Abstract
Introduction: Cardiac complications of COVID-19 are potentially life-threatening. The occurrence of myocardial injury in the context of COVID-19 is multifactorial and has generated increasing interest. Methods: A systematic review with a meta-analysis of the literature was performed. MEDLINE and EMBASE were searched. Two independent reviewers evaluated the selected manuscripts for the outcome “myocardial injury”, defined by troponin elevation above the 99th percentile. The study heterogeneity and risk of bias were evaluated. Results: Eight studies, with a total of 1,229 patients, were included. The frequency of myocardial injury was 16% (95% CI: 9%-27%). The heterogeneity among the studies was high (93%). Conclusions: Myocardial injury may occur in patients with COVID-19, with a frequency of 16% according to current studies. Continuous research is needed to update these findings as the pandemic evolves and to define the implications of myocardial injury in the context of this infection.
Keywords: COVID-19, myocardial injury, acute myocardial infarction, myocarditis, troponin
Introduction
The association between cardiovascular disease (CVD) and adverse outcomes in patients with COVID-19 has been consistently described. In the case series by Ruan et al, among 68 patients who died, 19% had CVD, versus none among those who survived (P<0.001) [1]. However, there is also evidence of acute cardiac damage in the context of the infection. Recently, the first proven case of direct cardiac damage was published, with a demonstration of viral particles inside the myocardium of a patient with COVID-19 and cardiogenic shock who underwent endomyocardial biopsy [2].
Troponin elevations, suggesting myocardial damage, are frequent in severe infections [3]. Abnormal troponin values have been frequently found in patients with COVID-19, especially when high-sensitivity troponin is used. Among the first 41 COVID-19 patients in China, 5 (12%) had acute myocardial injury (manifested by troponin elevations >99th percentile), and 4 of these patients required intensive care treatment [4], demonstrating the increased severity associated with this presentation. The aim of this study was to evaluate the frequency of acute myocardial injury in patients with COVID-19.
Methods
A systematic review of the literature was performed to evaluate the frequency of acute myocardial injury expressed by abnormal troponin levels (>99th percentile) in hospitalized patients with COVID-19.
Population
The study population included in-patients with confirmed COVID-19.
Exposure
Exposure was considered to be SARS-Cov-2 infection with clinical COVID-19.
Outcomes
The primary study outcome was abnormal troponin levels (>99th percentile), with or without clinical manifestations of acute cardiac injury.
Study types
The meta-analysis included case series or cohorts.
Sources of information
Two databases were searched: MEDLINE and Embase. Other manuscripts were manually added from reviews or other sources of data.
Search strategies
The search was performed until 04/02/2020. No language restrictions were applied. Search strategies were the following:
- MEDLINE: (myocarditis [MeSH Terms]) OR (myocarditis [Title/Abstract]) OR (carditis [Title/Abstract]) OR (myocardial infarction [MeSH Terms]) OR (“myocardial infarction” [Title/Abstract]) OR (“acute myocardial infarction” [Title/Abstract]) OR (“Infarction, Myocardial” [Title/Abstract]) OR (“Infarctions, Myocardial” [Title/Abstract]) OR (“Myocardial Infarctions” [Title/Abstract]) OR (“Myocardial Infarct” [Title/Abstract]) OR (“Infarct, Myocardial” [Title/Abstract]) OR (“Infarcts, Myocardial” [Title/Abstract]) OR (“Myocardial Infarcts” [Title/Abstract]) OR (“Heart Attack” [Title/Abstract]) OR (“Heart Attacks” [Title/Abstract]) AND (“SARS Virus” [mh] OR SARS [tiab] OR “severe acute respiratory syndrome coronavirus 2” [Supplementary Concept] OR “COVID-19” [Supplementary Concept] OR covid-19 [tiab] OR “sars-cov 2” [tiab] OR 2019 ncov [tiab] OR 2019-ncov [tiab])).
- EMBASE: ((troponin AND (“cardiovascular diseases” OR “doenças cardiovasculares”) AND (“covid-19” OR coronavirus OR “corona virus” OR “corona vírus”) myocarditis: ab,ti OR carditis: ab,ti OR ‘myocardial infarction’: ab,ti OR ‘acute myocardial infarction’: ab,ti OR ‘Infarction, Myocardial’: ab,ti OR ‘Infarctions, Myocardial’: ab,ti OR ‘Myocardial Infarctions’: ab,ti OR ‘Myocardial Infarct’: ab,ti OR ‘Infarct, Myocardial’: ab,ti OR ‘Infarcts, Myocardial’: ab,ti OR ‘Myocardial Infarcts’: ab,ti OR ‘Heart Attack’: ab,ti OR ‘Heart Attacks’: ab,ti AND (‘sars coronavirus’/exp OR ‘sars coronavirus’: ab,ti OR ‘sars’: ab,ti OR ‘severe acute respiratory syndrome coronavirus 2’: ab,ti OR ‘covid-19’: ab,ti OR ‘sars-cov 2’: ab,ti OR ‘2019ncov’: ab,ti OR ‘2019-ncov’:ab,ti).
Selection strategy
Manuscripts were selected according to title, abstract and full text and were analyzed by two independent reviewers. Discordances were resolved by a third reviewer. The quality of the studies was graded according to the Newcastle-Ottawa scale.
Statistical analysis
A meta-analysis of random effects was performed by the DerSimonian and Laird method, and the results are shown in forest plots. The measure of effect was the logit of the proportion of myocardial injury. The heterogeneity of studies was estimated by I2. In the presence of substantial (>50%) heterogeneity, a meta-regression was performed using clinical and demographic variables as determinants. The presence of bias was analyzed using a funnel plot and quantitatively by Egger’s test. The R software (r-project.org) version 3.6.3 was used for all analyses.
Results
The PRISMA flowchart is shown in Figure 1. After exclusion, eight manuscripts were considered eligible for the meta-analysis. The quality of the manuscripts was more frequently graded as fair (Supplementary Table 1).
Figure 1.
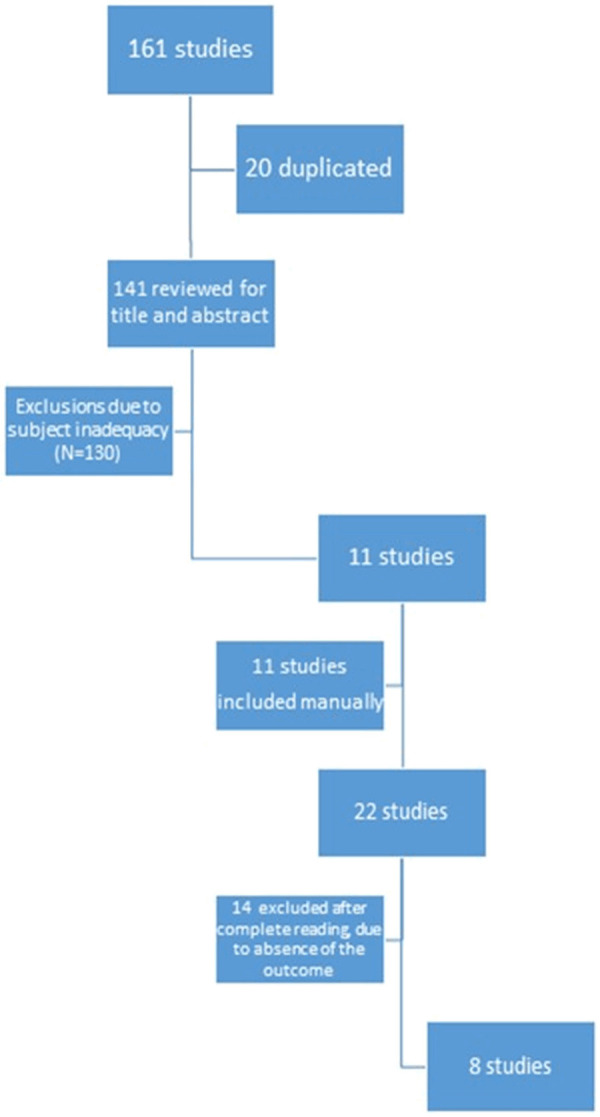
PRISMA flowchart.
Acute myocardial injury
Table 1 depicts some characteristics of the included studies and Table 2, the occurrence of cardiac injury in hospitalized COVID-19 patients. The frequencies of myocardial injury ranged from 3.3% to 44.4% [1,4-10]. Figure 2 shows the results of the meta-analysis. In the hospitalized patients with COVID-19, the frequency of myocardial injury was 16% (95% CI: 9%-27%). There was high heterogeneity among the studies (92%), so a meta-regression was performed (Table 2). Since age and the presence of chronic obstructive pulmonary disease (COPD) were found to be the sources of heterogeneity (Table 3), another meta-analysis was performed with stratification for these variables (Figure 3). The studies with outlier values (Ruan et al [1] and He et al [5]) were analyzed separately, resulting in different frequencies of myocardial injury, with 33% in the worst scenario; however, heterogeneity was still high (63% after stratification).
Table 1.
Summary of the basic characteristics of the studied literature
| Study (First author, publication year) | Population (location/number of patients) | Mean age (years) | Male gender (%) | Hypertension (%) | Diabetes (%) | COPD (%) |
|---|---|---|---|---|---|---|
| Huang et al, 2020 | China/41 | 49 | 73 | 15 | 20 | 2 |
| He et al, 2020 | China/54 | 68 | 63 | 44.4 | 14.8 | 3.7 |
| Wang et al, 2020 | China/138 | 56 | 54.3 | 31.2 | 10.1 | 2.9 |
| Zhou et al, 2020 | China/191 | 56 | 62 | 30 | 19 | 3 |
| Ruan et al, 2020 | China/150 | 50/67* | 53/49* | 23/29* | 13/12* | 1/3* |
| Yang et al, 2020 | China/52 | 59 | 67 | 17 | 8 | |
| Shi et al, 2020 | China/416 | 64 | 49.3 | 30.5 | 14.4 | 2.9 |
| Guo et al, 2020 | China/187 | 58 | 48.7 | 32.6 | 15 | 2.1 |
Discharged patients/patients who died.
Table 2.
Frequency of acute myocardial injury in patients with COVID-19
Figure 2.
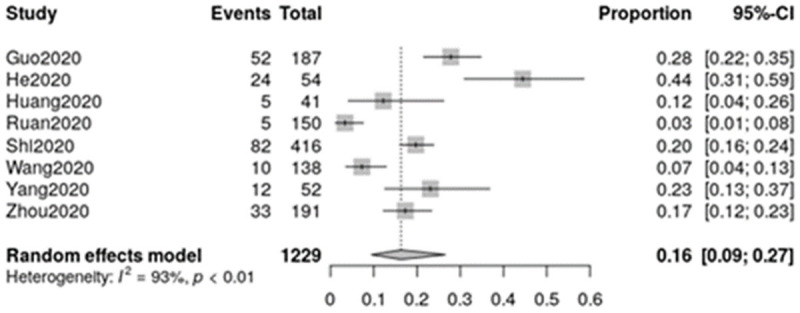
Meta-analysis of the frequency of myocardial injury.
Table 3.
Meta-regression for the analysis of heterogeneity among studies
| Coefficient | Explained heterogeneity | P value | |
|---|---|---|---|
| Age | 0,0889 | 2.35% | 0.029 |
| Male gender | -0.0007 | 0 | 0.98 |
| Hypertension | 0.0496 | 20.25% | 0.138 |
| Diabetes | -0.0556 | 5.43% | 0.238 |
| Prior cardiovascular disease | 0.0498 | 1.02% | 0.068 |
| Chronic obstructive pulmonary disease | 0.1048 | 30.66% | 0.016 |
Figure 3.
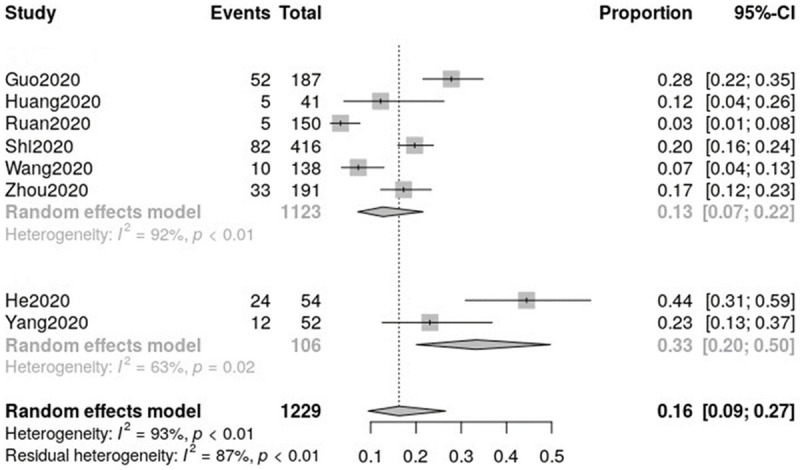
Stratified meta-analysis for the evaluation of heterogeneity.
Regarding the publication bias (Figure 4), although some asymmetry was observed on the funnel plot, there was no significant bias (P=0.3418).
Figure 4.
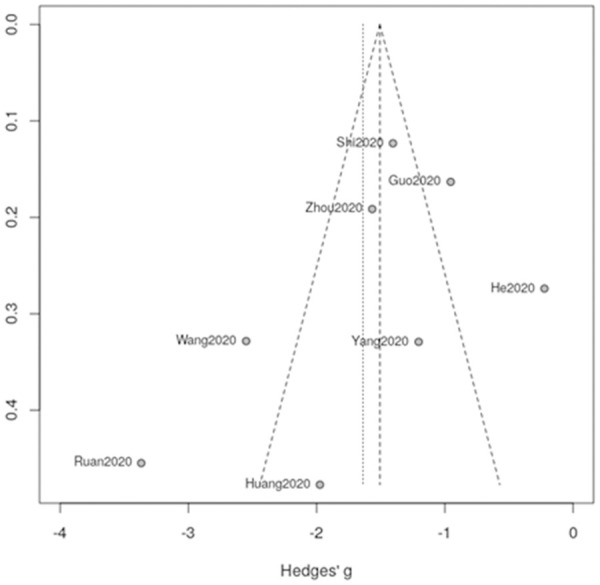
Funnel plot for the evaluation of publication bias.
Discussion
In the face of the COVID-19 pandemic-an unprecedented situation in modern medicine-it is of key importance to learn about the characteristics of the disease and related complications. Cardiac injury in COVID-19 is a main complication that should be accounted for in patients who clinically deteriorate and anticipated for in those patients with risk factors such as prior cardiovascular disease. Adequate comprehension of the frequency, predisposing factors and characteristics of cardiac injury in COVID-19 is therefore desirable.
The definition of acute cardiac injury is controversial, as most studies consider the elevation of troponin above the 99th percentile as the criterion for myocardial damage, without necessarily any association with clinical, electrocardiographic or imaging data. Additionally, the different sensitivities of tests and cutoff points for abnormalities may hamper the interpretation of the studies. Of note, the timing of the troponin measurements was different among the studies, and the patient severity was also variable. These may explain the different frequencies of myocardial injury between the studies; nonetheless, the overall frequency of 16% depicts an important issue, which should be underscored.
The mechanisms of myocardial injury in COVID-19 may include atherosclerotic plaque rupture (type I acute myocardial infarction), a supply/demand imbalance in the context of severe infection and sepsis (type II myocardial infarction), or direct myocardial damage, as demonstrated by Tavazzi et al [2], due to the presence of the pathophysiologic substrate (the ACE2 enzyme as the viral receptor) in cardiomyocytes [11]. All these factors may be precipitated or aggravated by systemic inflammation and the “cytokine storm” [1]. Abnormal troponin values, especially if high-sensitivity troponin is employed, have been frequently reported in patients with COVID-19 since the beginning of the pandemic. Among the first 41 Chinese patients with COVID-19, 5 (12%) had acute myocardial injury, and 4/5 needed intensive care support [4]. Clinical data are key to distinguishing the different disease entities, as shown in case reports; for example, Hu et al [12] described the case of a 37-year-old male admitted with chest pain and shortness of breath who was diagnosed with COVID-19 and displayed ST-segment elevation in inferior leads, troponin T>10,000 ng/L, BNP of 21,025 ng/L but had no coronary stenosis on the CT angiogram. An echocardiogram revealed severe left ventricular dysfunction, and the final diagnosis was fulminant myocarditis with cardiogenic shock. Therefore, it should be emphasized that abnormal troponin results may be multifactorial and should be interpreted carefully and in conjunction with other data due to the low specificity for the diagnosis of acute myocardial infarction. Nonetheless, as Chapman et al [13] suggested, troponin may also be viewed as relevant if emphasis is placed on its prognostic value (and not on the diagnosis of acute coronary artery disease) regarding the epidemiologic issue of recognizing the overall incidence of myocardial injury in COVID-19 patients. Accordingly, it must be underscored that abnormal troponin levels should be considered in the overall clinical context of the patient, not as an indication per se for procedures such as cardiac catheterization or for therapeutic measures such as the initiation of antiplatelet agents.
Finally, the current rate at which data and new publications are released makes it especially difficult to review the literature, which is evolving on a daily basis. However, a meta-analysis may be useful to provide an estimate of the frequency of COVID-19 adverse events, which in the case of myocardial injury constitutes a particularly dangerous complication that should be considered.
Conclusions
In the context of a severe infection, the implications of abnormal troponin measurements vary, and elevated troponin in COVID-19 may not necessarily imply the occurrence of acute myocardial infarction or myocarditis. Nonetheless, the present review shows that myocardial injury may occur in 16% of hospitalized patients with COVID-19, a frequency that is high enough to emphasize this complication in clinical care.
Acknowledgements
The authors thank Braulio Santos for discussing the results, Francijane Oliveira and Cyntia Aguiar for data search, and Marcelo Goulart for the support with the elaboration of figures.
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, Sepe PA, Resasco T, Camporotondo R, Bruno R, Baldanti F, Paolucci S, Pelenghi S, Iotti GA, Mojoli F, Arbustini E. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–915. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Musher DM, Abers MS, Corrales-Medina VF. Acute infection and myocardial infarction. N Engl J Med. 2019;380:171–176. doi: 10.1056/NEJMra1808137. [DOI] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.He XW, Lai JS, Cheng J, Wang MW, Liu YJ, Xiao ZC, Xu C, Li SS, Zeng HS. Impact of complicated myocardial injury on the clinical outcome of severe or critically ill COVID-19 patients. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:E011. doi: 10.3760/cma.j.cn112148-20200228-00137. [DOI] [PubMed] [Google Scholar]
- 6.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020:e200950. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020:e201017. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020:ehaa190. doi: 10.1093/eurheartj/ehaa190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chapman AR, Bularga A, Mills NL. High-sensitivity cardiac troponin can be an ally in the fight against COVID-19. Circulation. 2020;141:1733–1735. doi: 10.1161/CIRCULATIONAHA.120.047008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


