Abstract
Purpose
The SARS-CoV-2 epidemic started in December 2019 in Wuhan. The lockdown was declared on March 16, 2020 in France. Our centre had to adapt daily practices to continue to take care of bone and soft tissue tumours and emergencies. Through this study, we wanted to assess the various procedures implemented during the lockdown period between March 17 and May 10.
Methods
A monocentric retrospective cohort study was conducted in Cochin Hospital (Paris, France). Patients included were those who had surgery during the lockdown period. To take care of COVID-19 positive and negative patients, various procedures have been set up: reverse transcriptase polymerase chain reaction (RT-PCR) tests for all hospitalized patients, a specific unit for COVID-positive patients, a specific surgical room, and use of protective personal equipment.
To allow the effectiveness of the procedures implemented, we evaluated the number of complications attributed to SARS-CoV-2 and the number of patients who became COVID positive during hospitalization.
Results
During the lockdown period, there were 199 procedures of three types of procedures in our centre: 79 traumatology procedures (39.7%), 76 of bone and soft tissues tumours (38.2%), and 44 procedures related to infection (22.1%). We observed 13 complications (6.5%) during hospitalization, and only one patient became COVID-19 positive during the hospitalization.
Conclusion
The COVID-19 epidemic has been a challenge for organization and adaptation to manage all COVID-19 positive and COVID negative. Through this study, we wanted to assess our procedures taken. They had been effective due to the low number of contamination and complications.
Keywords: COVID-19, Orthopedic department, Traumatology, Bone tumor
Introduction
In December 2019, in Wuhan, Hubei Province, China, the outbreak of coronavirus disease 2019 (COVID-19) started caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2). This respiratory virus can be responsible for severe pneumonia: 15% of affected patients are hospitalized and 5% require hospitalization in intensive care [1].
The number of cases increased very quickly, and the spread of the virus was made all over the world in a few months: December in Asia and January in Europe and in the USA [2].
On March 11, because of its severity and its high contagiousness, the World Health Organization (WHO) declared COVID-19 outbreak as a pandemic [3].
The influx of patients and the high number of serious patients have developed into an unprecedented pandemic with enormous pressure on healthcare providers around the world. To try to control this pandemic, many countries decided to impose a lockdown period. France was one of the most affected countries in Europe with 161,267 individuals infected and 29,720 deaths (as of June 24) [4]. The confinement was declared on March 14, 2020 until May 15, 2020 to reduce contact rates in the population [5].
Paris and its region (Ile de France) being an epidemic spot, the white plan was launched on March 6, 2020. All elective surgery had to be stopped in order to decrease the influx of patients into hospitals and to redeploy medical and paramedical staff in different units to provide assistance in emergency departments, COVID-19 units, and intensive care units [6].
Only emergencies surgery was allowed.
Our centre, in Paris, is a teaching tertiary referral centre where we perform traumatology, bone and soft tissue tumours, along with elective orthopaedic procedures, including about 1000/year hip and knee arthroplasties. This facility has participated in the war against the COVID by continuing to perform urgent procedures during the pandemic, including trauma surgery in COVID-positive patients. A restructuration and a new organization of the orthopaedics unit had to be put in place in order to treat COVID-negative and COVID-positive patients.
The purpose of this retrospective study was to assess the effectiveness of the guidelines implemented in our orthopaedic and trauma centre, Cochin Hospital, during the lockdown imposed in France period between March 15 and May 11, 2020.
Patients and methods
Patients
This monocentric retrospective cohort study was conducted in Cochin Hospital (France). Patients included were those who had surgery during the lockdown period, between March 17 and May 10 in our department. Patients under 15 years old were excluded of the study.
Procedure
Our department is an orthopaedic and trauma centre. We continued performing traumatology and bone and soft tissue tumours during this period. Cochin Hospital received COVID-positive patients through emergency room. We therefore had to set up protocols and reorganize the department to take care of both COVID-positive patients and COVID-negative patients.
A specific unit was created, isolated from the others for COVID-positive patient. Medical and paramedical personnel have been trained and assigned to this unit in order to care for COVID-positive patients. The protective personal equipment measure, including over-blouse, glasses, and mask, were respected. A short circuit for COVID-positive patients has been created, and a COVID-positive operating room was available. Reverse transcriptase polymerase chain reaction (RT-PCR) tests were available to diagnose suspicious COVID-positive patients. All trauma patients had a RT-PCR before being hospitalized. Waiting their RT-PCR results, they were hospitalized in a specific zone where all protective procedures were applied. Visits were prohibited.
Data collection
We included data of all patients operated on in orthopaedics between March 17 and May 11 in our surgery department. We collected, before surgery, demographic data (age, body mass index, gender), date of admission, reason for admission to our department, the presence of risk factors for COVID (hypertension, diabetes mellitus, heart disease, lung disease, kidney disease, evolutive neoplasia, inflammatory disease), temperature and saturation, their COVID status, and if a RT-PCR was made. Post-operatively, we collected the date of surgery, the occupancy time of the operating room, complications, length of stay, COVID status at discharge, and discharge to another department or at home. Patients were reviewed between four and six weeks post-operatively to evaluate whether complications had occurred and their COVID status.
Outcomes
Our primary endpoint was to assess the effectiveness of the procedures implemented for COVID outbreak in our centre for patients operated on during the lockdown period. To allow the effectiveness, we evaluated the number of complications attributed to SARS-CoV-2 and the number of patients who became COVID-positive during hospitalization.
Our secondary criteria were to compare medical care between COVID-positive and COVID-negative patients for trauma and for bone and soft tissue tumour care. We evaluated the rate of complications during hospitalization and at six weeks, the occupancy time of the operating room, and the length of stay in each of the two groups.
Statistics
Continuous quantitative variables were described by mean and standard error (SD). A Wilcoxon test was used to compare the continuous variables with each other. Dichotomous variables were described by their number of events and their percentage. A Fischer test was used to compare the dichotomous variables. The threshold of significance retained was 5% for a power of 80% and a risk of the first species at 5%. All tests were two-sided. The R software (version 3.5.0) was used to perform the statistical analyses (https://www.r-project.org/).
Results
Demographic data
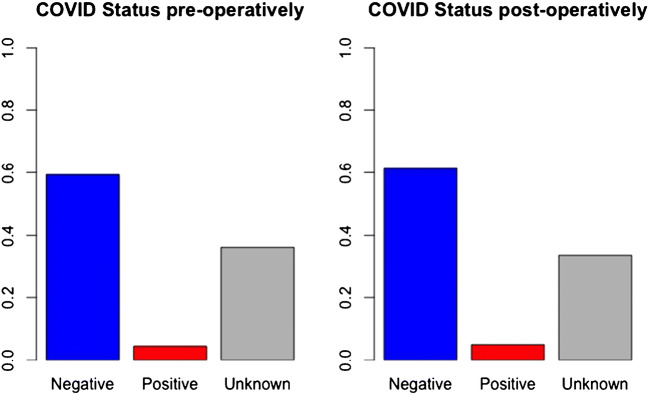
During the lockdown period, 199 procedures were made in our centre. There were three types of procedures: 79 traumatology procedures (39.7%), 76 bone and soft tissue tumours (38.2%), and 44 procedures related to infection (22.1%). The mean age of patients was 59.7 years (21.8) with a mean body mass index (BMI) at 24.3 kg/m2 (5.8), and 60.3% of patients were women. The detail of demographic data is available in Table 1. We did a systematic RT-PCR from June 04, 2020. The COVID status was available for 127 patients. Nine were COVID-positive patients (7%). Patients were significantly older in the COVID-19 positive group than COVID-19 negative group (73.3 years versus 63.1, p = 0.03). The demographical data of each group are reported in Table 2.
Table 1.
Demographic data
| Parameters | Values | Number | Statistics |
|---|---|---|---|
| Age (years) | 199 | 59.7 (21.8) | |
| Gender | F | 120 | 60.3% |
| H | 79 | 39.7% | |
| BMI (kg/m2) | 185 | 24.3 (5.8) | |
| Indication | Infection | 44 | 22.11% |
| Traumatology | 79 | 39.7% | |
| Tumor | 76 | 38.2% | |
| ASA | 198 | 1.9 (0.8) |
Table 2.
Demographic data for COVID-positive group and COVID-negative group
| Parameters | Values | N | Statistics* | N | Statistics* | p value |
|---|---|---|---|---|---|---|
| COVID status | 118 | Negative | 9 | Positive | ||
| Age | 118 | 63.1 (20.9) | 9 | 77.3 (18.1) | 0.03 | |
| Gender | F | 72 | 61.0% | 6 | 66.7% | 1.00 |
| H | 46 | 39.0% | 3 | 33.3% | ||
| BMI | 111 | 24.3 (6.0) | 5 | 21.4 (3.0) | 0.25 | |
| Indication | Infection | 26 | 22.0% | 2 | 22.2% | 0.43 |
| Traumatology | 54 | 45.8% | 6 | 66.7% | ||
| Tumour | 38 | 32.2% | 1 | 11.1% | ||
| ASA | 118 | 2.0(0.8) | 9 | 2.3(0.5) | 0.20 |
Effectiveness of the procedures implemented for COVID outbreak
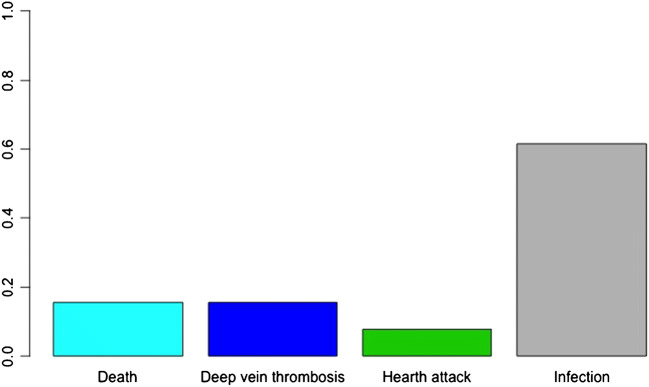
We observed 13 complications (6.5%) during hospitalization: two deep veins thrombosis, eight deep infections, one heart attack, and two patients died. Only one patient became COVID-19 positive during the hospitalization (Figs. 1 and 2). Our medical team, during the lockdown period, was composed by 19 surgeons: ten senior surgeons and nine residents. Three surgeons (15.7%) became COVID-19 positive at the end of the lockdown period.
Fig. 1.
Complications during hospitalization
Fig. 2.
Pre-operative and post-operative status
Medical care provided
We did not observe significant difference in the COVID-19-positive group versus COVID-19-negative group regarding complications during the hospitalization (p value = 0.36). Complication occurred for one COVID-19-positive patient (11.1%), for five COVID-19-negative patients (4.2%), and for seven with an unknown COVID-19 status (9.7%). The details of complications are detailed in Table 3.
Table 3.
Complications during hospitalization for COVID-positive and COVID-negative group
| Parameters | Values | Number | Statistics* | N | Statistics* | p value |
|---|---|---|---|---|---|---|
| COVID status | 118 | Negative | 9 | Positive | ||
| Complications during hospitalization | No | 113 | 95.8% | 8 | 88.9% | 0.36 |
| Yes | 5 | 4.2% | 1 | 11.1% | ||
| Time between surgery and complications (days) | 5 | 22.8 (13.4) | 1 | 3 (−) | 0.33 | |
| Details of complications | 0.50 | |||||
| Death | 0 | 0.0% | 1 | 11.1% | ||
| Hearth attack | 1 | 0.8% | 0 | 0.0% | ||
| Infection | 4 | 3.4% | 0 | 0.0% | ||
| Deep vein thrombosis | 1 | 0.8% | 0 | 0.0% | ||
| Pulmonary embolism | 0 | 0.0% | 0 | 0.0% | ||
We observed a significant difference for the occupancy time of the operating room. It was longer in the COVID-19 positive group (231.7 (112.8) minutes versus 137.5 minutes (90.9), p value < 0.01). We did not observe significant difference for intervention delay, length of stay, and for place of discharge (Table 4).
Table 4.
Data during hospitalization for COVID-positive and COVID-negative group
| Parameters | Values | Number | Statistics* | N | Statistics* | p value |
|---|---|---|---|---|---|---|
| COVID status | 118 | Negative | 9 | Positive | ||
| Intervention delay (days) | 118 | 2.1 (9.6) | 9 | 2.6 (3.5) | 0.36 | |
| Surgical time (min) | 118 | 137.5 (90.9) | 9 | 231.7 (112.8) | < 0.01 | |
| Place of discharge | Medical structure | 57 | 49.14% | 7 | 87.5% | 0.06 |
| Home | 59 | 50.86% | 1 | 12.5% | ||
| Length of stay (days) | 117 | 13.8(10.6) | 9 | 15.3(10.6) | 0.61 |
The mean delay of post-operative control was 36 days (13.2) in COVID-19-negative group versus 37 days (13.5) in COVID-19-positive group, no significant difference (p = 0.85). Fifty-six percent of COVID-19-positive patients had a post-operative control whereas 78.8% of COVID-19-negative patients had it (p = 0.21).
Two patients became COVID-Positive after hospital discharge without any major COVID-19-related complications. We did not observe a significant difference of the numbers of complications between the two groups (Table 5).
Table 5.
Data of post-operative control for COVID-positive and COVID-negative group
| Parameters | Values | Number | Statistics* | Number | Statistics* | p value |
|---|---|---|---|---|---|---|
| COVID status | 118 | Negative | 9 | Positive | ||
| Consultation | No | 25 | 21.2% | 4 | 44.4% | 0.21 |
| Yes | 93 | 78.8% | 5 | 55.6% | ||
| Delay of post-operative control (days) | 94 | 36.0 (13.2) | 5 | 37.2 (13.5) | 0.85 | |
| Complications | No | 96 | 91.4% | 5 | 83.3% | 0.44 |
| Yes | 9 | 8.6% | 1 | 16.7% | ||
| Details of complications | Death | 1 | 0.8% | 1 | 11.1% | 0.40 |
| Deep vein thrombosis | 0 | 0% | 0 | 0% | ||
| Pulmonary embolism | 0 | 0% | 0 | 0% | ||
| Others | 2 | 1.6% | 0 | 0% | ||
| Infection | 6 | 5.1% | 0 | 0% | ||
| Time between surgery and complications (days) | 9 | 25.2 (10.7) | 1 | 41 (−) | 0.22 |
Discussion
The SARS-CoV-2 epidemic started in December 2019 in Wuhan and then spread worldwide [7]. On March 11, WHO declared COVID 19 as a pandemic [3]. Many countries decided to put in place a lockdown of the population. The lockdown was declared on March 16, 2020 in France. The SARS-CoV-2 can cause damage to various organs, including the respiratory system, and can jeopardize the vital prognosis of patients [1]. Our orthopaedic centre, located in the heart of Paris, takes care of bone tumours and emergencies. We had to adapt our practices to continue taking care of malignant and/or progressive bone and soft tissue tumours and emergencies. Through this study, we wanted to assess the various procedures implemented during this period in our centre.
The surgical activity of our centre is divided into the categories of surgery: bone and soft tissue tumors, infectious emergencies, and traumatic emergencies. A total of 199 surgical procedures were performed from March 17 to May 10, 2020. Nine patients (4.5%) were diagnosed COVID-19 positive before the surgery. Thirteen patients (6.5%) presented complications. Only one complication (7.7%) can be attributed to COVID-19: one death in a COVID-19-positive patient. Also, only one patient became COVID-19 positive (0.5%) during hospitalization.
On May 29, 2020, every surgeon of our department had a serology from blood sample for SARS-CoV-2. Out of 19 surgeons present and in contact with patients during lockdown period, three (15.7%) were tested positive for COVID-19, of which two were symptomatic with minor forms and one asymptomatic.
In the literature, the rate of complications in COVID-19-positive patients undergoing surgical procedures is around 30% of mortality at one month, 50% of pulmonary complications, and 2% of thromboembolic complications [8]. We had nine COVID-19 positive patients who were followed for at least up to 30 days post-surgery. Of these nine patients, two died (22.2%).
The measures put in place were apparently effective: We report very few complications related to COVID-19, and few patients were contaminated during their hospitalization. Many guidelines have been dictated in the literature to deal with coronavirus [9].We followed the guidelines written by the Zhejiang University School of Medicine, the Handbook of COVID-19 Prevention [10] for the management of COVID-19-positive patients. Our procedures consisted in diagnosing all hospitalized patients to know their COVID-19 status. We were only able to make RT-PCR for all patients from April 4, 2020 because there were not enough RT-PCR kits available before this date. A waiting hospitalization area has been created in the hospitalization unit to find out the COVID-19 status of patients. Once the COVID-19 status was known, they were either hospitalized in the conventional unit or in the positive COVID-19-positive unit where trained paramedical took care of them. Protective personal equipment including over-blouse, glasses, and masks against the coronavirus were available. The other specificity was that a specific surgical room and elevator were dedicated to the COVID-19-positive patients.
COVID-19-positive and COVID-19-negative patients did not follow the same circuit for medical care. We decided not to perform chest CT scan on all patients contrary to some guidelines [10]. However, our procedures allowed for a low contamination rate of SARS-CoV-2 in patients (0.5%) and doctors (15.7%).
The SARS-CoV-2 epidemic had several impacts on daily surgical activity. First of all, an ethical question was asked every day for emergency, especially for traumatology patients: Should we favour orthopaedic treatments or surgery taking into account the risk/benefit balance? [9] Indeed, surgery could increase the risk of complications for patients (mortality figure throws) or to be infected. Second, the surgical activity during the lockdown period has been reduced and could be detrimental for resident’s education [11].
Finally, we were able to show, despite the increased surgical time due to protective procedures, that the medical care for COVID-19-positive and COVID-19-negative patients included similar care to non-COVID-19 patient in terms of intervention delay, length of stay, and to number of face-to-face consultations.
Once the lockdown was over, elective surgery has resumed. Orthopaedic elective surgery is functional surgery. Recommendations have been made for elective procedures [12]. It should be assessed if performing elective surgery is reasonable or not during the SARS-CoV-2 epidemic [13].
Conclusion
The COVID-19 epidemic has been a challenge for organization and adaptation to manage all urgent and emergent COVID-19-positive and COVID-19-negative patients and avoid increasing the risk SARS-CoV-2 infection. Through this study, we wanted to share our experience and assess our procedures. We think that these procedures have been effective due to the low number of contamination and complications linked to the coronavirus.
Data availability
Available on request.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Code availability
Available on request.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Roser M, Ritchie H, Ortiz-Ospina E, Hasell J (2020) Coronavirus pandemic (COVID-19). Our World in Data.; https://ourworldindata.org/coronavirus. Accessed 24 June 2020
- 3.WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020
- 4.Info coronavirus covid 19 - carte et donnees covid 19 en france. Gouvernement.fr. https://www.gouvernement.fr/info-coronavirus/carte-et-donnees Accessed 24 June 2020
- 5.Décret n° 2020–293 du 23 mars 2020 prescrivant les mesures générales nécessaires pour faire face à l’épidémie de covid-19 dans le cadre de l’état d’urgence sanitaire. 2020–293 23 Mars 2020. https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000041746694&categorieLien=id Accessed 24 June 2020
- 6.Gouvernement français. Préparation à la phase épidémique de COVID-19. https://solidarites-sante.gouv.fr/IMG/pdf/guide-covid-19-phase-epidemique-v15-16032020.pdf Accessed 24 June 2020
- 7.WHO | Middle East respiratory syndrome coronavirus (MERS-CoV) WHO. http://www.who.int/emergencies/mers-cov/en/ Accessed 24 June 2020
- 8.Archer JE, Odeh A, Ereidge S, Salem HK, Jones GP, Gardner A et al (2020) Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 10.1016/S0140-6736(20)31182-X [DOI] [PMC free article] [PubMed]
- 9.Ambrosio L, Vadalà G, Russo F, Papalia R, Denaro V. The role of the orthopaedic surgeon in the COVID-19 era: cautions and perspectives. J Exp Orthop. 2020;7(1):35. doi: 10.1186/s40634-020-00255-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Handbook of COVID-19 Prevention and Treatment | ALNAP. https://www.alnap.org/help-library/handbook-of-covid-19-prevention-and-treatment Accessed 24 June 2020
- 11.Pichard R, Kopel L, Lejeune Q, Masmoudi R, Masmejean EH (2020) Impact of the coronavirus disease 2019 lockdown on hand and upper limb emergencies: experience of a referred university trauma hand Centre in Paris. France Int Orthop. 10.1007/s00264-020-04654-2 [DOI] [PMC free article] [PubMed]
- 12.COVID-19: Elective Case Triage Guidelines for Surgical Care. 24 March 2020. American college of surgeons. https://www.facs.org/covid-19/clinical-guidance/elective-case Accessed 24 June 2020
- 13.Jain A, Jain P, Aggarwal S (2020) SARS-CoV-2 impact on elective Orthopaedic surgery: implications for post-pandemic recovery. J Bone Joint Surg Am. 10.2106/JBJS.20.00602 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available on request.