Abstract
Anomalies of the appendix have been reported mostly in adults as an incidental finding during surgery. The incidence of duplication of the vermiform appendix is reported to be 0.004% and <10 cases of appendicitis have been reported in duplicated appendix. This is a case report of an 18-year-old male who was diagnosed to have perforated appendicitis by imaging, and on open surgical exploration was found to have appendiceal duplication. Histopathological examination of both specimens revealed a perforated necrotic first appendix and an acutely inflamed second appendix. Surgeons must always bear in mind a high degree of suspicion regarding the possibility of duplicated appendices in all cases that are clinically and radiologically suspected to have acute appendicitis or perforated appendicitis. A thorough intraoperative examination of caecum is mandatory to avoid missing the duplication; thus, preventing post-operative complications and medicolegal issues.
INTRODUCTION
The vermiform appendix is a diverticulum of the caecum located at the ileocaecal junction. Being the most variable organ in terms of position, extent and organ relations, congenital anomalies of the vermiform appendix are rarely reported. These anomalies include partial or complete duplication of appendix, agenesis, branching appendix, etc. [1–3] The most common pathology involving the appendix is appendicitis; however, pathology in anomalous appendices is much less common with only few reported cases. Duplication of the vermiform appendix is a rare congenital anomaly, the incidence of which has been reported to be as low as 0.004%. The first case was reported in 1892 by Picoli [4] and since then, <100 cases of appendiceal duplication have been reported in medical literature of which <15 cases presented with appendicitis in the duplicated appendix similar to our case.
CASE REPORT
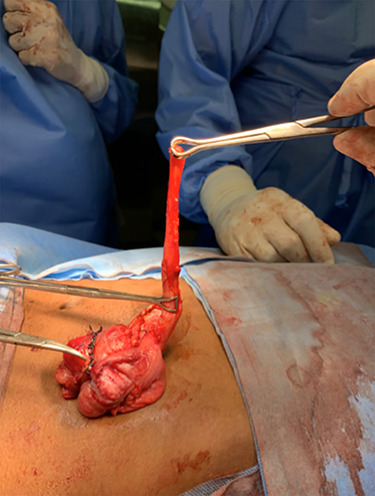
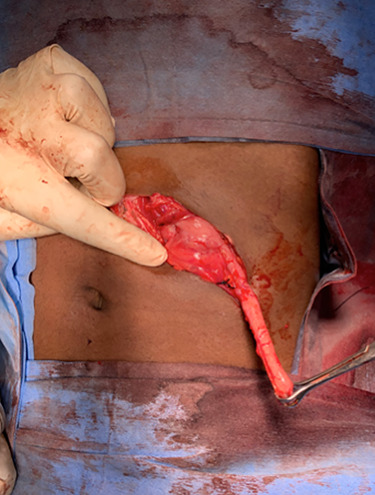
An 18-year-old Indian male presented to the emergency department with complaints of non-radiating abdominal pain in the right lower quadrant for the past 2 days, associated with three episodes of vomiting. Bowel habits were unaltered. On examination, tenderness was localized at McBurney’s point with presence of rebound tenderness. Laboratory investigations showed no abnormalities. Abdominal ultrasound showed a collection of size 2.1 × 1.1 cm near the ileocaecal junction with surrounding fatty inflammatory changes. The appendix could not be visualized in the right iliac fossa, and a radiological diagnosis suggestive of perforated appendix was made. Patient was taken up for emergency appendicectomy. Abdomen was opened through a Lanz incision. Upon entering the peritoneal cavity, seropurulent collection was noted with perforated necrotic sloughed-out gangrenous appendix near the ileocaecal junction in the right iliac fossa with omental adhesions around (Fig. 1). Dense adhesions were found between terminal ileum and lower medial caecal wall in the region of taenia coli. On release of adhesions, terminal ileal and caecal wall perforations were noted (Fig. 2). Abscess was drained and primary closure of terminal ileal and caecal wall perforations was done in two layers (Fig. 3). Base of sloughed-out appendix was identified and ligated and appendectomy was done. On thorough caecal examination and blunt dissection, incidentally an acutely inflamed second appendix was visualized (Fig. 4), the base of which was found to be branching 4 cm from base of perforated appendix, along the line of taenia coli (Figs 3, 5 and 6). Lateral peritoneal attachments to caecum and appendix were released, and second appendectomy was done (Fig. 7). Both specimens were sent for the histopathological examination, which confirmed the diagnosis of suppurative appendicitis with perforation in one specimen (Fig. 8a) and acute appendicitis in the other (Fig. 8b). Post-operative period was uneventful. Intra-abdominal drain was removed on post-operative day 4, as there was no evidence of bowel suture site leak after 72 hours. Patient was discharged on sixth post-operative day with no evidence of surgical site infection.
Figure 1.
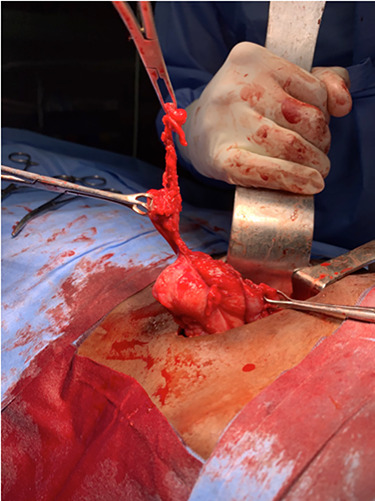
Perforated necrotic sloughed out gangrenous appendix near the ileocaecal junction in the right Iliac fossa with omental adhesions.
Figure 2.
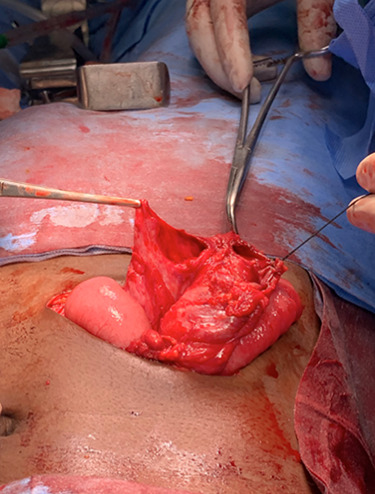
Terminal ileal wall and caecal wall perforations noted after release of adhesions.
Figure 3.
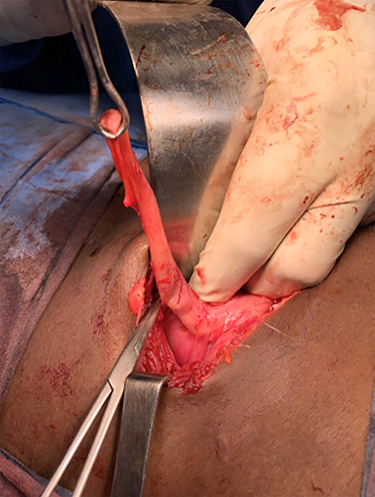
Terminal ileal and caecal wall perforations closed primarily in two layers: second incidentally identified appendix held with Babcock forceps and appendectomy stump of perforated appendix (artery forceps).
Figure 4.
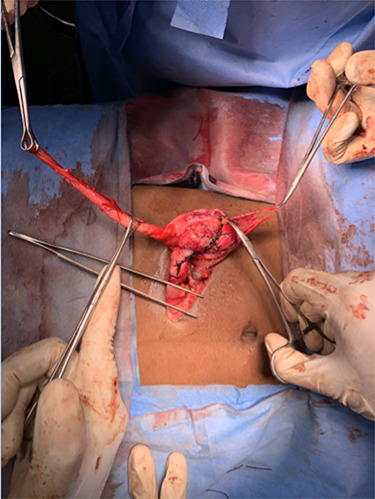
On thorough caecal examination and blunt dissection, incidentally an acutely inflamed second appendix was visualized to be arising from lateral wall of caecum.
Figure 5.
Base of second acutely inflamed appendix was found to be branching 4 cm from the stump of perforated appendix along line of taenia coli.
Figure 6.
Release of lateral peritoneal attachments to caecal wall to complete appendectomy of the second appendix.
Figure 7.

Completed second appendectomy with two appendectomy stumps in the caecum along taenia coli.
Figure 8.
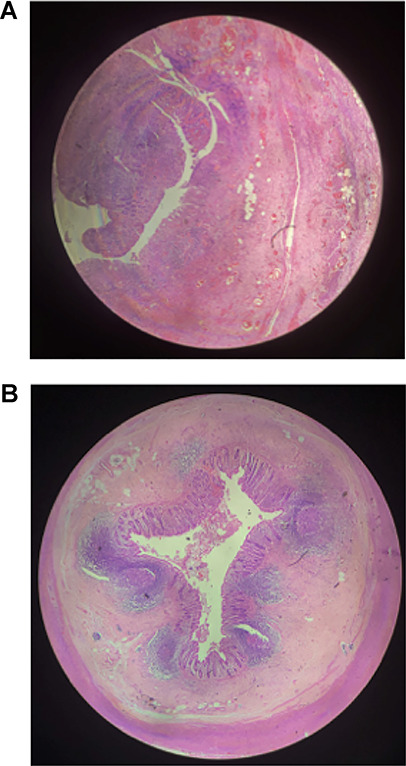
Histopathological examination (H&E stain; ×40 magnification): (a) appendix exhibiting extensive mucosal ulceration with suppurative transmural dense acute inflammation with area of perforation and (b) appendix showing focal ulceration of lining mucosa with lymphoid hyperplasia and mild transmural inflammatory infiltrate.
DISCUSSION
Appendiceal duplication is extremely rare with an incidence of 0.004–0.009% in appendectomy specimens. Duplication of the appendix was first classified by Cave (Fig. 9) in 1936, later updated by Wallbridge in 1962 and once again in 1993 by Bierman [2]. It can be either isolated or seen with caecal duplication. These anomalies are classified into types A, B, C and D. Type A has a single cecum with various degrees of incomplete appendiceal duplication. Type B has a normal appendix that arises from the cecum and is subdivided into four separate types depending on where the second appendix is located. Type B1 (avian-type appendix) arises symmetrically from the other side of the ileocaecal valve; resembling the arrangement of birds. Type B2 (taenia coli type) arises from the caecum at the usual site and the second branches at varying distances along the line of the taenia from the first. Type B3 arises from the hepatic flexure and Type B4 arises from the splenic flexure. Type C is a duplication of the cecum, each containing an appendix. Type D, the most recently described type by Mesko et al. in 1986 is a horseshoe appendix—a single appendix with two openings into the cecum.
Figure 9.
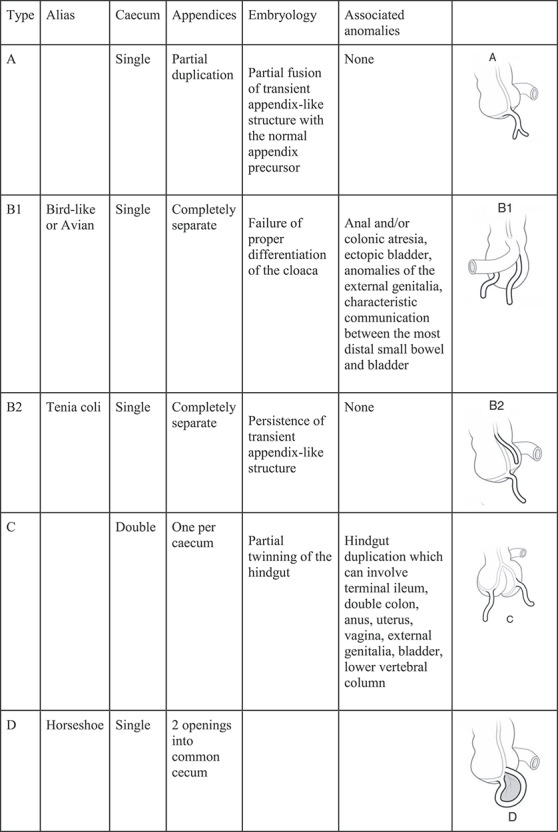
Modified Cave-Wallbridge classification of duplicated appendix [1].
The case described above falls under type B2 since there were two separate appendices found to be arising from the caecum with the duplicate appendix located over the taenia coli. Type B2 is the most frequently reported duplication of the appendix and is found to have no associated congenital anomalies. However, other types are seen to be associated with various anomalies such as hindgut duplication, colonic atresia, bladder anomalies, etc. This evokes surgical importance of further investigations in order to identify possible associated anomalies. The embryological aetiology of appendiceal duplication has been described by Coker et al. [1].
Histopathology confirmed the diagnosis of appendiceal duplication as seen in Fig. 8 [5]. The perforated appendix specimen was found to have extensive mucosal ulceration with suppurative transmural dense acute inflammation. The area of perforation was identified. The mesoappendix showed suppuration with haemorrhage and congestion. The second appendix was found to have focal ulceration of the lining mucosa with lymphoid hyperplasia. Also, mild transmural inflammatory infiltrate with few neutrophils, occasional lymphocytes and serosal congestion was noted in the second appendix.
Acute appendicitis can mimic various other causes of acute abdominal pain, such as Meckel’s diverticulitis, pelvic inflammatory disease, inflammatory bowel disease, etc., making the diagnosis rely heavily on imaging modalities. Ultrasound is deemed as inexpensive, fast, non-invasive and widely available with a well-established and reliable diagnostic accuracy. Abdominal ultrasound has been reported to have an accuracy of 71–97% whereas CT is reported to be 93–98% accurate [6].
However, preoperative radiological investigations do not guarantee the diagnosis of duplicated appendix. Therefore, thorough intraoperative examination of caecum is of paramount significance in detecting rare anomalies of the vermiform appendix, which may otherwise go unnoticed. A case of a child who underwent two appendectomies within a 5-month period for acute appendicitis has been reported [7]. This emphasizes the necessity of exploration every surgeon should carry out intraoperatively, to avoid medicolegal complications and patient anxiety due to missed appendicular anomalies.
Conflict of interest statement
None declared.
Funding
None.
References
- 1. Bhat GA, Reshi TA, Rashid A. Duplication of vermiform appendix. Indian J Surg 2016;78:63–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nazir S, Bulanov A, Ilyas MIM, Jabbour II, Griffith L. Duplicate appendix with acute ruptured appendicitis: a case report. Int Surg 2015;100:662–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vieira EPL, Bonato LM, Silva GGP, Gurgel JL. Congenital abnormalities and anatomical variations of the vermiform appendix and mesoappendix. J Coloproctol (Rio J) 2019;39: 279–87. [Google Scholar]
- 4. Dubhashi SP, Dubhashi UP, Kumar H, Patil C. Double appendix. Indian J Surg 2015;77:1389–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Souza SC, Costa SRMR, Souza IGS. Vermiform appendix: positions and length – a study of 377 cases and literature review. J Coloproctol 2015;35:212–6. [Google Scholar]
- 6. Old JL, Dusing RW, Yap W, Dirks J. Imaging for suspected appendicitis. Am Fam Physician 2005;71:71–8. [PubMed] [Google Scholar]
- 7. Maizels G. Duplication of the vermiformis appendix. S Afr Med J 1966;40:1123. [PubMed] [Google Scholar]


