67 (0.95) | 17.77 (0.95) | 19.66 (0.84) | 18.40 (0.42) | |
| Some college | 34.22 (0.28) | 20.44 (1.22) | 19.51 (0.96) | 21.00 (0.82) | 26.00 (0.49) | |
| College degree | 37.91 (0.42) | 55.04 (1.52) | 44.87 (1.44) | 36.75 (1.21) | 37.44 (0.68) | |
| Employment | < 0.0001 | |||||
| Working for pay | 54.78 (0.29) | 50.75 (1.42) | 65.38 (1.21) | 67.45 (1.03) | 56.33 (0.60) | |
| Not working for pay/unemployed | 45.22 (0.29) | 49.25 (1.42) | 34.62 (1.21) | 32.55 (1.03) | 43.67 (0.60) | |
| Ratio to FPL | < 0.0001 | |||||
| Less than 1.00 | 14.91 (0.27) | 37.67 (1.49) | 25.62 (1.21) | 26.11 (1.01) | 19.31 (0.53) | |
| 1.00 – 1.99 | 18.28 (0.21) | 21.78 (1.05) | 26.66 (1.13) | 26.99 (0.98) | 23.65 (0.51) | |
| 2.00 – 2.99 | 17.02 (0.18) | 12.12 (0.94) | 18.02 (1.13) | 15.55 (0.80) | 16.33 (0.44) | |
| 3.00 or over | 49.80 (0.44) | 28.43 (1.36) | 29.70 (1.30) | 31.36 (1.23) | 40.71 (0.76) | |
| Serious Psychological Distress | 0.0002 | |||||
| Not Present | 96.32 (0.09) | 97.73 (0.36) | 97.76 (0.32) | 97.13 (0.39) | 96.01 (0.21) | |
| Present | 3.68 (0.09) | 2.27 (0.36) | 2.24 (0.32) | 2.87 (0.39) | 3.99 (0.21) | |
| Depressed? | < 0.0001 | |||||
| No | 60.06 (0.29) | 69.25 (1.20) | 67.78 (1.27) | 68.34 (0.96) | 64.72 (0.56) | |
| Yes | 39.94 (0.29) | 30.75 (1.20) | 32.22 (1.27) | 31.66 (0.96) | 35.28 (0.56) |
n = unweighted; N = weighted; FPL = Federal Poverty Line NUSB = Not US - Born
Table 2 shows the results of the logistic regressions for the two outcomes (SPD, depression) and their relationship with immigration status. There was no statistically significant difference in SPD between immigrants and US-born. For the outcome of depression, after adjusting for demographic factors, immigrants were found to be 11% (OR 0.89, 95% CI [0.85,0.95]) less likely to suffer from depression compared to US-born.
Table 2:
Logistic models for relationship between SPD and immigration status; and Depression and immigration status, unadjusted and adjusted for demographics
| Unadjusted Odds Ratio (95% Cl) |
Adjusted Odds Ratio (95% Cl) |
|
|---|---|---|
| Serious Psychological Distress | ||
| Immigration Status | ||
| Non-Immigrant (ref) | - | - |
| Immigrant | 0.94 (0.85,1.04) | 0.98(0.85,1.13) |
| Depression | ||
| Immigration Status | ||
| Non-Immigrant (ref) | - | - |
| Immigrant | 0.77 (0.74,0.81)*** | 0.89 (0.85,0.95)*** |
p-value <0.05,
p-value <0.01,
p-value <0.001
Table 3 shows the results from the logistic models for the relationship between the outcomes (SPD, depression) and length of residence in the US. After adjusting for demographic variables, those less than 5 years were 43% (OR 0.57, 95% CI [0.39,0.83]) less likely, 5 to less than 10 years were 38% (0.62, 95% CI [0.43,0.91]) less likely, 10 to less than 15 years were 20% (OR 0.80, 95% CI [0.58,1.10]) less likely, and 15+ years were 17% (OR 1.17, 95% CI [1.00,1.36]) more likely to have SPD compared to those who were born in the United States. All of these were statistically significant except for those with 10 to less than 15 years residence in the US. With regards to the outcome of depression, the adjusted model showed compared to those born in the United States, those less than 5 years were 32% (OR 0.68, 95% CI [0.59,0.77]) less likely, 5 to less than 10 years were 20% (OR 0.80, 95% CI [0.70,0.91]) less likely, and 10 to less than 15 years were 20% (OR 0.80, 95% CI [0.71,0.89]) less likely to be depressed. The results for those with less than 5 years, 5 to less than 10 years, 10 to less than 15 years were statistically significant with p < 0.001.
Table 3:
Logistic models for relationship between SPD and number of years in the US; and Depression and number of years in the US, unadjusted and adjusted for demographics
| Unadjusted Odds Ratio (95% CI) |
Adjusted Odds Ratio (95% CI) |
|
|---|---|---|
| Serious Psychological Distress | ||
| Years in the United States | ||
| Born in US (ref) | - | - |
| < 5 | 0.61 (0.43,0.87)** | 0.57 (0.39,0.83)** |
| 5 – < 10 | 0.60 (0.42,0.85)** | 0.62 (0.43,0.91)* |
| 10 – <15 | 0.77 (0.58,1.03) | 0.80 (0.58,1.10) |
| 15 + | 1.09 (0.97,1.22) | 1.17 (1.00,1.36)* |
| Depression | ||
| Years in the United States | ||
| Born in US (ref) | - | - |
| < 5 | 0.67 (0.59,0.75)*** | 0.68 (0.59,0.77)*** |
| 5 – < 10 | 0.72 (0.63,0.81)*** | 0.80 (0.70,0.91)*** |
| 10 – < 15 | 0.70 (0.63,0.77)*** | 0.80 (0.71,0.89)*** |
| 15 + | 0.82 (0.78,0.86)*** | 0.97 (0.91,1.04) |
p-value <0.05,
p-value <0.01,
p-value <0.001
Table 4 shows the prevalence of depression and SPD with confidence interval for each time point overall. US-born (p<0.0001) were found to have a higher prevalence of depression compared to immigrants, however, the prevalence of depression decreased overtime (p=0.011) for both immigrants and US-born individuals. It was found that as length of residence increased, the prevalence of SPD (p=0.002) and depression (p<0.0001) increased for immigrants.
Table 4.
Prevalence of Depression and SPD by year with 95% Confidence Intervals
| Prevalence of Depression (95% Confidence Interval) | ||||
|---|---|---|---|---|
| Year | 2010 | 2012 | 2014 | 2016 |
| Immigrant | 0.357 (0.355,0.358) | 0.349 (0.348,0.351) | 0.319 (0.318,0.320) | 0.336 (0.335,0.337) |
| US-Born | 0.440 (0.439,0.40) | 0.379 (0.378,0.379) | 0.383 (0.382,0.383) | 0.384 (0.383,0.384) |
| Prevalence of SPD (95% Confidence Interval) | ||||
| Year | 2010 | 2012 | 2014 | 2016 |
| Immigrant | 0.0297 (0.0292,0.0301) | 0.0311 (0.0307,0.0316) | 0.0340 (0.0336,0.0343) | 0.0330 (0.0327,0.0333) |
| US-Born | 0.0356 (0.0354,0.0359) | 0.0312 (0.0310,0.0314) | 0.0332 (0.0331,0.0333) | 0.0402 (0.0400,0.0403) |
Figure 1 illustrates the trend in SPD and depression by immigration status. The immigrant population has a lower percentage of depression than their non-immigrants counterparts, and overall trends of depression for both groups have decreased from 2010–2016.
Figure 1:
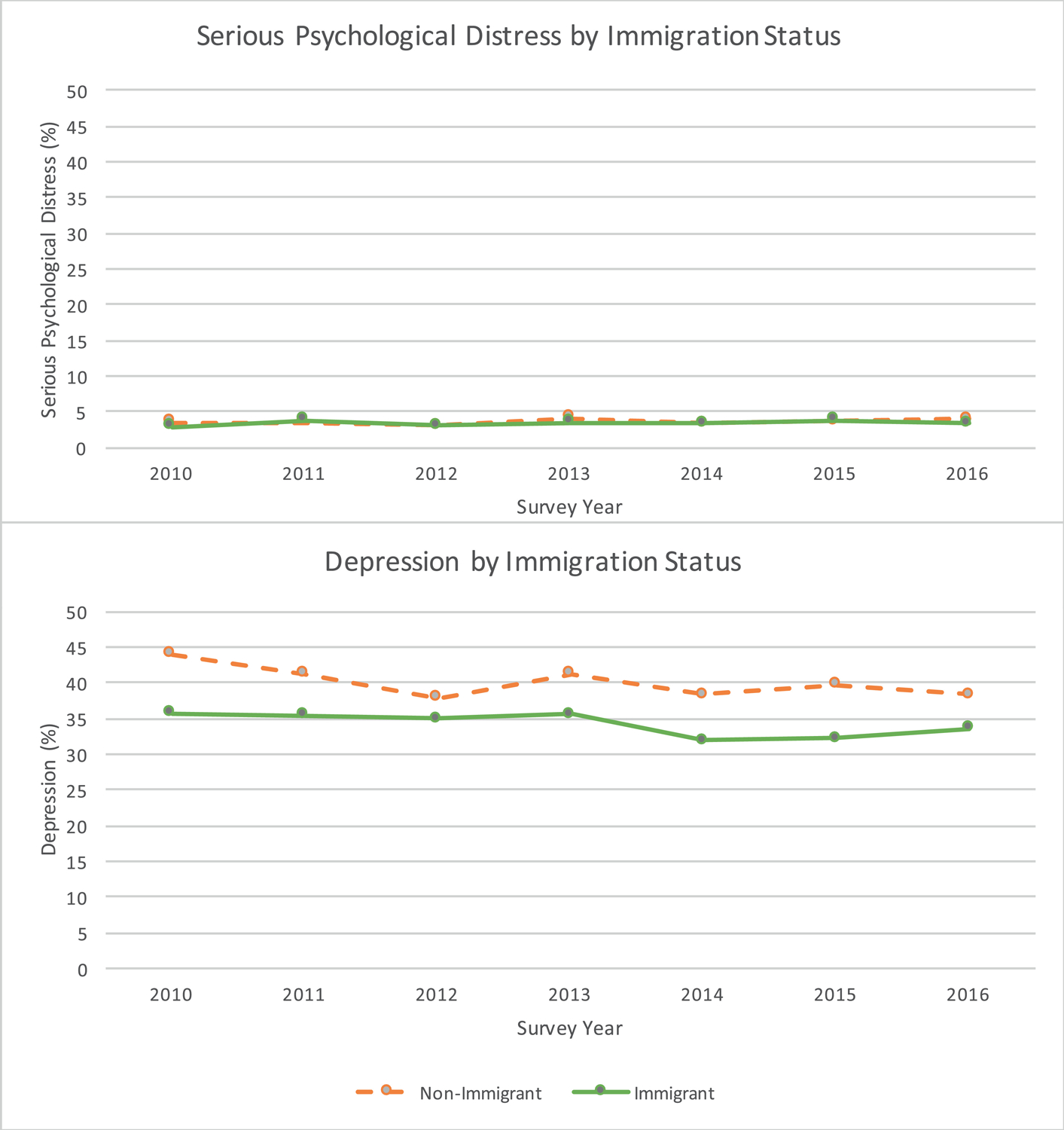
Trends in serious psychological distress & depression by immigration status
Footnote: National Health Interview Survey data is cross-sectional data, the survey was not collected form the same participants over the 2010 – 2016 period.
Figure 2 shows the trends in SPD and depression by the length of residence. From 2010–2016, the overall percentage of people with SPD has slightly increased for those in the US less than 5 years, 5 to less than 10 years, 15+ years and those who were born in the US. Serious psychological distress decreased over time for those in the US 10 to less than 15 years. The overall trend in percentage of depression has almost remained constant for those in the US less than 5 years, has slightly increased for those 5 to less than 10 years, has increased for those in the US 10 to less than 15 years, and has decreased for those with 15+ years and who were born in the United States.
Figure 2:
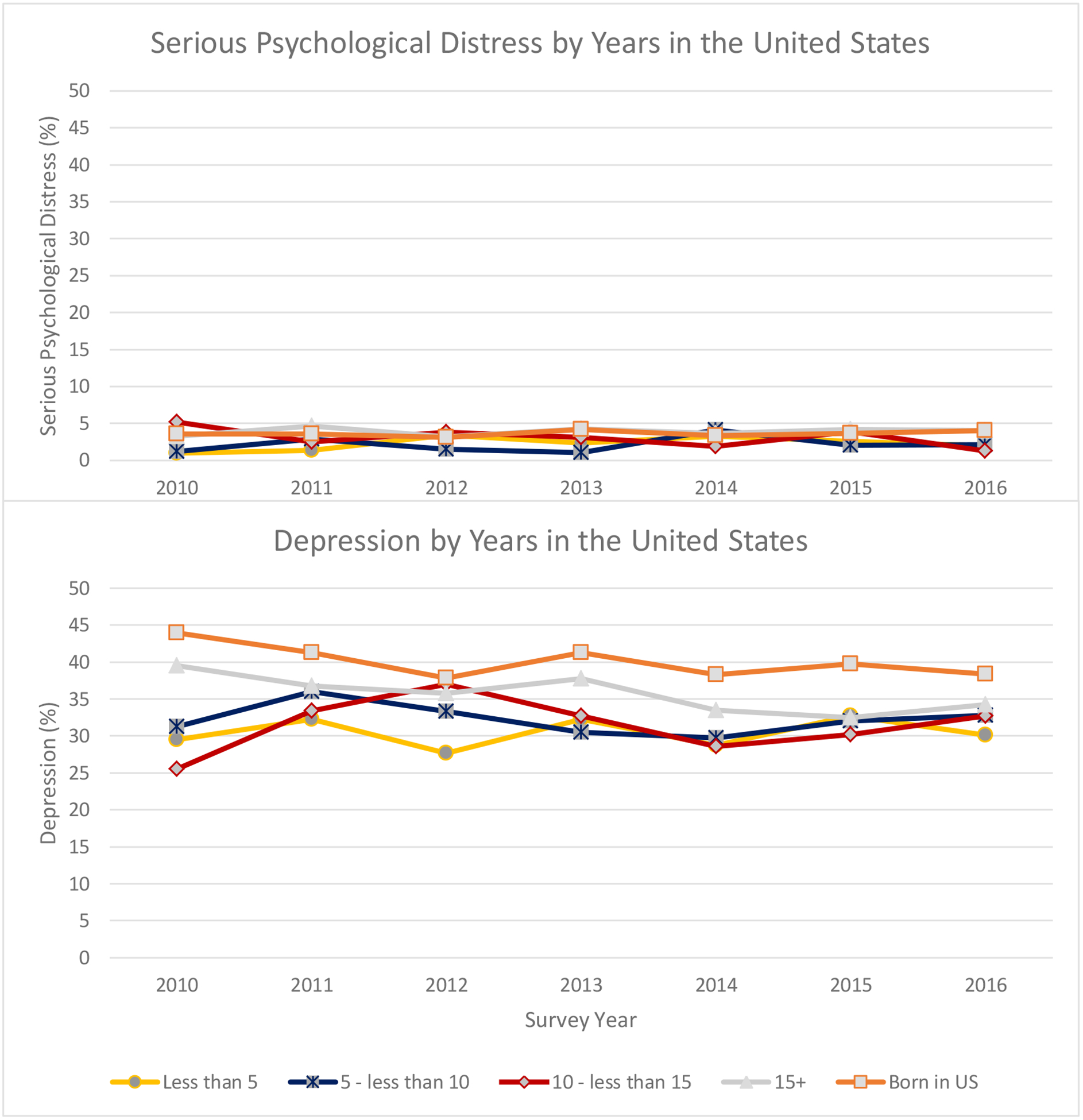
Trends in serious psychological distress & depression by years in the United States
Discussion
Analysis of the 2010–2016 NHIS data revealed that immigrants had a lower prevalence of depression than non-immigrants, with overall prevalence of depression decreasing across both groups over time. We found the odds of SPD and depression increased as the length of residence increased in immigrants, with the odds of SPD in immigrants who reside in the US 15 years or more surpassing the odds of the US-born population. After adjusting for demographics and co-morbidities, immigrants were found to be 11% less likely than US born individuals to report being depressed. Amongst immigrants, the more time they spend in the US, the more likely they are to resemble the US born population, in terms of reporting depression.
This is the first study to examine trends in depression and SPD prevalence, specifically looking at differences between those born in the US and immigrants in a national dataset over seven years. This is also the first study to our knowledge to reveal that the odds of immigrants reporting SPD are greater than non-immigrants, after immigrants have been in the US for 15 years or longer. There appears to be a protective aspect of immigrant status on SPD, as the results show that immigrants who have been in the US for less than 5 years are 43 percent less likely that non-immigrants to report SPD. These findings support the well-studied “health immigrant effect”, wherein recent migrants appear to have better health outcomes across disciplines, when compared to non-recent migrants28. However, this protective factor decreases over time and eventually goes away after immigrants have spent 15 or more years in the US. Additional research needs to be done to understand drivers of mental health among diverse immigrant groups.
Our findings are consistent with some previous research that found non-Hispanic foreign-born Whites to be more likely than US-born non-Hispanic Whites to report SPD29. Our study gives a new perspective by showing how the amount of time an immigrant spends in the US can also impact their likelihood of reporting SPD and depression. With regards to mental health trends, some previous studies have looked at longitudinal trends in SPD among various populations. Similar findings have been seen in a study conducted among immigrants in Canada. The findings showed that immigrants who lived in Canada for less than 2 years were less likely to report high mental distress compared to those who lived in Canada 2 to 20 years30. While our study is similar in that it looks at mental health trends, we took an extra step of creating immigrant population subgroups sorted by length of time spent as a resident in the US, in order to examine these trends in more detail, and reveal new insights.
Our findings suggest that residing in the US for an extended period of time increases the odds of reporting mental health conditions such as SPD and depression. Mental health interventions should be targeted towards long-term US immigrants to address depression and SPD in this population. Private and public insurance providers should revise protocols to ensure that immigrant populations have the ability to access adequate mental health care while residing in the US. “Community-based” mental health services are often under-funded and lack the resources needed to serve their communities, resulting in a weakened infrastructure31. Providing the necessary resources and support to these programs will help not only immigrant populations, but US born individuals as well. Future research should look into the possibility of exploring whether immigrants living in places with adequate mental health support, find their “healthy immigrant effect” persists longer than 5–10 years.
The study was strengthened by the use of a large sample size from multiple years of nationally representative data that allowed for the examination of trends and generalizability of the findings to the US population. However, there are a few limitations to this study. First, this is a cross-sectional study causation cannot be determined using the data. Second, this study examines immigrants as an entire population, not taking into account differences in immigrant status such as undocumented, naturalized citizens, refugees, and permanent residents, for example. Third, the immigrant data was pooled on a national level for purposes of the analysis; we did not separate immigrants by region of origin which may have impacted the way they responded to the survey. Prior research has shown that immigrant regions of origin can play an important role in prevalence of health conditions, and outcomes of chronic disease11,32. Fourth, we used a single item to define depression. Although, we did not use the “gold standard” of a psychiatric interview for the diagnosis of depression, for population surveys, the item used identified individuals likely to be depressed. Fifth, the dataset does not have community or health system level information needed to conduct multi-level analyses as all data is collected at the individual level. This may be an area of interest in future analyses within datasets that allow multi-level modelling.
Conclusions
In conclusion, the study found that the prevalence of depression is lower in immigrants compared to US-born and has decreased over time in both groups. Findings also showed that while newer immigrants have reduced odds of reporting SPD compared to US-born, the odds of SPD increase as the length of residence increases in immigrants, surpassing the odds of SPD in the US-born population for immigrants who reside in the US 15 years or longer. Mental health interventions targeting long-term immigrants in the US may show promise in improving mental health outcomes in this group. Immigration services should be sure to take into account potential underlying mental health conditions when interacting with heavy-immigrant communities.
Highlights:
Mental illness is highly prevalent impacting about18% of US adults
Immigrants are exposed to factors in migration that impact health outcomes
Immigrants had a lower prevalence of depression compared to US born
Odds of SPD increase as time in US increases, surpassing odds of SPD in US-born
Acknowledgements:
Financial Support: Effort partially supported by NIH/NIDDK (K24DK093699, R01DK118038, R01DK120861, PI: Egede), NIH/NIMHD (R01MD013826, PI: Egede/Walker), ADA (1-19-JDF-075, PI: Walker) and the study sponsors had no role in study design, collection, analysis, interpretation, or writing of report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors declare no conflict of interest.
Ethical Standards Disclosure: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Institutional Review Board of the Medical College of Wisconsin, Milwaukee, WI, USA.
References
- 1.Mental Health America. The State of Mental Health in America. 2015. http://www.mentalhealthamerica.net/issues/state-mental-health-america. Accessed June 21, 2018.
- 2.Luppa M, Sikorski C, Luck T, et al. Age- and gender-specific prevalence of depression in latest-life - Systematic review and meta-analysis. J Affect Disord. 2012;136(3):212–221. [DOI] [PubMed] [Google Scholar]
- 3.National Institute of Mental Health. Major Depression. 2017. https://www.nimh.nih.gov/health/statistics/major-depression.shtml. Accessed November 20, 2018.
- 4.Greenberg PE, Fournier A-A, Sisitsky T, Pike CT, Kessler RC. The Economic Burden of Adults With Major Depressive Disorder in the United States (2005 and 2010). J Clin Psychiatry. February 2015:155–162. [DOI] [PubMed] [Google Scholar]
- 5.Weissman J, Pratt L, Miller E, Parker J. Serious psychological distress among adults: United States, 2009 – 2013. NCHS Data Brief. 2015;203:1–8. [PubMed] [Google Scholar]
- 6.Pratt L, Dey A, Cohen A. Characteristics of adults with serious psychological distress as measured by the K6 scale: United States, 2001 – 04. Adv Data. 2007;382:1–18. [PubMed] [Google Scholar]
- 7.Murray CJL. The State of US Health, 1990–2010: Burden of Diseases, Injuries, and Risk Factors. JAMA. 2013;310(6):591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The Global Burden of Mental, Neurological and Substance Use Disorders: An Analysis from the Global Burden of Disease Study 2010. Forloni G, ed. PLOS ONE. 2015;10(2):e0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luciano A, Nicholson J, Meara E. The economic status of parents with serious mental illness in the United States. Psychiatr Rehabil J. 2014;37(3):242–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and Lifetime Prevalence of DSM-IV PsychiatricDisorders Among Mexican Americans and Non-Hispanic Whites in the United States: Results From the National Epidemiologic Survey on Alcohol and RelatedConditions. Arch Gen Psychiatry. 2004;61(12):1226. [DOI] [PubMed] [Google Scholar]
- 11.Dey AN, Lucas JW. Physical and mental health characteristics of U.S.- and foreign-born adults: United States, 1998–2003. Adv Data. 2006;(369):1–19. [PubMed] [Google Scholar]
- 12.Zong J, Batalova J, Hallock J. Frequently requested statistics on immigrants and immigration in the United States. 2018. https://www.migrationpolicy.org/article/frequently-requested-statistics-immigrants-and-immigration-united-states. Accessed June 21, 2018.
- 13.Wong EC, Miles JNV. Prevalence and Correlates of Depression Among New U.S. Immigrants. J Immigr Minor Health. 2014;16(3):422–428. [DOI] [PubMed] [Google Scholar]
- 14.Akresh IR, Frank R. Health Selection Among New Immigrants. Am J Public Health. 2008;98(11):2058–2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kennedy S, Kidd MP, McDonald JT, Biddle N. The Healthy Immigrant Effect: Patterns and Evidence from Four Countries. J Int Migr Integr. 2015;16(2):317–332. [Google Scholar]
- 16.Siddiqi A, Ornelas IJ, Quinn K, Zuberi D, Nguyen QC. Societal context and the production of immigrant status-based health inequalities: A comparative study of the United States and Canada. J Public Health Policy. 2013;34(2):330–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams DR, Haile R, González HM, Neighbors H, Baser R, Jackson JS. The Mental Health of Black Caribbean Immigrants: Results from the National Survey of American Life. Am J Public Health. 2007;97(1):52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alegría M, Sribney W, Woo M, Torres M, Guarnaccia P. Looking Beyond Nativity: The Relation of Age of Immigration, Length of Residence, and Birth Cohorts to the Risk of Onset of Psychiatric Disorders for Latinos. Res Hum Dev. 2007;4(1–2):19–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown MJ, Cohen SA, Mezuk B. Duration of US residence and suicidality among racial/ethnic minority immigrants. Soc Psychiatry Psychiatr Epidemiol. 2015;50(2):257–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garcini LM, Peña JM, Galvan T, Fagundes CP, Malcarne V, Klonoff EA. Mental disorders among undocumented Mexican immigrants in high-risk neighborhoods: Prevalence, comorbidity, and vulnerabilities. J Consult Clin Psychol. 2017;85(10):927–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li M, Anderson JG. Pre-migration Trauma Exposure and Psychological Distress for Asian American Immigrants: Linking the Pre- and Post-migration Contexts. J Immigr Minor Health. 2016;18(4):728–739. [DOI] [PubMed] [Google Scholar]
- 22.Kirmayer L, Narasiah L, Munoz M, et al. Common mental health problems in immigrants and refugees: general approach in primary care. CMAJ. 2011;183(12):E959–E967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the Prevalence of Major Depression and Comorbid Substance Use Disorders in the United States Between 1991–1992 and 2001–2002. Am J Psychiatry. 2006;163(12):2141–2147. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. National Health Interview Survey. 2018. https://www.cdc.gov/nchs/nhis/index.htm. Accessed June 25, 2018.
- 25.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. [DOI] [PubMed] [Google Scholar]
- 26.Peiper N, Clayton R, Wilson R, Illback R. The performance of the K6 Scale in a large school sample. Psychol Assess. 2015;27(1):228–238 [DOI] [PubMed] [Google Scholar]
- 27.Koya D, Egede L. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22:841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ichou M, Wallace M. The Healthy Immigrant Effect: The role of educational selectivity in the good health of migrants. Demogr Res. 2019;40(4):61–94. [Google Scholar]
- 29.Dallo FJ, Kindratt TB, Snell T. Serious psychological distress among non-Hispanic whites in the United States: the importance of nativity status and region of birth. Soc Psychiatry Psychiatr Epidemiol. 2013;48(12):1923–1930. [DOI] [PubMed] [Google Scholar]
- 30.Pahwa P, Karunanayake CP, McCrosky J, Thorpe L. Longitudinal trends in mental health among ethnic groups in Canada. Chronic Dis Inj Can. 2012;32(3):164–176. [PubMed] [Google Scholar]
- 31.Mapanga W, Casteleijn D, Ramiah C, et al. Strategies to strengthen the provision of mental health care at the primary care setting: An Evidence Map. PLoS ONE. 2019;14(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Engelman M, Ye LZ. The Immigrant Health Differential in the Context of Racial and Ethnic Disparities: The Case of Diabetes. Adv Med Sociol. 2019;19:147–171. [DOI] [PMC free article] [PubMed] [Google Scholar]


