Effective and empathetic communication skills have always been the foundation of excellent patient care. With the coronavirus disease 2019 (COVID-19) pandemic, these skills have become even more critical considering the potential severity of illness and high mortality rate in vulnerable populations. This is an opportune time to underscore the importance of goals of care conversations (GOC) and advance care planning (ACP). These types of discussions are often referred to under the umbrella of serious illness conversations (SIC). Serious illness conversations outline the “overall priorities and health expectations for care … based on [a patient’s] personal values, wishes, beliefs, and perception of quality of life, and what they characterize as meaningful and important.”1 Both GOC and ACP are dialogues between health care providers, patients, and—ideally—patients’ substitute decision makers (SDMs). The main difference between ACP and GOC is the context of the decision making. Where ACP is a discussion of future preferences, GOC relates to medical decision making in the moment.2
A 2014 review of the literature notes that SIC primarily occur with health care providers who are not familiar with a patient’s clinical circumstances.3 As such, primary care physicians are best positioned to initiate these conversations.3 Studies have found that early SIC lead to benefits including improved quality of life, reductions in anxiety and depression, and a decreased risk of aggressive medical interventions at the end of life.3–5 Despite the importance of these conversations, many physicians do not feel prepared to take on discussions of this type, as they were never trained to do so.3 Evidence supports that communication skills can be learned and improved, just like any medical procedure.4,6
Best practices in teaching SIC
The best approach to teaching SIC is interactive case-based sessions with communication skills practice.3 This more formal, curricular approach to teaching SIC does not preclude learning about SIC in the workplace. Preceptors teaching about SIC from the office to the hospital environment can assist learners through preparation, direct observation, support, and feedback. This is an ideal opportunity to take a flipped classroom approach. The preceptor can provide the learner with helpful resources to review ahead of the patient encounter (Table 1).7,8 Reviewing a selected framework or approach before the conversation, along with relevant clinical details, helps to set the stage for the encounter.
Table 1.
Serious illness conversation resources
| RESOURCE NAME | AUTHOR | DESCRIPTION | LINK |
|---|---|---|---|
| Approaches to Goals of Care Discussion7 | Ontario Palliative Care Network | PDF tool outlining a framework and suggested language to guide GOC | https://www.ontariopalliativecarenetwork.ca/sites/opcn/files/ApproachesToGoalsOfCare.pdf |
| Improving Your Goals of Care Conversations | Dr Leah Steinberg and Dr Christine Soong, Sinai Health System | Open-source, case-based e-module that guides learners through the steps of GOC | http://www.goalsofcaremodule.com |
| Serious Illness Conversation Guide (Figure 1)8 | Ariadne Labs | PDF of an evidence-based tool that outlines a framework and suggested language to guide GOC | https://www.ariadnelabs.org/wp-content/uploads/sites/2/2017/05/SI-CG-2017-04-21_FINAL.pdf |
| Address Goals of Care | Vital Talk | Web-based, evidence-informed tools, suggested language, and videos for GOC | https://www.vitaltalk.org/topics/reset-goals-of-care/ |
| CAPC COVID-19 Response Resources | CAPC | Open-source, COVID-19–specific conversation guides and videos | https://www.capc.org/toolkits/covid-19-response-resources/ |
| COVID-19 Goals of Care Communication Guide for Clinicians | Dr Katie Marchington, Postgraduate Medical Education, University of Toronto | 5-min video outlining steps to GOC | https://www.youtube.com/watch?v=FZtBLdsuh_I |
| Advance Care Planning Resource Library | Speak Up Canada | Resource library of videos, workbooks, and decision aids for ACP; includes links to province-specific resources | https://www.advancecareplanning.ca/resource-library/ |
| Powers of Attorney | Government of Ontario | PDF containing instructions and forms for continuing power of attorney for property and power of attorney for personal care | https://www.attorneygeneral.jus.gov.on.ca/english/family/pgt/poa.pdf |
ACP—advance care planning, CAPC—Centre for the Advancement of Palliative Care, COVID-19—coronavirus disease 2019, GOC—goals of care conversations.
Direct observation of the learner in this setting has multiple benefits, such as facilitating specific feedback to support performance improvement. Direct observation also allows the preceptor to step in if the learner requires assistance or guidance. If the patient or SDM is well known to the preceptor, this helps set a foundation of trust in the clinical encounter, while allowing for the addition of necessary biopsychosocial context. The presence of the preceptor also allows modeling of communication skills for learners who prefer to observe the preceptor facilitating SIC before leading these conversations themselves.
Part of the preceptor’s role is to underscore that these conversations are iterative in nature. So often, there is a hidden agenda of confirming a do-not-resuscitate order in SIC. The ultimate goal is to explore how a patient’s values and wishes link to medical treatment preferences. It is important for learners to understand that not securing a do-not-resuscitate order is not considered a failure of this process.
Step-by-step approach to SIC
First, it must be emphasized that a high-quality SIC curriculum or teaching experience should begin with communication skills development. These skills include active listening, deciding how to break bad news, and responding empathetically. A key teaching point is to talk less and listen more.
Second, there are several frameworks that standardize SIC, including the Serious Illness Conversation Guide, Vital Talk’s REMAP (reframe, expect emotion, map out patient goals, align with goals, and propose a plan) framework, and local adaptations such as the Ontario Palliative Care Network’s approach to GOC (Table 1 and Figure 1).4,6–9 No matter the framework used, they all share the same basic structure.
Figure 1.
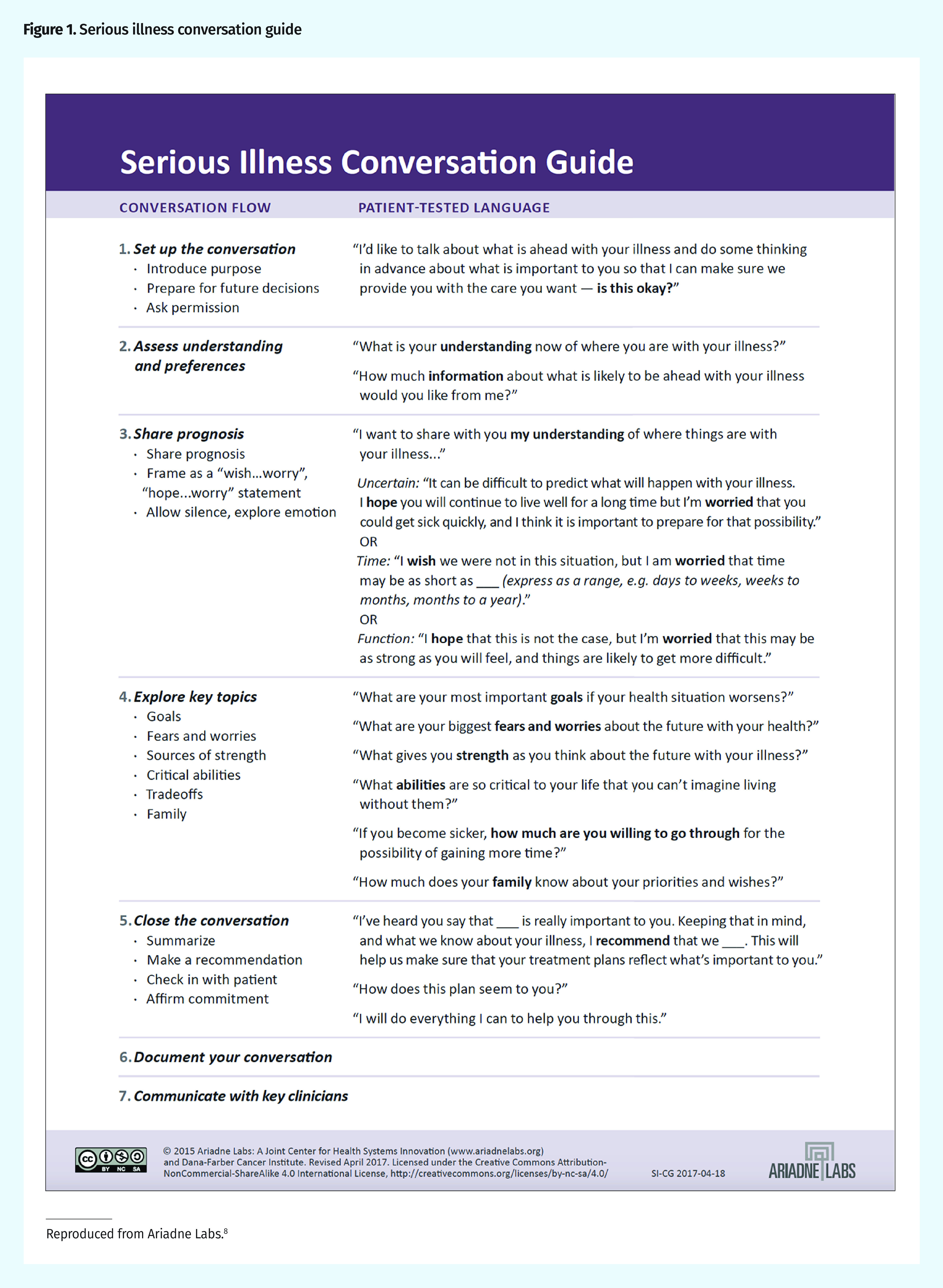
Serious illness conversation guide
Reproduced from Ariadne Labs.8
Substitute decision maker.
Ideally, a patient’s SDM will be present for the conversation, as it is vital to prepare SDMs for future decision making. Learners must be taught how to identify a patient’s SDM using provincial law. If an SDM is identified, this should be documented in the electronic medical record.
Illness understanding.
Learners must be taught to explore patients’ understanding of their own illnesses before providing any updates or clarifications. It is known that patients retain about 50% or less of medical information, and a further 25% is remembered incorrectly.10 By allowing the patient to do the talking, the learner can establish the patient’s understanding of previously given medical information and identify any knowledge gaps that might need to be clarified.
Information.
It is valuable to instruct learners to first ask if the patient has any questions. This allows the patient to free his or her mind of questions he or she has been waiting to ask, allowing the patient to focus on medical updates. This is also an opportunity to ask the patient how much he or she would like to know about his or her current medical condition. When giving information, learners should be taught to do so in a concise manner that imparts both the information and its meaning.
Values and goals.
Patients’ values and life experiences drive their decision making. Exploring values often begins with asking “Given the recent changes in your health, what is most important to you?” These values must then be distilled into information that is helpful in the setting of medical decision making. For example, if a patient shares that family is most important to him or her, a follow-up inquiry could be “Tell me about who is important to you and what you enjoy doing with them.” The learner might discover that the patient values sharing stories and laughing with family. This information can then be applied to future decision making. If the patient were to lose the ability to communicate and share stories owing to a medical illness, he or she might not consider that to be a meaningful quality of life. Learners should be instructed to probe deeper to discover what makes life meaningful to patients.
Function or trade-offs.
It might be useful to explain this section as an inquiry into what physical or cognitive abilities a patient might be willing to lose for the chance to live longer. As in the example above, the learner could ask “If you were in a situation where you were no longer able to share stories with your family, would that be a meaningful life for you?” Learners should be reminded that these conversations help to determine how a person wants to live and are not meant to focus on death.
Treatment plan (if a conversation regarding goals of care occurs).
After establishing illness understanding and identifying a patient’s values and acceptable quality of life, a treatment plan should be recommended. Rather than presenting treatment options as a menu, residents should be taught to provide patient-centred recommendations and aim for shared decision making. Using the example above, if the patient were to experience a severe stroke with little chance of cognitive recovery, and a decision needed to be made about using a feeding tube, then the learner could say to the SDM “Unfortunately, your loved one has suffered a severe stroke and is unlikely to verbally communicate again. Given that he most valued communicating with family, I do not recommend that we proceed with a feeding tube as it will not help achieve the quality of life that he described as meaningful.”
Code status.
Code status can best be addressed once a patient’s values are known. At that point, a recommendation should be given on whether life-sustaining therapies are likely to allow a patient to meet his or her goals and live a life that he or she has indicated would be meaningful.
Documentation.
It is imperative that family medicine learners be trained to document all SIC, ideally using headings and point-form notation, to impart the details of the conversation.
Conclusion
Primary care physicians are well positioned to engage in SIC with patients. Teaching SIC starts with communication skills development, followed by practice in a workplace setting or role-play with a step-by-step framework to clarify patient knowledge gaps and identify their goals and values.
Teaching tips
▸ Effective teaching of serious illness conversations (SIC) should first focus on communication skills development, including the role of empathy. Use guides, tools, or frameworks to teach learners efficient, thorough, patient-centred communication.
▸ The key components of SIC include establishing illness understanding, identifying a substitute decision maker, providing clinical information, determining values and goals, exploring trade-offs, and making a recommendation for the plan of care.
▸ Values-based SIC put the focus on how patients want to live and not how they want to die.
▸ Learners should be instructed to document all SIC, especially if a substitute decision maker is identified or resuscitation preferences are decided.
▸ Teaching should be practical, with learners having the opportunity to role-play or practise in the workplace.
Teaching Moment is a quarterly series in Canadian Family Physician, coordinated by the Section of Teachers of the College of Family Physicians of Canada. The focus is on practical topics for all teachers in family medicine, with an emphasis on evidence and best practice. Please send any ideas, requests, or submissions to Dr Viola Antao, Teaching Moment Coordinator, at viola.antao@utoronto.ca.
Footnotes
Competing interests
None declared
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de juillet 2020 à la page e193.
References
- 1.Health Quality Ontario and Ontario Palliative Care Network . Quality standards – palliative care: care for adults with a progressive life-limiting illness. Toronto, ON: Health Quality Ontario; 2018. Available from: https://www.hqontario.ca/portals/0/documents/evidence/quality-standards/qs-palliative-care-clinical-guide-en.pdf. Accessed 2020 Apr 16. [Google Scholar]
- 2.Myers J, Cosby R, Gzik D, Harle I, Harrold D, Incardona N, et al. Provider tools for advance care planning and goals of care discussions: a systematic review. Am J Hosp Palliat Care. 2018;35(8):1123–32. doi: 10.1177/1049909118760303. Epub 2018 Mar 12. [DOI] [PubMed] [Google Scholar]
- 3.Bernacki RE, Block SD, American College of Physicians High Value Care Task Force Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994–2003. doi: 10.1001/jamainternmed.2014.5271. [DOI] [PubMed] [Google Scholar]
- 4.Bernacki R, Paladino J, Neville BA, Hutchings M, Kavanagh J, Geerse OP, et al. Effect of the Serious Illness Care Program in outpatient oncology: a cluster randomized clinical trial. JAMA Intern Med. 2019;179(6):751–9. doi: 10.1001/jamainternmed.2019.0077. Epub 2019 Mar 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paladino J, Bernacki R, Neville BA, Kavanagh J, Miranda SP, Palmor M, et al. Evaluating an intervention to improve communication between oncology clinicians and patients with life-limiting cancer: a cluster randomized clinical trial of the Serious Illness Care Program. JAMA Oncol. 2019;5(6):801–9. doi: 10.1001/jamaoncol.2019.0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tulsky JA, Arnold RM, Alexander CS, Olsen MK, Jeffreys AS, Rodriguez KL, et al. Enhancing communication between oncologists and patients with a computer-based training program: a randomized trial. Ann Intern Med. 2011;155(9):593–601. doi: 10.1059/0003-4819-155-9-201111010-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ontario Palliative Care Network . Approaches to goals of care discussions. Toronto, ON: Ontario Palliative Care Network; 2017. Available from: https://www.ontariopalliativecarenetwork.ca/sites/opcn/files/ApproachesToGoalsOfCare.pdf. Accessed 2020 Jun 5. [Google Scholar]
- 8.Ariadne Labs [website] Serious illness conversation guide. Boston, MA: Ariadne Labs; 2015. Available from: www.ariadnelabs.org/wp-content/uploads/sites/2/2017/05/SI-CG-2017-04-21_FINAL.pdf. Accessed 2020 Jun 5. [Google Scholar]
- 9.Childers JW, Back AL, Tulsky JA, Arnold RM. REMAP: a framework for goals of care conversations. J Oncol Pract. 2017;13(10):e844–50. doi: 10.1200/JOP.2016.018796. Epub 2017 Apr 26. [DOI] [PubMed] [Google Scholar]
- 10.Kessels RPC. Patients’ memory for medical information. J R Soc Med. 2003;96(5):219–22. doi: 10.1258/jrsm.96.5.219. [DOI] [PMC free article] [PubMed] [Google Scholar]


