This cohort study examines the association between early contact with mental health services after an offense and reoffending in individuals with psychosis.
Key Points
Question
What is the association between early clinical contact with mental health services and reoffending after an index offense among individuals diagnosed with psychosis?
Findings
In this cohort study of 7030 offenders with psychosis, 2-year follow-up showed an association between increased contact with community mental health services within 30 days after an offense and reduced reoffending in male but not female offenders. Reoffending was associated with younger age and history of offense in male and female offenders, nonviolent offense type in male offenders, and being divorced, separated, widowed, or of unknown marital status in female offenders.
Meaning
These findings suggest that increased early contact with community mental health services after an offense may reduce the risk of reoffending in male offenders with severe mental illness; however, specific support may be needed for female offenders and those with less secure social relationships.
Abstract
Importance
Psychosis is a known risk factor for offending behavior, but little is known about the association between clinical contact with mental health services after an offense and reoffending.
Objective
To examine the association between early contact with mental health services and reoffending after an index offense in individuals with psychosis.
Design, Setting, and Participants
In this cohort study, individuals diagnosed with psychosis before their index offense from July 1, 2001, to December 31, 2012, and who received a noncustodial sentence were identified by linking health and offending databases in New South Wales, Australia. The incidence of and risk factors for reoffending and time to reoffending within 2 years from the index offense were examined using Cox proportional hazards regression and Kaplan-Meier survival estimates. Specifically, the association between contact with mental health services within 30 days after an offense and reoffending was examined. Data were analyzed from July 1, 2019, to March 5, 2020.
Exposures
Hospital admission, emergency department presentation, and contact with community mental health services associated with psychosis.
Main Outcomes and Measures
Reoffending within 2 years of the index offense was compared in individuals with and without clinical contact with mental health services within 30 days after an offense, with adjustment for potential confounders.
Results
Of the 7030 offenders with psychosis (4933 male [70.2%]; median age at the index offense, 34 [interquartile range, 26-42] years), 2605 (37.1%) had clinical contact with mental health services within 30 days after the index offense. The risk of reoffending was significantly lower in those with vs without clinical contact (adjusted hazard ratio [AHR], 0.83; 95% CI, 0.76-0.91). The risk of reoffending was 30% less in male offenders with 5 or more clinical contacts compared with male offenders with no clinical contact (AHR, 0.71; 95% CI, 0.59-0.84). Reoffending in both male and female offenders was associated with younger age (eg, AHR for male offenders aged <18 years, 3.31 [95% CI, 2.39-4.59]; AHR for female offenders aged <18 years, 2.60 [95% CI, 1.69-3.99]) and offending history (eg, AHR for male offenders with ≥4 prior offenses, 2.28 [95% CI, 1.98-2.64]; AHR for female offenders with ≥4 prior offenses, 2.22 [95% CI, 1.67-2.96]).
Conclusions and Relevance
In this cohort, early and frequent clinical contact with mental health services after an offense in individuals with psychosis was associated with reduced risk of reoffending in this group. More support may be needed for early treatment of those with serious mental illness who are at risk of reoffending.
Introduction
Offender populations are noted for the high numbers of individuals with mental illness, including serious mental illness, such as psychosis.1,2,3 The high costs of incarceration combined with its questionable rehabilitative and deterrent qualities have prompted moves to consider community-based alternatives for certain offender groups,4 including diversion into treatment for those with mental illness.5 Internationally, studies have found reduced rates of reoffending and other positive outcomes in those diverted by the courts into community-based mental health treatment.6,7,8 Albalawi et al9 recently reported the results of a population-based data-linkage study finding that reoffending was reduced in individuals with psychosis who received a treatment order from the local courts compared with those receiving punitive sanctions (eg, fines, community orders, bonds). Several studies have examined the effect of mandating contact with mental health services on reoffending as part of transitioning from prison to the community.10,11,12 In addition to these studies, psychotropic medication use has been shown to reduce violent and nonviolent offenses in individuals with psychosis.13,14,15
To our knowledge, no population-level study has examined the association between the frequency of contact with community mental health services beyond court-mandated treatments and offending behavior in those with psychosis. We herein examine the association between the frequency of clinical contact with community mental health services within 30 days after an offense and reoffending in the subsequent 2 years in individuals diagnosed with different types of psychosis in New South Wales (NSW), Australia. Early engagement with mental health services in those with serious mental illness may be important as a model of care for offenders to reduce the risk of reoffending and improve health and justice outcomes. A knowledge gap exists regarding whether the frequency of contact with community mental health services by offenders with psychosis has a role in reducing reoffending. We also examined the association between the characteristics of individuals with psychosis and reoffending and time to reoffending after the index offense.
Methods
In this cohort study, we used data from a population-based data-linkage study that examined the association between psychosis and offending behavior using administrative data collections in NSW. For the purpose of this report, offending is defined as a criminal charge that is proven in court. Ethics approvals were independently granted for the data linkage study from the NSW Population and Health Services Research Ethics Committee, NSW Aboriginal Health and Medical Research Council, Justice Health and Forensic Mental Health Network, and Corrective Services NSW. A waiver of consent for the linkage of study participants’ data was granted by the NSW Population and Health Services Research Ethics Committee. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Population
Our study included all individuals in NSW who were admitted to a hospital from July 1, 2001, to December 31, 2012, or who presented to an emergency department from January 1, 2005, to December 31, 2012, and received a diagnosis of psychosis before their index offense from July 1, 2001, to December 31, 2012, for which they received a noncustodial sentence (ie, not involving incarceration in an adult prison or a juvenile detention center) or no penalty. Psychosis cases were identified from the Admitted Patient Data Collection (APDC) and defined using codes from the International Classification of Diseases, Ninth Revision (ICD-9), and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), for schizophrenia and related psychoses (ICD-10 codes F20.0-F20.6, F20.8, F20.9, F22.0, F22.8, F22.9, F23.2, F23.3, F23.9, F25.0-F25.2, F25.9, and F29; ICD-9 code 295), affective psychoses (ICD-10 codes F30.2, F31.2, F31.5, F32.3, and F33.3; ICD-9 codes 296.8 and 296.9), and substance-related psychoses (ICD-10 codes F10.5, F13.5, F14.5, F15.5, F16.5, and F19.5; ICD-9 codes 291 and 292). Emergency department presentations for psychosis were recorded in the Emergency Department Data Collection (EDDC) using Systematized Nomenclature of Medicine–Clinical Terms (SNOMED-CT) codes and mapped to ICD-9 and ICD-10 codes. We applied a hierarchical approach to diagnosis in cases for which multiple diagnoses were recorded: any diagnosis of schizophrenia and related psychoses regardless of other types of psychoses, any diagnosis of affective psychoses without a diagnosis of schizophrenia and related psychoses, and any diagnosis of substance-related psychoses in the absence of a diagnosis of other types of psychoses.
Data Sources
Three health administrative data collections were used to identify mental health service contacts: the APDC, the EDDC, and the Mental Health Ambulatory Data Collection (MH-AMB). The APDC and EDDC were used to identify the study population.
The APDC data covered the period from July 1, 2001, to December 31, 2012, whereas EDDC data were available from January 1, 2005, to December 31, 2012. Six thousand two hundred twenty-one psychosis diagnoses (88.5%) were ascertained from the APDC. Any hospital admission time was discounted from the time at risk for the reoffending analysis. Mental health service contacts from the MH-AMB data collection covered the period from July 1, 2001, to December 31, 2014. We scrutinized the MH-AMB data collection to ensure that only those contacts of a clinical nature were included and removed codes relating to administrative matters such as opening and closing service requests, transporting and accompanying clients, and recording of missed appointments.
The NSW Bureau of Crime Statistics and Research’s Reoffending Database was used to identify dates for the index offense and reoffending during the study period in the cohort, the types of offenses, and prior offenses. The data from the Reoffending Database were available from July 1, 2001, to June 30, 2015. Mortality data were obtained from the NSW Registry of Births, Deaths and Marriages from July 1, 2001, to June 30, 2015, and enabled the removal of individuals who died during the study period.
Study Design
We defined an exposure window of 30 days from the date of the index offense during the study period for contact with a mental health service. We chose a 30-day window because this was the median time from the index offense to the first contact with mental health services during the study period. Those who had offended or died within 30 days of their index offense were excluded to avoid reverse causation.16,17 Reoffending was examined during a 2-year follow-up period after the 30-day window for contact with mental health services until study completion or death, whichever occurred first.
Statistical Analysis
Data were analyzed from July 1, 2019, to March 5, 2020. Descriptive statistics were used to summarize the characteristics of the study population at the time of the index offense (baseline) and clinical contact with mental health services during the follow-up period. Factors associated with reoffending during the follow-up period were examined for the whole cohort and separately for male and female offenders using Cox proportional hazards regression models. Potential confounders were included in the Cox proportional regression models to obtain adjusted hazard ratios (AHRs) for prior offenses, psychosis type, age group at the time of index offense, marital status, country of birth, indigenous status, and Socio-Economic Indices for Areas (SEIFA). SEIFA ranks geographic areas in Australia according to relative socioeconomic advantage and disadvantage using census data on income, educational attainment, employment, occupation, and housing.18 We examined the association between clinical contact with mental health services and the incidence of reoffending (second offense) during the follow-up period. Each individual in the cohort was followed up after the exposure window (30 days from the index offense) to the time to the second offense, death, or completion of the 2-year follow-up.
We examined time to reoffending in those who had mental health service contact and those who did not using Kaplan-Meier survival curves. We compared the median number of months from the index to the second offense in the clinical and nonclinical contact groups. Further, we compared the association between mental health service contact and time to reoffending in violent and nonviolent offenders. Sensitivity analysis was conducted to examine the association between contact with mental health services and reoffending by extending the exposure window to 90 days for contact with mental health services. Two-sided P < .05 indicated statistical significance.
Results
Characteristics of the Study Population
Of 7393 offenders with psychosis, 360 reoffended and 3 died within 30 days of their index offense and were excluded from the analysis, leaving 7030 individuals in the follow-up analysis (4933 male [70.2%] and 2097 female [29.8%]; median age at index offense, 34 [interquartile range (IQR), 26-42] years) (Table 1). More than two-thirds of the cohort (4750 [67.6%]) had a diagnosis of schizophrenia and related psychoses, followed by substance-related psychoses (1537 [21.9%]) and affective psychoses (743 [10.6%]). More male than female offenders were diagnosed with schizophrenia and related psychoses (3442 [69.8%] vs 1308 [62.4%]). Conversely, greater proportions of female than male offenders were diagnosed with substance-related psychoses (488 [23.3%] vs 1049 [21.3%]) and affective psychoses (301 [14.4%] vs 442 [9.0%]) (Table 1).
Table 1. Baseline Characteristics of the Study Population and Contact With Mental Health Services Within 30 Days From the Index Offense Date by Sex.
| Characteristic | Offender groupa | P value | ||
|---|---|---|---|---|
| All (n = 7030) | Male (n = 4933) | Female (n = 2097) | ||
| Age at the index offense, y | ||||
| Mean (SD) | 35.17 (11.59) | 35.18 (11.50) | 35.14 (11.82) | .92 |
| Median (IQR) | 34 (26-42) | 34 (27-42) | 34 (27-43) | |
| Age group at index offense, y | ||||
| <18 | 192 (2.7) | 105 (2.1) | 87 (4.1) | <.001 |
| 18-25 | 1347 (19.2) | 964 (19.5) | 383 (18.3) | |
| 26-35 | 2323 (33.0) | 1660 (33.7) | 663 (31.6) | |
| 36-45 | 1918 (27.3) | 1329 (26.9) | 589 (28.1) | |
| ≥46 | 1250 (17.8) | 875 (17.7) | 375 (17.9) | |
| Indigenous status | ||||
| No | 5429 (77.2) | 3916 (79.4) | 1513 (72.2) | <.001 |
| Yes | 464 (6.6) | 262 (5.3) | 202 (9.6) | |
| Unknown | 1137 (16.2) | 755 (15.3) | 382 (18.2) | |
| Marital status | ||||
| Married | 862 (12.3) | 506 (10.3) | 356 (17.0) | <.001 |
| Never married | 4054 (57.7) | 3012 (61.1) | 1042 (49.7) | |
| Other | 2114 (30.1) | 1415 (28.7) | 699 (33.3) | |
| Country of birth | ||||
| Other | 1109 (15.8) | 810 (16.4) | 299 (14.3) | .06 |
| Australia | 5050 (71.8) | 3525 (71.5) | 1525 (72.7) | |
| Unknown | 871 (12.4) | 598 (12.1) | 273 (13.0) | |
| SEIFA | ||||
| Advantaged (scores, 6-10) | 2750 (39.1) | 1957 (39.7) | 793 (37.8) | .15 |
| Disadvantaged (scores, 1-5) | 4280 (60.9) | 2976 (60.3) | 1304 (62.2) | |
| Type of psychosis | ||||
| Affective psychoses | 743 (10.6) | 442 (9.0) | 301 (14.4) | <.001 |
| Schizophrenia and related psychoses | 4750 (67.6) | 3442 (69.8) | 1308 (62.4) | |
| Substance-related psychoses | 1537 (21.9) | 1049 (21.3) | 488 (23.3) | |
| Type of the index offense | ||||
| Violent | 2722 (38.7) | 1908 (38.7) | 814 (39.0) | .91 |
| Nonviolent | 4308 (61.3) | 3025 (61.3) | 1283 (61.2) | |
| No. of prior offenses | ||||
| Mean (SD) | 1.31 (2.27) | 1.52 (2.41) | 0.83 (1.81) | <.001 |
| Median (IQR) | 0 (0-2) | 1 (0-2) | 0 (0-2) | |
| No. of prior offenses | ||||
| 0 | 3774 (53.7) | 2391 (48.5) | 1383 (66.0) | <.001 |
| 1-3 | 2416 (34.4) | 1836 (37.2) | 580 (27.7) | |
| ≥4 | 840 (11.9) | 706 (14.3) | 134 (6.4) | |
| Contact with mental health services within 30 d from the index offense date | ||||
| No | 4425 (62.9) | 3086 (62.6) | 1339 (63.9) | .30 |
| Yes | 2605 (37.1) | 1847 (37.4) | 758 (36.1) | |
| No. of contacts with mental health services within 30 d from the index offense date | ||||
| Mean (SD) | 1.61 (3.28) | 1.63 (3.30) | 1.56 (3.25) | .36 |
| Median (IQR) | 0 (0-2) | 0 (0-2) | 0 (0-2) | |
| No. of contacts with mental health services within 30 d from the index offense date | ||||
| 0 | 4425 (62.9) | 3086 (62.6) | 1339 (63.9) | .52 |
| 1-2 | 1150 (16.4) | 826 (16.7) | 324 (15.5) | |
| 3-4 | 570 (8.1) | 395 (8.0) | 175 (8.3) | |
| ≥5 | 885 (12.6) | 626 (12.7) | 259 (12.4) | |
Abbreviations: IQR, interquartile range; SEIFA, Socio-Economic Indices for Areas.
Unless otherwise indicated, data are expressed as number (percentage) of offenders. Percentages have been rounded and may not total 100.
Although most index offenses were nonviolent in nature (4308 [61.3%]) (Table 1), 2082 (29.6%) were violent acts intended to cause injury. Theft was the most frequent nonviolent index offense (861 [12.2%]). The proportions of violent and nonviolent index offenses were similar among male and female offenders.
Contact With Mental Health Services
A total of 2605 offenders (37.1%) had at least 1 mental health service contact within 30 days from their index offense (exposure window), with no significant difference between male and female offenders (Table 2). The median number of mental health service contacts within 30 days from the date of index offense was 0 (IQR, 0-2). Most (147 660 [95.3%]) clinical contacts during the follow-up occurred at community mental health services rather than hospital admissions (6763 [4.4%]) or emergency departments (496 [0.3%]). Our analysis showed that fewer individuals with substance-related psychoses (362 of 1537 [23.6%]) had mental health contacts compared with those with schizophrenia and related psychoses (1975 of 4750 [41.6%]) or affective psychoses (268 of 743 [36.1%]) within 30 days from the offense date. Contact with mental health services was associated with the type of offense, with more violent offenders having contact than nonviolent offenders (1176 of 2722 [43.2%] vs 1429 of 4308 [33.2%]). More of those with no clinical contact had offending histories than those with clinical contact (2183 of 4425 [49.3%] vs 1073 of 2605 [41.2%]). More individuals who were never married (1588 of 4054 [39.2%]) or had other marital status (ie, divorced, widowed, separated, or unknown; 746 of 2114 [35.3%]) had contact with mental health services than those who were married (271 of 862 [31.4%]) (Table 2).
Table 2. Baseline Characteristics of the Study Population by Contact With Mental Health Services Within 30 Days From the Index Offense Date.
| Characteristic | Offender groupa | P value | ||
|---|---|---|---|---|
| Overall (n = 7030) | ≥1 Contact (n = 2605) | No contact (n = 4425) | ||
| Sex | ||||
| Female | 2097 (30.0) | 758 (29.1) | 1339 (30.3) | .30 |
| Male | 4933 (70.0) | 1847 (70.9) | 3086 (69.7) | |
| Age at the index offense, y | ||||
| Mean (SD) | 35.17 (11.59) | 35.58 (11.70) | 34.93 (11.52) | .007 |
| Median (IQR) | 34 (26-42) | 34 (27-43) | 34 (26-42) | |
| Age at index offense, y | ||||
| <18 | 192 (2.7) | 89 (3.4) | 103 (2.3) | <.001 |
| 18-25 | 1347 (19.2) | 418 (16.0) | 929 (21.0) | |
| 26-35 | 2323 (33.0) | 871 (33.4) | 1452 (32.8) | |
| 36-45 | 1918 (27.3) | 731 (28.1) | 1187 (26.8) | |
| ≥46 | 1250 (17.8) | 496 (19.0) | 754 (17.0) | |
| Indigenous status | ||||
| No | 5429 (77.2) | 2055 (78.9) | 3374 (76.2) | .03 |
| Yes | 464 (6.6) | 164 (6.3) | 300 (6.8) | |
| Unknown | 1137 (16.2) | 386 (14.8) | 751 (17.0) | |
| Marital status | ||||
| Married | 862 (12.3) | 271 (10.4) | 591 (13.4) | <.001 |
| Never married | 4054 (57.7) | 1588 (61.0) | 2466 (55.7) | |
| Other | 2114 (30.1) | 746 (28.6) | 1368 (30.9) | |
| Country of birth | ||||
| Other | 1109 (15.8) | 423 (16.2) | 686 (15.5) | .05 |
| Australia | 5050 (71.8) | 1891 (72.6) | 3159 (71.4) | |
| Unknown | 871 (12.4) | 291 (11.2) | 580 (13.1) | |
| SEIFA | ||||
| Advantaged (scores, 6-10) | 2750 (39.1) | 1008 (38.7) | 1742 (39.4) | .58 |
| Disadvantaged (scores, 1-5) | 4280 (60.9) | 1597 (61.3) | 2683 (60.6) | |
| Type of psychosis | ||||
| Affective psychoses | 743 (10.6) | 268 (10.3) | 475 (10.7) | <.001 |
| Schizophrenia and related psychoses | 4750 (67.6) | 1975 (75.8) | 2775 (62.7) | |
| Substance-related psychoses | 1537 (21.9) | 362 (13.9) | 1175 (26.6) | |
| Type of index offense | ||||
| Nonviolent | 4308 (61.3) | 1429 (54.9) | 2879 (65.1) | <.001 |
| Violent | 2722 (38.7) | 1176 (45.1) | 1546 (34.9) | |
| No. of prior offenses | ||||
| Mean (SD) | 1.31 (2.27) | 1.09 (2.10) | 1.44 (2.35) | <.001 |
| Median (IQR) | 0 (0-2) | 0 (0-1) | 0 (0-2) | |
| No. of prior offenses | ||||
| 0 | 3774 (53.7) | 1532 (58.8) | 2242 (50.7) | <.001 |
| 1-3 | 2416 (34.4) | 835 (32.1) | 1581 (35.7) | |
| ≥4 | 840 (11.9) | 238 (9.1) | 602 (13.6) | |
Abbreviations: IQR, interquartile range; SEIFA, Socio-Economic Indices for Areas.
Unless otherwise indicated, data are expressed as number (percentage) of offenders. Percentages have been rounded and may not total 100.
Reoffending Rate
More than one-quarter of the cohort (2002 [28.5%]) reoffended during the 2 years of follow-up, with more than two-thirds of reoffenses (1337 [66.8%]) being nonviolent. Similar to the index offense type, the most common second offenses were acts intended to cause injury (464 [23.2%]). The most frequent nonviolent offenses were those against justice procedures, government security, and government operations (352 [17.6%]) (eg, breach of a community-based order, offenses against government operations/security). The likelihood of reoffending was the same for males and females during the follow-up period (AHR, 0.98; 95% CI, 0.89-1.09) (Table 3).
Table 3. Risk for Reoffending of the Study Population During the 2-Year Follow-up Perioda.
| Characteristic | Offender group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| All (n = 2002) | Male (n = 1437) | Female (n = 565) | |||||||
| Reoffending, No. (%) | AHR (95% CI) | P value | Reoffending, No. (%) | AHR (95% CI) | P value | Reoffending, No. (%) | AHR (95% CI) | P value | |
| Sex | |||||||||
| Female | 565 (28.2) | 1 [Reference] | NA | NA | NA | NA | NA | NA | NA |
| Male | 1437 (71.8) | 0.98 (0.89-1.09) | .73 | NA | NA | NA | NA | NA | NA |
| Age at index offense, y | |||||||||
| <18 | 83 (4.1) | 2.99 (2.31-3.88) | <.001 | 50 (3.5) | 3.31 (2.39-4.59) | <.001 | 33 (5.8) | 2.60 (1.69-3.99) | <.001 |
| 18-25 | 453 (22.6) | 1.89 (1.60-2.22) | <.001 | 331 (23.0) | 1.95 (1.61-2.37) | <.001 | 122 (21.6) | 1.76 (1.29-2.39) | <.001 |
| 26-35 | 759 (37.9) | 1.59 (1.37-1.85) | <.001 | 553 (38.5) | 1.64 (1.38-1.96) | <.001 | 206 (36.5) | 1.51 (1.15-1.99) | .003 |
| 36-45 | 461 (23.0) | 1.14 (0.97-1.33) | .10 | 331 (23.0) | 1.18 (0.98-1.42) | .08 | 130 (23.0) | 1.06 (0.79-1.41) | .71 |
| ≥46 | 246 (12.3) | 1 [Reference] | NA | 172 (12.0) | 1 [Reference] | NA | 74 (13.1) | 1 [Reference] | NA |
| Indigenous status | |||||||||
| No | 1593 (79.6) | 1 [Reference] | NA | 1178 (82.0) | 1 [Reference] | NA | 415 (73.5) | 1 [Reference] | NA |
| Yes | 151 (7.5) | 0.96 (0.81-1.13) | .61 | 86 (6.0) | 0.92 (0.74-1.15) | .46 | 65 (11.5) | 0.99 (0.76-1.3) | .96 |
| Unknown | 258 (12.9) | 0.74 (0.65-0.84) | <.001 | 173 (12.0) | 0.71 (0.61-0.84) | <.001 | 85 (15.0) | 0.8 (0.64-1.02) | .07 |
| Marital status | |||||||||
| Married | 186 (9.3) | 1 [Reference] | NA | 114 (7.9) | 1 [Reference] | NA | 72 (12.7) | 1 [Reference] | NA |
| Never married | 1221 (61.0) | 1.21 (1.03-1.42) | .02 | 921 (64.1) | 1.17 (0.96-1.43) | .12 | 300 (53.1) | 1.27 (0.97-1.65) | .08 |
| Other | 595 (29.7) | 1.28 (1.07-1.54) | .006 | 402 (28.0) | 1.20 (0.96-1.50) | .11 | 193 (34.2) | 1.48 (1.10-1.98) | .01 |
| Country of birth | |||||||||
| Other | 286 (14.3) | 1 [Reference] | NA | 221 (15.4) | 1 [Reference] | NA | 65 (11.5) | 1 [Reference] | NA |
| Australia | 1460 (72.9) | 1.01 (0.89-1.15) | .88 | 1037 (72.2) | 0.96 (0.83-1.12) | .64 | 423 (74.9) | 1.14 (0.87-1.5) | .33 |
| Unknown | 256 (12.8) | 0.98 (0.8-1.18) | .80 | 179 (12.5) | 0.99 (0.79-1.24) | .94 | 77 (13.6) | 0.97 (0.67-1.41) | .88 |
| SEIFA | |||||||||
| Advantaged (scores, 6-10) | 759 (37.9) | 1 [Reference] | NA | 557 (38.8) | 1 [Reference] | NA | 202 (35.8) | 1 [Reference] | NA |
| Disadvantaged (scores, 1-5) | 1243 (62.1) | 1.03 (0.94-1.13) | .56 | 880 (61.2) | 1.01 (0.91-1.13) | .82 | 363 (64.2) | 1.07 (0.9-1.27) | .46 |
| Type of psychosis | |||||||||
| Affective psychoses | 177 (8.8) | 1 [Reference] | NA | 112 (7.8) | 1 [Reference] | NA | 65 (11.5) | 1 [Reference] | NA |
| Schizophrenia and related psychoses | 1337 (66.8) | 1.13 (0.96-1.32) | .14 | 982 (68.3) | 1.07 (0.88-1.31) | .48 | 355 (62.8) | 1.23 (0.94-1.61) | .13 |
| Substance-related psychoses | 488 (24.4) | 1.21 (1.01-1.44) | .04 | 343 (23.9) | 1.19 (0.95-1.48) | .13 | 145 (25.7) | 1.20 (0.88-1.64) | .24 |
| Type of the first offense | |||||||||
| Violent | 665 (33.2) | 1 [Reference] | NA | 469 (32.6) | 1 [Reference] | NA | 196 (34.7) | 1 [Reference] | NA |
| Nonviolent | 1337 (66.8) | 1.27 (1.16-1.39) | <.001 | 968 (67.3) | 1.30 (1.17-1.46) | <.001 | 369 (65.3) | 1.19 (0.99-1.41) | .06 |
| No. of prior offenses | |||||||||
| 0 | 887 (44.3) | 1 [Reference] | NA | 576 (40.1) | 1 [Reference] | NA | 311 (55.0) | 1 [Reference] | NA |
| 1-3 | 739 (36.9) | 1.45 (1.31-1.60) | <.001 | 544 (37.9) | 1.37 (1.21-1.55) | <.001 | 195 (34.5) | 1.66 (1.38-2.00) | <.001 |
| ≥4 | 376 (18.8) | 2.29 (2.02-2.61) | <.001 | 317 (22.1) | 2.28 (1.98-2.64) | <.001 | 59 (10.4) | 2.22 (1.67-2.96) | <.001 |
| Contact with mental health services within 30 d from the first offense date | |||||||||
| No | 1349 (67.4) | 1 [Reference] | NA | 979 (68.1) | 1 [Reference] | NA | 370 (65.5) | 1 [Reference] | NA |
| Yes | 653 (32.6) | 0.83 (0.76-0.91) | <.001 | 458 (31.9) | 0.78 (0.69-0.87) | <.001 | 195 (34.5) | 1.00 (0.84-1.19) | .99 |
| No. of contacts with mental health services | |||||||||
| 0 | 1349 (67.4) | 1 [Reference] | NA | 979 (68.1) | 1 [Reference] | NA | 370 (65.5) | 1 [Reference] | NA |
| 1-2 | 313 (15.6) | 0.90 (0.79-1.01) | .08 | 222 (15.4) | 0.84 (0.72-0.97) | .02 | 91 (16.1) | 1.09 (0.87-1.38) | .44 |
| 3-4 | 132 (6.6) | 0.77 (0.64-0.92) | .004 | 95 (6.6) | 0.76 (0.61-0.94) | .01 | 37 (6.5) | 0.80 (0.57-1.13) | .20 |
| ≥5 | 208 (10.4) | 0.79 (0.68-0.91) | .001 | 141 (9.8) | 0.71 (0.59-0.84) | <.001 | 67 (11.9) | 1.02 (0.78-1.32) | .91 |
Abbreviations: AHR, adjusted hazard ratio; NA, not applicable; SEIFA, Socio-Economic Indices for Areas.
Adjusted by sex (total only), age at the first offense, marital status, country of birth, indigenous status, SEIFA, psychosis type, and number of prior offenses. Percentages have been rounded and may not total 100.
For the total cohort, the risk of reoffending was significantly lower in individuals with vs without clinical contact (AHR, 0.83; 95% CI, 0.76-0.91). The interaction between contact with mental health services and sex was statistically significant (AHR, 0.77; 95% CI, 0.63-0.95; P = .02). We found a linear decreasing trend between the number of clinical contacts with mental health services and the risk of reoffending in male offenders (AHR for 1-2 contacts, 0.84 [95% CI, 0.72-0.97]; AHR for 3-4 contacts, 0.76 [95% CI, 0.61-0.94). Reoffending was about 30% less frequent in male offenders who had 5 or more contacts with mental health services within 30 days from index offense compared with those who had no clinical contact (AHR, 0.71; 95% CI, 0.59-0.84). Contact with mental health services was not associated with reoffending in female offenders (Table 3). Incidence of reoffending in male offenders with clinical contact was 1.27 per 100 person-years (95% CI, 11.16-1.39); and in male offenders with no clinical contact, 1.70 per 100 person-years (95% CI, 1.59-1.81). In female offenders, the incidence of reoffending was 1.32 per 100 person-years (95% CI, 1.15-1.52) for those in the clinical contact group and 1.42 per 100 person-years (95% CI, 1.28-1.57) for those with no clinical contact.
Risk Factors Associated With Reoffending in Male and Female Offenders
Younger age was associated with reoffending in both male (eg, AHR for <18 years, 3.31; 95% CI, 2.39-4.59) and female (eg, AHR for <18 years, 2.60; 95% CI, 1.69-3.99) offenders (Table 3). Female offenders who were divorced, separated, or widowed or who had unknown marital status at the time of their index offense were at a higher risk of reoffending than married women (AHR, 1.48; 95% CI, 1.10-1.98) (Table 3). There was a linear association between the number of prior offenses (outside the study period) and reoffending in both male and female offenders. The risk of reoffending was more than doubled in male (AHR, 2.28; 95% CI, 1.98-2.64) and female (ARH, 2.22; 95% CI, 1.67-2.96) offenders with 4 or more prior offenses compared with those with no offenses prior to the study period. The risk of reoffending was significantly higher for male offenders with nonviolent compared with violent offenses (AHR, 1.30; 95% CI, 1.17-1.46) (Table 3).
Time to Reoffending
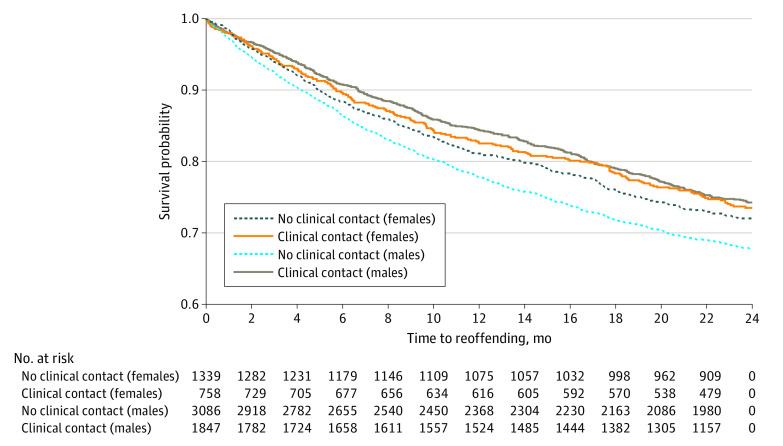
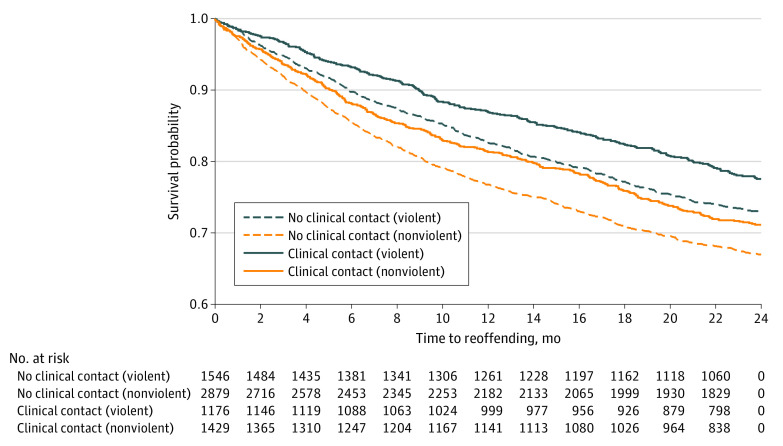
Time to reoffending after the index offense was examined using Kaplan-Meier survival analysis (Figure 1). Median time to reoffending was significantly longer for male offenders with clinical contact within 30 days from the index offense (8.89 [IQR, 4.04-16.04] months) than for those with no clinical contact (7.33 [IQR, 3.16-13.55] months) (P < .001). There was no significant difference between the median time to reoffending for female offenders who had clinical contact (7.92 [IQR, 3.29-15.22] months) and those who did not (7.74 [IQR, 3.52-14.86] months) (P = .40). Median time to reoffending was longer for violent offenders who had clinical contact during the follow-up (9.53 [IQR, 4.37-16.60] months) vs violent offenders with no clinical contact (8.52 [IQR, 3.78-14.99] months). Similarly, median time to reoffending was longer for nonviolent offenders who had clinical contact for mental health treatment (7.46 [IQR, 3.35-15.58] months) vs nonviolent offenders with no clinical contact with health services (6.92 [IQR, 3.06-13.35] months) (Figure 2).
Figure 1. Kaplan-Meier Plot of Time to Reoffending in 2-Year Follow-up for Those With and Without Contact With Mental Health Services Within 30 Days From the Index Offense by Sex.
Median time to reoffending in the 2 years among males with clinical contact within 30 days from the index offense was 8.89 (interquartile range [IQR], 4.04-16.04]) months; among males with no clinical contact, 7.33 (IQR, 3.16-13.55) months (P < .001, log-rank test). Median time to reoffending in the 2 years among females with clinical contact within 30 days of the index offense was 7.92 (IQR, 3.29-15.22) months; among females with no clinical contact, 7.74 (IQR, 3.52-14.86) months (P = .40, log-rank test).
Figure 2. Kaplan-Meier Plot of Time to Reoffending in 2-Year Follow-up for Those With and Without Contact With Mental Health Services Within 30 Days From the Index Offense by Type of Offense.
Median time to reoffending in the 2 years among individuals with nonviolent offenses with clinical contact within 30 days from the index offense was 7.46 (interquartile range [IQR], 3.35-15.58) months; among those without clinical contact, 6.92 (IQR, 3.06-13.35) months (P = .003, log-rank test). Median time to reoffending in the 2 years among individuals with violent offenses and clinical contact within 30 days of the index offense was 9.53 (IQR, 4.37-16.60) months; among those without clinical contact, 8.52 (IQR, 3.78-14.99) months (P = .003, log-rank test).
Sensitivity Analysis
The exposure window for contact with mental health services was extended from 30 days to 90 days from the offense date, which confirmed that the association between contact with mental health services and reoffending was significant only in male offenders within 2 years of follow-up. The risk of reoffending in this period was 11% less for male offenders who had contact with mental health services from the index offense (AHR, 0.89; 95% CI, 0.79-0.99). However, the risk for reoffending was not different for female offenders with and without contact with mental health services within 90 days after the index offense (AHR, 1.14; 95% CI, 0.95-1.36).
Discussion
In this cohort study, contact with mental health services within 30 days after an offense was associated with reduced reoffending in male offenders in the subsequent 2 years, with a linear trend between increased treatment contact and reduced reoffending. No such association was found in female offenders. Reoffending in the 2-year follow up was approximately 30% less in male offenders who had 5 or more clinical contacts than in those with no clinical contact. Similarly, time to reoffending was significantly longer in male, but not female, offenders with clinical contact within 30 days from index offense compared with those with no clinical contact. These findings were confirmed in sensitivity analysis by extending the treatment exposure window for clinical contact with mental health services from 30 to 90 days.
The association between clinical contact and reduced reoffending in male offenders may reflect greater emphasis by mental health services on minimizing harm to the community inflicted by males who are violent. Our findings indicate that offending, particularly violent offending, is more frequent in males with psychosis than females.
Female offenders who were married were less likely to reoffend than those who were widowed, divorced, or separated or had unknown relationship status, suggesting that being in a stable relationship may be protective. These results suggest the need for enhanced mental health services for female offenders at risk of reoffending and supportive social and occupational management for this group.19
Our study is unique in following up a large population of offenders with psychosis who did not receive a custodial sentence and thus are at risk of reoffending. We applied a conservative approach to examine the effect size of the association between clinical contact with mental health services and reoffending by examining clinical contact only during the 30 days after an offense (exposure window). Those who offended within 30 days from the index offense were excluded from the study to avoid reverse causation.
Despite previous studies that examined the effect of court diversion5,6,7,9,20,21,22 or postprison mental health transition programs10,11,12 on reoffending for those with psychosis, our study did not target any specific mental health program aimed at offenders but examined early contact with mainstream community mental health services. However, the present study enhances this previous work showing the importance of treatment for those with serious mental illness (psychosis) in the offending conundrum.9
Strengths and Limitations
One strength of the current design was the determination of clinical contact with community mental health services, which accounted for more than 95% of all contacts of the cohort within 30 days from offending. This was achieved by scrutinizing the service contact reasons and removing those associated with administrative and bureaucratic matters. One limitation of the design is that we could not examine the type of treatment received. Because previous studies have shown a positive association between antipsychotic medication use and reduced reoffending,13,14,15,23,24,25 future work could examine the effects of both mental health service contact and medication on reoffending. This would enhance our knowledge about the type of support needed to reduce offending in women and groups at high risk.
Our study design varied from previous work examining risk factors for reoffending in individuals with serious mental illness that used control groups with no mental illness or other types of mental illness.26,27 Some studies with small sample sizes examined the effects of community mental health interventions by comparing the treatment and nontreatment groups.10,12,28,29 We also compared the risk of and time to reoffending in the groups with and without clinical contact after adjusting for the confounding effects of demographic characteristics, offending history, and the type of psychosis.
We acknowledge the limitations of the data because the periods for extraction of diagnostic data from APDC and EDDC were not the same. Individuals diagnosed and receiving treatment by general clinicians or private psychiatrists were not included in the cohort. However, this number is likely to be small.
Conclusions
This study suggests an association between early engagement and frequent use of community mental health services in a short term (30 days) after an offense and reduced offending behavior in those with psychosis. Disappointingly, this association was found only in male offenders and not female offenders. This suggests that greater attention should be paid to the treatment needs of female offenders with psychosis in the justice system. We found that use of mental health services was lower in individuals with offending histories, suggesting that this group may require greater access to mental health services. Further work is needed to support early treatment and diverting those with psychosis into treatment.
References
- 1.Fazel S, Grann M. The population impact of severe mental illness on violent crime. Am J Psychiatry. 2006;163(8):1397-1403. doi: 10.1176/ajp.2006.163.8.1397 [DOI] [PubMed] [Google Scholar]
- 2.Butler T, Andrews G, Allnutt S, Sakashita C, Smith NE, Basson J. Mental disorders in Australian prisoners: a comparison with a community sample. Aust N Z J Psychiatry. 2006;40(3):272-276. doi: 10.1080/j.1440-1614.2006.01785.x [DOI] [PubMed] [Google Scholar]
- 3.Steadman HJ, Osher FC, Robbins PC, Case B, Samuels S. Prevalence of serious mental illness among jail inmates. Psychiatr Serv. 2009;60(6):761-765. doi: 10.1176/ps.2009.60.6.761 [DOI] [PubMed] [Google Scholar]
- 4.Weatherburn D. The effect of prison on adult re-offending. Crime and Justice Bulletin. August 2010; No. 143. Accessed July 15, 2019. https://www.bocsar.nsw.gov.au/Documents/CJB/cjb143.pdf
- 5.Davidson F, Heffernan E, Greenberg D, Butler T, Burgess P. A critical review of mental health court liaison services in Australia: a first national survey. Psychiatry Psychol Law. 2016;23(6):908-921. doi: 10.1080/13218719.2016.1155509 [DOI] [Google Scholar]
- 6.Steadman HJ, Naples M. Assessing the effectiveness of jail diversion programs for persons with serious mental illness and co-occurring substance use disorders. Behav Sci Law. 2005;23(2):163-170. doi: 10.1002/bsl.640 [DOI] [PubMed] [Google Scholar]
- 7.McNiel DE, Binder RL. Effectiveness of a mental health court in reducing criminal recidivism and violence. Am J Psychiatry. 2007;164(9):1395-1403. doi: 10.1176/appi.ajp.2007.06101664 [DOI] [PubMed] [Google Scholar]
- 8.Canada K, Barrenger S, Ray B. Bridging mental health and criminal justice systems: a systematic review of the impact of mental health courts on individuals and communities. Psychol Public Policy Law. 2019;25(2):73-91. doi: 10.1037/law0000194 [DOI] [Google Scholar]
- 9.Albalawi O, Chowdhury NZ, Wand H, et al. Court diversion for those with psychosis and its impact on re-offending rates: results from a longitudinal data-linkage study. BJPsych Open. 2019;5(1):e9. doi: 10.1192/bjo.2018.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stewart LA, Farrell-MacDonald S, Feeley S. The impact of a community mental health initiative on outcomes for offenders with a serious mental disorder. Crim Behav Ment Health. 2017;27(4):371-384. doi: 10.1002/cbm.2005 [DOI] [PubMed] [Google Scholar]
- 11.Martin ML. Effectiveness of mental health follow-up on recidivism of psychiatrically diagnosed released inmates. Dissertation Abstracts International: Section B: the Sciences and Engineering. 2017;77(8-B[E]). Published March 2016. Accessed July 9, 2019. https://search.proquest.com/openview/8dda9ea7d36450df6da3b5aa79f5b613/1.pdf?pq-origsite=gscholar&cbl=18750&diss=y
- 12.Morrissey JP, Domino ME, Cuddeback GS. Expedited Medicaid enrollment, mental health service use, and criminal recidivism among released prisoners with severe mental illness. Psychiatr Serv. 2016;67(8):842-849. doi: 10.1176/appi.ps.201500305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fazel S, Zetterqvist J, Larsson H, Långström N, Lichtenstein P. Antipsychotics, mood stabilisers, and risk of violent crime. Lancet. 2014;384(9949):1206-1214. doi: 10.1016/S0140-6736(14)60379-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rezansoff SN, Moniruzzaman A, Fazel S, McCandless L, Somers JM. Adherence to antipsychotic medication and criminal recidivism in a Canadian provincial offender population. Schizophr Bull. 2017;43(5):1002-1010. doi: 10.1093/schbul/sbx084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohr P, Knytl P, Voráčková V, Bravermanová A, Melicher T. Long-acting injectable antipsychotics for prevention and management of violent behaviour in psychotic patients. Int J Clin Pract. 2017;71(9):e12997. doi: 10.1111/ijcp.12997 [DOI] [PubMed] [Google Scholar]
- 16.Sattar N, Preiss D. Reverse causality in cardiovascular epidemiological research: more common than imagined? Circulation. 2017;135(24):2369-2372. doi: 10.1161/CIRCULATIONAHA.117.028307 [DOI] [PubMed] [Google Scholar]
- 17.Ioannidis JPA. Why most discovered true associations are inflated. Epidemiology. 2008;19(5):640-648. doi: 10.1097/EDE.0b013e31818131e7 [DOI] [PubMed] [Google Scholar]
- 18.Australian Bureau of Statistics Socio-Economic Indexes for Areas (SEIFA). Updated March 17, 2018. Accessed January 16, 2018. https://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa
- 19.Mullen PE. Schizophrenia and violence: from correlations to preventive strategies. Adv Psychiatr Treat. 2006;12(4):239-248. doi: 10.1192/apt.12.4.239 [DOI] [Google Scholar]
- 20.Bradford D, Smith N. An Evaluation of the NSW Court Liaison Services. NSW Bureau of Crime Statistics and Research; 2009. [Google Scholar]
- 21.Skrzpiec G, Wundersits J, McRostie H. Magistrates Court Diversion Program: An Analysis of Post-Program Offending. Office of Crime Statistics and Research; 2004. [Google Scholar]
- 22.Newitt E, Stojcevski V. Mental Health Diversion List: Evaluation Report. Magistrates Court Tasmania; 2009. [Google Scholar]
- 23.Baruch N, Das M, Sharda A, et al. An evaluation of the use of olanzapine pamoate depot injection in seriously violent men with schizophrenia in a UK high-security hospital. Ther Adv Psychopharm. 2014;4(5):186-192. doi: 10.1177/2045125314531982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mortlock AM, Larkin F, Ross CC, Gupta N, Sengupta S, Das M Effectiveness of paliperidone depot injection in seriously violent men with comorbid schizophrenia and dissocial personality disorder in a UK high-security hospital. Ther Adv Psychopharm. 2017;7(5):169-179. doi: 10.1177/2045125317693513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kasinathan J, Sharp G, Barker A Evaluation of olanzapine pamoate depot in seriously violent males with schizophrenia in the community. Ther Adv Psychopharm. 2016;6(5):301-307. doi: 10.1177/2045125316656319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fazel S, Yu R. Psychotic disorders and repeat offending: systematic review and meta-analysis. Schizophr Bull. 2011;37(4):800-810. doi: 10.1093/schbul/sbp135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonta J, Law M, Hanson K. The prediction of criminal and violent recidivism among mentally disordered offenders: a meta-analysis. Psychol Bull. 1998;123(2):123-142. doi: 10.1037/0033-2909.123.2.123 [DOI] [PubMed] [Google Scholar]
- 28.Harris V, Koepsell TD. Criminal recidivism in mentally ill offenders: a pilot study. Bull Am Acad Psychiatry Law. 1996;24(2):177-186. [PubMed] [Google Scholar]
- 29.Harris GT, Rice ME, Quinsey VL. Violent recidivism of mentally disordered offenders: the development of a statistical prediction instrument. Crim Justice Behav. 1993;20(4):315-335. doi: 10.1177/0093854893020004001 [DOI] [Google Scholar]