Abstract
Background
Total joint arthoplasty (TJA) cost containment has been a key focus for the Centers for Medicare and Medicaid Services spawning significant research and programmatic change, including a move toward early discharge and outpatient TJA. TJA outpatients receive few, if any, medical interventions before discharge, but the type and quantity of interventions provided for TJA patients who stay overnight in the hospital is unknown. This study quantified the nature, frequency, and outcome of interventions occurring overnight after primary TJA.
Methods
1725 consecutive primary unilateral TJAs performed between 2012 and 2017 by a single surgeon in a rapid-discharge program, managed by a perioperative internal medicine specialist, were reviewed. Medical records were examined for diagnostic tests, treatments, and procedures, results of interventions, and readmissions.
Results
759 patients were discharged on postoperative day 1. Eighty-four percent (641 of 759) received no medical interventions during their overnight hospital stay. Twelve (1.6%) received diagnostic tests, 90 (11.9%) received treatments, and 29 (3.8%) received procedures. Ninety-two percent (11 of 12) of diagnostic tests were negative, 66% of 100 treatments in 90 patients were intravenous fluids for oliguria or hypotension, and all procedures were in and out catheterizations for urinary retention. 90-day all-cause readmission rates were similar in patients who received (2.5%) and did not receive (3.3%) a clinical intervention.
Conclusion
Most patients received no overnight interventions, suggesting unnecessary costly hospitalization. The most common issues addressed were oliguria, urinary retention, and hypotension. Protocols to prevent these conditions would facilitate outpatient TJA, improve patient safety, and reduce costs.
Keywords: total joint arthroplasty, cost, outpatient, complications, interventions
Since its original description, the primary goals of total joint arthroplasty (TJA) have remained consistent: to safely perform a durable reconstruction that reduces pain, restores function, and improves quality of life [1]. Refinements in surgical technique, pain management, blood conservation, and rehabilitation have resulted in quicker recovery [[2], [3], [4]], providing a foundation for early discharge after TJA. These developments have become part of Centers for Medicare and Medicaid Services efforts to contain costs while maintaining the safety and quality of TJA. Evidence has demonstrated early discharge TJA to be safe [[5], [6], [7], [8], [9], [10], [11], [12]] and cost saving [13,14], without increasing readmission rates [[15], [16], [17]]. In fact, the paradigm has shifted, and in the modern context, prolonged inpatient lengths of stay have been associated with higher unplanned 90-day readmission rates [18]. However, discharge on the same day of surgery has been criticized as potentially hazardous, with surgeons advocating an overnight stay to observe patients for life-threatening complications and those that will trigger a readmission [[19], [20], [21]].
A goal for better health care is to reduce unnecessary care, waste, and harm to patients by improving clinical practices and deterring patients and providers from the belief that more is better [22,23]. Prior efforts to decrease expenditure by eliminating unnecessary health care modalities have proven to be effective in a variety of settings [24,25]. Whether TJA patients discharged on postoperative day 1 (POD 1) receive beneficial medical interventions the night of surgery, necessitating their stay in the hospital, remains unknown. The purpose of this study was to determine what interventions patients discharged the day after surgery receive overnight in the hospital after TJA, and if these interventions warrant inpatient level care for all patients. Our primary aim was to quantify the nature, frequency, and outcome of diagnostic tests, treatments, and procedures among patients staying one night in the hospital. A secondary aim was to compare 90-day readmission rates between patients discharged on POD 1 who received an overnight intervention to those who did not receive an intervention. We hypothesized that there would be no difference in 90-day readmissions between patients discharged on POD 1 who underwent an overnight intervention (diagnostic test, treatment, and/or procedure) and patients who underwent no intervention.
Methods
Study Sample
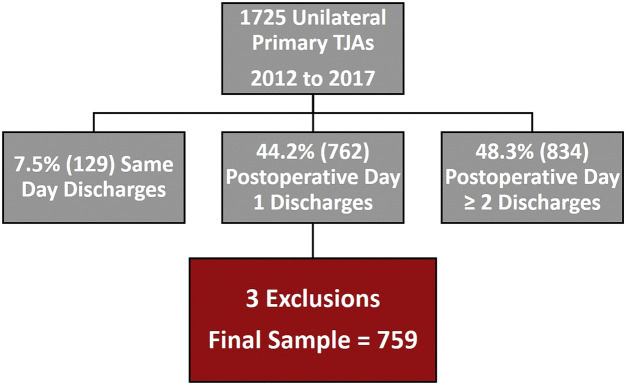
We identified 1725 primary unilateral TJAs consecutively performed during a 5-year period from 2012 to 2017 with institutional review board approval. All cases were performed by a single and high-volume surgeon at a tertiary care referral center. Seven hundred sixty-two (44%) of the cases discharged from the hospital on POD 1 formed the study sample (Fig. 1 ). Three patients were excluded from analysis. For 2 of these patients, interventions were for chest X-rays before Medicare approved discharge to extended care facilities on POD 1. One patient expired on POD 1 after acute onset of chest pain on awakening from total hip arthroplasty (THA) in the recovery room. The patient underwent electrocardiogram positive for acute myocardial infarction followed by cardiac catheterization with percutaneous coronary intervention for coronary artery blockage. Unfortunately, the patient suffered an acute occlusion of their drug-eluting stent the next morning and expired despite repeated cardiac catheterization. This patient was excluded because there is no way to know when he would have been discharged absent this unexpected event.
Fig. 1.
Flow diagram of patient population during study period showing patients included and excluded from study. TJAs, total joint arthroplasties.
Patient Care Protocols
As part of our standardized perioperative care program, all patients underwent preoperative risk assessment and medical clearance and optimization within 4 weeks of surgery by a perioperative internal medical specialist whose practice focuses exclusively on hip and knee arthroplasty patients. Each patient's surgery was discussed at a coordinated care conference attended by key members of the multidisciplinary team the week before their scheduled surgery. The goal of the meeting is to share information across disciplines and proactively develop patient care plans, shared with everyone who provides direct care or services to the patient. Preoperatively, patients and family members received comprehensive clinic-based joint replacement education and attended a hospital-based joint replacement class. Postoperatively, all patients were encouraged to ambulate by the afternoon on the day of surgery and received the same standardized rehabilitation protocol. Postoperative care was assumed by the operative surgeon, internal medicine specialist, clinic staff, and a multidisciplinary inpatient care team. The same modern perioperative pain control, clinical, and rehabilitation protocols were used for all patients.
Perioperative and Postoperative Pain Control and Anesthesia Protocols
A standardized multimodal preoperative pain protocol was used in all cases. Unless allergic or contraindicated, patients were given acetaminophen (1000 mg orally) 24 hours before surgery and oxycodone (10-20 mg orally), celecoxib (200 mg orally), and pregabalin (75 mg orally) immediately before surgery. Intraoperatively, surgeries were performed with standardized light general anesthesia (desflurane or sevoflurane) and a low-dose intrathecal, single-shot spinal injection of either 0.40 mg of morphine with a median of 10.5 mg of bupivacaine local anesthetic or 25 mcg of fentanyl with a median of 7.5 mg of bupivacaine. Beginning January 1, 2015, the spinal anesthesia medication cocktail was changed from morphine to fentanyl. Between September 01, 2012 and May 31, 2016, patients were instructed not to consume liquids after 12 AM on the day of surgery. Beginning June 1, 2016, patients were allowed to drink liquids up to 2 hours before surgery. Patient-specific and goal-directed fluid therapy involved preoperative, intraoperative, and postoperative administration of approximately 2000 mL total of crystalloid sodium lactate unless patients had significant renal diseases in which case normal saline was used. Postoperatively, patient's ability to void was observed. In and out catheterization was performed in patients who failed to spontaneously urinate after 8 hours from the time of their preoperative void. In addition, if the patient is able to urinate within those 8 hours but makes less than 300 cc of urine on their own, we perform an in and out catheterization and restart the clock. Patients who are unsuccessful in spontaneously voiding after 3 catheterizations get a consultation with urology and are taught either self-catheterization or have a Foley docked to be managed by urology.
In knees only, a periarticular injection of 0.2% (200 mg) of ropivacaine, 0.5 mg of epinephrine, 80 mcg of clonidine, and 30 mcg of ketorolac (removed for patients with renal insufficiency) equal to 101.3 mL of total volume was used immediately after final implant fixation. Postoperatively, unless allergic or contraindicated, patients received acetaminophen (1000 mg orally thrice a day), oxycontin (10-20 mg orally every 12 hours), celecoxib (200 mg orally twice a day), oxycodone (5-10 mg hourly as needed for mild pain and 10-20 mg hourly as needed for moderate pain), or hydromorphone (0.5 mg intravenously every 20 minutes as needed for severe pain).
Surgical Procedures
For all total knee arthroplasties (TKAs), a medial parapatellar approach was used. Standard coronal plane femoral bone cuts were made with computer-aided navigation (Stryker Navigation, Kalamazoo, MI), and tibial cuts performed with an extramedullary alignment. Before closure, a medium Hemovac (Zimmer Biomet, Warsaw, IN) drain was placed in all knees. The posterolateral approach was used in all hip surgeries with the patient in a lateral decubitus position. Acetabular and femoral components were implanted with consistent surgical technique, and a postoperative drain was not used.
Rapid Recovery Protocols
As the joint replacement program care coordination and experience evolved and matured, the expectations for early discharge subsequently progressed. Between 2011 and 2013, patients were educated with the expectation of being discharged to home no later than POD 2 if medically appropriate per the perioperative medicine specialist and physically safe per the physical therapist. During that time, however, patients were allowed to discharge the morning after surgery, if so motivated. Beginning in 2014, patients were routinely informed to anticipate discharge home the morning after surgery. In 2015, appropriate patients (as identified by the Outpatient Arthroplasty Risk Assessment [OARA] score) were offered outpatient surgery with same-day discharge in the ambulatory surgery center or the hospital [26].
Data Collection
Data for this study were prospectively recorded in and retrieved from the electronic medical record (EMR) and verified for accuracy. A retrospective review of the EMR was completed for each patient. Demographic data, including patient age in years, sex, body mass index (BMI) in kg/m2, American Society of Anesthesiologists Physical Status classification (ASA-PS; 1, 2, 3, or 4), and type of procedure (THA or TKA), were recorded. All-cause inpatient readmissions within 90 days of discharge were recorded for each patient. Medical records were sorted by type, and the laboratory/blood bank, radiology reports, and diagnostic tests/treatments/procedures sections were searched for records dated either the day of or the day after patients' surgeries. Internal medicine staff progress notes were reviewed for additional test results, treatments, and overall status of the patient. The results review section of the EMR was also evaluated for data on additional tests and results. For each intervention, the date, time, results, and cause for the intervention were recorded. The study outcome variables were medical interventions, separated into 3 categories: diagnostic tests, treatments, and procedures. Interventions used to look for pathology in a patient were defined as diagnostic tests, including cardiac enzymes, electrocardiograms, ultrasounds, urinalysis, and X-rays. Treatments were all interventions administered orally or intravenously to improve a patients' condition. Procedures were defined as invasive interventions, such as cardiac or urinary catheterization. We recorded all medical interventions that varied from the preoperative treatment plan, were beyond standard-of-care or routine interventions, and that patients could not complete at home. Therefore, routine basic metabolic panels, hemoglobin and iron levels, blood sugar control, over-the-counter treatments, and patient comfort measures were not recorded. If an intervention was performed before 4 PM on the day of surgery, we did not include it in our counts because the same intervention (eg, in and out catheterization) could have been performed for same-day discharge patients. This permitted us to more accurately answer the question—what beneficial medical interventions are provided for TJA patients who stay overnight in the hospital?
Medical interventions were reviewed by the perioperative internal medicine specialist to confirm medical necessity and inclusion in the study.
Data Analysis
Minitab 19 (Minitab Inc, State College, PA) was used for data analysis. The number of patients receiving each type of diagnostic test, treatment, and/or procedure is reported along with the symptoms prompting each intervention and the results of each intervention. Continuous data are reported as means and standard deviations, and categorical data are reported as numbers and proportions. The proportions of hospital readmissions within 90 days of discharge in patients who underwent an overnight intervention and those who did are presented. Post hoc calculation of statistical power using alpha 0.05 was too low to present the results of statistical tests.
Results
The final analysis sample of 759 cases was predominantly comprised of female (453; 59.7%) and TKA (459; 61%) patients (Table 1 ). Average age and BMI were 62.9 (±10.8) years and 32.7 (±6.8) kg/m2, respectively. Most patients (58.9%) had an ASA-PS classification of 3 or 4. All patients were discharged home with either outpatient or in-home physical therapy.
Table 1.
Demographic Characteristics Overall and by Intervention Type.
| Characteristic | Overall | Diagnostic Tests |
Treatments |
Procedures |
|||
|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | ||
| Sex | |||||||
| % Female | 59.7 | 96.7 | 1.3 | 13.7 | 86.3 | 2.4 | 97.6 |
| % Male | 40.3 | 98.0 | 2.0 | 9.2 | 90.8 | 5.9 | 94.1 |
| Mean (SD) age (y) | 62.9 (10.8) | 67.1 (5.7) | 62.8 (10.8) | 64.6 (8.0) | 62.7 (11.1) | 62.6 (6.9) | 62.9 (10.9) |
| Mean (SD) BMI (kg/m2) | 32.7 (6.8) | 32.5 (6.2) | 32.7 (6.8) | 33.4 (7.0) | 32.6 (6.8) | 32.3 (6.3) | 32.7 (6.8) |
| ASA-PS classification | |||||||
| 1 or 2 | 41.1 | 2.3 | 97.7 | 9.7 | 90.3 | 3.3 | 96.7 |
| 3 or 4 | 58.9 | 1.1 | 98.9 | 13.4 | 86.6 | 4.3 | 95.7 |
| Procedure | |||||||
| THA | 39.0 | 2.0 | 98.0 | 13.8 | 86.2 | 6.4 | 93.6 |
| TKA | 61.0 | 1.3 | 98.7 | 10.6 | 89.4 | 2.2 | 97.8 |
ASA-PS: 1 = normal healthy patients, 2 = patients with mild systemic disease, 3 = patients with severe systemic disease, and 4 = patients with a severe systemic disease that is a constant threat to life.
SD, standard deviation; BMI, body mass index; ASA-PS, American Society of Anesthesiology Physical Status Classification; THA, total hip arthroplasty; TKA, total knee arthroplasty.
Fifteen percent (119 of 759) of TJA patients discharged on POD 1 experienced 1 or more overnight medical interventions. Table 2 shows the number of patients who received diagnostic tests, treatments, and procedures, as well as the total number of interventions collectively received. The average number of interventions per patient was 0.20 ± 0.50 (range, 0-3).
Table 2.
Types of Medical Interventions Performed With Patients Discharged on POD 1 (N = 759).
| Intervention | Number of Patients (%) | Number of Interventions |
|---|---|---|
| Diagnostic tests | 12 (1.6) | 12 |
| Treatments | 90 (11.9) | 100 |
| Procedures | 30 (3.8) | 31 |
POD, postoperative day.
Thirteen patients (13 of 759; 1.7%) underwent 13 diagnostic tests (Table 3 ), all of which were negative with none of these patients readmitted to the hospital within 90 days. Table 1 presents the proportion of patients who received and did not receive diagnostic tests based on sex, age, BMI, ASA-PS classification, and procedure type.
Table 3.
Diagnostic Tests Ordered for Patients Discharged on POD 1.
| Diagnostic Test | Number of Patients | Symptoms | Test Result | 90-Day All-Cause Readmissions |
|---|---|---|---|---|
| Bladder ultrasound | 4 | Urinary retention | Negative | None |
| EKG | 3 | Chronic intermittent noncardiac chest pain | Negative | None |
| Angina | Negative and positive | None | ||
| Urinalysis | 2 | Acute hyponatremia on BMP | Positive | None |
| Asymptomatic (low sodium noted on BMP) | Negative | None | ||
| X-ray abdomen KUB | 2 | Abdominal distension | Negative | None |
| RUE venous Doppler ultrasound | 1 | RUE pain and swelling | Negative | None |
| Hand X-ray | 1 | Hand pain after fall | Negative | None |
EKG, electrocardiogram; BMP, basic metabolic panel; KUB, kidneys, ureters, bladder; RUE, right upper extremity.
Most (66 of 100; 66%) of 100 treatments in 90 patients were intravenous (IV) fluids for oliguria or hypotension (Table 4 ). Two patients who underwent a treatment (both IV fluids for oliguria) were readmitted to the hospital within 90 days, 1 for a gastrointestinal bleed and 1 for acute kidney injury and acute hypercapnic respiratory failure. Table 1 shows the prevalence of treatments based on demographic characteristics.
Table 4.
Treatments Ordered for Patients Discharged on POD 1.
| Treatment | Number of Patients | Symptoms | 90-Day All-Cause Readmissions |
|---|---|---|---|
| Anti-opioid | 1 | Oversedation | None |
| Cholinergic agonist and α-1 blocker | 10 | Urinary retention | None |
| Electrolyte supplementation | 7 | Hypokalemia | None |
| Fiorinal | 1 | Migraine headache | None |
| IV fluids | 54 | Oliguria | 1 GI bleed; 1 AKI and acute hypercapnic respiratory failure |
| IV fluids | 12 | Hypotension | None |
| IV fluids | 1 | Chronic kidney disease | None |
| IV fluids | 1 | Acute hyponatremia | None |
| IV fluids | 1 | Near syncope | None |
| IV iron | 5 | Iron deficiency | None |
| Loop diuretic | 4 | Oliguria | None |
| Loop diuretic | 2 | Acute hyponatremia | None |
| Loop diuretic | 1 | Chronic hyponatremia/SIADH | None |
POD, postoperative day; IV, intravenous; GI, gastrointestinal; AKI, acute kidney injury; SIADH, syndrome of inappropriate antidiuretic hormone secretion.
Thirty patients (30 of 759; 3.9%) underwent 31 procedures before discharge on POD 1. Twenty-nine of the procedures were in and out catheterizations for urinary retention. As shown in Table 1, procedures were more common in male patients than female patients and in patients undergoing THA.
One patient who received an in and out catheterization was readmitted within 90 days for treatment of a periprosthetic joint infection.
Examination of all-cause readmissions indicated that equivalent proportions of patients who received an intervention before discharge on POD 1 (2.5%) and those who did not (3.3%) were readmitted to the hospital within 90 days.
Discussion
In the United States, it has been estimated that $158-$226 billion of annual health care expenses are unnecessary and the result of overtreatment [27]. Overtreatment occurs when patients are subjected to care that is rooted in outdated habits and which sound science does not support. The exponentially increased demand for TJA [28] has imposed an enormous economic burden on the health care system, accounting for more Medicare expense than any other inpatient procedure [29]. Not surprisingly, cost containment has become a primary focus of policy and research on TJA. Multiple strategies have been adopted to improve the value of TJA, but like the overall health care system, the savings potentially achievable from a reduction in wasteful spending may be more significant than from direct cuts in care or coverage. As part of the effort to reduce cost, hospital lengths of stay have decreased after primary TJA [13]. However, there is disagreement regarding the optimal inpatient length of stay. Some surgeons cite early discharge TJA as safe [[5], [6], [7], [8], [9], [10], [11]] and without increased readmission rates [[15], [16], [17]], whereas others criticize early discharge TJA as risky, claiming inpatient stays allow for the recognition of life-threatening complications and those complications that prompt readmission [[19], [20], [21]]. With the removal of TKA from the inpatient-only list, hospitals and payers must now consider all Medicare TKA patients as potential outpatients [30]. Furthermore, with the current coronavirus pandemic of 2020, patients must minimize their time in the inpatient setting where more medically ill patients and transmittable contagious diseases exist. Therefore, understanding the true value and necessity of an overnight in-hospital stay is critical. This study sought to answer the question of whether there is a benefit for early discharge patients to stay in the hospital overnight? The results of this study describe the small number and consistent nature of hospital interventions among patients discharged on POD 1 after primary TJA and demonstrate that there is no difference in readmission rates between those patients who experienced an intervention and those who did not. The findings indicate that better identification of patients requiring an overnight stay, as well as prevention methods for urinary retention, oliguria, and hyponatremia, is required to further enhance patient safety via elimination of unnecessary and costly hospital stays.
We observed that only 1.6% of patients discharged on POD 1 after primary TJA underwent a diagnostic test beyond routine standard of care. This is a novel finding, as the number of patients receiving a postoperative test after primary TJA has not been described. All but 2 of the diagnostic tests were negative, suggesting that a further reduction in testing may be possible without compromising patient safety. Similarly, these results may be interpreted to mean that not every early discharge patient requires diagnostic testing after TJA, as has recently been emphasized by Richardson et al [31], who suggested that routine postoperative hemoglobin monitoring may be unnecessary. Future studies should seek to determine which patients require diagnostic tests and whether these tests are required to be performed in the inpatient setting or whether they can be safely conducted at home and reported to health care providers who can respond in instances of an abnormal result.
In the present study, 3.6% of patients discharged on POD 1 after primary TJA required a procedure, and all the procedures were in and out catheterizations for postoperative urinary retention (POUR). Future research should determine whether this procedure can be taught to patients and/or their caregivers to be performed safely at home. Coupled with the knowledge of which patients are at high risk and the recent report suggesting that avoiding certain anesthetic agents reduces the incidence of POUR [32], the elimination of catheterizations could lower the incidence of in-hospital procedures to nearly 0.
This study found that a total of 84 patients required a postoperative treatment before discharge on POD 1. Sixty-eight percent of postoperative treatments were IV fluids for hypotension, oliguria, or as part of a urinary retention treatment plan. Many early discharge protocols focus on keeping patients hydrated preoperatively, intraoperatively, and postoperatively [3,16]. The results of the present study were used by our multidisciplinary team to reassess our perioperative hydration protocols, and future research should be conducted on the ideal fluid optimization. In addition, as previously suggested, research may be conducted to evaluate the necessity of receiving these treatments as an inpatient and to explore the feasibility of doing them at home under the direct or indirect supervision of a health care provider.
Perhaps the most notable finding of this study was that 84% of patients discharged on POD 1 did not require any intervention before discharge, suggesting that these patients did not receive any benefit from an overnight stay and endured an unnecessary hospital stay. Our all-cause readmission rates were low and similar to those previously reported in the literature [17]. Our finding that there was no significant difference in the readmission rates between patients requiring an intervention and those not requiring an intervention suggests that same-day discharge may be safe and unlikely to result in increased complications for many patients. Eliminating unnecessary overnight stays in the hospital for appropriate patients would reduce the cost of care by up to $1625-$2025 [15] without increasing the risk, thereby improving the value of TJA.
This descriptive study is not without limitations, including its retrospective cohort design. Despite inherent bias of this study design, all data were prospectively collected on consecutive cases performed by a single surgeon with consistent protocols, which may reduce selection and interpretation biases. It should be noted that this study was not designed to evaluate interventions received by unhealthy patients requiring prolonged inpatient care but instead relatively healthier patients discharged on POD 1. Some patients in the cohort were eligible for but declined same-day discharge. Thus, findings may add to the utility of the OARA score in safely identifying and educating patients eligible for outpatient TJA [26]. Future studies may seek to determine whether a predictive model, or even the OARA score, is capable of determining which same-day discharge eligible patients require an intervention overnight. In addition, it has been suggested that pain, muscle weakness, and dizziness are the main reasons why patients stay in the hospital longer than expected [33]. It is unknown if patients in this study felt they required an inpatient stay because of pain, weakness, or dizziness. Therefore, it is possible that some of the patients receiving no medical interventions might not have been ready to leave the hospital on the day of surgery. In addition, it is possible that patients requiring readmission did so at another institution, in which case the readmission rates may be underreported.
In conclusion, the results of this study demonstrate that most patients discharged on POD 1 after primary TJA did not require any medical interventions. In addition, there was no difference in readmission rates between the patients who required an intervention and those who did not. These data suggest that overnight hospitalization after TJA may be unnecessary for more patients than are currently identified. Adequate hydration and avoidance of POUR seem to be the greatest targets of perioperative optimization and should be the focus of additional research. The goals of transitioning to outpatient TJA include improving the patient experience and reducing per capita cost of health care, and the results of this study suggest that eliminating the overnight stay in a large percentage of TJA patients may help achieve these goals.
Ethical Board Review
This study received institutional review board approval before initiation. The study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. This study was carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act.
Acknowledgment
The project described was supported by the Indiana University Health–Indiana School of Medicine Strategic Research Initiative.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.arth.2020.07.021.
Appendix A. Supplementary Data
References
- 1.Charnley J. Arthroplasty of the hip: a new operation. Lancet. 1961;277:1129–1132. doi: 10.1016/S0140-6736(61)92063-3. [DOI] [PubMed] [Google Scholar]
- 2.Argenson J.-N.A., Husted H., Lombardi A., Booth R.E., Thienpont E. Global forum: an international perspective on outpatient surgical procedures for adult hip and knee reconstruction. J Bone Joint Surg Am. 2016;98:e55. doi: 10.2106/JBJS.15.00998. [DOI] [PubMed] [Google Scholar]
- 3.Berend M.E., Lackey W.G., Carter J.L. Outpatient-focused joint arthroplasty is the future: the Midwest center for joint replacement experience. J Arthroplasty. 2018;33:1647–1648. doi: 10.1016/j.arth.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Dorr L.D., Thomas D.J., Zhu J., Dastane M., Chao L., Long W.T. Outpatient total hip arthroplasty. J Arthroplasty. 2010;25:501–506. doi: 10.1016/j.arth.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 5.Berger R.A., Jacobs J.J., Meneghini R.M., Della Valle C., Paprosky W., Rosenberg A.G. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 6.Berger R.A., Sanders S., Gerlinger T., Della Valle C., Jacobs J.J., Rosenberg A.G. Outpatient total knee arthroplasty with a minimally invasive technique. J Arthroplasty. 2005;20:33–38. doi: 10.1016/j.arth.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 7.Berger R.A., Sanders S.A., Thill E.S., Sporer S.M., Della Valle C. Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients. Clin Orthop Relat Res. 2009;467:1424–1430. doi: 10.1007/s11999-009-0741-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parcells B.W., Giacobbe D., Macknet D., Smith A., Schottenfeld M., Harwood D.A. Total joint arthroplasty in a stand-alone ambulatory surgical center: short-term outcomes. Orthopedics. 2016;39:223–228. doi: 10.3928/01477447-20160419-06. [DOI] [PubMed] [Google Scholar]
- 9.Kolisek F.R., McGrath M.S., Jessup N.M., Monesmith E.A., Mont M.A. Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res. 2009;467:1438–1442. doi: 10.1007/s11999-009-0730-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shah R.R., Cipparrone N.E., Gordon A.C., Raab D.J., Bresch J.R., Shah N.A. Is it safe? Outpatient total joint arthroplasty with discharge to home at a freestanding ambulatory surgical center. Arthroplast Today. 2018;4:484–487. doi: 10.1016/j.artd.2018.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoeffel D.P., Daly P.J., Kelly B.J., Giveans M.R. Outcomes of the first 1,000 total hip and total knee arthroplasties at a same-day surgery center using a rapid-recovery protocol. JAAOS Glob Res Rev. 2019;3:e022. doi: 10.5435/JAAOSGlobal-D-19-00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiser M.C., Kim K.Y., Anoushiravani A.A., Iorio R., Davidovitch R.I. Outpatient total hip arthroplasty has minimal short-term complications with the use of institutional protocols. J Arthroplasty. 2018;33:3502–3507. doi: 10.1016/j.arth.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Molloy I.B., Martin B.I., Moschetti W.E., Jevsevar D.S. Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg. 2017;99:402–407. doi: 10.2106/JBJS.16.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aynardi M., Post Z., Ong A., Orozco F., Sukin D.C. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J. 2014;10:252–255. doi: 10.1007/s11420-014-9401-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sutton J.C., Antoniou J., Epure L.M., Huk O.L., Zukor D.J., Bergeron S.G. Hospital discharge within 2 days following total hip or knee arthroplasty does not increase major complication and readmission rates. J Bone Joint Surg. 2016;98:1419–1428. doi: 10.2106/JBJS.15.01109. [DOI] [PubMed] [Google Scholar]
- 16.Stambough J.B., Nunley R.M., Curry M.C., Steger-May K., Clohisy J.C. Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. J Arthroplasty. 2015;30:521–526. doi: 10.1016/j.arth.2015.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sibia U.S., Waite K.A., Callanan M.A., Park A.E., King P.J., MacDonald J.H. Do shorter lengths of stay increase readmissions after total joint replacements? Arthroplast Today. 2017;3:51–55. doi: 10.1016/j.artd.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams J., Kester B.S., Bosco J.A., Slover J.D., Iorio R., Schwarzkopf R. The association between hospital length of stay and 90-day readmission risk within a total joint arthroplasty bundled payment initiative. J Arthroplasty. 2017;32:714–718. doi: 10.1016/j.arth.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Pulido L., Parvizi J., Macgibeny M., Sharkey P.F., Purtill J.J., Rothman R.H. In Hospital complications after total joint arthroplasty. J Arthroplasty. 2008;23:139–145. doi: 10.1016/j.arth.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 20.Parvizi J., Mui A., Purtill J.J., Sharkey P.F., Hozack W.J., Rothman R.H. Total joint arthroplasty. J Bone Joint Surg. 2007;89:27–32. doi: 10.2106/JBJS.E.01443. [DOI] [PubMed] [Google Scholar]
- 21.Courtney P.M., Boniello A.J., Berger R.A. Complications following outpatient total joint arthroplasty: an analysis of a national database. J Arthroplasty. 2017;32:1426–1430. doi: 10.1016/j.arth.2016.11.055. [DOI] [PubMed] [Google Scholar]
- 22.Levinson W., Kallewaard M., Bhatia R.S., Wolfson D., Shortt S., Kerr E.A. ‘Choosing Wisely’: a growing international campaign. BMJ Qual Saf. 2015;24:167–174. doi: 10.1136/bmjqs-2014-003821. [DOI] [PubMed] [Google Scholar]
- 23.Cassel C.K., Guest J.A. Choosing wisely. JAMA. 2012;307:1801. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 24.Bindraban R.S., van Beneden M.L., Kramer M.H., van Solinge W.W., Neppelenbroek S.I., van Wijnen M. A multicenter before-after study on reducing unnecessary diagnostics by changing the attitude of caregivers: protocol for the RODEO project. JMIR Res Protoc. 2018;7:e10473. doi: 10.2196/10473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vegting I.L., van Beneden M., Kramer M.H.H., Thijs A., Kostense P.J., Nanayakkara P.W.B. How to save costs by reducing unnecessary testing: lean thinking in clinical practice. Eur J Intern Med. 2012;23:70–75. doi: 10.1016/j.ejim.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Ziemba-Davis M., Caccavallo P., Meneghini R.M. Outpatient joint arthroplasty—patient selection: update on the outpatient Arthroplasty Risk Assessment Score. J Arthroplasty. 2019;34:S40–S43. doi: 10.1016/j.arth.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 27.Hackbarth A.D., Hackbarth A.D. Eliminating waste in US health care. JAMA. 2012;307:1513. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 28.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am Vol. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 29.Hawker G.A., Badley E.M., Croxford R., Coyte P.C., Glazier R.H., Guan J. A population-based nested case-control study of the costs of hip and knee replacement surgery. Med Care. 2009;47:732–741. doi: 10.1097/MLR.0b013e3181934553. [DOI] [PubMed] [Google Scholar]
- 30.Yates A.J., Kerr J.M., Froimson M.I., Della Valle C.J., Huddleston J.I. The unintended impact of the removal of total knee arthroplasty from the Center for Medicare and Medicaid Services inpatient-only list. J Arthroplasty. 2018;33:3602–3606. doi: 10.1016/j.arth.2018.09.043. [DOI] [PubMed] [Google Scholar]
- 31.Richardson S., Chiu Y.F., Blevins J.L., Romero J.A., Buller L.T. Presented at the American Academy of Hip and Knee Surgeons; Dallas, TX: 2019. Routine postoperative hemoglobin monitoring of benefit in patients undergoing total hip and knee arthroplasty? [Google Scholar]
- 32.Ziemba-Davis M., Nielson M., Kraus K., Duncan N., Nayyar N., Meneghini R.M. Identifiable risk factors to minimize postoperative urinary retention in modern outpatient rapid recovery total joint arthroplasty. J Arthroplasty. 2019;34:S343–S347. doi: 10.1016/j.arth.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 33.Husted H., Lunn T.H., Troelsen A., Gaarn-Larsen L., Kristensen B.B., Kehlet H. Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthop. 2011;82:679–684. doi: 10.3109/17453674.2011.636682. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.