Acute kidney injury (AKI), a predictor for poor clinical outcomes, has been reported as a severe complication of different coronavirus infections, including novel coronavirus disease 2019 (COVID-19) [1]. COVID-19 is considered more contagious than previous coronavirus infections, e.g., severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) [2], but comparisons of mortality rates from AKI among these three coronavirus infections remain uninvestigated. We therefore conducted a systematic review and meta-analysis comparing the mortality rate in patients with SARS, MERS, and COVID-19 who developed AKI.
A systematic search of PUBMED and EMBASE from inception to June 5, 2020, included the keywords “coronavirus”, “COVID-19”, “MERS”, “SARS”, “acute kidney injury”, “prognosis”, and “mortality” with suitable MeSH terms to identify observational studies of relevance, e.g., case reports, case series, cross-sectional studies, and cohort studies. Reference lists of included, published, systematic reviews identified in the search were screened for additional studies. We excluded conference abstracts, review articles, or studies without reports of AKI mortality. Two reviewers (YTC, SCS) screened titles and abstracts of search results for relevance and individually and independently assessed the full texts of selected results. The final list of included studies was derived by discussion and unanimous agreement from both authors. Statistical analyses were performed using MedCalc for Windows, version 15.0 (MedCalc Software, Ostend, Belgium). We report the mortality rate from AKI in SARS, MERS, and COVID-19 infections as proportions with 95% confidence interval (CI) based on random effects model, represented by forest plot. We detected heterogeneity among studies using the Cochran Q test, with p value < 0.10 indicating significant heterogeneity, and calculated I2 statistic to determine the proportion of total variation in study estimates attributable to heterogeneity.
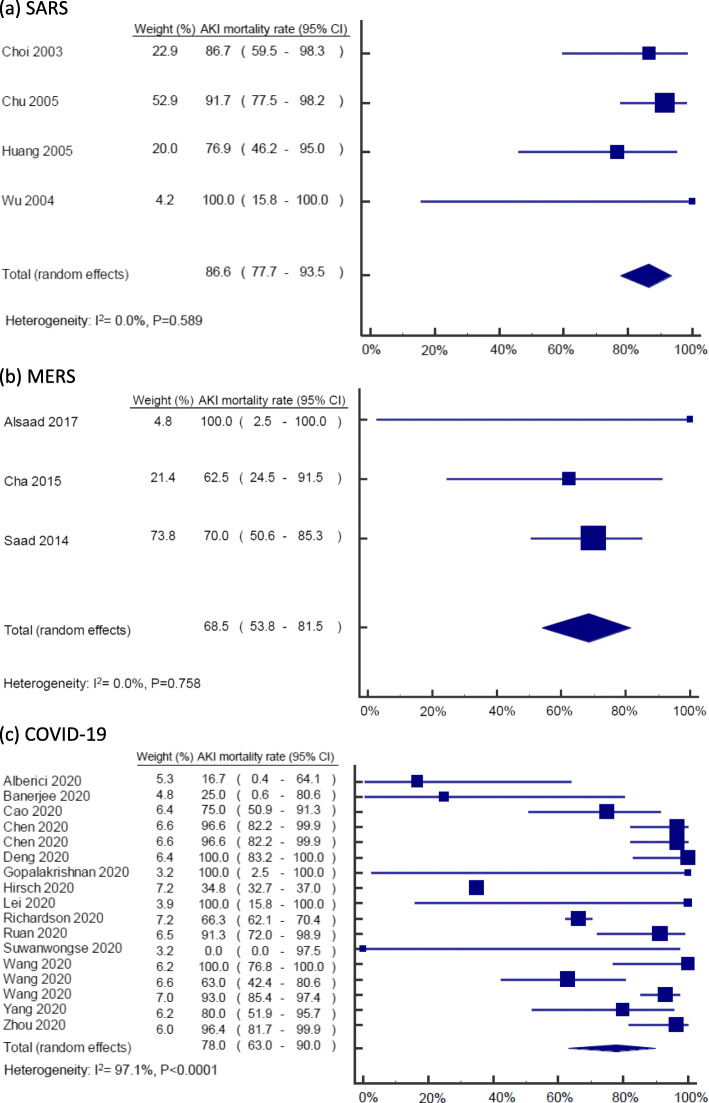
After screening 97 records in total, we excluded 74 articles (15 duplicates, 11 irrelevant to study question, 1 conference abstract, 5 review articles and 42 lacking data on AKI mortality). Our final analysis included 23 articles comprising 4, 3 and 16 on SARS, MERS and COVID-19 infection, respectively. Demographic data for included articles are presented in Table 1. Overall, mortality in patients with SARS, MERS and COVID-19 infection, and developing AKI, was 77.4% (95%CI: 64.7–88.0). We found the mortality rate of AKI was highest in SARS (86.6%; 95%CI: 77.7–93.5), followed by COVID-19 (76.5%; 95%CI: 61.0–89.0) and MERS (68.5%; 95%CI: 53.8–81.5). There was no evidence of statistical heterogeneity among studies reporting AKI mortality in SARS (I2: 0.0%, p = 0.589) and MERS (I2: 0.0%, p =v0.758), but there was for COVID-19 infection (I2: 97.0%, p < 0.001) (Fig. 1).
Table 1.
Study characteristics
| Author and year | Country/city | AKI male (%) | AKI age (median) | Settings | Total case numbers | AKI case numbers | Baseline serum creatinine (mg/dL) | RRT/AKI case (%) | AKI mortality (%) | Overall mortality (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| SARS | ||||||||||
| Huang 2005 [3] | Taiwan/Taipei | 77 | 65* | Hospitalization | 78 | 13 | 1.20 | 38 | 77 | 19 |
| Wu 2004 [4] | Taiwan/Taipei | 50 | 58* | Hospitalization | 2 | 2 | 1.05 | NA | 100 | 100 |
| Chu 2005 [5] | China/Hong Kong | 69 | 54 | Hospitalization | 536 | 36 | 1.06 | 28 | 92 | 14 |
| Choi 2003 [6] | China/Hong Kong | NA | NA | Hospitalization | 267 | 15 | NA | NA | 87 | 12 |
| MERS | ||||||||||
| Saad 2014 [7] | Saudi Arabia | NA | NA | Hospitalization | 70 | 30 | NA | NA | 70 | 60 |
| Alsaad 2017 [8] | Saudi Arabia | 100 | 33 | Intensive care unit | 1 | 1 | NA | 0 | 100 | 100 |
| Cha 2015 [9] | Korea | 63 | 73* | Hospitalization | 30 | 8 | 1.60 | 38 | 63 | 17 |
| COVID-19 | ||||||||||
| Alberici 2020 [10] | Italy/Brescia | 67 | 58* | Kidney transplantation/hospitalization | 20 | 6 | 3.13 | 17 | 17 | 25 |
| Hirsch 2020 [11] | USA/New York | 64 | 69 | Hospitalization | 5449 | 1993 | 1.24 | 14 | 35 | 16 |
| Lei 2020 [12] | China/Wuhan | NA | NA | Hospitalization | 34 | 2 | NA | NA | 100 | 21 |
| Chen 2020 [13] | China/Wuhan | NA | NA | Hospitalization | 274 | 29 | NA | 10 | 97 | 41 |
| Deng 2020 [14] | China/Wuhan | NA | NA | Hospitalization | 225 | 20 | NA | NA | 100 | 48 |
| Wang 2020 [15] | China/Wuhan | NA | NA | Hospitalization | 107 | 14 | NA | NA | 100 | 18 |
| Yang 2020 [16] | China/Wuhan | NA | NA | Hospitalization | 52 | 15 | NA | 60 | 80 | 62 |
| Gopalakrishnan 2020 [17] | USA | 100 | 49 | Hospitalization | 1 | 1 | 1.00 | 100 | 100 | 100 |
| Suwanwongse 2020 [18] | USA/New York | 100 | 88 | Hospitalization | 1 | 1 | 1.16 | 0 | 0 | 0 |
| Banerjee 2020 [19] | UK/London | 25 | 59* | Kidney transplantation/hospitalization | 7 | 4 | 2.54 | 75 | 25 | 14 |
| Zhou 2020 [20] | China/Wuhan | NA | NA | Hospitalization | 191 | 28 | NA | 36 | 96 | 28 |
| Wang 2020 [21] | China/Wuhan | NA | NA | Hospitalization | 339 | 27 | NA | NA | 63 | 19 |
| Richardson 2020 [22] | USA/New York | NA | NA | Hospitalization | 2351 | 523 | NA | 15 | 66 | 20 |
| Wang 2020 [23] | China/Wuhan | NA | NA | Intensive care unit | 344 | 86 | NA | 10 | 93 | 39 |
| Ruan 2020 [24] | China/Wuhan | NA | NA | Hospitalization | 150 | 23 | NA | 22 | 91 | 45 |
| Cao 2020 [25] | China/Wuhan | NA | NA | Hospitalization | 102 | 20 | NA | 30 | 75 | 17 |
AKI acute kidney injury, NA not available, RRT renal replacement therapy
*Age was represented by the mean value
Fig. 1.
Forest plot of AKI mortality in coronavirus infections from included studies: a SARS, b MERS, and c COVID-19
The present analyses indicate AKI as a poor prognosis factor in coronavirus infections, whereby AKI mortality in COVID-19 is higher than MERS but lower than SARS infections. Possible mechanisms of higher AKI mortality following coronavirus infections are multifactorial (e.g., severe sepsis-related multi-organ failure, direct kidney involvement, and acute respiratory distress syndrome) [26–28], although comparative pathogenesis of kidney involvement among the three infections remains unclear.
To our best knowledge, this is the first systematic review exploring AKI mortality of different coronavirus infections. However, we should be cautious about interpreting causal relationships between coronavirus infections and AKI, given the nature of observational data. Also, clinical heterogeneity between studies should be noted; for example, various healthcare systems of included studies may produce different AKI mortality rates. Coronaviruses are unlikely to be eliminated in the near future, and our synthesis indicates that AKI secondary to coronavirus infection may contribute to higher mortality. Hence, in the current exceptional pandemic, first-line healthcare providers should recognize the importance of timely detection of AKI and consider all available treatment options for maintenance of kidney functions to prevent death in COVID-19 patients [29].
Acknowledgements
None.
Abbreviations
- AKI
Acute kidney injury
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
- MERS
Middle East respiratory syndrome
- SARS
Severe acute respiratory syndrome
Authors’ contributions
YCY and SCS contributed equally to this work. YCY and SCS contributed to the critical analysis, interpretation of the data, and drafting of the manuscript. MJH and YCC contributed to the study supervision and administrative, technical, or material support. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
This original article has not been published and is not under consideration by another journal.
Competing interests
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yih-Ting Chen and Shih-Chieh Shao contributed equally to this work.
References
- 1.Chen Y-T, Shao S-C, Hsu C-K, Wu I-W, Hung M-J, Chen Y-C. Incidence of acute kidney injury in COVID-19 infection: a systematic review and meta-analysis. Critical Care. 2020;24(1):346. [DOI] [PMC free article] [PubMed]
- 2.Naicker S, Yang CW, Hwang SJ, Liu BC, Chen JH, Jha V. The novel coronavirus 2019 epidemic and kidneys. Kidney Int. 2020;97(5):824–828. doi: 10.1016/j.kint.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang JW, Chen KY, Tsai HB, Wu VC, Yang YF, Wu MS, Chu TS, Wu KD. Acute renal failure in patients with severe acute respiratory syndrome. J Formos Med Assoc. 2005;104(12):891–96. [PubMed] [Google Scholar]
- 4.Wu VC, Hsueh PR, Lin WC, Huang JW, Tsai HB, Chen YM, Wu KD. SARS. Research Group of the National Taiwan University College of Medicine and National University Hospital: Acute renal failure in SARS patients: more than rhabdomyolysis. Nephrol Dial Transplant. 2004;19(12):3180–182. [DOI] [PMC free article] [PubMed]
- 5.Chu KH, Tsang WK, Tang CS, Lam MF, Lai FM, To KF, Fung KS, Tang HL, Yan WW, Chan HWH, et al. Acute renal impairment in coronavirus-associated severe acute respiratory syndrome. Kidney Int. 2005;67(2):698–705. doi: 10.1111/j.1523-1755.2005.67130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi KW, Chau TN, Tsang O, Tso E, Chiu MC, Tong WL, Lee PO, Ng TK, Ng WF, Lee KC, et al. Outcomes and prognostic factors in 267 patients with severe acute respiratory syndrome in Hong Kong. Ann Intern Med. 2003;139(9):715–23. doi: 10.7326/0003-4819-139-9-200311040-00005. [DOI] [PubMed] [Google Scholar]
- 7.Saad M, Omrani AS, Baig K, Bahloul A, Elzein F, Matin MA, Selim MA, Al Mutairi M, Al Nakhli D, Al Aidaroos AY, et al. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis. 2014;29:301–06. doi: 10.1016/j.ijid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alsaad KO, Hajeer AH, Al Balwi M, Al Moaiqel M, Al Oudah N, Al Ajlan A, AlJohani S, Alsolamy S, Gmati GE, Balkhy H, et al. Histopathology of Middle East respiratory syndrome coronovirus (MERS-CoV) infection - clinicopathological and ultrastructural study. Histopathology. 2018;72(3):516–24. doi: 10.1111/his.13379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cha RH, Joh JS, Jeong I, Lee JY, Shin HS, Kim G, Kim Y. Critical Care Team of National Medical Center: Renal Complications and Their Prognosis in Korean Patients with Middle East Respiratory Syndrome-Coronavirus from the Central MERS-CoV Designated Hospital. J Korean Med Sci. 2015;30(12):1807–814. doi: 10.3346/jkms.2015.30.12.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alberici F, Delbarba E, Manenti C, Econimo L, Valerio F, Pola A, Maffei C, Possenti S, Zambetti N, Moscato M, et al. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020;97(6):1083–88. doi: 10.1016/j.kint.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirsch JS, Ng JH, Ross DW, Sharma P, Shah HH, Barnett RL, Hazzan AD, Fishbane S, Jhaveri KD. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98(1):209–18. [DOI] [PMC free article] [PubMed]
- 12.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, Zhan LY, Jia Y, Zhang L, Liu D, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. E Clinical Medicine. 2020;23:100385. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deng Y, Liu W, Liu K, Fang YY, Shang J, Zhou L, Wang K, Leng F, Wei S, Chen L, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: a retrospective study. Chin Med J (Engl) 2020;133(11):1261–267. doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang D, Yin Y, Hu C, Liu X, Zhang X, Zhou S, Jian M, Xu H, Prowle J, Hu B, et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan. China. Crit Care. 2020;24(1):188. doi: 10.1186/s13054-020-02895-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang X, Yu Y, Xu J, Shu H. Xia Ja, Liu H, Wu Y, Zhang L, Yu Z, Fang M et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gopalakrishnan A, Mossaid A, Lo KB, Vasudevan V, McCullough PA, Rangaswami J. Fulminant Acute Kidney Injury in a Young Patient with Novel Coronavirus 2019. Cardiorenal Med. 2020;10(4):217–22. [DOI] [PMC free article] [PubMed]
- 18.Suwanwongse K, Shabarek N. Rhabdomyolysis as a Presentation of 2019 Novel Coronavirus Disease. Cureus. 2020;12(4):e7561.Suwanwongse K, Shabarek N: Rhabdomyolysis as a Presentation of 2019 Novel Coronavirus Disease. Cureus. 2020;12(4):e7561. [DOI] [PMC free article] [PubMed]
- 19.Banerjee D, Popoola J, Shah S, Ster IC, Quan V, Phanish M. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020;97(6):1076–82. [DOI] [PMC free article] [PubMed]
- 20.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1038. [DOI] [PMC free article] [PubMed]
- 21.Wang L, He W, Yu X, Hu D, Bao M, Liu H, Zhou J, Jiang H. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80(6):639–45. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, Barnaby DP, Becker LB, Chelico JD, Cohen SL, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–59. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Y, Lu X, Li Y, Chen H, Chen T, Su N, Huang F, Zhou J, Zhang B, Yan F, et al. Clinical Course and Outcomes of 344 Intensive Care Patients with COVID-19. Am J Respir Crit Care Med. 2020;201(11):1430–434. doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruan Q, Yang K, Wang W, Jiang L, Song J. Correction to: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan. China. Intensive Care Med. 2020;46(6):1294–297. doi: 10.1007/s00134-020-06028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao J, Tu WJ, Cheng W, Yu L, Liu YK, Hu X, Liu Q: Clinical Features and Shortterm Outcomes of 102 Patients with Corona Virus Disease 2019 in Wuhan, China. Clin Infect Dis. 2020;ciaa243. [DOI] [PMC free article] [PubMed]
- 26.Eckerle I, Müller MA, Kallies S, Gotthardt DN, Drosten C. In-vitro renal epithelial cell infection reveals a viral kidney tropism as a potential mechanism for acute renal failure during Middle East Respiratory Syndrome (MERS) Coronavirus infection. Virol J. 2013;10:359. doi: 10.1186/1743-422X-10-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Puelles VG, Lütgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, Chilla S, Heinemann A, Wanner N, Liu S, et al. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. 2020. 10.1056/NEJMc2011400. [DOI] [PMC free article] [PubMed]
- 28.Singer M. The role of mitochondrial dysfunction in sepsis-induced multi-organ failure. Virulence. 2014;5(1):66–72. doi: 10.4161/viru.26907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ronco C, Reis T, Husain-Syed F. Management of acute kidney injury in patients with COVID-19. Lancet Respir Med. 2020;8(7):738–42. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.