ABSTRACT
Objective:
To investigate (1) the concurrent validity of the Nursing Home Life-Space Diameter (NHLSD) and the Home-based Life-Space Assessment (Hb-LSA), (2) the correlated factors of life-space, and (3) the factors that affected the NHLSD score for the elderly in a geriatric health service facility, or Roken.
Methods:
This cross-sectional study included 32 participants in a Roken. Staff members, who had received essential guidance for assessment, examined the cognitive function, physical function, mood, communication ability, objective quality of life, vitality, and daily behavior of the participants. Correlation analysis between NHLSD and other measurements and multiple regression analysis with NHLSD as a dependent variable were conducted.
Results:
NHLSD and Hb-LSA were significantly correlated (r=0.710, P<0.01). NHLSD was significantly correlated with more measurements than Hb-LSA was; i.e., NHLSD was significantly correlated with communication ability, independence of daily living (Barthel Index; BI), maximum knee extension strength, grip strength, function in daily living, and three QOL measurements: positive affects, ability to communicate, and spontaneity and activity. A stepwise multiple regression analysis indicated that the BI total score, the maximum knee extension strength, and spontaneity and activity (one of the QOL items) were significantly correlated with the NHLSD score.
Conclusions:
NHLSD can measure the mobility levels of elderly persons in Roken. In addition to physical conditions and dependence of ADLs, spontaneity (or low levels of apathy) may be an important factor for promoting physical activity in Roken.
Keywords: life-space, physical activity, rehabilitation, wheel chair
INTRODUCTION
For the elderly, decreased physical activity raises the risks of morbidity from other diseases, mortality, falls, and the progression of cognitive decline.1,2,3,4) Certain amounts of physical activity are considered to extend healthy life expectancy for elderly persons, especially in residential facilities where residents tend to spend their time passively and find it difficult to maintain their usual routines.5,6) Although the inactivity of institutionalized elderly persons who need daily life assistance is a major issue, few studies have been published regarding the effects of inactivity or the factors that promote physical activity in institutionalized settings.
In Japan, geriatric health service facilities, or Roken, are transitional facilities between hospital and home, and they have an important role in promoting community-based care at home to reduce hospitalization.7) Recently, Roken have been required to facilitate more patients to return home. Hamaoka et al.8) surveyed changes in independence levels of daily living for community-dwelling chronic stroke patients. They revealed that low-activity subjects and those needing care had significantly reduced activities of daily living (ADLs, as measured by the Barthel Index), and the living area was an independent factor of changes in ADLs. This study indicated that not only increasing the independence level for ADLs but also promoting physical activity are important factors to promote returning home. This study suggested that expansion of the life-space influences changes in ADLs for stroke patients, and this suggestion may be generalized to elderly persons with physical disabilities.
There are three methods for measuring physical activity: pedometers, accelerometers, and questionnaires9,10,11). For elderly persons with physical disabilities, questionnaires may be preferable; it may be difficult for them to set pedometers or accelerometers to accurately measure physical activity,12) or the presence of such devices may make them uncomfortable. Tinetti et al.13) developed the Nursing Home Life-Space Diameter (NHLSD) to measure optimal activity levels by directly assessing the extent and frequency of mobility for the elderly in nursing homes. Although NHLSD is reported to have high inter-rater reliability and test–retest reliability, to date, no study has examined the concurrent validity of NHLSD with other measurements of activity. In Japan, Ohnuma et al.12) developed the Home-based Life-Space Assessment (Hb-LSA) to evaluate life-space mobility for elderly people who require long-term care at home. The test–retest reliability, inter-rater reliability, concurrent validity, and convergent validity with life-space assessment and bed-leaving time have been confirmed. During our study, no life-space assessment for institutionalized older adults existed in Japan.
The NHLSD and Hb-LSA have similar structures, but a few differences exist. These assessments are observational scales that measure the subjects’ life-space by assessing three items to determine activity levels: the extent, frequency, and dependence of mobility. However, the scoring methods of activity extent and frequency are different. Moreover, it is not clear which method is most suitable for measuring life-space in Roken. For example, NHLSD evaluates the activity range by two out of four diameters between outside the bedroom to within the facility, but Hb-LSA evaluates by only one out of five diameters. It may be that NHLSD is preferable for the elderly in Roken who are often restricted from going outdoors. Therefore, we applied Hb-LSA, the validity of which has been already confirmed, for institutionalized older adults and evaluated whether NHLSD was suitable for assessing in the Roken setting.
There are few studies reporting the use of these measurements in institutionalized settings.13-16) Tinetti et al.13) reported that mobility and the extent of life-space were correlated with functional characteristics such as participation in social activities. Okamoto et al.14) reported that physical activity was correlated with cognitive function and muscle mass of the lower limbs. Jansen et al.15) carried out a cross-sectional study which assessed life-space using a wireless sensor network in a nursing home, and reported that gait speed, cognitive function, and depressive symptoms were associated with time spent away from a private room. However, most subjects in the above studies could walk with/without aids. Therefore, we were interested in whether the findings from these studies could be applied to elderly persons in Roken, who mostly use wheel chairs.16)
The present study had three aims: (1) to investigate the concurrent validity of NHLSD and Hb-LSA, (2) to search for correlated factors of life-space, and (3) to determine the factors that affect the NHLSD score in Roken for elderly persons with physical disabilities.
METHODS
Study Design
The present study was a cross-sectional study performed in a Roken.
Participants
Subjects in the geriatric health facility who met the following criteria were invited to participate in the present study: (1) being able to walk or navigate a wheel chair with/without human assistance regardless of independent transfer, (2) not having severe auditory or visual impairments, and (3) not having severe cognitive impairment, i.e., having a Mini-Mental State Examination (MMSE)17) score of 5 to 25.
Assessment
Before assessment, four chief care staff members (mean years of experience: 20.3 ± 0.5) learned the essential assessment methods (e.g., the aims of assessments and the scoring methods). These care staff members assessed participants using three observation scales, the Nurses’ Observation Scale for Geriatric Patients (NOSGER),18) the health-related Quality of Life Questionnaire for the Elderly with Dementia in Japan (QOL-D),19) and the Dementia Behavior Disturbance Scale (DBD scale).20) NOSGER deals with the daily behavior of elderly patients and measures impairment in six dimensions: (i) memory, (ii) instrumental activities of daily living, (iii) activities of daily living, (iv) mood, (v) social behavior, and (vi) disturbing behavior. The higher the total score is, the more subjects need to be helped. NOSGER is reported to have high inter-rater reliability (rtt=0.68–0.89), retest reliability (rs=0.80–0.90), and correlation with psychometric standards. QOL-D is an observational measurement of QOL in elderly persons with dementia. This measurement evaluates the QOL in six response sets: positive affects, negative affects and actions, restlessness, ability to communicate, attachment to others, and spontaneity and activity. QOL-D is reported to have high inter-rater reliability (rtt=0.63–0.93) and high internal consistency (Cronbach’s α=0.79–0.91). The DBD scale is an objective assessment of behavioral disturbance for persons with dementia. This scale is reported to have high test–retest reliability (rs=0.96), internal consistency (Cronbach’s α=0.95), and inter-rater reliability (rtt=0.71±0.10).20)
Two physical therapists assessed the maximum knee extension strength, grip strength, and life-space in the facility (using both Hb-LSA12) and NHLSD13)). The maximum knee extension strength was measured using a μTas F-100 (ANIMA, Tokyo, Japan), and the maximum of two measurements from the right and left legs was selected. In the same way, grip strength was measured with a Grip-D (Takei Scientific Instruments, Tokyo, Japan), and the maximum of two measurements on the dominant side or the nonparetic side was selected as representative data.
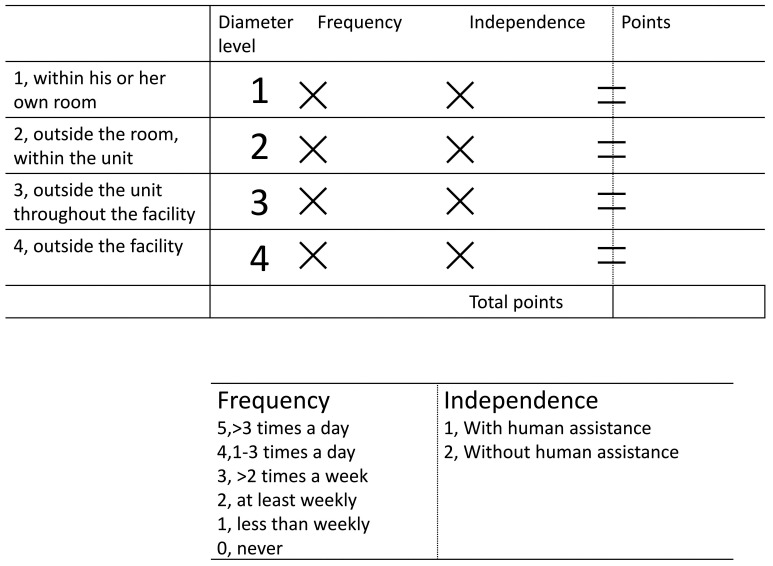
NHLSD (Fig. 1) measures the participants’ life-space over a 2-week period by assessing three items that represent activity levels: the extent, frequency, and dependence of mobility. NHLSD has high inter-rater reliability (rtt=0.951) and retest reliability (rs=0.922). NHLSD was moderately correlated with the dependency of ADLs such as eating (r=0.526), bathing (r=0.510), and frequency of participation in social activities (r=0.565).13) Hb-LSA measures participants’ life-space over a 1-month period by assessing the same three items as NHLSD. The main difference between Hb-LSA and NHLSD is the extent of the measured activity. Hb-LSA measures the extent of movement in five areas: “in bed”, “in the bedroom”, “between the bedroom and another room”, “outdoors in a site of the home”, and “outside from the site of home”. To apply the assessment to institutionalized older adults, we regarded “in a site of the home” to be “in a site of the facility”, and “outside the home” as “outside the facility”. To evaluate NHLSD and Hb-LSA, two physical therapists directly observed the subjects and assessed the overall life-space and whether assistance was required.
Fig. 1.
Assessment table to calculate the Nursing Home Life-Space Diameter (NHLSD). NHLSD measures the participants’ life-space over a 2-week period. NHLSD is the sum of the scores of each diameters: NHLSD = Diameter1 * Frequency1 (i) * Dependence1 (j) + Diameter2 * Frequency2 (i) *Dependence2 (j) + Diameter3 * Frequency3 (i) * Dependence3 (j) + Diameter4 *Frequency4 (i) * Dependence4 (j): i=0 to 5, j=1 or 2
Three occupational therapists and two speech therapists assessed cognitive function (MMSE),17) mood (five-item Geriatric Depression Scale; GDS-521)), communication ability (Brief Communication Ability Scale; BCAS22)), apathy (Apathy Scale23)), and activities of daily living (Barthel Index; BI24)).
Ethical Considerations
This study was approved by the Ethical Review Board of Takasaki University of Health and Welfare (approval number: 2820). Written consent was obtained from each participant and their families after providing full information regarding the purpose of this study, the risks and benefits, confidentiality, anonymity, and freedom of participation.
Statistical Analysis
First, we confirmed the concurrent validity of NHLSD by analyzing the correlation between NHLSD and Hb-LSA using Pearson’s correlation coefficient. Before analyzing correlations with NHLSD, we confirmed the normality of the data distribution and the score range of the total NHLSD. Then, we investigated associations between NHLSD and other parameters. Finally, we conducted stepwise multiple regression analyses to reveal factors influencing life-space in institutionalized elderly persons using NHLSD scores as the dependent variable, and other measurements that were significantly correlated with NHLSD as independent variables. Before extracting variables for multiple regression analyses, we confirmed multicollinearity by examining whether the absolute values of the correlation coefficients exceeded 0.9. Data were analyzed using the Japanese version of SPSS Statistics for Windows version 23.0 (IBM Corporation, Armonk, NY, USA).
RESULTS
Table 1 shows the demographic data of the 32 participants who were enrolled in the present study.
Table 1. Demographic data.
| Mean ± SD, or n (%) | Median (min–max) | |
| Age (years) | 86.5 ± 6.6 | 87.5 (77–95) |
| Gender: male/female (n) | 5 (15.6)/27 (84.4) | |
| Care need level (n) | ||
| 1 | 4 (12.5) | |
| 2 | 9 (28.1) | |
| 3 | 11 (34.4) | |
| 4 | 7 (21.9) | |
| 5 | 1 (3.1) | |
| MMSE (points) | 15.6 ± 5.1 | 16 (8–25) |
| BI (points) | 56.9 ± 29.2 | 60 (15–95) |
| NHLSD (points) | 36.2 ± 11.5 | 29 (11–65) |
| Hb-LSA (points) | 31.0 ± 11.3 | 37 (16–60) |
| Causal disorders for institutionalization (n) ‡ | ||
| Cerebrovascular diseases | 8 (25.0) | |
| Orthopedic disorders | 13 (40.6) | |
| Pulmonary/cardiovascular diseases | 3 (9.4) | |
| Dementia | 3 (9.4) | |
| Others | 5 (15.6) | |
| Mobility (n) | ||
| Walking | 9 (28.1) | |
| Wheelchair | 23 (71.9) |
‡: Only the main causal diseases are stated.
Concurrent Validity and Distribution of NHLSD as an Assessment Tool for Life-space Mobility
The NHLSD score was significantly correlated with the Hb-LSA score (r=0.710, P<0.001). The mean NHLSD score for the 32 participants was 36.2 ± 11.5. Table 2 shows the NHLSD score distribution for the four assessed diameters. Almost all participants moved around within diameter 1 (bedrooms) and diameter 2 (outside the room, within the unit) at least once a day in the 2-week period of the assessment. In contrast, most participants moved around in diameter 3 (outside the unit, throughout the facility) once a week or less, and only 5 of 32 participants moved around in diameter 4 (outside the facility) within the two-week period.
Table 2. Score distribution of NHLSD.
| Frequency | Dependence | NHLSD score for each diameter Mean ± SD |
|||||||
| Diameter | 0 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | |
| 1: Within his or her own room | 0 | 0 | 0 | 1 (3.1) |
20 (62.5) |
11 (34.4) |
10 (31.3) |
22 (68.7) |
7.3 ± 2.3 |
| 2: Outside the room | 0 | 0 | 0 | 0 | 2 (6.3) |
30 (93.7) |
8 (25.0) |
24 (75.0) |
17.0 ± 4.6 |
| 3: Outside the unit throughout the facility | 2 (6.3) |
5 (15.6) |
13 (40.6) |
6 (18.8) |
6 (18.8) |
0 | 17 (53.1) |
15 (46.9) |
10.0± 6.4 |
| 4: Outside the facility | 27 (84.4) |
3 (9.4) |
2 (6.3) |
0 | 0 | 0 | 31 (96.9) |
1 (3.1) |
1.1 ± 3.3 |
| NHLSD total score | 36.2 ± 11.5 | ||||||||
Values in parentheses are percentages.
Frequency: 5, >3 times a day, 4, 1–3 times a day, 3, >2 times a week, 2, at least weekly, 1, less than weekly, 0, never.
Dependence: 2, without human assistance, 1, with human assistance.
Association Between NHLSD and Motor Function, Cognitive Function, and ADLs
Table 3 shows the associations between NHLSD and motor function, cognitive function, and dependence for ADLs. NHLSD significantly correlated with BCAS (r=0.422, P=0.016), BI (r=0.746, P<0.001), maximum knee extension strength (r=0.606, P<0.001), grip strength (r=0.516, P=0.003), NOSGER total score (r=−0.460, P=0.008), and three items of the QOL-D [positive affects (r=0.449, P=0.010), ability to communicate (r=0.400, P=0.023), and spontaneity and activity (r=0.523, P=0.002)]. For Hb-LSA, almost the same measurement items were correlated as for the NHLSD. However, QOL-D items were only significantly correlated using NHLSD.
Table 3. Association between NHLSD, Hb-LSA, and other parameters.
| NHLSD | Hb-LSA | |||
| Correlation coefficient | P value | Correlation coefficient | P value | |
| Hb-LSA (points) | 0.710* | <0.001 | − | |
| MMSE (points) | 0.349 | 0.050 | 0.335 | 0.061 |
| GDS-5 (points) | 0.051 | 0.781 | 0.043 | 0.813 |
| Apathy score (points) | −0.276 | 0.126 | −0.329 | 0.066 |
| BCAS (points) | 0.422* | 0.016 | 0.426* | 0.015 |
| BI total score (points) | 0.746* | <0.001 | 0.676 * | <0.001 |
| Motor function | ||||
| Maximum knee extension strength (kgf) | 0.606* | <0.001 | 0.446* | 0.015 |
| Grip strength (kgf) | 0.516* | 0.003 | 0.467* | 0.009 |
| NOSGER total score (points) | −0.460* | 0.008 | −0.415* | 0.018 |
| DBD Scale (points) | 0.093 | 0.618 | 0.075 | 0.687 |
| QOL-D (points) | ||||
| Positive affects | 0.449* | 0.010 | 0.079 | 0.667 |
| Negative affects | 0.091 | 0.625 | 0.150 | 0.420 |
| Communication | 0.400* | 0.023 | 0.101 | 0.584 |
| Restlessness | 0.116 | 0.536 | 0.270 | 0.142 |
| Attachment | 0.155 | 0.404 | −0.032 | 0.864 |
| Spontaneity | 0.523* | 0.002 | 0.155 | 0.398 |
QOL-D items: Negative affects, negative affects and actions; Communication, ability to communicate; Attachment, attachment to others; Spontaneity, spontaneity and activity. *P<0.05.
Factors That Affect NHLSD Score
Stepwise multiple regression analysis indicated that the BI total score (standardized partial regression coefficient: β= 0.490), maximum knee extension strength (β=0.368), and spontaneity and activity (one of the QOL-D items) (β=0.296) were significantly correlated with the NHLSD score (Table 4). There were no variables for which the absolute correlation value coefficients exceeded 0.9. The adjusted R2 of this regression analysis was 0.711. The Durbin-Watson statistic of this regression analysis was 2.543.
Table 4. Factors that affect the NHLSD score.
| Partial regression coefficient | Standardized partial regression coefficient | t-value | 95% CI | P value | ||
| Lower limit | Upper limit | |||||
| Constant | 2.40 | 0.558 | −6.447 | 11.236 | 0.582 | |
| BI total | 0.249 | 0.490 | 4.278 | 0.129 | 0.368 | <0.01 |
| Maximum knee extension strength | 0.930 | 0.368 | 3.361 | 0.360 | 1.499 | <0.01 |
| QOL-D Spontaneity and activity | 0.903 | 0.296 | 2.718 | 0.219 | 1.587 | 0.012 |
Stepwise multiple regression analysis was carried out using the NHLSD score as a dependent variable, and other measurements significantly correlated with NHLSD as independent variables. CI, confidence interval.
F-value: 23.983 (P<0.01), R2=0.742, adjusted R2=0.711, Durbin-Watson statistic: 2.543.
DISCUSSION
The present study investigated (1) the concurrent validity of NHLSD, (2) correlated factors with NHLSD, and (3) factors that affected the NHLSD score. We demonstrated that (1) NHLSD had significant concurrent validity, (2) NHLSD was significantly correlated with more measurements than Hb-LSA was [BCAS, BI, maximum knee extension strength, grip strength, NOSGER total score, and three items of QOL-D (positive affects, ability to communicate, and spontaneity and activity)], and (3) that the BI total score, the maximum knee extension strength, and spontaneity and activity were significantly associated with the NHLSD score.
Could NHLSD Evaluate Activity Levels for Institutionalized Elderly Persons in Roken?
NHLSD was significantly correlated with Hb-LSA (r=0.710, P<0.01). Moreover, NHLSD was significantly correlated with more measurements than Hb-LSA was, i.e., NHLSD was correlated with three QOL-D items, but Hb-LSA was not. Consequently, NHLSD may be measurable for the elderly in Roken. Because Hb-LSA includes some items unsuitable for Roken, such as inquiring about activities outside the premises (i.e., “outdoors in a site of the home” and “outside from the site of home”, NHLSD may be a more valid evaluation.
We found that almost all participants moved within their units at least once a day (in the bedroom: 96.9%, in their own units: 100%), whereas few participants moved outside the unit or facilities daily (outside the unit: 18.8%, outside the facility: 0%). Jansen et al.15) investigated activity levels in nursing homes using a wireless sensor network and revealed that almost all residents (90%) were restricted to private rooms and the surrounding living unit. den Ouden et al.5) researched activity in seven nursing homes by observing residents during five random observation times per day. They reported that residents were mainly observed in a lying or sitting position (range: 89%–92%). Ice6) investigated nursing home residents’ activities at 5-min intervals and revealed that residents spent 65% of their time doing little or nothing, and they spent the majority of their time in their rooms sitting alone. Although the difference between nursing homes in western countries and Roken is that nursing homes are the final residences, whereas Roken are intermediate facilities, these studies suggest that the activity levels of institutionalized elderly persons were quite low, as confirmed by our study. Jansen et al.5) inferred from these findings that “some nursing home residents may be worried by the thought of entering a less controlled environment” or “others may feel drawn out of isolation in their room towards more eventful places”. Furthermore, Ice6) indicated that these conditions of inactivity have continued since 1974, and that a more meaningful and enriched environment is required in nursing homes.
Associated Factors of Life-space for the Elderly in Roken
Multiple regression analysis demonstrated a significant association for NHLSD with three factors (in descending order of the standardized partial regression coefficient): BI total score (β= 0.490), maximum knee extension strength (β=0.368), and spontaneity and activity (one of the QOL-D items) (β=0.296).
Many studies have reported associations among life-space in community settings and physical performance,25,26) cognitive function,27) psychosocial factors,28) concerns about falling,29) and apathy.26) Webber et al.30) presented a conical model of the theoretical framework for mobility in older adults. This model is composed of mobility determinants related to cognitive, psychosocial, physical, environmental, and biographical influences. In institutionalized settings, the framework of Webber et al. has been partially validated by recent studies. For example, a cross-sectional study15) using a wireless sensor network to measure mobility in the life-space reported that gait speed, apathy, depressive symptoms, and institutional meal routines were the only modifiable predictors of time spent away from the private room. Another cross-sectional study31) investigated the association between mobility, participation, and wheel chair-related factors, such as wheel chair skills, in long-term care residents, and reported that wheel chair-related factors were associated with participation frequency through their relationship with mobility.
In the present study, we investigated the association between mobility in the life-space and cognitive, psychosocial, and physical factors, and confirmed the above studies except for two findings. First, we demonstrated that mobility in the life-space was not associated with cognitive function, which is different from the findings of Okamoto’s study.14) Differences in the conditions of the participants between the above study and ours (in terms of the mean MMSE score and BI total; those included in our study were mildly more disabled) may have caused this discrepancy. In other words, because some participants with moderate dementia may have wandered frequently in the facility, whereas participants with mild dementia may not have had a tendency to wander, life-space did not correlate with cognitive function. Second, stepwise multiple regression analysis for the NHLSD score indicated that the BI total score, maximum knee extension strength, and spontaneity and activity (one of the QOL-D items) were significantly correlated, in the above order with respect to the standardized partial regression coefficients. Institutionalized elderly persons who can move to many places by themselves may be required to perform several ADLs (particularly basic ADLs); this may explain why BI is most strongly associated with the NHLSD score. In addition, maximum knee extension strength plays an important role in independence in basic ADLs, such as transferring from the bed to the wheelchair,32) which is the first requirement for elderly persons to leave their rooms. Furthermore, spontaneity is greatly involved in improving QOL and independence of daily living,33) and spontaneity may be associated with the NHLSD score. To promote patient mobility in their life-space, not only dependence for ADLs and physical condition but also spontaneity are important. Therefore, interventions to raise motivation (e.g., by disclosing patients’ goal attainments or by planning programs which patients may enjoy, may feel attracted to, or which have individualized roles) are required.
The present study has some limitations. We did not assess wandering behavior adequately; therefore, the relation between life-space and wandering could not be discussed. Because of the cross-sectional nature of this study, causal relationships between mobility in the life-space and physical, cognitive, and psychosocial factors could not be elucidated. Although mobility in the life-space was measured using NHLSD, i.e., utilizing scores for measuring life-space and the frequency and independence of movement, it is difficult to assess how patients spend their time in their life-space, except during common hours such as mealtimes and tea time. We used Hb-LSA to confirm concurrent validity. Hb-LSA has a similar structure to that of NHLSD but also has a few differences in definitions of diameter and dependence. To further examine the validity of NHLSD, another evaluation using a different method is required. The number of participants we included was low, and we were unable to generalize the level of dementia and mobility. To analyze the results for each level of dementia and mobility, further research with increased numbers of participants is required. Therefore, our results must be interpreted with caution.
ACKNOWLEGMENTS
This publication was supported by JSPS KAKENHI Grant Number 17K18054.
Footnotes
CONFLICT OF INTEREST: The authors declare no conflicts of interest.
REFERENCES
- 1.Fries JF: Physical activity, the compression of morbidity, and the health of the elderly. J R Soc Med 1996;89:64–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kopperstad Ø,Skogen JC,Sivertsen B,Tell GS,Sæther SM: Physical activity is independently associated with reduced mortality: 15-years follow-up of the Hordaland Health Study (HUSK). PLoS One 2017;12:e0172932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klenk J,Kerse N,Rapp K,Nikolaus T,Becker C,Rothenbacher D,Peter R,Denkinger MD, ActiFE Study Group: Physical activity and different concepts of fall risk estimation in older people–results of the ActiFE-Ulm Study. PLoS One 2015;10:e0129098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Groot C,Hooghiemstra AM,Raijmakers PG,van Berckel BN,Scheltens P,Scherder EJ,van der Flier WM,Ossenkoppele R: The effect of physical activity on cognitive function in patients with dementia: a meta-analysis of randomized control trials. Ageing Res Rev 2016;25:13–23. [DOI] [PubMed] [Google Scholar]
- 5.den Ouden M,Bleijlevens MH,Meijers JM,Zwakhalen SM,Braun SM,Tan FE,Hamers JP: Daily (in)activities of nursing home residents in their wards: an observation study. J Am Med Dir Assoc 2015;16:963–968. [DOI] [PubMed] [Google Scholar]
- 6.Harper Ice G: Daily life in a nursing home. J Aging Stud 2002;16:345–359. [Google Scholar]
- 7.Toba K,Nakamura Y,Endo H,Okochi J,Tanaka Y,Inaniwa C,Takahashi A,Tsunoda N,Higashi K,Hirai M,Hirakawa H,Yamada S,Maki Y,Yamaguchi T,Yamaguchi H: Intensive rehabilitation for dementia improved cognitive function and reduced behavioral disturbance in geriatric health service facilities in Japan. Geriatr Gerontol Int 2014;14:206–211. [DOI] [PubMed] [Google Scholar]
- 8.Hamaoka K,Yoshimoto Y,Hashimoto T,Sato A: The life area of stroke patients living at home influences the changes in their activities of daily living. Rigakuryoho Kagaku 2012;27:465–468 [in Japanese with English abstract]. [Google Scholar]
- 9.Aoyagi Y,Shephard RJ: Habitual physical activity and health in the elderly: The Nakanojo Study. Geriatr Gerontol Int 2010;10(Suppl 1):S236–S243. [DOI] [PubMed] [Google Scholar]
- 10.Furuta K,Sasuga Y,Kazama K: Study on the relationship between physical activity and fitness in elderly living at home by using “Life Corder” and “Functional Fitness”. J Jpn Soc Nurs Health Care 2004;6:15–23 [in Japanese]. [Google Scholar]
- 11.Kitamura N,Sato T,Kawagoshi A,Satake M,Shioya T: Evaluation of physical activity in the daily life of healthy young subjects with special reference to the reliability and validity of IPAQ as evaluated by a triaxial accelerometer. Rigakuryoho Kagaku 2010;25:767–771 [in Japanese with English abstract]. [Google Scholar]
- 12.Ohnuma T,Hashidate H,Yoshimatsu T,Abe T: Clinical usefulness of indoor life-space assessment in community-dwelling older adults certified as needing support or care. Nippon Ronen Igakkai Zasshi. Jpn J Geriatr 2014;51:151–160. [DOI] [PubMed] [Google Scholar]
- 13.Tinetti ME,Ginter SF: The nursing home life-space diameter. A measure of extent and frequency of mobility among nursing home residents. J Am Geriatr Soc 1990;38:1311–1315. [DOI] [PubMed] [Google Scholar]
- 14.Okamoto S,Kawakubo K,Noda N: Relation between physical activities, nutrient intake, cognitive function in special nursing home for elderly. J Metab Clin Nutr 2011;14:141–149. [Google Scholar]
- 15.Jansen CP,Diegelmann M,Schnabel EL,Wahl HW,Hauer K: Life-space and movement behavior in nursing home residents: results of a new sensor-based assessment and associated factors. BMC Geriatr 2017;17:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Japan Association of Geriatric Health Service Facilities. Survey of rehabilitation in geriatric health service facilities. 2016. [in Japanese].
- 17.Folstein MF,Folstein SE,McHugh PR: “Mini-mental state”. J Psychiatr Res 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 18.Wahle M,Hller S,Spiegel R: Validation of the NOSGER (Nurses’ Observation Scale for Geriatric Patients): reliability and validity of a caregiver rating instrument. Int Psychogeriatr 1996;8:525–547. [DOI] [PubMed] [Google Scholar]
- 19.Terada S,Ishizu H,Fujisawa Y,Fujita D,Yokota O,Nakashima H,Haraguchi T,Ishihara T,Yamamoto S,Sasaki K,Nakashima Y,Kuroda S: Development and evaluation of a health-related quality of life questionnaire for the elderly with dementia in Japan. Int J Geriatr Psychiatry 2002;17:851–858. [DOI] [PubMed] [Google Scholar]
- 20.Mizoguchi T,Iijima S,Eto F,Ishizuka A,Orimo H: Reliability and validity of Japanese version of the dementia behavior disturbance scale. Nippon Ronen Igakkai Zasshi. Jpn J Geriatr 1993;30:835–840. [in Japanese with English abstract] [DOI] [PubMed] [Google Scholar]
- 21.Yesavage JA,Brink TL,Rose TL,Lum O,Huang V,Adey M,Leirer VO: Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1982-1983;17:37–49. [DOI] [PubMed] [Google Scholar]
- 22.Takeda A,Kawai Y,Hattori Y,Watanabe Y,Mizuno Y,Tabata O,Kawamura Y,Shibayama H,Sobue G: Development of a brief communication ability scale for Japanese demented elderly. Nippon Ronen Igakkai Zasshi. Jpn J Geriatr 2004;41:402–407 [in Japanese with English abstract]. [DOI] [PubMed] [Google Scholar]
- 23.Starkstein SE,Fedoroff JP,Price TR,Leiguarda R,Robinson RG: Apathy following cerebrovascular lesions. Stroke 1993;24:1625–1630. [DOI] [PubMed] [Google Scholar]
- 24.Mahoney FI,Barthel DW: Functional evaluation: The Barthel Index. Md State Med J 1965;14:61–65. [PubMed] [Google Scholar]
- 25.May D,Nayak US,Isaacs B: The life-space diary: a measure of mobility in old people at home. Int Rehabil Med 1985;7:182–186. [DOI] [PubMed] [Google Scholar]
- 26.Tung JY,Rose RV,Gammada E,Lam I,Roy EA,Black SE,Poupart P: Measuring life space in older adults with mild-to-moderate Alzheimer’s disease using mobile phone GPS. Gerontology 2014;60:154–162. [DOI] [PubMed] [Google Scholar]
- 27.Barnes LL,Wilson RS,Bienias JL,Mendes de Leon CF,Kim HJ,Buchman AS,Bennett DA: Correlates of life space in a volunteer cohort of older adults. Exp Aging Res 2007;33:77–93. [DOI] [PubMed] [Google Scholar]
- 28.Simmons SF,Schnelle JF,MacRae PG,Ouslander JG: Wheelchairs as mobility restraints: predictors of wheelchair activity in nonambulatory nursing home residents. J Am Geriatr Soc 1995;43:384–388. [DOI] [PubMed] [Google Scholar]
- 29.Uemura K,Shimada H,Makizako H,Yoshida D,Doi T,Yamada M,Suzuki T: Factors associated with life-space in older adults with amnestic mild cognitive impairment. Geriatr Gerontol Int 2013;13:161–166. [DOI] [PubMed] [Google Scholar]
- 30.Webber SC,Porter MM,Menec VH: Mobility in older adults: a comprehensive framework. Gerontologist 2010;50:443–450. [DOI] [PubMed] [Google Scholar]
- 31.Mortenson WB,Miller WC,Backman CL,Oliffe JL: Association between mobility, participation, and wheelchair-related factors in long-term care residents who use wheelchairs as their primary means of mobility. J Am Geriatr Soc 2012;60:1310–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ikezoe T,Asakawa Y,Hazaki K,Kanzaki H,Irie S,Kawano I,Morinaga T: Knee extensor strength for independent locomotion in the elderly. Rigakuryoho Kagaku 1997;12:179–181 [in Japanese]. [Google Scholar]
- 33.Toba K,Nakai R,Akishita M,Iijima S,Nishinaga M,Mizoguchi T,Yamada S,Yumita K,Ouchi Y: Vitality Index as a useful tool to assess elderly with dementia. Geriatr Gerontol Int 2002;2:23–29. [Google Scholar]