ABSTRACT
Aspergillus is a common environmental pathogen. However, clinically significant disease only occurs in a small proportion of patients. Although rare in its occurrence, it remains a considerable cause of morbidity and mortality in certain cohorts of patients. We describe a rare case of Aspergillus disease masquerading as a primary lung malignancy. Computer tomography pulmonary angiogram scan demonstrated a right upper lobe 8 x 6.5 cm soft-tissue lesion. Positron emission tomography CT demonstrated this lesion to be intensely fluorodeoxyglucose avid. Initial bronchoscopy demonstrated occluded subsegmental right upper lobe bronchus with white friable material. Follow-up bronchoscopy demonstrated evidence of a previous inflammatory process with cavitation and destruction of sub-lobar bronchial tree. Serial chest radiographs demonstrated almost complete resolution of the right upper lobe mass. Thus, this presentation of an Aspergillus-related lung mass masquerading as a primary lung malignancy provided several important learning points pertaining to diagnosis and ensuing management.
Keywords: Aspergillosis, Lung cancer, Malignancy, Positron emission tomography—CT (PET-CT), Bronchoscopy
INTRODUCTION
Aspergillus is a common environmental pathogen. However, clinically significant disease only occurs in a small proportion of patients. Although rare in its occurrence, it remains a considerable cause of morbidity and mortality in certain cohorts of patients. Aspergillus is a fungal infective pathogen that can affect the lungs in a variety of different ways resulting in asthma, allergic bronchopulmonary aspergillosis, aspergilloma (mycetoma), invasive aspergillosis and extrinsic allergic alveolitis. Risk factors for the development of Aspergillus include transplantation, immunosuppression and concurrent use of corticosteroids and in those with chronic respiratory disease. Due to its varying presentations, patients may present across a whole range of symptoms from mild dyspnoea and wheeze to massive life-threatening haemoptysis [1–2]. It can be managed medically in the form of antifungal treatment (i.e. voriconazole) or surgical management for aspergilloma in the setting of super-imposed infection or massive haemoptysis. Aspergillomas are the most common presentation in the spectrum of Aspergillus-related lung disease [1–4]. We describe a rare case of Aspergillus disease masquerading as a primary lung malignancy.
CASE PRESENTATION
We describe a case of a 25-year-old pregnant young lady who presented with sudden-onset dyspnoea and pleuritic chest pain but no clinical signs of infection or sepsis, with a history of recent travel to Pakistan. She had a past medical history of dengue fever 5 years ago but no other significant comorbidities. She had no calf tenderness or swelling and no family history of venous thromboembolism (VTE) or history of previous VTE. Twelve-lead electrocardiogram demonstrated sinus rhythm and no features suggestive of pulmonary embolism.
Initial investigations included a full blood panel with inflammatory markers (all within normal range) and a plain chest radiograph which demonstrated a mass in the right upper zone (Fig. 1). Computer tomography pulmonary angiogram (CTPA) scan demonstrated an 8 x 6.5 cm soft-tissue lesion within the right upper lobe (Fig. 2). This mass appeared to extend from the right hilum to the pleural surface and contained multiple small arterial branches. Her delivery date was brought forward pending further investigations. Positron emission tomography CT (PET-CT) demonstrated this lesion to be intensely fluorodeoxyglucose (FDG) avid (Fig. 3).
Figure 1.

Plain chest radiograph demonstrating a right upper zone mass.
Figure 2.
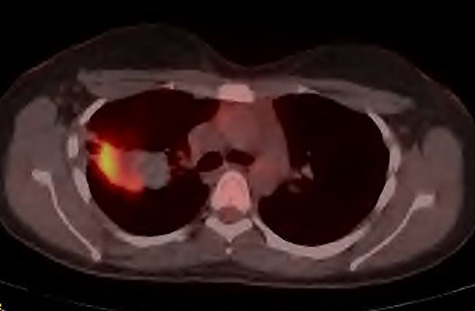
PET-CT demonstrating the right upper lobe lesion to be intensely FDG avid.
Figure 3.
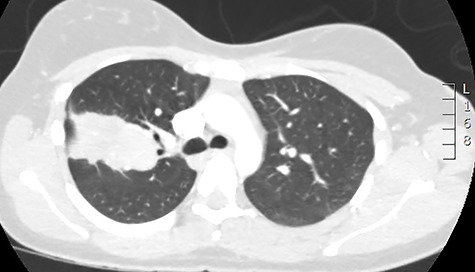
CT scan demonstrating the large apparent right upper lobe mass.
Blood serology demonstrated raised immunoglobulin E (IgE) titres. Investigations for tuberculosis were proven negative, and the patient had a positive radioallergosorbent test (RAST) for Aspergillus fumigatus. Fibreoptic bronchoscopy was suboptimal, and bronchoalveolar lavage (BAL) is performed. Initial bronchoscopy demonstrated findings of a normal trachea and left bronchial tree anatomy and normal right bronchial intermedius and right lower lobe bronchus anatomy. The bronchus to the right upper lobe demonstrates an occluded subsegmental bronchus with white friable material, an endobronchial brush was pushed through occluded bronchus and biopsies were taken and sent for cytology, microscopy, culture and sensitivity and BAL washings.
The case was rediscussed at the lung multidisciplinary meeting, and the plan was for the patient to undergo thoracic surgical intervention to remove the mass due to its uncertain nature. As the patient had remained asymptomatic with no haemoptysis and there was no interval change in the mass on surveillance imaging, the patient was brought back for follow-up bronchoscopy. This demonstrated evidence of a previous inflammatory process with cavitation and destruction of sub-lobar bronchial tree. Impression was that the last bronchoscopy had cleared the airway and the patient coughed and cleared the lung distally. The procedure was largely uncomplicated. The patient was subsequently discharged after they had recovered from the anaesthetic. Serial chest radiographs demonstrated almost complete resolution of the right upper lobe mass (Fig. 4). Furthermore, serial IgE titres demonstrated decreasing levels, and this was without the patient being commenced on any antifungal treatment.
Figure 4.

Plain chest radiograph demonstrating resolution of the right upper zone mass.
DISCUSSION
There are sparse reports in written literature commenting on resolution of an Aspergillus-related mass following bronchoscopy without specific antifungal treatment or surgical intervention. Furthermore, the presence of an Aspergillus lung mass which is not aspergilloma or an aspergilloma cavity within a malignancy masquerading as a primary lung neoplasm has not been described previously. Other infective processes such as actinomycosis masquerading as a primary lung neoplasm have been mentioned [5].
Aspergillosis has been described causing lobar collapse and mimicking late-onset asthma [6], and it has even been described in the post-cardiac surgery setting presenting as a mediastinal mass requiring surgical intervention [7]. In the case of Aspergillus-related lung disease causing lobar collapse, the diagnosis was made at bronchoscopy, and although the presentation was atypical, the variant of allergic bronchopulmonary aspergillosis is well described [1–2]. In the case of postsurgical setting, the infected mediastinal collection was a sequelae following venous reconstructive surgery for superior vena cava syndrome. The postsurgical invasive aspergillosis following cardiac surgery in immunocompetent individuals has been previously reported [8–9]. The chronic necrotizing form of Aspergillus lung disease causing nodules that were mimicking lung malignancy has also been described in a case series [10]. However, this was not reported as Aspergillus-related lung mass masquerading as a primary lung neoplasm. Interestingly, the lung nodules identified as part of this case series demonstrated the necrotizing granulomas to be containing fungal hyphae. On follow-up none of the nodules has recurred or progressed [10].
The case illustrates the importance of correlating radiological findings with the clinical assessment of the patient and the positive blood test findings. Furthermore, it emphasizes the importance of always treating the patient primarily and not the imaging finding. The sub-lobar bronchial tree destruction and bronchoscopic findings were suggestive of an infective or inflammatory process. Thus, this presentation of an Aspergillus-related lung mass masquerading as a primary lung malignancy provided several important learning points pertaining to diagnosis and ensuing management.
FINANCIAL SUPPORT
None to declare.
CONFLICT OF INTEREST
None to declare.
REFERENCES
- 1. Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis. Thorax 2015;70:270–7. [DOI] [PubMed] [Google Scholar]
- 2. Gao Y, Soubani A. Advances in the diagnosis and management of pulmonary aspergillosis. Adv Respir Med 2019;87:231–43. [DOI] [PubMed] [Google Scholar]
- 3. Meeker DP, Gephardt GN, Cordasco EM Jr. Hypersensitivity pneumonitis versus invasive pulmonary aspergillosis: two cases with unusual pathologic findings and review of the literature. Am Rev Respir Dis 1991;143:431–6. [DOI] [PubMed] [Google Scholar]
- 4. Shimaoka Y, Ishida T, Kawasaki S. An autopsy case of aspergillus pneumonia after inhalation of a great deal of dust in a mushroom factory. J Jpn Resp Soc 2006;44:659–64. [PubMed] [Google Scholar]
- 5. Katsenos S, Galinos I, Styliara P, Galanopoulou N, Psathakis K. Primary bronchopulmonary actinomycosis masquerading as lung cancer: apropos of two cases and literature review. Case Rep Infect Dis 2015;2015:609637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baggott C, Sharp C, Bhatt N, Plummeridge M, Adamali H. Lesson of the month 1: a cough that doesn't fit the mould. Clin Med (Lond) 2015;15:492–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Farid S, AbuSaleh O, Aburjania N, Sohail MR. Postsurgical mediastinal aspergilloma masquerading as malignancy. BMJ Case Rep 2017;2017:bcr2017221140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leffert RL, Hackett RL. Aspergillus aortitis following replacement of aortic valve. J Thorac Cardiovasc Surg 1967;53:866–7. [PubMed] [Google Scholar]
- 9. Rajbanshi BG, Hughes JE, DeSimone DC. Surgical excision of invasive aspergillosis of the right ventricle presenting as intractable ventricular arrhythmia and right ventricular mass. Mayo Clin Proc 2012;87:926–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dermawan JK, Ghosh S, Mukhopadhyay S. Expanding the spectrum of chronic necrotising (semi-invasive) aspergillosis: series of eight cases presenting as radiologically solid lung nodules mimicking malignancy. Histopathology 2020;76:685–97. [DOI] [PubMed] [Google Scholar]


