Abstract
Background: Clinical trials that evaluated long-term clinical outcomes of thrombus aspiration before primary percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) have shown different results. Thus, this study was designed to evaluate the long-term clinical outcomes and trends in present usage of thrombosuction in STEMI patients undergoing primary PCI. Methods: This was a single-center, retrospective study conducted at a tertiary-care center in India between January 2016 and December 2018. A total of 241 patients with STEMI who underwent primary PCI were differentiated into thrombus aspiration or standard primary PCI group. Primary endpoint was major adverse cardiac events (MACE) at 1-year. The other safety outcome measured at 1-year follow-up was stent thrombosis. Results: Among 241 patients, 119 patients were included in the thrombus aspiration group and 122 patients were included in the standard primary PCI group. All patients underwent 1-year follow-up. MACE rate was found to be 4.2% and 4.9% in thrombus aspiration and standard primary PCI group (P=0.79), respectively. Death from any cause was found to be higher in thrombus aspiration 7 (5.9%) compared to standard primary PCI group 5 (4.1%). Of which, cardiac death has occurred in 5 (4.2%) patients of thrombus aspiration group and 4 (3.3%) patients of standard primary PCI group (P=0.747). Definite stent thrombosis was observed in 1 (0.8%) patient of both the groups (P=1.00). Conclusion: The study concludes that there was no significant benefit of thrombus aspiration concerning mortality rate or any other clinical outcomes at 1-year in STEMI patients.
Keywords: Percutaneous coronary intervention, ST-segment elevation myocardial infarction, thrombus aspiration
Introduction
Despite the improvement in the management of ST-elevation myocardial infarction (STEMI), the death rate still remains constantly high [1,2]. Primary percutaneous coronary intervention (PCI) remains the cornerstone in the treatment by reducing the death rate; however, one of the most important challenges in the management of STEMI is the establishment of normal coronary blood flow after PCI [3,4]. The presence of large thrombus load at the site of lesion may provide an increased risk of distal embolization and microvascular occlusion even after stent implantation or balloon dilation which is known as a no-flow phenomenon [5,6]. This reduced flow is related to reperfusion injury which leads to arrhythmias, contractile dysfunction, microvascular impairment and irreversible myocardial damage [7]. Hence, intracoronary thrombectomy was designed as an adjunctive tool in the restoration of normal coronary blood flow in STEMI [8,9]. Several studies showed that thrombectomy devices can preserve microvascular function by preventing distal embolization in the microvasculature [10,11]. Still there are lacunae of knowledges on the application of these thrombectomy devices in STEMI patients [3,12]. The controversy of using routine thromboaspiration has intensified after the recent publication of TOTAL Trial. Thus, this study was designed to evaluate the long term clinical outcomes and trends in present usage of thrombosuction in STEMI patients undergoing primary PCI.
Methods
Study design and patient population
This was a single-center, retrospective study conducted at a tertiary-care center in India. The records of consecutive 241 patients with STEMI who underwent primary PCI between January 2016 and December 2018 were included in the study. Eligible patients were differentiated into thrombus aspiration or standard primary PCI group.
Inclusion criteria
All consecutive patients with STEMI who underwent primary PCI within the stipulated time period was included in this study.
Exclusion criteria
The patients who presented >24 hours after the onset of symptoms, age <18 years and who needed emergency coronary artery bypass grafting were excluded from this study.
Ethics
The study protocol was approved by the Ethics Committee of the respective authority of our institution. Written informed consent will be obtained from all patients, before inclusion in the study.
Study intervention
The primary PCI was performed according to standard techniques through the femoral or radial artery in the cardiac catheterization laboratory. Before the intervention, all patients were administered with dual antiplatelet drug such as aspirin 300 mg as a loading dose and other medications such as second antiplatelet and statins, respectively. All thrombus aspiration was performed at the discretion of the operator. Procedural characteristics like culprit vessel, number of diseased vessels, use of stents, and other medications were analyzed. At the time of discharge from the hospital, all patients has been prescribed with aspirin 70 mg with clopidogrel (75 mg) OD or prasugrel 10 mg or ticagrelor 90 mg BD.
Data collection
Patients’ demographics such as age, sex, history of diabetes, hypertension, smoking, hypercholesterolemia, PCI or coronary artery bypass graft (CABG) and family history of ischemic heart disease (IHD), presence of renal insufficiency, myocardial infarction, stroke, and unstable angina were collected. Procedural and lesion characteristics were obtained from the records and noted.
Clinical outcomes and follow-up
All patients were followed-up through outpatient visits or telephonic contact. The primary outcome measures were major adverse cardiovascular events (MACE) at 1-year. The MACE is defined as a composite of cardiac death, myocardial infarction and target vessel revascularization (TVR). In this study, MI is defined based on the development of new Q waves in two or more contiguous leads of the ECG and with or without elevated cardiac enzymes or followed by significant elevation of creatine kinase >3 times the upper limit of normal or without new Q waves in the ECG. Target vessel revascularization is defined as the re-intervention of any segment of the target vessel. The other safety outcome measured at a 1-year follow-up was stent thrombosis which is defined according to the academic research consortium definition of stent thrombosis [13].
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and categorical variables were expressed as frequencies and percentages. Continuous variables were compared using the Mann-Whitney U test and categorical variables were compared using the chi-square test or Fisher’s exact test. A p-value of <0.05 was considered statistically significant. The analysis was performed using statistical package for social sciences (SPSS) software (IBM SPSS, version 20.0. Armonk, 2012).
Results
Baseline characteristics
The total study population comprised of 241 patients, of whom, 119 patients were included in the thrombus group and 122 patients were included in the standard primary PCI group. The mean age of the study population was 57.72 years. Baseline characteristics were well balanced except that there were less hypertensive people in thrombus aspiration group as compared to conventional PPCI group (56 vs. 73, P=0.047). With respect to medication, it was noted that conventional PPCI group received more ACE inhibitor drugs than thrombus aspiration group (38 vs. 28, P=0.035).
Baseline characteristics are illustrated in Table 1.
Table 1.
Baseline characteristics of the study population
| Characteristics | Thrombus aspiration (n=119) | Standard primary PCI (n=122) | p value |
|---|---|---|---|
| Age (Mean ± SD, years) | 56.99±11.13 | 58.44±11.06 | 0.310 |
| Male, n (%) | 106 (89.1%) | 103 (84.4%) | 0.288 |
| Risk Factors | |||
| Diabetes mellitus, n (%) | 42 (35.3%) | 38 (31.1%) | 0.494 |
| Smoking, n (%) | 74 (62%) | 65 (53%) | 0.264 |
| Hypertension, n (%) | 56 (47.1%) | 73 (59.8%) | 0.047* |
| Hypercholesterolemia, n (%) | 64 (54%) | 56 (46%) | 0.576 |
| Positive Family history, n (%) | 14 (12%) | 12 (10%) | 0.986 |
| Cardiac history | |||
| Renal insufficiency, n (%) | 5 (4%) | 4 (3%) | 0.986 |
| Previous stroke, n (%) | 1 (0.8%) | 0 (0%) | 0.310 |
| Previous MI, n (%) | 2 (1.7%) | 0 (0%) | 0.150 |
| Previous CABG, n (%) | 0 (0%) | 0 (0%) | |
| Previous PCI, n (%) | 2 (1.7%) | 0 (0%) | 0.150 |
| Unstable angina, n (%) | 119 (100%) | 122 (100%) | |
| Myocardial infarction, n (%) | 119 (100%) | 121 (99.2%) | 0.322 |
| Anti-platelet drugs | |||
| Aspirin, n (%) | 119 (100%) | 122 (100%) | 0.569 |
| Clopidogrel, n (%) | 62 (52.1%) | 63 (51.7%) | 0.731 |
| Prasugrel, n (%) | 7(5.9%) | 16 (13.1%) | 0.056 |
| Other antiplatelet, n (%) | 50(42%) | 43 (35.2%) | 0.280 |
| Other medications | |||
| Heparin, n (%) | 119 (100%) | 122 (100%) | 0.088 |
| ACE inhibitor, n (%) | 23 (19.3%) | 38 (31.1%) | 0.035* |
| Angiotensin II antagonist, n (%) | 1 (0.8%) | 5 (4.1%) | 0.105 |
| Beta-blockers, n (%) | 32 (26.9%) | 42.34.4 (%) | 0.205 |
| Calcium antagonist, n (%) | 1 (0.8%) | 0 (0%) | 0.310 |
| Nitrates, n (%) | 4 (3.4%) | 9 (7.4%) | 0.168 |
| Statins, n (%) | 119 (100%) | 122 (100%) | 0.911 |
| Other lipid lowering drugs, n (%) | 1 (0.8%) | 1 (0.8%) | 0.986 |
| Diuretics, n (%) | 6 (5%) | 7 (5.7%) | 0.811 |
| Baseline LVEF | 35% +/- 5% | 34% +/- 4% | 0.15 |
MI - Myocardial infarction; CABG - Coronary artery bypass graft; PCI - Percutaneous coronary intervention; LVEF: left ventricular ejection fraction;
Significant.
Lesion and procedural characteristics
The radial route was found to be the most commonly used route for angioplasty in both the groups and single-vessel disease was observed more in both groups. There were no significant differences in arterial access, no. of vessels treated in patients between the groups (P>0.05).
Among the study population, type C lesions were found to be significantly higher in thrombus aspiration group compared to standard primary PCI group [110 (86.6%) vs. 97 (72.9%), P=0.011]. Similarly, stent diameter was found to be significantly higher in the thrombus aspiration group (3.277±0.4059) compared to the standard primary PCI group (3.103±0.4272), respectively (P=0.001). Whereas, pre-balloon dilation showed standard primary PCI group was significantly higher than the thrombus aspiration group [108 (81.2%) vs. 86 (67.7%), P=0.013]. All the other characteristics such as post-balloon dilation, device success, and procedure success did not show any significant difference (P>0.05).
Lesion and procedural characteristics are depicted in Table 2.
Table 2.
Lesion and procedural characteristics of the study population
| Characteristics | Thrombus aspiration (n=119) | Standard primary PCI (n=122) | p value |
|---|---|---|---|
| Vessel treated | |||
| MVD, n (%) | 7 (5.9%) | 11 (9%) | 0.355 |
| SVD, n (%) | 112 (94.1%) | 111 (91%) | |
| Arterial access site | |||
| Femoral, n (%) | 29 (24%) | 20 (16.4%) | 0.154 |
| Radial, n (%) | 89 (75%) | 102 (83.6%) | |
| Brachial, n (%) | 1 (1%) | 0 (0%) | |
| Vessel Name | |||
| LAD, n (%) | 55 (43.3%) | 61 (45.9%) | 0.274 |
| LCX, n (%) | 15 (11.8%) | 26 (19.5%) | |
| OM1, n (%) | 1 (0.8%) | 1 (0.8%) | |
| OM2, n (%) | 1 (0.8%) | 1 (0.8%) | |
| RCA, n (%) | 55 (43.3%) | 44 (33.1%) | |
| Lesion type | |||
| Type A, n (%) | 4 (3.1%) | 3 (2.3%) | 0.011* |
| Type B1, n (%) | 10 (7.9%) | 19 (14.3%) | |
| Type B2, n (%) | 3 (2.4%) | 13 (9.8%) | |
| Type B3, n (%) | 0 (0%) | 1 (0.8%) | |
| Type C, n (%) | 110 (86.6%) | 97 (72.9%) | |
| Pre balloon dilation, n (%) | 86 (67.7%) | 108 (81.2%) | 0.013* |
| Post balloon dilation, n (%) | 102 (80.3%) | 117 (88%) | 0.090 |
| Device success, n (%) | 124 (97.6%) | 132 (99.2%) | 0.292 |
| Procedure success, n (%) | 115 (90.6%) | 128 (96.2%) | 0.505 |
| Stent | |||
| Diameter (Mean ± SD, mm) | 3.277±0.405 | 3.103±0.4272 | 0.001* |
| Length (Mean ± SD, mm) | 25.22±7.584 | 25.06±7.706 | 0.863 |
| Antiplatelet during hospital stay | |||
| Aspirin, n (%) | 119 (100%) | 121 (99%) | 0.968 |
| Clopidogrel, n (%) | 59 (49.6%) | 59 (48.4%) | 0.148 |
| Prasugrel, n (%) | 10 (8.4%) | 20 (16.4%) | |
| Ticagrelor, n (%) | 50 (42%) | 43 (35.2%) | |
MVD - Multi vessel disease; SVD - Single vessel disease; LAD - Left anterior descending artery; LCX - Left circumflex artery; OM - Obtuse marginal artery; RCA - Right coronary artery;
Significant.
Clinical outcomes
At 1-year follow-up, the MACE rate was found to be 4.2% and 4.9% in thrombus aspiration and standard primary PCI group, respectively (P=0.79). Kaplan-Meier curve for MACE is shown in Figure 1. The death from any cause was found to be higher in thrombus aspiration 7 (5.9%) compared to standard primary PCI group 5 (4.1%). Of these, 5 (4.2%) patients in thrombus aspiration group and 4 (3.3%) patients in standard primary PCI group had cardiac death (P=0.747). Whereas, 2 (1.7%) patients in thrombus aspiration group and 1 (0.8%) patient in standard primary PCI group had non-cardiac death (P=0.747). There was no statistically significant difference in cardiac and non-cardiac death between the two groups. Definite stent thrombosis was observed in each 1 (0.8%) patient of both the groups and there is no significant difference between the two groups (P=1.00). There was insignificantly higher left ventricular ejection fraction seen among the subjects of thrombus aspiration group than standard PCI group (P=0.09) from baseline. Clinical outcomes are demonstrated in Table 3.
Figure 1.
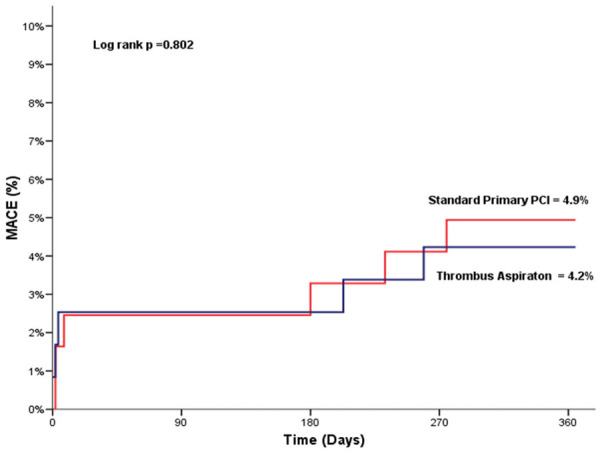
Kaplan-Meier curve for major adverse cardiac events (MACE).
Table 3.
Clinical outcomes at 1-year follow-up
| Outcomes | Thrombus aspiration (n=119) | Standard primary PCI (n=122) | p value |
|---|---|---|---|
| MACE, n (%) | 5 (4.2%) | 6 (4.9%) | 0.79 |
| Death from any cause, n (%) | 7 (5.9%) | 5 (4.1%) | |
| Cardiac death, n (%) | 5 (4.2%) | 4 (3.3%) | 0.747 |
| Non-cardiac death, n (%) | 2 (1.7%) | 1 (0.8%) | 0.619 |
| Myocardial infarction, n (%) | 0 (0%) | 0 (0%) | |
| Target lesion revascularization, n (%) | 0 (0%) | 2 (1.6%) | 0.498 |
| Stent thrombosis, n (%) | 1 (0.8%) | 1 (0.8%) | 1.00 |
| Definite stent thrombosis, n (%) | 1 (0.8%) | 1 (0.8%) | 1.00 |
| Probable stent thrombosis, n (%) | 0 (0%) | 0 (0%) | |
| Possible stent thrombosis, n (%) | 0 (0%) | 0 (0%) | |
| LVEF at 1 year | 42 +/- 12% | 45 +/- 10% | 0.09 |
MACE - Major adverse cardiac events; LVEF: left ventricular ejection fraction.
Discussion
In this retrospective study involving patients with STEMI, we aimed to evaluate the impact of adjunctive thrombectomy on MACE during long-term follow-up. It was observed that during long-term follow-up at 1-year, MACE rate in the two groups was similar.
Similar to this study results, many thrombus aspiration randomized trials have shown inconsistent results with respect to mortality rate. Some studies have shown mortality benefits [14,15] whereas some studies have shown no significant results [16-18]. Further, those studies reported that these inconsistencies among previous analyses may be due to several factors such as differences in the follow-up time, duration of symptoms, number of participating centers, and the finding of mechanical aspiration devices that may be inferior to manual aspiration devices [18,19].
Thrombus aspiration may not be a totally risk-free procedure as the first randomized trial on routine thromboaspiration failed to demonstrate a significant benefit of thrombus aspiration in term of short-term mortality [9], though at the end of 1-year follow up it was observed that mortality rate was lower in thrombus aspiration group compared to primary PCI [20]. Similarly, in the TASTE trial, they reported that possible differences in clinical events will evident only with longer follow-up [3]. These results indicate that possible harmful effects of adjunctive thrombus aspiration occur only in the starting in-hospital duration.
In support of this study, a recent updated comprehensive meta-analysis of 18 randomized control trials with 20,641 STEMI patients demonstrated that routine thrombus aspiration before primary PCI has no apparent benefit on MACE, cardiac death and all-cause mortality [4]. In addition, this study observed that there was no difference in stent thrombosis between the two groups. However, the recent updated comprehensive meta-analysis also explained that the trend of lower stent thrombosis with thrombus aspiration could probably due to an overestimation of the treatment effect [4]. Further, the prospective randomized TOTAL trial reported that there was no difference in the clinical outcomes with thrombus aspiration compared to conventional primary PCI [21]. Based on this evidence, the present study supports that thrombus aspiration has given neutral outcomes compared to primary PCI in the long-term follow-up. Although mechanical thrombus aspiration has been shown to improve the outcomes in acute ischemic stroke [22], the routine thrombus aspiration may not appear to improve the clinical outcomes but can be useful in improving the myocardial reperfusion. The one possible reason behind this could be ineffectivity of available thrombus aspiration devices [23].
Study limitations
This study does have few limitations such as it represents a single-center experience with a small number of sample sizes to assess the impact of thrombus aspiration efficacy on medium-term mortality. As it is a retrospective study it was not possible to account for all confounding influences.
Conclusion
This retrospective study comparing thrombus aspiration with conventional primary PCI in STEMI patients found no significant benefit of thrombus aspiration with respect to mortality rate or any other clinical outcomes at 1-year. Thrombus aspiration can be useful in STEMI patients to improve myocardial reperfusion. Further studies are required to evaluate the benefit of thrombus aspiration in selected patient populations.
Disclosure of conflict of interest
None.
References
- 1.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Ting HH, O’Gara PT, Kushner FG, Ascheim DD, Brindis RG, Casey DE Jr, Chung MK, de Lemos JA, Diercks DB, Fang JC, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. 2016;67:1235–50. doi: 10.1016/j.jacc.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Kushner FG, Hand M, Smith SC, King SB, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE Jr, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American college of cardiology foundation/American heart association task force on practice guidelines. J Am Coll Cardiol. 2009;54:2205–41. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 3.Fröbert O, Lagerqvist B, Olivecrona GK, Omerovic E, Gudnason T, Maeng M, Aasa M, Angerås O, Calais F, Danielewicz M, Erlinge D, Hellsten L, Jensen U, Johansson AC, Kåregren A, Nilsson J, Robertson L, Sandhall L, Sjögren I, Ostlund O, Harnek J, James SK TASTE Trial. Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med. 2013;369:1587–1597. doi: 10.1056/NEJMoa1308789. [DOI] [PubMed] [Google Scholar]
- 4.Elgendy AY, Elgendy IY, Mahmoud AN, Bavry AA. Long-term outcomes with aspiration thrombectomy for patients undergoing primary percutaneous coronary intervention: a meta-analysis of randomized trials. Clin Cardiol. 2017;40:534–41. doi: 10.1002/clc.22691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henriques J, Zijlstra F, Ottervanger J, De Boer MJ, Van’T Hof A, Hoorntje J, Suryapranata H. Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J. 2002;23:1112–1117. doi: 10.1053/euhj.2001.3035. [DOI] [PubMed] [Google Scholar]
- 6.Silva-Orrego P, Colombo P, Bigi R, Gregori D, Delgado A, Salvade P, Oreglia J, Orrico P, Biase A, Piccalò G, Bossi I, Klugmann S. Thrombus aspiration before primary angioplasty improves myocardial reperfusion in acute myocardial infarction: the DEAR-MI (dethrombosis to enhance acute reperfusion in myocardial infarction) study. J Am Coll Cardiol. 2006;48:1552–1559. doi: 10.1016/j.jacc.2006.03.068. [DOI] [PubMed] [Google Scholar]
- 7.Opie L. Reperfusion injury and its pharmacologic modification. Circulation. 1989;80:1049–62. doi: 10.1161/01.cir.80.4.1049. [DOI] [PubMed] [Google Scholar]
- 8.Sardella G, Mancone M, Bucciarelli-Ducci C, Agati L, Scardala R, Carbone I, Francone M, Roma AD, Benedetti G, Conti G, Fedele F. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size: the EXPIRA (thrombectomy with export catheter in infarct-related artery during primary percutaneous coronary intervention) prospective, randomized trial. J Am Coll Cardiol. 2009;53:309–315. doi: 10.1016/j.jacc.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Svilaas T, Vlaar PJ, van der Horst IC, Diercks GF, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358:557–567. doi: 10.1056/NEJMoa0706416. [DOI] [PubMed] [Google Scholar]
- 10.Antoniucci D, Valenti R, Migliorini A, Parodi G, Memisha G, Santoro GM, Sciagrà R. Comparison of rheolytic thrombectomy before direct infarct artery stenting versus direct stenting alone in patients undergoing percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2004;93:1033–1035. doi: 10.1016/j.amjcard.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 11.Napodano M, Pasquetto G, Saccà S, Cernetti C, Scarabeo V, Pascotto P, Reimers B. Intracoronary thrombectomy improves myocardial reperfusion in patients undergoing direct angioplasty for acute myocardial infarction. J Am Coll Cardiol. 2003;42:1395–1402. doi: 10.1016/s0735-1097(03)01041-6. [DOI] [PubMed] [Google Scholar]
- 12.Resnic FS, Wainstein M, Lee MK, Behrendt D, Wainstein RV, Ohno-Machado L, Kirshenbaum JM, Rogers CD, Popma JR, Piana R. No-reflow is an independent predictor of death and myocardial infarction after percutaneous coronary intervention. Am Heart J. 2003;145:42–46. doi: 10.1067/mhj.2003.36. [DOI] [PubMed] [Google Scholar]
- 13.Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, McFadden E, Lansky A, Hamon M, Krucoff MW, Serruys PW Academic Research Consortium. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344–2351. doi: 10.1161/CIRCULATIONAHA.106.685313. [DOI] [PubMed] [Google Scholar]
- 14.Burzotta F, De Vita M, Gu YL, Isshiki T, Lefèvre T, Kaltoft A, Dudek D, Sardella G, Orrego PS, Antoniucci D, De Luca L, Biondi-Zoccai GG, Crea F, Zijlstra F. Clinical impact of thrombectomy in acute ST-elevation myocardial infarction: an individual patient-data pooled analysis of 11 trials. Eur Heart J. 2009;30:2193–203. doi: 10.1093/eurheartj/ehp348. [DOI] [PubMed] [Google Scholar]
- 15.Bavry AA, Kumbhani DJ, Bhatt DL. Role of adjunctive thrombectomy and embolic protection devices in acute myocardial infarction: a comprehensive meta-analysis of randomized trials. Eur Heart J. 2008;29:2989–3001. doi: 10.1093/eurheartj/ehn421. [DOI] [PubMed] [Google Scholar]
- 16.De Luca G, Navarese EP, Suryapranata H. A meta-analytic overview of thrombectomy during primary angioplasty. Int J Cardiol. 2013;166:606–12. doi: 10.1016/j.ijcard.2011.11.102. [DOI] [PubMed] [Google Scholar]
- 17.Mongeon FP, Bélisle P, Joseph L, Eisenberg MJ, Rinfret S. Adjunctive thrombectomy for acute myocardial infarction: a bayesian meta-analysis. Circ Cardiovasc Interv. 2010;3:6–16. doi: 10.1161/CIRCINTERVENTIONS.109.904037. [DOI] [PubMed] [Google Scholar]
- 18.Tamhane UU, Chetcuti S, Hameed I, Grossman PM, Moscucci M, Gurm HS. Safety and efficacy of thrombectomy in patients undergoing primary percutaneous coronary intervention for acute ST elevation MI: a meta-analysis of randomized controlled trials. BMC Cardiovasc Disord. 2010;10:10. doi: 10.1186/1471-2261-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaltoft A, Bøttcher M, Nielsen SS, Hansen HH, Terkelsen C, Maeng M, Kristensen J, Thuesen L, Krusell LR, Kristensen SD, Andersen HR, Lassen JF, Rasmussen K, Rehling M, Nielsen TT, Bøtker HE. Routine thrombectomy in percutaneous coronary intervention for acute ST-segment-elevation myocardial infarction: a randomized, controlled trial. Circulation. 2006;114:40–7. doi: 10.1161/CIRCULATIONAHA.105.595660. [DOI] [PubMed] [Google Scholar]
- 20.Vlaar PJ, Svilaas T, van der Horst IC, Diercks GF, Fokkema ML, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Cardiac death and reinfarction after 1 year in the thrombus aspiration during percutaneous coronary intervention in acute myocardial infarction study (TAPAS): a 1-year follow-up study. Lancet. 2008;371:1915–20. doi: 10.1016/S0140-6736(08)60833-8. [DOI] [PubMed] [Google Scholar]
- 21.Jolly SS, Cairns JA, Yusuf S, Rokoss MJ, Gao P, Meeks B, Kedev S, Stankovic G, Moreno R, Gershlick A, Chowdhary S, Lavi S, Niemela K, Bernat I, Cantor WJ, Cheema AN, Steg PG, Welsh RC, Sheth T, Bertrand OF, Avezum A, Ravinay Bhindi R, Natarajan MK, Horak D, Leung RC, Kassam S, Rao SV, El-Omar M, Mehta SR, Velianou JL, Pancholy S, Džavík V TOTAL Investigators. Outcomes after thrombus aspiration for ST elevation myocardial infarction: 1-year follow-up of the prospective randomised total trial. Lancet. 2016;387:127–35. doi: 10.1016/S0140-6736(15)00448-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elgendy IY, Kumbhani DJ, Mahmoud A, Bhatt DL, Bavry AA. Mechanical thrombectomy for acute ischemic stroke: a meta-analysis of randomized trials. J Am Coll Cardiol. 2015;66:2498–505. doi: 10.1016/j.jacc.2015.09.070. [DOI] [PubMed] [Google Scholar]
- 23.Elgendy IY, Mahmoud AN, Mansoor H, Mojadidi MK, Bavry AA. Evolution of acute ischemic stroke therapy from lysis to thrombectomy: similar or different to acute myocardial infarction? Int J Cardiol. 2016;222:441–7. doi: 10.1016/j.ijcard.2016.07.251. [DOI] [PubMed] [Google Scholar]


