ABSTRACT
Background:
Virtual reality (VR) technology has been recently introduced in a variety of clinical settings, such as physical, occupational, cognitive, and psychological rehabilitation or training. However, the clinical efficacy of VR rehabilitation compared with traditional training techniques remains to be elucidated.
Case:
A 90-year-old man underwent VR-guided, dual-task, body trunk balance training in the sitting position using a newly developed medical device (mediVR KAGURA, mediVR, Inc., Toyonaka, Japan) after his physical activity level had plateaued. The patient had difficulty in walking outside the hospital even after having undergone traditional physical training. VR-guided training was performed for 40 min every weekday for 2 weeks. Trunk balance training was performed using reaching tasks, and cognitive stimulation was designed to emulate the cognitive processing involved when walking in a city or town. After the VR-guided training, the patient’s 6-min walk distance improved from 430 m to 500 m even though there had been no improvement in muscle strength of the lower extremities. Furthermore, the patient could successfully walk outside the hospital without falling or colliding with obstacles.
Discussion:
It is noteworthy that the patient’s walking ability improved further by the addition of VR-guided, dual-task, trunk balance training carried out in the sitting position. This finding suggests several possible new approaches to overcoming walking disability. Walking requires lower-extremity muscle strength, postural balance, and dual-task processing. Currently, no effective quantitative methods have been identified for postural balance and dual-task training with the patient in the sitting position. Herein, we discuss the possible advantages of VR-guided rehabilitation over traditional training methods.
Keywords: body trunk balance, dual task, reaching, virtual reality, walking
INTRODUCTION
Virtual reality (VR) technology has been recently introduced in a variety of clinical settings, e.g., physical, occupational, cognitive, and psychological rehabilitation or training.1,2) In particular, VR-guided body balance training to address neurological disorders such as stroke has garnered a lot of attention from physicians and therapists. Balance is essential for walking, and walking ability is a critical basic function associated with the quality of life.1,2,3,4,5) Walking is a harmonized physical activity requiring (1) lower-extremity muscle strength, (2) postural or trunk balancing ability, and (3) dual-task processing.5,6,7,8) Whereas lower-extremity muscle strength can be increased by various methods, no effective quantitative approach has been identified to train for balance and dual-task processing skills with the subject in the sitting position.5,6,7,8) VR-guided training can be applied to rehabilitation of walking disabilities, such as those associated with disuse syndrome after hospitalization in elderly people. Although this new technology is expected to become an increasingly useful tool to overcome the lack of human and economic resources associated with rehabilitation medicine, the clinical efficacy of VR rehabilitation compared with traditional training techniques remains to be elucidated.1,2,3,4,5,6,7,8)
CASE
A 90-year-old man with muscle atrophy and disuse syndrome resulting from approximately 1-month’s hospitalization following the successful management of an acute hemorrhagic rectal ulcer at another hospital was transferred to Eishinkai Kishiwada Rehabilitation Hospital for rehabilitation. The patient’s physical activity levels improved and reached a plateau after 1 month of traditional physical and occupational training at our hospital. At that time, his height was 160 cm, his weight was 47.4 kg, and his cognitive function corresponded to a mini-mental state examination (MMSE) score of 26. As shown in Table 1, at baseline, the patient’s 6-min walk distance (6MWD) was 430 m, the timed up and go (TUG) test result was 9.3 s, the 10-m walk test was completed in 6.4 s, and the Berg balance scale (BBS) score was 50. No motor dysfunctions such as paralysis were noted, and the functional independence measure (FIM) was 100. However, the risk of falling or colliding with obstacles such as telephone poles persisted when the patient walked outside the hospital, suggesting the presence of impaired dual-task processing or attention deficits. When the TUG and 10-m walk tests were evaluated in dual-task mode by asking the patient to count backward from 100 by 2 during the tests, the times required were much longer than the single-task times (Table 1). Baseline values of the Trail Making Test (TMT) and the Clinical Assessment for Attention (CAT, developed by the Japan Society for Higher Brain Dysfunction) also indicated the presence of generalized attention impairment, such as the inability to perform TMT part B and the prolonged time required to complete visual cancellation (Table 2).
Table 1. Serial changes in physical performance test results.
| Parameter | Baseline | After VR rehabilitation |
| Mini-mental state examination | 26 | 26 |
| Six-minute walking test, m | 430 | 500 |
| Timed up and go test, s | 9.3 | 7.8 |
| dual-task mode, s | 14.7 | 11.5 |
| Ten-meter walk test, s | 6.4 | 6.5 |
| dual-task mode, s | 12.1 | 9.6 |
| Berg balance scale | 50 | 53 |
| Functional independence measure | 100 | 100 |
| Motor | 76 | 76 |
| Cognitive | 24 | 24 |
| Numerical rating scale for enjoyment (0–10) | 7 | 7 |
| Reaching distance in the sitting position, cm* | ||
| Left hand 0° | 19.3 | 23.8 |
| Left hand 45° | 22.3 | 33.3 |
| Left hand 90° | 34.7 | 36.7 |
| Right hand 90° | 23.5 | 40.6 |
| Right hand 135° | 18.9 | 36.0 |
| Right hand 180° | 18.1 | 24.2 |
| Hand grip, kg | ||
| Left | 20.6 | 20.9 |
| Right | 19.2 | 22.1 |
| Knee extension, kg | ||
| Left | 21.2 | 21.4 |
| Right | 19.1 | 18.9 |
Timed up and go tests and 10-m walk tests were also executed in dual-task mode by asking the patient to count backward from 100 by 2 during the activity.
*0° is to the left side and 180° is to the right side as viewed from above.
Table 2. Trail-making test and clinical assessment for attention.
| Parameter | Baseline | After VR rehabilitation |
| Trail-making test | ||
| Part A, s | 226 | NA |
| Part B, s | Could not complete | NA |
| Clinical assessment for attention | ||
| Digit span, forward | 7 | 7 |
| Digit span, backward | 3 | 5 |
| Tapping span, forward | 5 | 5 |
| Tapping span, backward | 4 | 4 |
| Visual cancellation (triangles) | ||
| Time required, s | 342 | 148 |
| Correct rate, % | 100 | 100 |
| Success rate, % | 98 | 100 |
| Visual cancellation (symbols) | ||
| Time required, s | 327 | 190 |
| Correct rate, % | 74 | 81 |
| Success rate, % | 100 | 98 |
| Visual cancellation (3) | ||
| Time required, s | 416 | 441 |
| Correct rate, % | 93 | 98 |
| Success rate, % | 100 | 100 |
| Visual cancellation (Japanese Kana) | ||
| Time required, s | 508 | 467 |
| Correct rate, % | 92 | 96 |
| Success rate, % | 100 | 100 |
| Symbol digit modalities test | ||
| Accomplishment rate within 90 s, % | 12 | 14 |
| Memory updating (three span) | ||
| Correct rate, % | 75 | 75 |
| Memory updating (four span) | ||
| Correct rate, % | 25 | 50 |
| Positional Stroop test | ||
| Time required, s | 109 | 145 |
| Correct rate, % | 99 | 100 |
The success rate was calculated as the number of correct answers/the total number of responses.
NA, not available, i.e., the tests were not performed.
The auditory detection task and paced auditory serial addition test could not be performed because of the patient’s severe hearing impairment. The continuous performance test could not be performed because of the unavailability of the designated operating system for the computer.
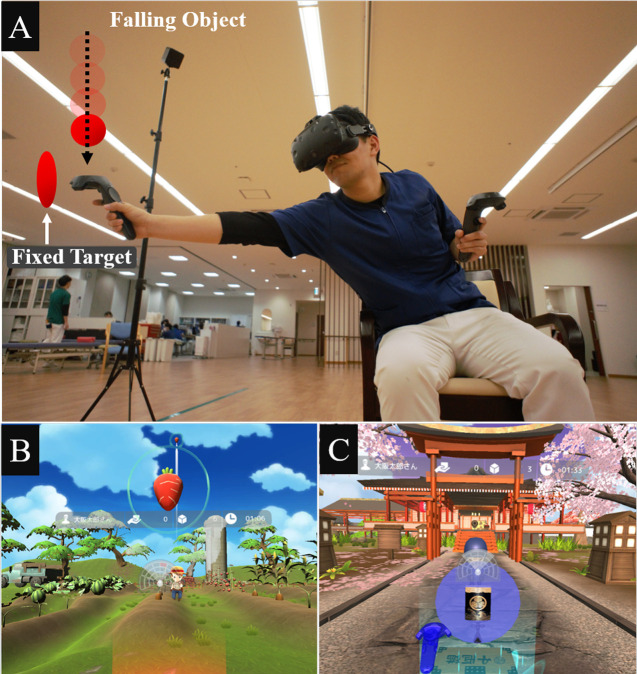
To help the patient regain the ability to walk independently, in addition to conventional rehabilitation practices, we utilized a newly introduced medical device for VR-guided, dual-task, body trunk balance training (mediVR KAGURA, mediVR, Inc., Toyonaka, Japan, commercially available from February 4, 2019).5) The mediVR KAGURA system was developed to help patients regain walking ability by improving their dual-task processing and trunk balancing.5) We applied VR-guided training because no additional improvements could be expected in the patient as a result of the aforementioned traditional physical and occupational training; however, the efficacy of VR-guided training remained unclear. As shown in Fig. 1, the patient was instructed to catch red or blue falling objects or to touch red or blue fixed targets in a three-dimensional virtual space with his right or left hand controllers, respectively. To ensure safety, the training was performed with the patient in the sitting position: training in the standing position is prohibited according to the device package insert. The mediVR KAGURA system can provide videogame-like training to enhance motivation and to ensure adherence. By setting seven parameters, i.e., the distance, angle, height, and size of the object; the size of the controller; the inter-task interval; and the falling speed or time limit for each task, the therapist can provide patients with reaching training in a dual-task fashion utilizing various levels of physical and cognitive stimulation. Cognitive stimulation was designed to emulate the way in which cognitive and attention functions are processed during walking. For example, a red object should be caught using the right hand controller and the blue object should be caught using the left hand controller. Differentiation of the color of objects emulates the cognitive processing required to differentiate traffic signals. The recognition of a new object in three-dimensional space and a timely reaching response, with consideration of the aforementioned seven parameters, emulate the cognitive processing involved in hazard perception and facilitate hazard avoidance, such as colliding with other people when walking outside the hospital.
Fig. 1.
Images of mediVR KAGURA-guided rehabilitation. (A) A physical therapist demonstrates VR-guided training tasks. The patient is instructed to catch red or blue falling objects or to touch red or blue fixed targets with their right or left hand controllers, respectively, in a three-dimensional virtual space. These tasks can be provided in the style of a videogame such as (B) a falling carrot thrown by a farmer or (C) a fixed small box bearing a symbol (similar to a police badge) that is used in a popular Japanese television period drama.
The VR system places a radar screen at the center of the head-mounted display to indicate the direction of the next task, and the patient needs to regularly refer to this radar screen. To evaluate or train the attentional ability of the patient, some gaming characteristics have been added that are designed to attract attention away from the radar screen. VR-guided training was performed for 40 min every weekday for 2 weeks (5 days per week). First, we tried to provide 20 min of VR-guided training on a trial basis because Japanese health insurance guidelines define 20 min of rehabilitation as 1 unit. However, the patient was eager to undergo VR-guided therapy for 40 min without any interval because he found it enjoyable (corresponding to a numerical enjoyment rating scale score of 7).
Serial changes in physical performance and attention test scores 2 weeks after the VR-guided training are shown in Table 1 and Table 2, respectively. The 6MWD improved from 430 m to 500 m despite the absence of improvements in MMSE, FIM, or muscle strength of the lower extremities [which was evaluated by knee extension measured using a handheld dynamometer (µTas F-1, Anima, Tokyo, Japan)]. TUG test results improved by 1.5 s (from 9.3 to 7.8 s) with a 3.2 s improvement for dual-task TUG. There was no improvement in the 10-m walk test, but the test performance improved by 2.5 s when carried out in dual-task mode. Regarding the BBS score, reaching forward, placing alternating feet on a stool, and tandem stance improved by 1 point each. The patient did not get bored of participating in the VR-based rehabilitation program, as indicated by there being no changes in the numerical rating score for enjoyment. Several attention test indices, including the digit span backward test, the time required to complete visual cancellations of a triangle or symbol, and the correct rate of memory updating (four span) drastically improved. As a result of 2 weeks of VR-guided training, the patient could successfully walk outside the hospital without falling or colliding with obstacles. However, after the 2 weeks of VR-guided training, the patient was unfortunately discharged to a nursing home for nonmedical reasons. Consequently, potential additional improvements from further training could not be attempted. Informed consent for the submission of this case report was obtained from the patient by the attending physical therapist in compliance with the standard operating procedures defined by the institutional ethics committee at Eishinkai Kishiwada Rehabilitation Hospital.
DISCUSSION
It is noteworthy that, after the lower limb strength had plateaued, the walking ability of this patient was improved by the addition of VR-guided, dual-task, body trunk balance training executed with the patient seated. We believe that it would not have been possible to improve the walking ability without VR-guided training in this case because the patient’s walking ability had reached a plateau 1 month after traditional physical and occupational training at our hospital. This result challenges the traditional belief that walking rehabilitation should be provided in the standing position, especially by encouraging patients to walk. Consequently, this finding suggests that there may be several possible new approaches to improving walking disability.6)
For example, reaching training using hooks or hoops is a very conventional and fundamental approach to improving postural or trunk balance.7) However, postural balance training cannot be quantitatively performed in a replicable way using these conventional approaches.5) It is time consuming to change the intensity of postural balance stimulation because therapists need to repeatedly change the position of the hook for each task. In contrast, VR facilitates an easy, prompt, quantitative, and replicable method of training by accurately setting the distance, angle, height, or other parameters in a three-dimensional virtual space.5) The therapist’s only responsibility is to adjust these parameters by typing numbers on the operating panel of a computer. Moreover, the unpredictable nature of VR-training tasks may require much more precise postural control for patients. The rationale for sitting training is that two-thirds of the total body weight is centered in the upper body, and improved upper body balance is expected to result in stable balancing during walking.9) Consequently, we speculated that tailor-made, optimized, and unpredictable VR-guided training tasks might make a greater contribution to more effective postural and trunk balance than conventional approaches, even when performed in a sitting position.
Likewise, conventional dual-task training is provided by asking patients to talk with the therapist, to count backward from 100 by a specific number, or to perform tasks such as the paper–scissors–stone game simultaneously with walking.7,8) However, we consider that these conventional dual-task training schemes do not directly emulate the cognitive functions needed while walking in a city or town. Although the current patient could walk steadily inside the hospital with a 6MWD of 430 m at baseline after 1 month of conventional rehabilitation at our institution, his walking ability remained unstable with the risk of falling or colliding with obstacles outside the hospital. This may have resulted from information overload or attention deficits. One of the strengths of VR-guided training is the controllability of cognitive stimulation in a uniform environment in a way that mimics the cognitive processes needed during walking in a city or town as described in the case presentation section above.5) During VR-guided rehabilitation, the patient continuously had to think about the next task, i.e., when and where the next falling object will appear, followed by timely reaching tasks, emulating the conditions of hazard perception and avoidance. As a result, in the current patient, several parameters, including the 6MWD, the TUG test with and without dual tasking, the dual-task 10-m walk test, the BBS, and the likelihood of falling outside the hospital improved even without improvements in the MMSE or FIM scores or the lower-extremity muscle strength. VR seems to be a more appropriate technology than augmented or mixed reality technologies when trying to provide patients with uniform and replicable environments for cognitive stimulation or evaluation. This is because the landscape or environmental information changes when augmented or mixed reality technologies are used in different locations.
Because of improvements in several CAT indices in the current patient, we speculated that VR-guided attention training contributed to improved walking ability outside of the hospital. TMT or components of CAT have been used to evaluate attention deficits for decades.10,11) Attention deficits are historically categorized into five components, as proposed by Sohlberg et al., namely, focused, selective, sustained, alternating, and divided attention.12) The patient’s general attention might have improved; however, we also understand that his focused and selective attention were profoundly impacted by the VR-guided training because the digit span backward test, the time required to complete visual cancellations of a triangle or symbol, and the correct rate of memory updating (four span) markedly improved.11,12)
Regrettably, for nonmedical reasons, the current patient was discharged after 2 weeks of VR-guided training; consequently, additional improvement could not be attempted, even though longer intervention is considered to be more effective.13) Furthermore, the advantages and disadvantages of VR-guided rehabilitation have not yet been clearly identified. It appears that VR-guided training safely increases motivation, although the majority of evidence has been obtained in the upper limb rehabilitation of stoke patients.14,15,16) VR-guided training can make rehabilitation more enjoyable and it is expected to contribute to effective training in this case report.13)
There are several two-dimensional programs available for trunk balance training in clinical settings. For example, the Nintendo Wii Fit (Nintendo, Kyoto, Japan) is reportedly effective in improving BBS or TUG.17,18) However, some physicians have suggested that VR, which is three-dimensional in nature, has additional advantages in providing accurate instructions and quantitative assessments compared to two-dimensional programs.5) Consequently, the differences between two- and three-dimensional VR-guided training is another pertinent subject for research in the field of rehabilitation.
In conclusion, we presented an interesting case in which VR-guided, dual-task, body trunk balance training with the subject in the sitting position helped improve walking ability. However, the nature of this single case report limits the reliability of the identified efficacy of VR-guided training and also limits the external validity. Because the number of patients with walking disability is increasing worldwide in this era of super-aged societies and because VR-guided training in the sitting position can be provided safely without additional human resources, the clinical efficacy of this type of training warrants further evaluation in prospectively designed studies.
Footnotes
CONFLICTS OF INTEREST: Masahiko Hara is the chief executive officer and a stockholder of mediVR, Inc., a company that holds several patents on VR-guided, dual-task rehabilitation. However, this case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Kyohei Omon and Hideo Ishikawa have no conflicts of interest to declare.
REFERENCES
- 1.Massetti T,da Silva TD,Crocetta TB,Guarnieri R,de Freitas BL,Bianchi Lopes P,Watson S,Tonks J,de Mello Monteiro CB: The clinical utility of virtual reality in neurorehabilitation: a systematic review. J Cent Nerv Syst Dis 2018;10:1179573518813541. 10.1177/1179573518813541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tieri G,Morone G,Paolucci S,Iosa M: Virtual reality in cognitive and motor rehabilitation: facts, fiction and fallacies. Expert Rev Med Devices 2018;15:107–117. 10.1080/17434440.2018.1425613 [DOI] [PubMed] [Google Scholar]
- 3.de Amorim JSC,Leite RC,Brizola R,Yonamine CY: Virtual reality therapy for rehabilitation of balance in the elderly: a systematic review and META-analysis. Adv Rheumatol 2018;58:18. 10.1186/s42358-018-0013-0 [DOI] [PubMed] [Google Scholar]
- 4.Lin IH,Tsai HT,Wang CY,Hsu CY,Liou TH,Lin YN: Effectiveness and superiority of rehabilitative treatments in enhancing motor recovery within 6 months poststroke: a systemic review. Arch Phys Med Rehabil 2019;100:366–378. 10.1016/j.apmr.2018.09.123 [DOI] [PubMed] [Google Scholar]
- 5.Hara M,Kitamura T,Murakawa Y,Shimba K,Yamaguchi S,Tamaki M: Safety and feasibility of dual-task rehabilitation program for body trunk balance using virtual reality and three-dimensional tracking technologies. Prog Rehabil Med 2018;3:20180016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peurala SH,Karttunen AH,Sjögren T,Paltamaa J,Heinonen A: Evidence for the effectiveness of walking training on walking and self-care after stroke: a systematic review and meta-analysis of randomized controlled trials. J Rehabil Med 2014;46:387–399. 10.2340/16501977-1805 [DOI] [PubMed] [Google Scholar]
- 7.Gordon NF,Gulanick M,Costa F,Fletcher G,Franklin BA,Roth EJ,Shephard T, American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention: Physical activity and exercise recommendations for stroke survivors. Stroke 2004;35:1230–1240. 10.1161/01.STR.0000127303.19261.19 [DOI] [PubMed] [Google Scholar]
- 8.Trombetti A,Hars M,Herrmann FR,Kressig RW,Ferrari S,Rizzoli R: Effect of music-based multitask training on gait, balance, and fall risk in elderly people: a randomized controlled trial. Arch Intern Med 2011;171:525–533. 10.1001/archinternmed.2010.446 [DOI] [PubMed] [Google Scholar]
- 9.McCollum G,Leen TK: Form and exploration of mechanical stability limits in erect stance. J Mot Behav 1989;21:225–244. 10.1080/00222895.1989.10735479 [DOI] [PubMed] [Google Scholar]
- 10.Corrigan JD,Hinkeldey NS: Relationships between Parts A and B of the Trail Making Test. J Clin Psychol 1987;43:402–409. [DOI] [PubMed] [Google Scholar]
- 11.Toyokura M,Nishimura Y,Akutsu I,Watanabe F: Clinical significance of an easy-to-use dual task for assessing inattention. Disabil Rehabil 2017;39:503–510. 10.3109/09638288.2016.1152601 [DOI] [PubMed] [Google Scholar]
- 12.Sohlberg MM,Mateer CA: Effectiveness of an attention-training program. J Clin Exp Neuropsychol 1987;9:117–130. 10.1080/01688638708405352 [DOI] [PubMed] [Google Scholar]
- 13.Laver KE,Lange B,George S,Deutsch JE,Saposnik G,Crotty M: Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev 2017;11:CD008349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yates M,Kelemen A,Sik Lanyi C: Virtual reality gaming in the rehabilitation of the upper extremities post-stroke. Brain Inj 2016;30:855–863. 10.3109/02699052.2016.1144146 [DOI] [PubMed] [Google Scholar]
- 15.Dias P,Silva R,Amorim P,Lains J,Roque E,Pereira IS,Pereira F,Santos BS,Potel M: Using virtual reality to increase motivation in poststroke rehabilitation. IEEE Comput Graph Appl 2019;39:64–70. 10.1109/MCG.2018.2875630 [DOI] [PubMed] [Google Scholar]
- 16.McGrane N,Galvin R,Cusack T,Stokes E: Addition of motivational interventions to exercise and traditional physiotherapy: a review and meta-analysis. Physiotherapy 2015;101:1–12. 10.1016/j.physio.2014.04.009 [DOI] [PubMed] [Google Scholar]
- 17.Tripette J,Murakami H,Ryan KR,Ohta Y,Miyachi M: The contribution of Nintendo Wii Fit series in the field of health: a systematic review and meta-analysis. PeerJ 2017;5:e3600. 10.7717/peerj.3600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agmon M,Perry CK,Phelan E,Demiris G,Nguyen HQ: A pilot study of Wii Fit exergames to improve balance in older adults. J Geriatr Phys Ther 2011;34:161–167. 10.1519/JPT.0b013e3182191d98 [DOI] [PubMed] [Google Scholar]