Abstract
Bladder injury is the most common urological trauma following the gynecological procedure. Normal vaginal delivery candidates with unresponsive and prolonged ascites and bladder‐emptying complaints should be examined for bladder rupture. We also suggest measurement of ascitic fluid creatinine levels in these patients.
Keywords: bladder rupture, creatinine, gynecological procedure, urological trauma, vaginal delivery
Bladder injury is the most common urological trauma following the gynecological procedure. Normal vaginal delivery candidates with unresponsive and prolonged ascites and bladder‐emptying complaints should be examined for bladder rupture. We also suggest measurement of ascitic fluid creatinine levels in these patients.
1. INTRODUCTION
Injury to the bladder is an uncommon occurrence in 1.6% of blunt traumas; however seldom, it can be spontaneous. 1 Increased visceral pressure and weakening of the bladder are the chief predisposing causes of the bladder rupture. Diagnosing bladder rupture has faced many challenges within the past few years, even by the means of diagnostic modalities such as CT scan. 2 Bladder traumas can be intraperitoneal (within the peritoneum), where urine leaks into the peritoneal space. The most common clinical findings include hematuria (gross), supra‐pubic pain, and inability to void. 3
An increase in intraperitoneal pressure during intrapartum and postpartum has also been reported to cause bladder rupture. 4
2. CASE REPORT
A 27‐year‐old primipara had a normal vaginal delivery where a healthy boy with 41 weeks of gestational age was born. There was no history of previous abortion, abdominal surgery, or trauma before the delivery. The patient was discharged on 2nd postoperative day with normal electrolytes and vital signs and without any complications.
Three days later, she was presented to the emergency department with drowsiness and abdominal distention. Physical examination and laboratory results showed generalized abdominal tenderness and moderate ascites, followed by acute renal failure (Cr: 5 mg/dL, normal range: 0.5‐1.1 mg/dL). The patient underwent a session of hemodialysis, owing to her uremic state. Because of her deteriorating condition, the patient was referred to another hospital equipped with specialized wards. Her vitals were as follows: blood pressure of 80/60 mm Hg, pulse rate of 143/min, and temperature of 38.4.
The abdomen was distended due to ascites, documented from the previous center. The patient did not have any history of urinary problems, but bladder‐emptying issues. Mild tenderness in hypogastrium was also reported. There was no abdominal rigidity or guarding. Vaginal examination revealed a healthy episiotomy without significant bleeding.
Due to the primary suspicion of septic shock, the conservative treatment was implemented as follows: fluid therapy and empirical antibiotic. Diuresis was treated by the placement of catheter to decompress the bladder. Her laboratory data showed WBC 20 300 (N 90%, L 8%), Hb 11.1 g/dL, BUN 53, Cr 3.1, ESR 47, and CRP ++, and blood culture was negative. The only abnormality in the abdominal ultrasonography was moderate ascites, and the analysis showed high serum ascites albumin gradient (SAAG) of 1.8, glucose 82, LDH 1964, WBC 2800 (poly 90%), and RBC 800. The ascitic fluid culture was positive for gram‐positive cocci. A contrast‐enhanced CT imaging of the abdomen and pelvis was performed. The main finding in the imaging was moderate ascites with multiple septations where no other organ damage or abnormality was seen (Figure 1). A week following antibiotic therapy, patient was in good general conditions therefore, was transferred to post‐ICU. The urinary catheter was discontinued, but due to persistent difficulty of voiding, a urinary catheter was reinserted.
Figure 1.
Ascitic fluid in abdominal‐pelvic fossa
Ten days after her admission, the patient complained of having abdominal pain. Also, no improvement in ascites volume was seen. Further analysis of ascites showed LDH 5245, protein 3.6, WBC 970, RBC 1390, and high serum ascites albumin gradient.
Due to the concern of secondary peritonitis and owing to unresponsiveness to the treatment, abdominal laparoscopy was performed, and severe adhesion in abdominal fossa was seen along with fibrin tissue and severe inflammation. Pathologic report stated no malignant cell or granulomatosis, and only nonspecific inflammatory cell was seen. ADA (adenosine deaminase) and second culture were negative. However, the patient had abdominal pain and prolonged ascites.
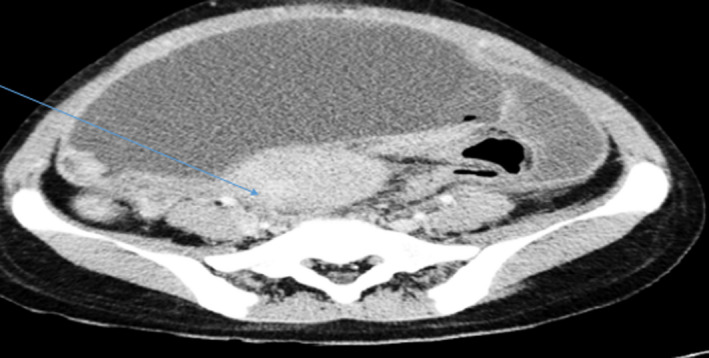
Finally, the patient underwent a midline abdominal laparotomy. Surprisingly, a defect in the posterior wall of the urinary bladder was detected, consistent with intraperitoneal bladder rupture (Figures 2 and 3). Analysis of Cr in ascites showed urinary ascites (ascites Cr: 9.2 mg/dL). Throughout the examination, we found that a bladder rupture was missed. Two weeks after the repair of the bladder wall, ascitic fluid and pain were decreased. We did not notice the patient's inability to void bladder after the initial urinary catheter removal. We assume that measuring Cr levels in ascitic fluid would have saved invasive and expensive examination.
Figure 2.
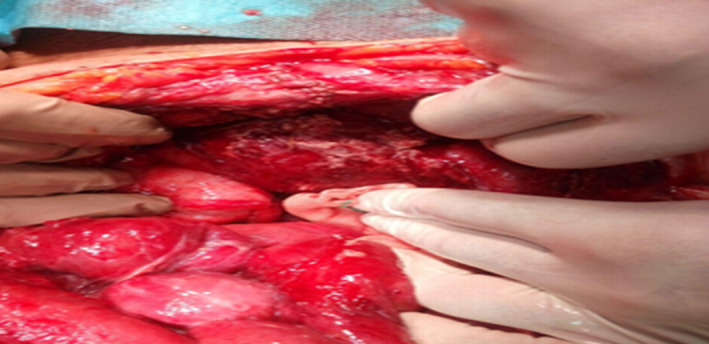
Open laparotomy finding related to bladder rupture
Figure 3.
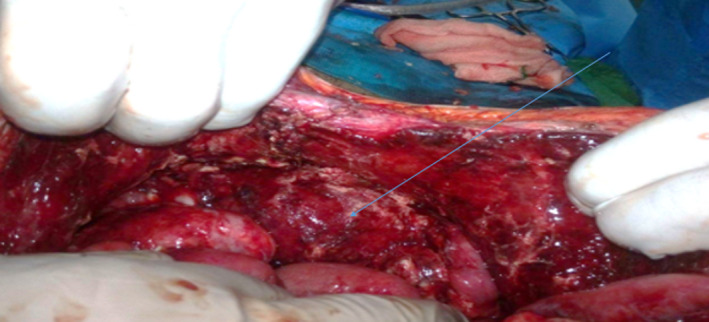
Repaired bladder rupture
3. DISCUSSION
Bladder injuries can occur due to blunt or penetrating trauma. Some blunt traumas are iatrogenic, which occur following the obstetric/gynecologic surgery or vaginal delivery. 5 , 6
In comparison with cesarean section, normal vaginal delivery rarely leads to urinary system injury. In 1995, Kibel et al reported this injury for the first time. 7 Later, few more cases in this regard were reported. 8 , 9 , 10
Urinary bladder rupture after vaginal delivery is usually caused by uterine rupture. Unsatisfactory bladder emptying during pregnancy causes the retention of urine. During delivery, this can build the pressure in the bladder and cause the rupture. Furthermore, continuous pressure from the head of the fetus during contractions, particularly if the patient is not catheterized, can lead to the rupture. Interestingly, a small amount of urination is likely to be deceiving for clinicians in such cases. 10
Previous reports have demonstrated multiple presentations such as abdominal ascites and pain related to peritonitis or sepsis following bladder rupture. Our case had unexplained prolonged ascites for 10 days following delivery. However, a case of delayed diagnosis of bladder rupture for 20 days has been reported. 11 Studies have mentioned anuria or urinary retention as a sign of bladder rupture. Unfortunately, in our cases, none of the common signs of bladder rupture was seen. One of the important presentations of bladder rupture is the inability to empty the bladder completely, of which our patient complained after the removal of the initial catheter. Instrumental delivery or deep vaginal tears (not documented in our case) are the other risk factors for bladder injury following delivery. Contrary to other reports, hematuria, another important sign of the rupture was also not found in this case. 12
Conclusively, beyond symptoms and signs, suspicion of the physician to bladder rupture may be an important factor for rapid diagnosis of bladder rupture.
Irritation due to urine following intraperitoneal rupture may result in peritonitis or sepsis. Nonetheless, the diagnosis of sepsis leads to the delay in the diagnosis of urinary peritonitis. 13 , 14 , 15 Our case had prolonged ascites after the eradication of infectious peritonitis (negative culture). Urinary ascites is suspected when the analysis of fluid shows higher creatinine or urea than the serum. 16
Our patient's ascitic fluid creatinine was 9 mg/dL. Some reports have noticed pseudo‐renal failure because of creatinine diffusion into the circulation. 17 Mokoena and Naidu have reported creatinine elevation near to 4.1 mg/dL. 18 Transient creatinine elevation related to hemodynamic instability was seen in this case, which was treated by conservative management. The diagnosis of bladder rupture is done with cystography. Because of the low index of suspicion to bladder injury and invasiveness of the technique, this procedure is not common in the initial steps of patients’ evaluation. For the prevention of bladder rupture, emptying of the bladder during delivery is advised. Nevertheless, our patient underwent urinary catheterization during labor.
4. CONCLUSION
In summary, even without known risk factors, a physician must notice patients’ urologic and abdominal complaints following the vaginal delivery. Prolonged ascites and unresponsiveness to initial medical treatment must be precisely noticed. 19 Before complex and expensive evaluation, the analysis of ascitic fluid for creatinine concentration is an initial and a simple diagnostic tool for urinary ascites. Voiding history should be elicited in all postpartum women with unexplained ascites, peritonitis, and shock.
CONFLICT OF INTEREST
The authors deny any conflict of interest in any terms or by any means during the study. All the fees provided by the research center fund and deployed accordingly.
AUTHOR CONTRIBUTIONS
BH and AZ: conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. SN: designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript. MG: coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
ACKNOWLEDGMENTS
Published with written consent of the patient.
Hadian B, Nazarpoor S, Garshasebi M, Zafar Mohtashami A. Missed bladder rupture following vaginal delivery: Possible role of assessing ascitic fluid creatinine levels?. Clin Case Rep. 2020;8:1247–1250. 10.1002/ccr3.2900
REFERENCES
- 1. Gomez RG, Ceballos L, Coburn M et al Consensus statement on bladder injuries. BJU Int. 2004;94(1):27‐32. [DOI] [PubMed] [Google Scholar]
- 2. Palthe S, Dijkstra GA, Steffens MG. A case of spontaneous urinary bladder rupture secondary to urinary retention due to an urethral stricture. Urol Case Rep. 2018;17:85‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morey AF, Brandes S, Dugi DD et al Urotrauma: AUA guideline. J Urol. 2014;192(2):327‐335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Farahzadi A, Mohammadipour S. A late presentation of spontaneous bladder rupture during labor. Urol Case Rep. 2016;8:24‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cohen AJ, Packiam VT, Nottingham CU, Pariser JJ, Faris SF, Bales GT. Iatrogenic bladder injury: national analysis of 30‐day outcomes. Urology. 2016;97:250‐256. [DOI] [PubMed] [Google Scholar]
- 6. Teeluckdharry B, Gilmour D, Flowerdew G. Urinary tract injury at benign gynecologic surgery and the role of cystoscopy: a systematic review and meta‐analysis. Obstet Gynecol. 2015;126(6):1161‐1169. [DOI] [PubMed] [Google Scholar]
- 7. Kibel AS, Staskin DR, Grigoriev VE. Intraperitoneal bladder rupture after normal vaginal delivery. J Urol. 1995;153(3):725‐727. [DOI] [PubMed] [Google Scholar]
- 8. Kattan S. Maternal urological injuries associated with vaginal deliveries: change of pattern. Int Urol Nephrol. 1997;29(2):155‐161. [DOI] [PubMed] [Google Scholar]
- 9. Png K, Chong Y, Ng C. Two cases of intraperitoneal bladder rupture following vaginal delivery. Singapore Med J. 2008;49(11):e327‐e329. [PubMed] [Google Scholar]
- 10. BaHeti VH, Wagaskar VG, Patwardhan SK. Missed iatrogenic bladder rupture following normal vaginal delivery. J Clin Diagn Res. 2015;9(10):PD01‐PD02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Farahzadi A, Mohammadipour S. A late presentation of spontaneous bladder rupture during labor. Urol Case Rep. 2016;8:24‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lynch TH, Martínez‐Piñeiro L, Plas E et al EAU guidelines on urological trauma. Eur Urol. 2005;47(1):1‐15. [DOI] [PubMed] [Google Scholar]
- 13. Alhamzawi HH, Abdelrahman HM, Abdelrahman KM, El‐Menyar A, Al‐Thani H, Latifi R. Delayed presentation of traumatic intraperitoneal rupture of urinary bladder. Case Rep Urol. 2012;2012:1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dat A, Yip CL, Hanegbi U. Beware of the ‘Ascites’ patient: delayed presentation of traumatic intraperitoneal bladder rupture. Urol Case Rep. 2016;4:11‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ghosh S, Chatterjee N, Mukhopadhyay M, Brahmachari R, Maity P, Das A. Urinary ascites‐a consequence of intraoperative injury. J Assoc Physicians India. 2015;63:77. [PubMed] [Google Scholar]
- 16. Sharma A, Teh B, Morgan D, Bell D, Woodhouse C. When ascites is not ascites. Postgrad Med J. 2008;84(995):502‐503. [DOI] [PubMed] [Google Scholar]
- 17. Mark A, Meister M, Opara B, Chow R. Nontraumatic urinary bladder rupture presenting as renal pseudo‐failure and ascites. Radiol Case Rep. 2017;12(2):304‐307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mokoena T, Naidu A. Diagnostic difficulties in patients with a ruptured bladder. Br J Surg. 1995;82(1):69‐70. [DOI] [PubMed] [Google Scholar]
- 19. Shah R, Ramakrishnan M, Ahmed B, Abuamr K, Yousef O. Perforated bladder as a cause of abdominal ascites in a patient presenting with acute onset abdominal pain. Cureus. 2017;9(5):e1241. [DOI] [PMC free article] [PubMed] [Google Scholar]


