Abstract
Given varying state-level laws regarding cannabis use, the objective of the review was to summarize contemporary literature on the relationship between adolescent cognitive function and academic performance with cannabis use. Frequency and quantity of cannabis use were associated with decreased functional connectivity of the brain. Earlier age at cannabis initiation and more frequent use was associated with poorer executive control and academic performance. Social determinants such as minimal parental monitoring, peer use and low social cohesion were associated with more frequent adolescent use. Race/ethnicity and residence were other factors influencing cannabis use. To prevent cannabis use disorders among adolescents, interventions should aim to prevent early initiation that can lead to chronic use in youth who may be more at risk.
Current Opinion in Psychology 2021, 38:38–48
This review comes from a themed issue on Cannabis
Edited by Ken C Winters and Joel Mader
For a complete overview see the Issue and the Editorial
Available online 16th July 2020
https://doi.org/10.1016/j.copsyc.2020.07.006
2352-250X/© 2020 The Authors. Published by Elsevier Ltd. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Cannabis, also referred to as marijuana, is one of the most commonly used substances globally in terms of occurrence (the likelihood of an individual becoming a user) and frequency (number of users in the population) [1]. In terms of care and treatment, cannabis is the most commonly reported illicit psychoactive substance used among U.S. youth [2,3•]. Throughout the past 25 years, although its decriminalization, medicalization, and legalization in the U.S. has led to a shift in societal perceptions and usage patterns among Americans, there is no consensus that state-level cannabis laws and medical marijuana laws (MML) moving towards decriminalization and legalization have necessarily increased cannabis use among adolescents [3•]. The statistics reflect that across the United States, there was no increase in average frequency of cannabis use among adolescents post-legalization in the US, with some data demonstrating an average 7% decrease in monthly use among adolescents post cannabis legalization (K. Winters, PhD, unpublished data, 2019).
Despite the apparent decrease in average cannabis use, there are less protective trends for cannabis use disorders (CUD), or the overuse or misuse of cannabis that can lead to addiction [4], with at least one study suggesting an increase in CUDs among adolescents since recreational medical marijuana laws (RML) [5]. Individuals may be more at risk for overusing cannabis or developing a CUD because of increased accessibility to cannabis through MML and legalization of recreational use in some states. However, there has also been increase in the potency of cannabis product over time possibly contributing to increasing CUD prevalence in the US [6].
Risk perception, which impacts cannabis use, has varied over time and is almost cyclical [7]. Policy changes leading to a decrease in risk perception was at its lowest during the Woodstock generation in the 60’s and late 70’s. During this time, there was an increase in cannabis consumption among middle and high school students. The perception of cannabis harmfulness subsequently increased in the 80’s to early 90’s, and by the mid 90’s, the perception of cannabis harmfulness began to decrease again [3•]. A 2019 study found risk perception in adolescents was directly associated with lifetime cannabis use [8]. In addition to a low-risk perception among cannabis consumers, there can also be positive beliefs about its use, such as cannabis use increasing creativity [8].
One consideration supporting the investigation of cannabis use in a vulnerable populations such as adolescents is cannabis potency or Δ-9 tetrahydrocannabinol (THC) concentration increasing over time [6,9,10]. An examination of cannabinoid concentration in cannabis products confiscated by the U.S. Drug Enforcement Administration demonstrates cannabis potency tripling from ∼4% in 1995 to ∼12% in 2014 [9]. A higher THC dosage will increase the possibility of addiction, but can also modify the effect of cannabis on brain development, cognitive function and mental health [9,10]. Therefore, a better understanding of the sequelae associated with more frequent use and/or more potent cannabis exposure is crucial information to adequately guide policy for this population.
Evidence in the extant literature regarding the long-term effects of chronic cannabis use on adolescent neurological functioning is limited and inconclusive. Researchers believe there is some evidence suggesting structural changes may result from persistent use, and these changes might be correlated with decreased academic performance, impairments in cognition, and increased prevalence of addictive and mood disorders [3•,10].
Understanding this public health problem among adolescents is essential to estimate the effect of frequency of use and CUD on adolescent cognitive function. Consequently, this review aims to synthesize the current literature of limited yet varied studies on the impact of cannabis use on cognitive function and academic performance among adolescents across the country. The review will add to the existing research that looks at cannabis use among adolescents for mental health outcomes [11••], by examining adolescent cognitive function, academic performance and related consequences associated with cannabis use.
The review also includes some discourse about the relevance of these findings in the context of the global Covid-19 public health emergency [12]. Estimates suggest that the COVID-19 pandemic could result in a projected 7500 additional deaths from alcohol and drug misuse and suicide [13]. Economic change and social disconnection are the two most replicated factors associated with suicide [14]. Given reported [12] increases in number of legal cannabis sales and quantity purchased since the emergence of COVID-19 pandemic, it is worth expanding the interpretation of our review findings for adolescents living in this shifting global order.
Methods
The authors searched for relevant articles in the following databases: MEDLINE, CINAHL and PsycInfo. The search strategy included relevant keywords and MESH terms on cannabis use, cognitive function and adolescents (Table 1 ). The selected studies were published in the last five years, from January 1, 2015 until March 5, 2020.
Table 1.
Search strategy
| Database | Cannabis | Adolescents | Cognitive function |
|---|---|---|---|
| PSCYINFO | (Cannabi* OR ‘Marijuana Smoking’ OR ‘Medical Marijuana’ OR ‘Marijuana Smoking’ OR tetrahydrocannabinol) | Adolescen* OR teen* OR teenager* OR ‘young people’ OR ‘school-aged children’ OR youth* OR student OR juvenil* OR ‘High School’ | Cognit* |
| MEDLINE | (‘Cannabinoids’[Mesh] OR ‘Marijuana Smoking’[Mesh] OR ‘Marijuana Abuse’[Mesh] OR ‘Medical Marijuana’[Mesh] OR marijuana smoking or therapeutic use [Mesh] OR ‘Medical Marijuana’[Mesh] OR ‘tetrahydrocannabinol’ OR Cannabi* OR Marijuana OR Tetrahydrocannabinol) | Adolescen* OR teen* OR teenager* OR ‘young people’ OR ‘school-aged children’ OR youth* OR student OR juvenil* OR ‘High School’ | Cogni* |
| CINAHL | (MH ‘Cannabis’) OR (MH ‘Medical Marijuana’) | (MH ‘Adolescence’) OR (MH) | (MH ‘Cognition’) |
Study eligibility criteria
Both experimental and observational studies were included. The study designs included case-control, cross-sectional, cohort and randomized controlled trials.
Inclusion criteria
-
•
Peer-reviewed articles
-
•
Adolescents aged 12–17 years residing in the United States without any restrictions on sex and race/ethnicity
-
•
Articles published in the English language
Exclusion criteria
-
•
Review studies without data or findings
-
•
Presence of existing comorbidities as a confounder
Main outcomes
The primary outcome was cognitive function. Secondary outcomes included academic performance, and cannabis use in the context of polysubstance use. The primary exposure was cannabis use.
Search screening
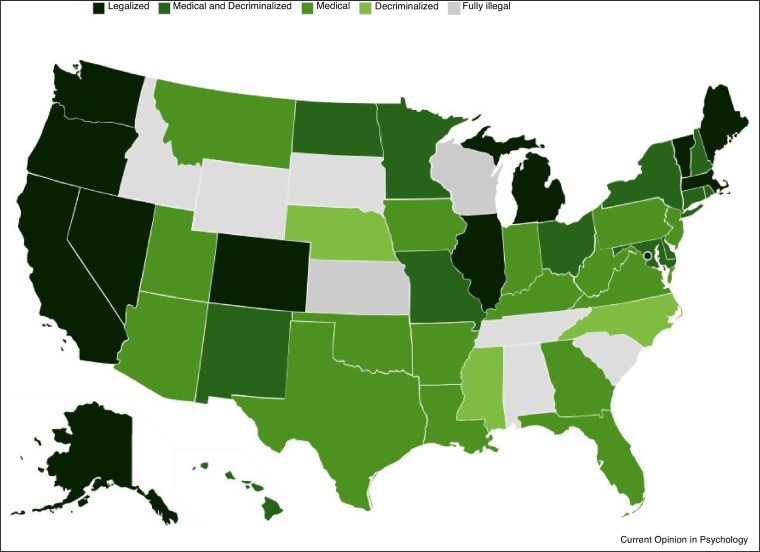
The authors imported articles into Covidence Software to initiate the search screening process based on the search criteria identified in Table 1. Three authors (MC, SK and YM) screened the titles and abstracts independently to assess studies that met the inclusion criteria. The articles were selected if there was consensus reached by two of three authors. To minimize bias during the screening process, a third author resolved any disagreements between two reviewing authors. Subsequently, the authors conducted full screening of articles to meet the eligibility criteria using the same consensus guidelines. A standardized data sheet form was created to perform data extraction. The form included author, publication year, demographic information, study setting, study population, study design, prevalence of cannabis use, study measures of association and overall study findings. Data was collected from multiple states with varying cannabis policies. None of the states eligible to be included in the review had legalized recreational use, and two of the states (Virginia and Texas) had limited TCH/CBD programs, with the remaining states having policies short of recreational use or comprehensive medical marijuana use programs (see Figure 1 ) [15]. States with no policy or position on cannabis use were not included in the review because to our knowledge, there were no studies conducted in these settings.
Figure 1.
Map of Marijuana Legality by State As of July, 2020 [41].
Results
In this review, we found that cannabis use demonstrated persistent effects on cognitive health outcomes among adolescents and was associated with both the frequency of use and early age of initiation of cannabis use [16, 17, 18]. The following sections provide greater details of these associations.
Cognitive outcomes
The studies included in the review shed light on patterns of use, and the impacts of use on cognitive function, including academic performance. Early age of first cannabis use, frequent use and having a CUD were related to lower cognitive function measured by several brain biomarkers discussed below. Despite this inverse relationship between cannabis use and cognitive function, one study found some protective effects among occasional users.
The study conducted by Becker et al. [18] determined, through the assessment of diffusion tensor imaging results, that cannabis users (who started using before age 17) had decreased white matter growth in specific regions of the brain, such as the central and parietal regions of the right and left superior longitudinal fasciculus [18]. This altered development of white matter contributed to functional impairment and decreased cognitive function observed among cannabis users [18]. This was shown by the diminished performance in verbal learning and memory observed amongst cannabis users compared to non-users [18]. In addition to these effects on verbal learning and memory, cannabis use may also result in deleterious effects on resting functional connectivity among adolescents with CUD [16]. Camchong et al. [16] assessed resting functional connectivity, intelligence quotient (IQ), and cognitive function among 43 healthy controls and 22 treatment-seeking adolescents with CUD [16]. They determined that adolescents with CUD showed decreased functional connectivity, lower IQ scores, and slower cognitive function compared to the healthy controls [16]. The most impacted areas of the brain among adolescents with cannabis use disorder were identified as the anterior cingulate cortex and orbitofrontal cortex [16]. Both Becker et al. [18] and Camchong et al. [16] explored the effects of cannabis use on adolescent brain development through longitudinal studies and identified significant impacts on multiple areas of the brain. Camchong et al. [16] further expanded upon the conclusions of Becker et al. [18] by examining resting functional connectivity, which previously was not done. Both studies presented similar findings with respect to the deleterious effects of cannabis use on adolescent brain development and subsequent diminished cognitive outcomes.
Cognitive outcomes such as reaction time, recall and accuracy have been shown to be associated with cannabis use [19]. A study conducted by Sweeney et al. [19] evaluated working memory among individuals with substance use disorder, with cannabis being the primary substance of abuse [19]. Adolescents were assigned to either the experimental or control group where adolescents in the experimental group received working memory training, and those in the control did not [19]. After adjusting for cannabis use, participants who received training were less likely to have working memory impairment, specifically they exhibited faster reaction time [19].
Frequency of cannabis use and age of onset also affects cognitive outcomes such as executive control [19,20•]. The frequency of cannabis use and age of onset can lead to deleterious effects on working memory, such as reduced recall time and sustained attention [19,20•]. Scott et al. [20•] examined the relationship between the frequency of cannabis use and age, and determined that adolescents who were frequent users had worse measures of executive control when compared to non-users [20•]
Age of onset of cannabis use was also significantly associated with executive control, where earlier age of cannabis use was associated with worse performance of executive functioning among occasional cannabis users [20•]. However in this study, compared to non-use, occasional use was associated with better executive control, memory, and social cognition [20•].
Academic performance
One relevant measure for cognitive function among adolescents is academic performance [17]. The findings related to academic performance were an extension of the cognitive function findings with a negative association between cannabis use and academic performance, but some racial/ethnic differences in terms of academic metrics were highlighted.
One longitudinal study by Reboussin et al. [21] examined how patterns of academic and behavioral problems in the first grade relate to longitudinal transitions in marijuana use from middle school to high school among African Americans [21]. Academic difficulties were found to co-occur with externalizing and attention/concentration problems [21]. Youth who experienced academic problems in conjunction with attention/concentration problems were more likely to use cannabis [21].
Targeted interventions may further be necessary as literature highlights racial and ethnic differences in cannabis use [22]. For example, the study conducted by Knopf et al. [22] determined that white youth are at the highest risk of cannabis use during middle and high school [22]. Though the study conducted by Reboussin et al. [21] focused only on African Americans and the Knopf et al. [22] study included multiple races, both concluded that marijuana use was associated with poor academic outcomes [21,22].
Earlier age of onset of cannabis use also plays an integral role in academic performance. The study conducted by Buchy et al. [23] examined the relationship between IQ and cannabis use among 678 youth at clinical high risk of psychosis and 263 health controls [23]. They concluded that there were significant differences in IQ scores among early onset, late-onset, and naïve cannabis users [23]. IQ scores were significantly higher among late-onset cannabis users when compared to early onset and naïve cannabis users [23]. The authors hypothesized that higher IQ may lead youth at clinical high risk of psychosis to delay the onset of their cannabis use during adolescence [23]. They further postulate that there may be an interactive effect between cannabis use and IQ when age of onset occurs during a sensitive development period [23]. These findings were only observed among youth at clinically high risk of psychosis and not among healthy controls [23].
A prospective cohort study conducted by Meier and colleagues among youth from an upper-middle-class community determined that persistent cannabis use throughout high school was associated with lower grade point averages and lower scholastic aptitude test scores [24]. However, these effects were not significant after controlling for persistent alcohol and tobacco use and therefore cannabis may not solely account for poor academic performance [24]. These findings highlight one of the considerable difficulties in substance use research and delineating the effects of the primary exposures when there is polysubstance use and their corresponding effects [24].
Risk factors associated with polysubstance use
There were studies providing evidence of a relationship between social environment, cannabis use and polysubstance use [25,26••,27] For example, one study was able to predict the longitudinal risk of marijuana, tobacco and alcohol use based on an adolescent's social environment [25]. As opposed to the previously mentioned Knopf et al. [22] findings [22] which examined cannabis use among multiple races, Musci et al. examined the risk factors associated with African American youths only and tobacco use and cannabis use. In the Musci et al. study, some of the traits found in the social environment of an adolescent who uses marijuana and/or tobacco at least moderately were low parental monitoring and multiple friends who engaged in substance use [25]. In the Mason and Mennis study, general disorder in a living environment or social disorganization in an adolescent’s neighborhood and living within an urban city environment was an indication of behaviors leading to cannabis use [26••]. This study discussed areas in a city considered to be ‘favorite places’ that were associated with risk behaviors for cannabis use [26••].
The difference between synthetic and plant-based cannabinoid use is also a consideration when evaluating cannabis use among contemporary adolescents. In the 2017 Ninnemann et al. study, adolescents who regularly used cannabis were more likely to use synthetic cannabinoids [27]. It was also found that females and African Americans on average use less synthetic cannabinoids than males and people of other races and ethnicities. On the other hand, the presence of synthetic cannabinoid use was not indicative of subsequent marijuana use [27].
Discussion
This review adds to the preceding literature by considering the impact of cannabis use on adolescent brain development, and specifically on cognitive function and academic performance [11••]. When assessing marijuana use among adolescents, individual motivating factors and social environmental factors appeared to be stronger explanatory variables than state policies or governing laws. Specifically, as previously mentioned in this review, higher cannabis use was not always associated with medical marijuana legalization or RML in states. The first state law allowing medical use of cannabis was enacted in 1996 [28]. Since the 1990’s, an increasing number of states within the United States have begun to revise policies that loosen federal restrictions on marijuana and lean toward decriminalization of use [28].
Our study findings support the need for continuing research to examine national trends of adolescent cannabis use as state policies and laws regarding medical and commercial marijuana continue to evolve in the U.S. [29••] In addition to laws and ordinances, other possible moderating factors between adolescent cannabis use and cognitive function are settings or areas of social congregation in urban locales, less family support, less parental monitoring, less social capital, and/or less social cohesion. At-risk adolescents with any of these risk factors may be heavier/more frequent users or have a CUD, with increased odds of lower cognitive function and academic performance in some instances.
There are differences in patterns of cannabis use by race and ethnicity that can have differential impact on cognitive function and academic performance. For racial/ethnic minorities, cannabis use may be more harmful on academic performance compared to adolescents who are not racial/ethnic minorities and live in more supportive resource-rich environments that provide advantages fostering academic development [30]. More studies are needed to examine the reason for this racial/ethnic differences and disparities.
Finally, there has been a recent shift in social and health paradigms because of the COVID-19 public health emergency, with the United States as one of the epicenters of the pandemic [31]. One of the unintended consequences of COVID-19 is its impact on mental health of the general population. There is limited data on COVID-19 related mental health outcomes in the US, however, data from China, suggests that during the time of Covid-19 pandemic, mitigation policies, including social distancing and social isolation led to increased levels of anxiety and depression in the general population [32]. An increase in these mental health conditions may have an impact on substance use initiation, frequency and quantity of use, and use related problems [33,34], particularly among adolescents who may be experiencing a number of challenging mental health conditions that are present during this time [11••].
Study limitations
The overall finding was that harmful effects are more likely associated with more frequent or heavier use, but there was no structured consistent guidance or definition of a ‘more frequent’ or ‘heavier’ user.
The lack of standardized measures for cannabis use did not allow for a deeper analysis or comparison among studies and prohibited any type of data pooling or analysis [35]. While there are number of self-report validated scales capturing information on patterns and modalities of cannabis use [36], there are limited complementary biomarker tests providing information beyond substance presence, to help with understanding cannabis toxicity levels for adolescents that would be considered harmful use. Besides varying definitions for ‘heavy’, ‘moderate’ or ‘light’ use, there is also minimal descriptions on THC concentration or potency. Relatedly, there is no concrete guidance about biochemical differences between synthetic and plant-based marijuana use on adolescents’ cognitive function or mental health. Finally, there were limited longitudinal studies to understand temporal patterns and relationships.
Conclusion
This review found adolescent cannabis use was associated with poorer outcomes on key markers and milestones for adolescent cognitive function. The study findings will be of interest to parents, educators and the scientific community who serve and work with adolescent populations. It should be noted that there are still significant gaps to be addressed, including studies using systematic methods are needed that assess outcomes using standardized measures for dosage, THC exposure and frequency of use, and, longitudinal studies. Additionally, cannabis studies should be conducted in the context of individual’s community and social environment.
Recent global health events have catapulted the US along with other countries into an unprecedented phase of physical distancing and isolation in response to the Covid-19 epidemic [37, 38, 39]. There may be a simultaneous increase in prevalence of depression, anxiety, stress and loneliness in the general population because of these distancing measures [40]. During and immediately after the social distancing phase, it is anticipated that substance use, including cannabis use, will be used as a coping mechanism and increase among people who experience some of these mental health conditions. This is relevant for adolescents who were already engaging in cannabis use or at-risk of use, as they may also increase their use while adapting to the Covid-19 crisis.
Not only can physical distancing have a direct impact on cannabis use and mental health, but also the sudden and unexpected change of environment and social norms can potentially propagate other negative outcomes or unintended consequences of the pandemic in all segments of the population. Therefore, to prevent the disruption of successful long-term adolescent trajectories, more research is urgently needed regarding the deleterious health effects of more frequent cannabis use or CUD during the COVID-19 pandemic on cognitive function, academic performance, mental health and resilience.
Funding
The project was supported by the National Institutes of Health and awards NIDA K99DA046311; NIMHD 1 S21 MD010683-01; NIMHD U54MD002266; NIMHD U54MD012393; NIAAA U34AA026219 and NLM 5U01LM012675. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement
Nothing declared.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
• of special interest
•• of outstanding interest
| Author, year | Study type | Sample size | Study location | Mean age (years) | % Female | % Male | Cannabis prevalence | Measure of association | 95% confidence interval/p-value | Study conclusion |
|---|---|---|---|---|---|---|---|---|---|---|
| Cognitive performance | ||||||||||
| Becker [18] | Cohort | 46 | Minnesota | – | 30.4%-non-users | 69.6%-non-users | – | – | - p values for all outcomes were <0.05 | Heavy cannabis use resulted in decreased longitudinal growth in the brain white matter structure areas of the brain and reduced performance in verbal learning and memory compared to non-cannabis users. |
| 30.4%-cannabis users | 69.6%-cannabis users | |||||||||
| Camchong [16] | Cohort | 65 | Minneapolis and St. Paul, MN | Females = 16.5 ± 2.7 | 47% | 51% | – | – | - p values for all outcomes were <0.05 | Among adolescents diagnosed with cannabis use disorder, there is decreased functional connectivity in the brain's frontally mediated network, lower IQ, and slower cognitive functions compared to non-users. |
| Males = 17.6 ± 2.4 | ||||||||||
| Scott [20•] | Cohort | 4,568 | Philadelphia, PA | 17.6 ± 1.7 | 31% | 69% | 4.97% | – | - p values for all outcomes were <0.05 | - Mild executive control deficits were reported among adolescents who are frequent users (3–4 times per week) compared to non-users. |
| - Early age of initiation resulted in poorer executive control deficits only among occasional users (1–2 times per week). | ||||||||||
| - Occasional users had better executive control, memory and social cognition compared to non-users. | ||||||||||
| Sweeney [19] | RCT | 37 | Baltimore, MD | 16.2 | 16.20% | 83.80% | – | PSAT (control)- 0.31(0.04); PSAT (experimental) - 0.42 (0.04) | p < 0.05 | Adolescent cannabis use is associated with working memory impairment. |
| Academic performance | ||||||||||
| Meier [24] | Cohort | 254 | New England, US | Time pt 1:14/15 Time pt 2:17/18 | – | – | 19% | β = −0.18 | - 95% CI: -0.30, −0.05; p = 0.006 | Persistent cannabis use (10–19 times in the past year) was associated with lower GPA in 12th grade, lower GPA specifically after accounting for 9th grade results and lower SAT scores during 12th grade. |
| β = −0.13 | - 95% CI: -0.24, −0.03; p = 0.014 | |||||||||
| β = −0.13 | - 95% CI: -0.26, −0.007; p = 0.038 | |||||||||
| Reboussin [21] | Longitudinal | 458 | Baltimore, MD | Range: 10.62–13.12 | 48% | 52% | 60% | (aOR = 10.83), | - 95% CI: (2.16, 54.39) p < 0.05 | Academic problems occur in combination with both externalizing cannabis use and attention/concentration problems in African Americans, although to a lesser extent with externalizing cannabis use problems. |
| (aOR = 5.99) | - 95% CI: (1.37–26.12) p < 0.05 | |||||||||
| Knopf [22] | Longitudinal | 6509 | Southern CA | Range: 11.5–17 | 50% | 50% | – | N/A, descriptive | N/A, descriptive | - White youth had a higher likelihood of alcohol and marijuana use compared to other races/ethnicities. |
| - Nonwhite youth had worse academic performance compared to whites. | ||||||||||
| - Greater alcohol or marijuana use was associated with academic unpreparedness and delinquency. | ||||||||||
| - Greater marijuana use was associated with lower academic performance and worse mental health outcomes. | ||||||||||
| Buchy [23] | Prospective cohort | 941 | Multi-site | CHR-15.7 | CHR-42% | CHR-58%; | CHR early onset: 122 (18.0%) | ANCOVA: F(3,641) = 6.13. | p < 0.05 | Earlier age at onset of cannabis use may be a more important factor for IQ than current use or frequency |
| HC-16.2 | HC-48% | HC-52% | Late onset: 227 (33.5%) Naïve: 327 (48.2%) | |||||||
| Risk factors associated with polysubstance use | ||||||||||
| Mason and Mennis [26••] | Longitudinal | 248 | Richmond, VA | 13–14 | 57% | 43% | – | Neighborhood disorder ([aOR] = 1.77) | Neighborhood disorder ([CI] = 1.01, 3.09), | Neighborhood disorder and city environment promote peer risk behaviors which influence cannabis use of urban adolescents. |
| City places x peer network risk (aOR = 8.17) | City places x peer network risk (CI = 1.91, 35.02) | |||||||||
| Johnson [29••] | Cross sectional | 115379 | Multi-site | Grades 9–12 | 50% | 50% | 1999–2009 (44%–37%), 2009 (41%) | – | – | Despite lenient changes in marijuana policies throughout the US, marijuana use among high school students has been declining. |
| Musci, 2015 | Longitudinal | 556 | Baltimore, MD | 11.88–17.81 | 46% | 54% | – | - Gene x environment for tobacco: OR = 1.33 | - p = 0.038 | - Taking the interaction into account, most users of marijuana and tobacco were shown to have social environments with low parent monitoring and friends that used substances (not limited to marijuana and tobacco) |
| - Gene x environment for marijuana OR = 0.10 | - p = 0.046 | |||||||||
| Johnson [43] | Cross sectional | 735352 | Multi-site, US | Grades 9-12 | – | – | 22.7% (MML states) | - aOR = 0.93 | - 95% CI: 0.86–0.89 | Medical marijuana law enactment and its inclusion of more liberalized provisions were associated with slightly lowered odds of past 30-day marijuana use. |
| 19.8% (non-MML states) | - aOR = 0.98 | - 95% CI: 0.96–0.998 | ||||||||
| Johnson [42] | Cross sectional | 715014 | Multi-site, US | Grades 9–12 | – | – | – | - 0.92 | - 95% CI: 0.87-0.97; p < 0.05 | - Medical Marijuana laws enactment was associated with decreased odds of past 30 day alcohol use, past 30 day alcohol and marijuana use. |
| - 0.93 | - 95% CI: 0.87-0.99; p < 0.05 | - States with less restrictive medical marijuana laws had decreased odds of past 30 day alcohol and marijuana use. | ||||||||
| - 0.94 | - 95% CI: (0.92-0.97); p < 0.001 | |||||||||
| - 0.96 | - 95% CI: (0.94, 0.99; p < 0.05 | |||||||||
| Ninnemann [27] | Longitudinal | 964 | Galveston, TX | Grades 9–12 | 56% | 44% | – | aOR = 0.60 | - p = .005 | - Plant-based marijuana use was predictive of subsequent synthetic cannabinoid use, but synthetic cannabinoid use was not predictive of later marijuana use. |
| aOR = 0.50 | - p = .046 | - Females and African Americans were less likely to use synthetic cannabinoids compared to males, and other races respectively. | ||||||||
*Abbreviations used- PSAT (Paced Serial Addition Test); aPR (adjusted Prevalence Ratio); CI (Confidence Interval); OR (odds Ratio); PCA (Principal Component Analysis); aOR (Adjusted Odds Ratio); ANCOVA (Analysis of Covariance); RCT (Randomized Controlled Trials); CHR (Clinical High Risk).
CRediT authorship contribution statement
Elena Cyrus: Conceptualization, Methodology, Formal analysis, Validation, Writing - original draft, Supervision, Project administration. Makella S Coudray: Methodology, Formal analysis, Investigation, Writing - original draft. Sandra Kiplagat: Methodology, Formal analysis, Investigation, Writing - original draft. Yandra Mariano: Formal analysis, Investigation, Writing - original draft. Ines Noel: Investigation, Writing - original draft. Jerome T Galea: Writing - review & editing. Dexter Hadley: Writing - review & editing. Jessy G Dévieux: Writing - review & editing. Eric Wagner: Writing - review & editing.
References
- 1.Anthony J.C., Lopez-Quintero C., Alshaarawy O. Cannabis epidemiology: a selective review. Curr Pharm Des. 2016:6340–6352. doi: 10.2174/1381612822666160813214023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Office of Adolescent Health: Marijuana Use in Adolescence. U.S. Department of Health & Human services.
- 3•.Hammond C.J., Chaney A., Hendrickson B., Sharma P. Cannabis use among U.S. adolescents in the era of marijuana legalization: a review of changing use patterns, comorbidity, and health correlates. Int Rev Psychiatry. 2020:4194. doi: 10.1080/09540261.2020.1713056. [DOI] [PMC free article] [PubMed] [Google Scholar]; This review concluded that marijuana policy changes have mixed effects on U.S. adolescent health. Evidence suggests that there are increased motor vehicle accidents and emergency room visits due to increased cannabis use. There are also potential bene®ts from decriminalization.
- 4.Gordon A.J., Conley J.W., Gordon J.M. Medical consequences of marijuana use: a review of current literature. Curr Psychiatry Rep. 2013:4194. doi: 10.1007/s11920-013-0419-7. [DOI] [PubMed] [Google Scholar]
- 5.Cerdá M., Mauro C., Hamilton A., et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. 2019;77:165–171. doi: 10.1001/jamapsychiatry.2019.3254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hasin D.S. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology. 2018:195–212. doi: 10.1038/npp.2017.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopez-Quintero C., Neumark Y. Effects of risk perception of marijuana use on marijuana use and intentions to use among adolescents in Bogotá, Colombia. Drug Alcohol Depend. 2010:65–72. doi: 10.1016/j.drugalcdep.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 8.Galván G., Guerrero-Martelo M., Vásquez De la Hoz F. Cannabis: a cognitive illusion. Rev Colomb Psiquiatr (English ed) 2017:95–102. doi: 10.1016/j.rcpeng.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 9.ElSohly M.A., Mehmedic Z., Foster S., Gon C., Chandra S., Church J.C. Changes in cannabis potency over the last 2 decades (1995-2014): analysis of current data in the United States. Biol Psychiatry. 2016:613–619. doi: 10.1016/j.biopsych.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lubman D.I., Cheetham A., Yücel M. Cannabis and adolescent brain development. Pharmacol Ther. 2015:1–16. doi: 10.1016/j.pharmthera.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 11••.Gobbi G., Atkin T., Zytynski T., et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry. 2019:426–434. doi: 10.1001/jamapsychiatry.2018.4500. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors conducted a systematic review and meta-analysis which concluded that adolescent cannabis use was signi®cantly increased the likelihood of depression, suicidal ideation and suicidal attempt.
- 12.Hansen C. 2020. Coronavirus Pandemic Boosts Marijuana Sales While Many Businesses Struggle. [Google Scholar]
- 13.Well Being Trust: The COVID Pandemic Could Lead to 75,000 Additional Deaths from Alcohol and Drug Misuse and Suicide. Well Being Trust & The Robert Graham Center Analysis.
- 14.Act now to get ahead of a mental health crisis, specialists advise U.S.Yuki Noguchi: The Coronavirus Crisis.
- 15.VanDolah H.J., Bauer B.A., Mauck K.F. Clinicians’ guide to cannabidiol and hemp oils. Mayo Clin Proc. 2019;94:1840–1851. doi: 10.1016/j.mayocp.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Camchong J., Lim K.O., Kumra S. Adverse effects of cannabis on adolescent brain development: a longitudinal study. Cereb Cortex. 2017;27:1922–1930. doi: 10.1093/cercor/bhw015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scott J.C., Slomiak S.T., Jones J.D., Rosen A.F.G., Moore T.M., Gur R.C. Association of cannabis with cognitive functioning in adolescents and young adults. JAMA Psychiatry. 2018;75:585. doi: 10.1001/jamapsychiatry.2018.0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Becker M.P., Collins P.F., Lim K.O., Muetzel R.L., Luciana M. Longitudinal changes in white matter microstructure after heavy cannabis use. Dev Cogn Neurosci. 2015;16:23–35. doi: 10.1016/j.dcn.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sweeney M.M., Rass O., DiClemente C., et al. Working memory training for adolescents with cannabis use disorders: a randomized controlled trial. J Child Adolesc Subst Abuse. 2018;27:211–226. doi: 10.1080/1067828X.2018.1451793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20•.Scott J.C., Wolf D.H., Calkins M.E., et al. Cognitive functioning of adolescent and young adult cannabis users in the Philadelphia neurodevelopmental cohort. Psychol Addict Behav. 2017;31:423–434. doi: 10.1037/adb0000268. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study systematically assessed current literature on the association between adolescent cannabis use and cognitive function. The authors concluded that frequent of heavy cannabis use had deleterious effects on cognitive function. This was not affected by current age or age of onset of cannabis use..
- 21.Reboussin B.A., Green K.M., Milam A.J., Furr-Holden D.M., Johnson R.M., Ialongo N.S. The role of neighborhood in urban black adolescent marijuana use. Drug Alcohol Depend. 2015;154:69–75. doi: 10.1016/j.drugalcdep.2015.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knopf A. Nonwhite youth have more academic problems on alcohol and marijuana than white youth. Brown Univ Child Adolesc Behav Lett. 2016;32:4–5. [Google Scholar]
- 23.Buchy L., Seidman L.J., Cadenhead K.S., et al. Evaluating the relationship between cannabis use and IQ in youth and young adults at clinical high risk of psychosis. Psychiatry Res. 2015;230:878–884. doi: 10.1016/j.psychres.2015.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meier M.H., Hill M.L., Small P.J., Luthar S.S. Associations of adolescent cannabis use with academic performance and mental health: a longitudinal study of upper middle class youth. Drug Alcohol Depend. 2015:207–212. doi: 10.1016/j.drugalcdep.2015.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Musci R.J., Uhl G., Maher B., Ialongo N.S. Testing gene × environment moderation of tobacco and marijuana use trajectories in adolescence and young adulthood. J Consult Clin Psychol. 2015:866–874. doi: 10.1037/a0039537. [DOI] [PubMed] [Google Scholar]
- 26••.Mason M.J., Mennis J. Young urban adolescents’ activity spaces, close peers, and the risk of cannabis use: a social-spatial longitudinal analysis. Subst Use Misuse. 2018:2032–2042. doi: 10.1080/10826084.2018.1452260. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors conducted a longitudinal social-spatial analysis which concluded that increased cannabis use was associated with preference for city places and adolescents with risky peer networks.
- 27.Ninnemann A.L., Choi H.J., Stuart G.L., Temple J.R. Longitudinal predictors of synthetic cannabinoid use in adolescents. Pediatrics. 2017:e20163009. doi: 10.1542/peds.2016-3009. [DOI] [PubMed] [Google Scholar]
- 28.Mead A. The legal status of cannabis (marijuana) and cannabidiol (CBD) under U.S. Law. Epilepsy Behav. 2017:288–291. doi: 10.1016/j.yebeh.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 29••.Johnson R.M., Fairman B., Gilreath T., et al. Past 15-year trends in adolescent marijuana use: differences by race/ethnicity and sex. Drug Alcohol Depend. 2015:8–15. doi: 10.1016/j.drugalcdep.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study analysed data from the National Youth Risk Behavior Survey and concluded that Despite considerable changes in state marijuana policies over the past 15 years, marijuana use among high school students has largely declined. Their ®ndings also illustrated that the prevalence of past 30 day marijuana use from 1999±2013 was lowest among Asians and highest among American Indians/Alaskan Natives. The differences between male-female marijuana use decreased over time.
- 30.Card D., Rothstein J. Racial segregation and the black-white test score gap. J Public Econ. 2007:2158–2184. doi: 10.1016/j.jpubeco.2007.03.006. [DOI] [Google Scholar]
- 31.Fauci Anthony S., Lane C., Redfield R. Covid-19 — navigating the uncharted. N Engl J Med. 2020;382:1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatry. 2020:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Corroon J.M., Mischley L.K., Sexton M. Cannabis as a substitute for prescription drugs - a cross-sectional study. J Pain Res. 2017:989–998. doi: 10.2147/JPR.S134330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kosiba J.D., Maisto S.A., Ditre J.W. Patient-reported use of medical cannabis for pain, anxiety, and depression symptoms: systematic review and meta-analysis. Soc Sci Med. 2019:181–192. doi: 10.1016/j.socscimed.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 35.Griffith L.E., Van Den Heuvel E., Fortier I., et al. Statistical approaches to harmonize data on cognitive measures in systematic reviews are rarely reported. J Clin Epidemiol. 2015:154–162. doi: 10.1016/j.jclinepi.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Piontek D., Kraus L., Klempova D. Short scales to assess cannabis-related problems: a review of psychometric properties. Subst Abuse Treat Prev Policy. 2008:25. doi: 10.1186/1747-597X-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eubank S., Eckstrand I., Lewis B., Venkatramanan S., Marathe M., Barrett C.L., Commentary on Ferguson, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. Bull Math Biol. 2020:1–7. doi: 10.1007/s11538-020-00726-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferguson N.M., Laydon D., Nedjati-Gilani G., et al. ImperialAcUk; 2020. Impact of Non-pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gt Walker P., Whittaker C., Watson O., et al. The global impact of COVID-19 and strategies for mitigation and suppression. Imp Coll COVID-19 Response Team. 2020:413–422. doi: 10.1126/science.abc0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Torales J., O’Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020:317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 41.DISA Global Solutions: Map of Marijuana Legality by State. https://disa.com/map-of-marijuana-legality-by-state.
- 42.Johnson J.K., Johnson R.M., Hodgkin D., Jones A.A., Matteucci A.M., Harris S.K. Heterogeneity of state medical marijuana laws and adolescent recent use of alcohol and marijuana: Analysis of 45 states, 1991-2011. Subst Abuse. 2018;39(2):247–254. doi: 10.1080/08897077.2017.1389801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson J., Hodgkin D., Harris S.K. The design of medical marijuana laws and adolescent use and heavy use of marijuana: Analysis of 45 states from 1991 to 2011. Drug Alcohol Depend. 2017;170:1–8. doi: 10.1016/j.drugalcdep.2016.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]