Abstract
Background: Parenting a child with a serious life-threatening illness (SLTI) may impact parents' mental health. The protective association of social support with anxiety over time following an acute medical event has not been empirically tested in a sample of parents of children with oncologic and nononcologic serious illnesses.
Objective: To test the potential association of perceived social support with anxiety in parents of children with SLTIs over time.
Design: Prospective cohort study.
Setting/Subjects: Two hundred parents of 158 children in the Decision Making in Serious Pediatric Illness study, conducted at the Children's Hospital of Philadelphia.
Measurements: Parental anxiety and perceived social support were assessed using the Hospital Anxiety and Depression Scale (HADS) and the Social Provisions Scale (SPS). We performed bivariate linear regressions to test cross-sectional and longitudinal associations between the SPS and anxiety scores at baseline, 12 months, and 24 months.
Results: The average SPS total and subscale scores decreased significantly from baseline to 12 months, and increased from 12 to 24 months. The average HADS-Anxiety scores decreased significantly from baseline to 12 months, and remained stable at 24 months. Cross-sectionally, total SPS scores were negatively associated with anxiety scores at each time point. Longitudinally, SPS scores were associated with anxiety scores, although this association weakened in adjusted modeling.
Conclusions: Over a two-year period, higher levels of perceived social support were associated with lower levels of anxiety in parents of seriously ill children. Clinicians and researchers should work to optimize social support for families to improve parental mental health outcomes.
Keywords: anxiety, children with serious illness, parents, social support
Introduction
Parenting a child with a serious life-threatening illness (SLTI) is remarkably demanding. In addition to serious physical, financial, and psychosocial implications,1–4 parents' mental health is particularly adversely affected1,2,4–14: psychological distress is reported to be present in as many as 70% of these parents.12 and clinical anxiety and depression in as many as 25–28%.13,15
Perceived social support, defined as the “subjective judgment that family and friends would provide quality assistance during times of trouble,”16 may improve the mental well-being of parents of children with serious illness. This support may come in the form of emotional (e.g., spending time, expressing affection) or practical (e.g., helping with child care or household tasks) support.4,16 Qualitative,17–20 case/control,21 and cross-sectional22 studies have suggested that perceived social support may lessen the impact of a child's illness on parents' mental health, and more specifically, research on parents of children with cancer has found that perceived social support may affect parental mood,21 stress and coping,6,21 levels of psychological distress,23,24 and mental health-related functioning.25
The protective association of perceived social support with parental anxiety over time has been empirically tested in parents of children with cancer,24,25 but not in other diagnosis groups. This raises the question about whether findings from previous studies would also apply to parents of children with other diagnoses.26–28 Studies on parents of children with various nonmalignant diseases have highlighted the relationship between social support and psychological outcomes,29,30 although these studies have not investigated this relationship over time. In addition, while the long-term effect of social support on parental anxiety has been tested from the point of diagnosis,24 no longitudinal studies have been completed that have studied the relationship between social support and anxiety after an acute medical event, such as a child's hospitalization.
In the following analysis, we tested the hypothesis that a higher perceived social support among parents of children with SLTIs would be associated cross-sectionally and over time with lower levels of anxiety.
Methods
Study design and participants
The participants in this study were parents of seriously ill children in the Decision Making in Serious Pediatric Illness study, a prospective cohort study on parental decision making in the pediatric serious illness context. This study was conducted at the Children's Hospital of Philadelphia (CHOP) from September 2010 to December 2014. CHOP's Institutional Review Board approved the study protocol.
“Parents” included biological, adoptive, or foster parents, and extended family members who were the child's primary decision makers. Parents were eligible for participation if they and their child met the following criteria: the child was a patient at CHOP and had been admitted to the pediatric, neonatal, or cardiac intensive care units, or had been referred to the pediatric advanced care team for palliative care services; the child's attending physician thought that the child had a serious illness and that the parents would likely have to make a major medical decision within the next 12–24 months; the parent was responsible for medical decisions because the child was younger than 18 years or cognitively impaired; and the parents spoke English. Parents were not eligible if the child had died, been discharged, or experienced a nonaccidental injury; or if the parent had lost custody rights. In addition, parents were ineligible if the child's physician deemed the parent to be emotionally overwhelmed or the physician thought the child might die within a month (due to the longitudinal study design; n = 6, <1% of screened parents).
Parents who consented to participate completed a one-hour in-person interview at baseline (i.e., during the hospital admission), and 20-minute interviews by phone or online at subsequent interviews. Other details about recruitment and study procedures have been reported previously.31–33
Measures
Demographics
Parents completed a baseline demographic questionnaire, which included diagnosis, age, race, ethnicity, educational attainment, and relationship status.
Hospital Anxiety and Depression Scale
Parental anxiety was assessed at baseline, 12, and 24 months with the 14-item Hospital Anxiety and Depression Scale (HADS),34 which consists of 2 subscales (HADS-Anxiety and HADS-Depression), each of which contain 7-items. Items are rated on a 4-point scale (0–3) with a maximum summated score of 21 for each subscale; higher summated scores indicate higher anxiety/depression levels.35 In our sample, the HADS-Anxiety subscale Cronbach's alpha coefficient was 0.86, consistent with previous studies of caregivers in the palliative care setting.36–38
Social Provisions Scale
Parent-reported social support was assessed at baseline, 12, and 24 months with the Social Provisions Scale (SPS), which is a 24-item, validated measure used in previous research to study respondents' perceptions of social support.39–45 The SPS was developed based on the six social provisions identified by Weiss (1974), including guidance (perceived ability to obtain advice or information from others), reliable alliance (perceived ability to rely on others for practical assistance), reassurance of worth (recognition by others of one's competence, skills, and value), social integration (feeling connected to a group that shares similar interests and concerns), attachment (a sense of emotional closeness from which one can derive a sense of security), and opportunity to provide nurturance (a sense that others rely on one for their well-being).46,47 Each provision is assessed by four items, and items are scored along a 4-point Likert scale (1 = strongly disagree to 4 = strongly agree). Higher summated scores (across the entire instrument and for each provision) indicate higher perceived levels of social support.41,42,48 In our sample, Cronbach's alpha for the total scale was 0.91 and the subscales ranged from 0.56 to 0.78 (Attachment, 0.71; Reassurance of Worth, 0.78; Social Integration, 0.56; Reliable Alliance, 0.56; Guidance, 0.75; Opportunity to Provide Nurturance, 0.63), consistent with previous studies that reported total scale alphas ranging from 0.71 to 0.9243,49–53 and subscale alphas from 0.34 to 0.83.43,49,53
Child's perceived health status
Parents were asked to rate their child's current health, with 1 being worst health and 10 being best health.
Statistical analyses
We first described mean SPS and HADS-Anxiety scores at baseline, 12 months, and 24 months. We next performed bivariate linear regressions to test the cross-sectional association between SPS total scores and anxiety scores at baseline, 12 months, and 24 months, as well as the longitudinal association between baseline SPS total scores and anxiety scores at 12 and 24 months. Based on previous literature6,21,23–25,54 and the commonly accepted 10% cutoff for change-in-estimate criterion of confounder identification,55 we also adjusted for baseline anxiety levels, parent type (i.e., mother, father, other caregiver), parent educational attainment, and child's perceived health. Statistical analyses were performed using the statistical software package Stata/IC 15.1 (StataCorp, College Station, TX), and p-values <0.05 were considered statistically significant.
In additional exploratory analysis, we performed multivariate regression using stepwise backward elimination to determine the most parsimonious model of SPS subscales that predict anxiety scores at baseline, 12 months, and 24 months. In brief, we began with the full model of all subscales and covariates, and sequentially eliminated subscales at each step with a p-value ≥0.2, which is the level-of-stay significance recommended for small datasets.56
Due to the patient population (i.e., children with serious illnesses) and the longitudinal study design, some participants were, inevitably, lost to follow-up. Restricting the analysis to complete cases (i.e., parents who had responses to all variables) using listwise deletion would reduce the sample from 200 to 83 parents, resulting in significant loss of statistical power, larger standard errors (SEs), and wider confidence intervals.57 Because of limitations of complete case analysis,58,59 we used multiple imputation to generate sets of plausible estimates of missing values.57,58 Multiple imputation is a flexible, simulation-based statistical technique57 that has been used to address missing data in previous palliative care research.59–61 We performed multiple imputation using chained equations (MICE) to generate M = 20 imputed datasets following a linear regression model.57 Overall, 7.6–8.3% of cases were imputed across variables.
Finally, we conducted logistic regression modeling to assess whether there were any associations between demographic or social support variables and nonparticipation or attrition.
Results
Description of sample
Of 295 parents approached, 95 parents declined to participate (67.8% participation rate). Our sample consisted of 200 parents (of 158 children) (Table 1) who completed the baseline interview, 113 (of 90 children) who completed the 12-month interview, and 97 (of 77 children) who completed the 24-month interview.
Table 1.
Demographic and Clinical Characteristics of Children and Parents at Baseline
| N (%) | |
|---|---|
| Children's characteristics (n = 158) | |
| Age | |
| 1 Year or less | 107 (67.7) |
| 2–4 Years | 19 (12.0) |
| 5–9 Years | 11 (7.0) |
| 10–18 Years | 21 (13.3) |
| Gender | |
| Female | 73 (46.2) |
| Male | 85 (53.8) |
| Race | |
| White | 118 (74.7) |
| African American | 20 (12.6) |
| More than one race/other | 17 (10.8) |
| Missing | 3 (1.9) |
| Ethnicity | |
| Non-Hispanic | 137 (86.7) |
| Hispanic | 19 (12.0) |
| Missing | 2 (1.3) |
| Primary complex chronic condition (Note: not mutually exclusive; thus, the % does not sum to 100%) | |
| Cardiovascular | 77 (48.7) |
| Respiratory | 89 (56.3) |
| Congenital or genetic | 111 (70.3) |
| Neuromuscular | 63 (39.9) |
| Metabolic | 17 (10.8) |
| Malignancy | 15 (9.5) |
| Renal | 16 (10.1) |
| Other | 53 (33.5) |
| Parents' characteristics (n = 200) | |
| Parent type | |
| Mother | 136 (68) |
| Father | 60 (30) |
| Other | 4 (2) |
| Age | |
| Mean/SD | 33.7 (7.92) |
| Missing | 1 |
| Race | |
| White | 161 (80.5) |
| African American | 22 (11.0) |
| More than one race/other | 15 (7.5) |
| Missing | 2 (1.0) |
| Ethnicity | |
| Non-Hispanic | 180 (90) |
| Hispanic | 17 (8.5) |
| Missing | 3 (1.5) |
| Highest education level completed | |
| High school/general educational development | 33 (16.5) |
| Trade/technical/vocational | 8 (4.0) |
| College/graduate school | 159 (79.5) |
| Relationship status | |
| Married/partnered | 171 (85.5) |
| Separated/divorced/widowed | 6 (3.0) |
| Single | 23 (11.5) |
| No. of other children | |
| 0 | 66 (33.0) |
| 1–4 | 123 (61.5) |
| 5+ | 10 (5.0) |
| Missing | 1 (0.5) |
| Employment status | |
| Full-time | 99 (49.5) |
| Part-time | 23 (11.5) |
| Not employed/looking for employment | 34 (17.0) |
| Homemaker | 42 (21.0) |
| Retired | 2 (1.0) |
Unless otherwise noted, cell entries are percentages. Percentages are within each demographic or clinical characteristic variable, and include missing data if present.
SD, standard deviation.
The average total SPS score at baseline was 87.5 (SE 0.57) out of 96 possible points (Table 2). This mean score decreased to 76.7 (SE 0.93) at 12 months, and increased to 83.0 (SE 1.06) at 24 months (Table 2). The differences between baseline SPS scores and 12-month (F1.66 = 146.0; p < 0.01) and 24-month (F1,88 = 23.0; p < 0.01) SPS scores were statistically significant. Average SPS subscale scores ranged from 13.9 for Social Integration to 15.3 for Reliable Alliance (out of 16 possible points) at the baseline interview. These scores followed a similar pattern to the SPS total scores over time, dipping at 12 months (lowest score: Attachment 11.6; highest score: Reassurance of worth 13.6) and rebounding at 24 months (lowest score: Social integration 13.1; highest score: Reliable alliance 14.5) (Table 2).
Table 2.
Descriptive Statistics of Study Measures Across Time Points
| Study measure | Baseline visit (N = 200) |
12-Month visit (N = 113) |
24-Month visit (N = 97) |
|---|---|---|---|
| M (SE) | M (SE) | M (SE) | |
| SPS total score (24–96) | 87.5 (0.57) | 76.7 (0.93) | 83.0 (1.06) |
| SPS subscale scores (4–16) | |||
| Guidance | 14.9 (0.14) | 13.4 (0.20) | 14.1 (0.23) |
| Reliance alliance | 15.3 (0.10) | 13.1 (0.19) | 14.5 (0.20) |
| Reassurance of worth | 14.0 (0.13) | 13.6 (0.22) | 13.4 (0.21) |
| Social integration | 13.9 (0.12) | 12.0 (0.16) | 13.1 (0.21) |
| Attachment | 14.8 (0.13) | 11.6 (0.23) | 13.8 (0.24) |
| Opportunity to provide nurturance | 14.6 (0.11) | 13.0 (0.18) | 14.1 (0.19) |
| HADS-Anxiety (0–21) | 10.0 (0.32) | 8.4 (0.41) | 8.4 (0.44) |
HADS, Hospital Anxiety and Depression Scale; SE, standard error; SPS, Social Provisions Scale.
The average HADS-Anxiety score at baseline was 10.0 (SE 0.32) out of 21 possible points. This mean score decreased to 8.4 (SE 0.41) at 12 months and remained at 8.4 (SE 0.44) at 24 months (Table 2). Differences between baseline and 12-month (F1,92 = 7.3; p < 0.01) and 24-month (F1,91 = 10.1; p < 0.01) anxiety levels were statistically significant.
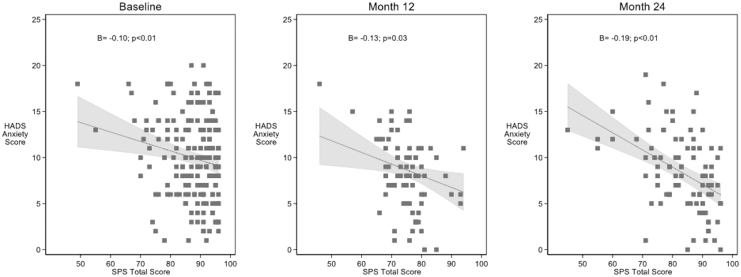
Cross-sectional association between total SPS scores and HADS-Anxiety
Cross-sectionally, total SPS scores were negatively associated with HADS-Anxiety scores at baseline (B = −0.10, p < 0.01, 95% CI = −0.17 to −0.03), 12 months (B = −0.13, p = 0.03; 95% CI = −0.24 to −0.01), and 24 months (B = −0.19, p < 0.01; 95% CI = −0.25 to −0.12) (Fig. 1). After adjusting for parent role, parent education, and child's perceived health, total SPS scores remained negatively associated with HADS-Anxiety scores at each interview (Table 3, top portion). The adjusted estimates represent small-to-medium effect sizes of SPS scores on HADS-Anxiety scores.
FIG. 1.
Cross-sectional association of perceived social support with anxiety at each time point.
Table 3.
Adjusted Models of Perceived Social Support and Anxiety
| Time (N) | Covariates | B | 95% CI | p |
|---|---|---|---|---|
| Cross-sectional | ||||
| Baseline (200) | (intercept) | 23.4 | <0.01 | |
| SPS total | −0.1 | −0.21 to −0.05 | <0.01 | |
| Parent role (dad) | −1.3 | −2.56 to 0.06 | 0.06 | |
| Parent role (other) | −0.2 | −4.60 to 4.20 | 0.92 | |
| Parent education | 0.1 | −0.24 to 0.52 | 0.48 | |
| Child's perceived health | −0.4 | −0.61 to −0.13 | <0.01 | |
| 12 Months (113) | (intercept) | 22.7 | <0.01 | |
| SPS total | −0.1 | −0.24 to −0.02 | 0.03 | |
| Parent role (dad) | −0.9 | −2.55 to 0.78 | 0.30 | |
| Parent role (other) | 1.6 | −2.43 to 5.60 | 0.43 | |
| Parent education | −0.1 | −0.60 to 0.49 | 0.85 | |
| Child's perceived health | −0.6 | −1.00 to −0.09 | 0.02 | |
| 24 Months (97) | (intercept) | 26.2 | <0.01 | |
| SPS total | −0.2 | −0.22 to −0.09 | <0.01 | |
| Parent role (dad) | −2.1 | −3.30 to −0.87 | <0.01 | |
| Parent role (other) | Omitted | N/A | ||
| Parent education | 0.2 | −0.33 to 0.65 | 0.52 | |
| Child's perceived health | −0.6 | −1.00 to −0.26 | <0.01 | |
| Longitudinal | ||||
| 12 Months (113) | (intercept) | 18.5 | <0.01 | |
| SPS total at baseline | −0.1 | −0.20 to −0.01 | 0.06 | |
| Anxiety at baseline | 0.2 | 0.05 to 0.41 | 0.01 | |
| Parent type (dad) | −0.3 | −1.90 to 1.30 | 0.73 | |
| Parent type (other) | 0.6 | −4.20 to 5.40 | 0.80 | |
| Parent education | 0.1 | −0.48 to 0.69 | 0.72 | |
| Child's perceived health | −0.5 | −0.98 to −0.08 | 0.02 | |
| 24 Months (97) | (intercept) | 11.0 | <0.01 | |
| SPS total at baseline | −0.01 | −0.09 to 0.07 | 0.78 | |
| Anxiety at baseline | 0.5 | 0.32 to 0.62 | <0.01 | |
| Parent type (dad) | −0.9 | −2.30 to 0.44 | 0.18 | |
| Parent type (other) | Omitted | N/A | ||
| Parent education | 0.1 | −0.36 to 0.54 | 0.68 | |
| Child's perceived health | −0.8 | −1.20 to −0.51 | <0.01 | |
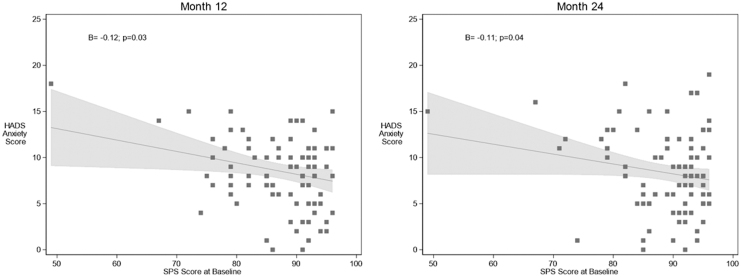
Longitudinal association between baseline SPS scores and subsequent HADS-Anxiety
Longitudinally, baseline SPS scores were associated with HADS-Anxiety scores at each follow-up interview. Higher baseline SPS scores remained negatively associated with lower HADS-Anxiety scores at 12 months (B = −0.12, p = 0.03; 95% CI = −.23 to −.01) and 24 months (B = −0.11, p = 0.04; 95% CI = −0.21 to −0.01) (Fig. 2). In the adjusted models, this association was present at 12 months (p = 0.06) with a small-to-medium effect size, but had dissipated by 24 months (p = 0.78) (Table 3, bottom portion).
FIG. 2.
Longitudinal association of perceived social support at baseline with anxiety at 12 and 24 months.
Additional exploratory analysis
To examine which aspect of social support was most strongly associated with subsequent anxiety levels, we implemented backward stepwise elimination in a multivariable regression model, accounting for baseline anxiety levels, parent type, parent education, and child's perceived health, to determine the most parsimonious combination of subscales to predict anxiety. The correlation between SPS subscales in this sample is displayed in Supplementary Table S1. After sequentially removing each subscale with a p-value of ≥0.2,56 we retained the Social Integration subscale at baseline (p < 0.01), at 12 months (p = 0.02), and at 24 months (p = 0.03) (Supplementary Table S2).
Finally, using logistic regression modeling, we identified only weak, statistically nonsignificant, and inconsistent associations between participant characteristics and missingness over time (analysis not shown).
Discussion
Among parents of children with primarily nononcologic SLTIs over a two-year period, we found that higher levels of perceived social support were associated with lower levels of anxiety in both the cross-sectional and longitudinal models. Specifically, the Social Integration subscale from the SPS appeared to be most consistently predictive of anxiety levels over time. This longitudinal association between perceived social support at baseline and subsequent levels of anxiety was present a year later, even when accounting for baseline levels of anxiety, as well as parent type, parent education, and child's perceived health, before dissipating by 24 months. Finally, in this sample, the association between perceived social support and anxiety occurred in the context where both anxiety and social support scores decreased significantly in the 12 months following hospitalization.
Our observation of a statistically significant, medium-to-small-sized inverse association between social support and parental anxiety, both cross-sectionally and longitudinally, is consistent with, and extends beyond, previous studies. Qualitative studies have found that while parents sometimes felt isolated from their social network, parents identified social support as critical for coping with the emotional stress of parenting a seriously ill child.17–20 One cross-sectional case/control study of parents of children with cancer found that poor social support was the most important factor linked with poor mental health outcomes.21
Our two-year study time frame allowed us to examine the temporal relationship between social support and anxiety, affirming our hypothesis that social support has a protective association on parental anxiety over time. A study of 163 mothers of children with cancer also observed an inverse relationship between social support at the time of their child's hospitalization for stem cell transplantation and mothers' mental health-related functioning in the subsequent year.25 A five-year study of 94 parents of children with cancer, conversely, found that social support variables explained a proportion of the psychological distress for fathers five years after diagnosis, but not for mothers.24 This study, however, examined overall satisfaction with social support and quantity of positive/negative social interactions; our study used the SPS, which examined specific dimensions of social support. This study also focused on the oncology setting, whereas our study included a large sample of parents of children with nonmalignant SLTIs. Parents of children with nonmalignant diseases in previous studies had longer caregiving trajectories, greater unmet needs, fewer social support resources, and higher self-rated poorer overall health,26 in addition to less developed, accessible, and flexible health care services27 compared with families of children with malignant disease. Finally, while the association between social support and anxiety dissipated by 24 months in our adjusted modeling, this finding was not unexpected given that social support may be a dynamic, rather than fixed, attribute.
Beyond providing much firmer evidence of the association between perceived social support and parental anxiety, this study also has three other findings that warrant discussion. First, we observed that anxiety scores decreased significantly from baseline to 12 months, and were stable from 12 until 24 months. This decrease over time is consistent with previous studies, which found that parental anxiety and distress levels peak at the time of the child's diagnosis and trended downward to near-normative levels at 6,23 12,25 and 2062 months, and as far out as five years.24 Our analysis examined anxiety levels after an acute medical event (i.e., hospitalization), regardless of time since diagnosis. Anxiety levels likely spike during hospitalization, subsiding to more normal levels afterward. Future studies are needed to better understand fluctuations in parents' anxiety from a child's diagnosis through the course of illness, particularly surrounding acute medical events such as hospitalizations.
Second, we noted a significant decrease in perceived social support levels over time, particularly from baseline to 12 months, which is consistent with previous studies. One study of 94 parents of children with cancer found that the amount of perceived support peaked at diagnosis (which the authors termed “crisis support”) and declined during the first year, stabilizing at a fairly constant level through five years.24 Qualitative studies have observed that parents' social support networks may shrink,63 and parents may feel “forgotten,”18 as time passes after their child's diagnosis. Our findings indicate that, similar to social support following a diagnosis, “crisis” levels of social support may increase during hospitalization and decrease in the subsequent year.
Third, our analysis examined the specific dimensions of social support, which may provide a more nuanced understanding of how social support impacts parental anxiety. In particular, we found that the Social Integration subscale, which relates to the feeling of being connected to others who have similar interests, concerns, and shared experiences,64 was significantly associated with lower parental anxiety across time. Feeling connected to a network of family, friends, or other parents of ill children may be important for coping and adjustment to a child's diagnosis and treatment.28,63,65,66 Greater understanding of the concept of social integration may be important for understanding the impact of social support on parental anxiety, and how clinicians could best intervene to improve parental mental health outcomes during the course of their child's illness.
Our findings should be interpreted with four main limitations in mind. First, we recognize that while we observed an association between perceived social support and parental anxiety, we cannot infer causation. Second, the parent sample was demographically homogeneous, limiting generalizability. Third, we used multiple imputation to address missing data. We did not find a consistent pattern of missingness in participants over time, but the possibility that data were not missing entirely at random could not be ruled out.24,62 Fourth, we did not account for family-level factors (e.g., family cohesion) or personal factors (e.g., coping style or prior traumatic life events), which have been associated with parental distress and posttraumatic stress disorder (PTSD) symptomatology in pediatric oncology research.14,66
Despite these limitations, the results of this study suggest that clinicians might support parents by helping them tap into various forms of social support. For example, clinicians could help parents identify additional sources of support, particularly in the year following an acute medical event when parents may experience a significant decline in “crisis” levels of social support. Clinicians could connect parents with networks of other parents of children with similar illnesses, where parents may feel a natural sense of connectedness due to shared experiences.63 Future intervention-based research, however, is greatly needed in this area.
In conclusion, our analysis suggests that higher levels of social support are associated with lower levels of parental anxiety after an acute event, such as hospitalization, in parents of children with serious illnesses. While more work is needed to understand how to optimize support over time for different groups of parents (particularly those of children with nonmalignant disease), clinicians should work with all parents to develop strategies for addressing social support needs, particularly following an acute medical event.
Supplementary Material
Acknowledgments
We thank all parents who participated in this study. We also thank Dr. Jennifer Faerber for her guidance on the statistical analysis, and members of the University of Pennsylvania School of Nursing Palliative Care Scholars group for their review of this article.
Funding Information
Funding for this project was provided by the National Institute of Nursing Research grant 1R01NR012026.
Author Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. Carnevale FA, Alexander E, Davis M, et al. : Daily living with distress and enrichment: The moral experience of families with ventilator-assisted children at home. Pediatrics 2006;117:e48. [DOI] [PubMed] [Google Scholar]
- 2. Sullivan-Bolyai S, Sadler L, Knafl KA, et al. : Great expectations: A position description for parents as caregivers: Part I. Pediatr Nurs 2003;29:457–461 [PubMed] [Google Scholar]
- 3. Whiting M: Impact, meaning and need for help and support: The experience of parents caring for children with disabilities, life-limiting/life-threatening illness of technology dependence. J Child Health Care 2013;17:92–108 [DOI] [PubMed] [Google Scholar]
- 4. Eskola K, Bergstraesser E, Zimmermann K, et al. : Maintaining family life balance while facing a child's imminent death-A mixed methods study. J Adv Nurs 2017;73:2462–2472 [DOI] [PubMed] [Google Scholar]
- 5. Chen J, Clark MJ: Family function in families of children with Duchenne Muscular Dystrophy. Fam Community Health 2007;30:296–304 [DOI] [PubMed] [Google Scholar]
- 6. Kuster PA, Badr LK: Mental health of mothers caring for ventilator-assisted children at home. Issues Ment Health Nurs 2006;27:817–835 [DOI] [PubMed] [Google Scholar]
- 7. Leonard BJ, Brust JD, Nelson RP: Parental distress: Caring for medically fragile children at home. J Pediatr Nurs 1993;8:22–30 [PubMed] [Google Scholar]
- 8. Mastroyannopoulou K, Stallard P, Lewis M, et al. : The impact of childhood non-malignant life-threatening illness on parents: Gender differences and predictors of parental adjustment. J Child Psychol Psychiatry 1997;38:823–829 [DOI] [PubMed] [Google Scholar]
- 9. Miles MS, Holditch-davis D, Burchinal P, et al. : Distress and growth outcomes in mothers of medically fragile infants. Nurs Res 1999;48:129–140 [DOI] [PubMed] [Google Scholar]
- 10. Mooney-Doyle K, Deatrick JA: Parenting in the face of childhood life-threatening conditions: The ordinary in the context of the extraordinary. Palliat Support Care 2016;14:187–198 [DOI] [PubMed] [Google Scholar]
- 11. Patterson JM, Leonard BJ, Titus JC: Home care for medically fragile children: Impact on family health and well-being. J Dev Behav Pediatr 1992;13:248–255 [PubMed] [Google Scholar]
- 12. Rosenberg AR, Dussel V, Kang T, et al. : Psychological distress in parents of children with advanced cancer. JAMA Pediatr 2013;167:537–543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Siden H, Steele R: Charting the territory: Children and families living with progressive life-threatening conditions. Paediatr Child Health 2015;20:139–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sloper P: Predictors of distress in parents of children with cancer: A prospective study. J Pediatr Psychol 2000;25:79–91 [DOI] [PubMed] [Google Scholar]
- 15. Muscara F, McCarthy MC, Woolf C, et al. : Early psychological reactions in parents of children with a life threatening illness within a pediatric hospital setting. Eur Psychiatry 2015;30:555–561 [DOI] [PubMed] [Google Scholar]
- 16. Lakey B: Social Support and Social Integration: National Cancer Institute: Behavioral Research Program. https://cancercontrol.cancer.gov/brp/research/constructs/social_support.html, 2008. (last accessed September12, 2019)
- 17. Contro N, Davies B, Larson J, et al. : Away from home: Experiences of Mexican American families in pediatric palliative care. J Soc Work End Life Palliat Care 2010;6:185–204 [DOI] [PubMed] [Google Scholar]
- 18. Gage EA: The dynamics and processes of social support: Families' experiences coping with a serious paediatric illness. Sociol Health Illn 2013;35:405–418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nicholas DB, Beaune L, Barrera M, et al. : Examining the experiences of fathers of children with a life-limiting illness. J Soc Work End Life Palliat Care 2016;12:126–144 [DOI] [PubMed] [Google Scholar]
- 20. Robert R, Zhukovsky DS, Mauricio R, et al. : Bereaved parents' perspectives on pediatric palliative care. J Soc Work End Life Palliat Care 2012;8:316–338 [DOI] [PubMed] [Google Scholar]
- 21. Dockerty JD, Williams SM, McGee R, et al. : Impact of childhood cancer on the mental health of parents. Med Pediatr Oncol 2000;35:475–483 [DOI] [PubMed] [Google Scholar]
- 22. Katz S: When the child's illness is life threatening: Impact on the parents. Pediatr Nurs 2002;28:453–463 [PubMed] [Google Scholar]
- 23. Hoekstra-Weebers JE, Jaspers JP, Kamps WA, et al. : Psychological adaptation and social support of parents of pediatric cancer patients: A prospective longitudinal study. J Pediatr Psychol 2001;26:225–235 [DOI] [PubMed] [Google Scholar]
- 24. Wijnberg-Williams BJ, Kamps WA, Klip EC, et al. : Psychological distress and the impact of social support on fathers and mothers of pediatric cancer patients: Long-term prospective results. J Pediatr Psychol 2006;31:785–792 [DOI] [PubMed] [Google Scholar]
- 25. Rini C, Manne S, DuHamel K, et al. : Social support from family and friends as a buffer of low spousal support among mothers of critically ill children: A multilevel modeling approach. Health Psychol 2006;27:593–603 [DOI] [PubMed] [Google Scholar]
- 26. Monterosso L, Kristjanson LJ: Supportive and palliative care needs of families of children who die from cancer: An Australian study. Palliat Med 2008;22:59–69 [DOI] [PubMed] [Google Scholar]
- 27. Price J, Jordan J, Prior L, et al. : Comparing the needs of families of children dying from malignant and non-malignant disease: An in-depth qualitative study. BMJ Support Palliat Care 2012;2:127–132 [DOI] [PubMed] [Google Scholar]
- 28. Inglin S, Hornung R, Bergstraesser E: Palliative care for children and adolescents in Switzerland: A needs analysis across three diagnostic groups. Eur J Pediatr 2011;170:1031–1038 [DOI] [PubMed] [Google Scholar]
- 29. Gallagher S, Phillips AC, Oliver C, et al. : Predictors of psychological morbidity in parents of children with intellectual disabilities. J Pediatr Psychol 2008;33:1129–1136 [DOI] [PubMed] [Google Scholar]
- 30. Stremler R, Haddad S, Pullenayegum E, et al. : Psychological outcomes in parents of critically ill hospitalized children. J Pediatr Nurs 2017;34:36–43 [DOI] [PubMed] [Google Scholar]
- 31. Feudtner C, Walter JK, Faerber JA, et al. : Good-parent beliefs of parents of seriously ill children. JAMA Pediatr 2015;169:39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hill DL, Nathanson PG, Carroll KW, et al. : Changes in parental hopes for seriously ill children. Pediatrics 2018;141:e20173549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hill DL, Nathanson PG, Fenderson RM, et al. : Parental concordance regarding problems and hopes for seriously iIll children: A two-year cohort study. J Pain Symptom Manage 2017;53:911–918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mitchell AJ, Meader N, Symonds P: Diagnostic validity of the Hospital Anxiety and Depression Scale (HADS) in cancer and palliative settings: A meta-analysis. J Affect Disord 2010;126:335–348 [DOI] [PubMed] [Google Scholar]
- 35. Karadeniz Cerit K, Cerit C, Nart Ö, et al.: Post-traumatic stress disorder in mothers of children who have undergone cancer surgery. Pediatr Int 2017;59:996–1001 [DOI] [PubMed] [Google Scholar]
- 36. Besier T, Born A, Henrich G, et al. : Anxiety, depression, and life satisfaction in parents caring for children with cystic fibrosis. Pediatr Pulmonol 2011;46:672–682 [DOI] [PubMed] [Google Scholar]
- 37. Gough K, Hudson P: Psychometric properties of the Hospital Anxiety and Depression Scale in family caregivers of palliative care patients. J Pain Symptom Manage 2009;37:797–806 [DOI] [PubMed] [Google Scholar]
- 38. Hudson PL, Thomas K, Trauer T, et al. : Psychological and social profile of family caregivers on commencement of palliative care. J Pain Symptom Manage 2011;41:522–534 [DOI] [PubMed] [Google Scholar]
- 39. Hawkins WE, Tan PP, Hawkins MJ, et al. : Depressive symptomatology and specificity of social support. Psychol Rep 1999;84:1180–1186 [DOI] [PubMed] [Google Scholar]
- 40. Vangel Jr SJ, Rapport LJ, Hanks RA: Effects of family and caregiver psychosocial functioning on outcomes in persons with traumatic brain injury. J Head Trauma Rehabil 2011;26:20–29 [DOI] [PubMed] [Google Scholar]
- 41. Cutrona CE, Russell DW: Social Provisions Scale. https://www.coursehero.com/file/31839017/Social-provisions-scaledoc, 1987 (last accessed September12, 2019)
- 42. Baron RS, Cutrona CE, Hicklin D, et al. : Social support and immune function among spouses of cancer patients. J Pers Soc Psychol 1990;59:344–352 [DOI] [PubMed] [Google Scholar]
- 43. Russell DW, Cutrona CE: Social support, stress, and depressive symptoms among the elderly: Test of a process model. Psychol Aging 1991;6:190–201 [DOI] [PubMed] [Google Scholar]
- 44. Thurston S, Paul L, Loney P, et al. : Associations and costs of parental symptoms of psychiatric distress in a multi-diagnosis group of children with special needs. J Intellect Disabil Res 2011;55:263–280 [DOI] [PubMed] [Google Scholar]
- 45. Rosenbaum JL, Smith JR, Yan Y, et al. : Impact of a neonatal-bereavement-support DVD on parental grief: A randomized controlled trial. Death Stud 2015;39:191–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Weiss RS: The provisions of social relationships. In: Rubin Z. (ed): Doing Unto Others. Englewood Cliffs, NJ: Prentice-Hall, 1974, pp. 17–26 [Google Scholar]
- 47. Cutrona CE, Russell DW: The provisions of social relationships and adaptation to stress In: Jones WH, Perlman D (eds): Advances in Personal Relationships, Volume 1. Stamford, CT: JAI Press, 1982, pp. 37–67 [Google Scholar]
- 48. Grov EK, Fossa SD, Sorebo O, et al. : Primary caregivers of cancer patients in the palliative phase: A path analysis of variables influencing their burden. Soc Sci Med 2006;63:2429–2439 [DOI] [PubMed] [Google Scholar]
- 49. Chiu C, Moti R, Ditchman N: Validation of the Social Provisions Scale in people with multiple sclerosis. Rehabil Psychol 2016;61:297–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Green BL, Furrer C, McAllister C: How do relationships support parenting? Effects of attachment style and social support on parenting behavior in an at-risk population. Am J Community Psychol 2007;40:96–108 [DOI] [PubMed] [Google Scholar]
- 51. McLean AM, Jarus T, Hubley AM, et al. : Associations between social participation and subjective quality of life for adults with moderate to severe traumatic brain injury. Disabil Rehabil 2014;36:1409–1418 [DOI] [PubMed] [Google Scholar]
- 52. Ribas AC, Lam CS: Social support and quality of life among Latinos with mental illness. J Nerv Ment Dis 2010;198:137–143 [DOI] [PubMed] [Google Scholar]
- 53. Vogel DL, Wei M: Adult attachment and help-seeking intent: The mediating roles of psychological distress and perceived social support. J Couns Psychol 2005;52:347 [Google Scholar]
- 54. Casale M, Wild L, Cluver L, et al. : The relationship between social support and anxiety among caregivers of children in HIV-endemic South Africa. Psychol Health Med 2014;19:490–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lee PH: Is a cutoff of 10% appropriate for the change-in-estimate criterion of confounder identification? J Epidemiol 2014;24:161–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Vittinghoff E, Glidden DV, Shiboski SC, eds, et al.: Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models, 2nd ed. New York, NY: Springer, 2012 [Google Scholar]
- 57. StataCorp: Multiple-imputation reference manual. Stata Press, College Station, TX, 2017 [Google Scholar]
- 58. Allison P: Missing Data. Thousand Oaks, CA: Sage Publications, Inc., 2002 [Google Scholar]
- 59. Fielding S, Fayers P, Loge J, et al. : Methods for handling missing data in palliative care research. Palliat Med 2006;20:791–798 [DOI] [PubMed] [Google Scholar]
- 60. Fisher K, Seow H, Cohen J, et al. : Patient characteristics associated with prognostic awareness: A study of a Canadian palliative care population using the InterRAI Palliative Care Instrument. J Pain Symptom Manage 2015;49:716–725 [DOI] [PubMed] [Google Scholar]
- 61. Zimmermann C, Swami N, Krzyzanowska M, et al. : Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. Lancet 2014;383:1721–1730 [DOI] [PubMed] [Google Scholar]
- 62. Dahlquist LM, Czyzewski DI, Jones CL: Parents of children with cancer: A longitudinal study of emotional distress, coping style, and marital adjustment two and twenty months after diagnosis. J Pediatr Psychol 1996;21:541–554 [DOI] [PubMed] [Google Scholar]
- 63. Verberne LM, Kars MC, Schouten-van Meeteren AYN, et al. : Parental experiences and coping strategies when caring for a child receiving paediatric palliative care: A qualitative study. Eur J Pediatr 2019;178:1075–1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ulvick J, Spink K: Social provisions and young women's health-related physical activity. Women Health 2015;55:960–974 [DOI] [PubMed] [Google Scholar]
- 65. Grootenhuis MA, Last BF: Adjustment and coping by parents of children with cancer: A review of the literature. Support Care Cancer 1997;5:466–484 [DOI] [PubMed] [Google Scholar]
- 66. Manne S, Duhamel K, Redd WH: Association of psychological vulnerability factors to post-traumatic stress symptomatology in mothers of pediatric cancer survivors. Psychooncology 2000;9:372–384 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.