ABSTRACT
Objective:
The aim of this study was to validate the usefulness of the measurement of lung insufflation capacity (LIC) using the LIC TRAINER (LT) in patients with amyotrophic lateral sclerosis (ALS).
Methods:
This retrospective study was conducted in the rehabilitation departments of the Japanese National Center of Neurology and Psychiatry and involved 20 ALS patients who underwent respiratory therapy between April 1, 2014, and December 2017. The vital capacity (VC), maximum insufflation capacity (MIC), and LIC measurements at the start of respiratory therapy were extracted from the medical records, and patients were divided into three groups: group A, VC could not be measured; group B, VC could be measured, but MIC was less than VC; and group C, MIC was larger than VC. LIC could be measured in all groups. In group C, paired t-tests were used to analyze whether there was a significant difference in the volumes measured using different methods.
Results:
LIC was 950, 1863±595, and 2980±1176 ml in groups A (n=1), B (n=10), and C (n=9), respectively. In groups A and B, LIC could be measured in all patients, even when VC or MIC could not be measured. In group C, the measured LIC value was significantly greater than MIC (p=0.003).
Conclusion:
LIC could be successfully measured using the LT. By using the LT, it was feasible to conveniently perform LIC measurements, suggesting that it could be a useful device for performing respiratory therapy in ALS patients.
Keywords: amyotrophic lateral sclerosis, lung insufflation capacity, lung volume recruitment, new device, respiratory therapy
INTRODUCTION
Amyotrophic lateral sclerosis (ALS) is an intractable disease with an unknown etiology. With disease progression, respiratory disorders induced by a decrease in the strength of the muscles necessary for breathing or coughing becomes a factor that determines survival.1) Respiratory therapy is one of the methods used to provide respiratory care in ALS; furthermore, airway clearance techniques are required in ALS patients.2) Lung volume recruitment (LVR) using a bag valve mask (BVM) is recommended in the guidelines for treating patients with muscular dystrophy, and this technique is known to complement coughing strength and maintain airway clearance.3) The inspiratory volume attained through LVR is called the maximum insufflation capacity (MIC); it is measured using a Wright respirometer through expiration that is amplified with several breaths and air stacking using the patient’s vocal cords and LVR.2)
However, in ALS patients, LVR is difficult when air stacking is not possible because of progression in bulbar palsy or the presence of a tracheostomy, in addition to ventilatory impairment caused by decreased respiratory muscle strength. In such cases, a method for sustained LVR that does not require air stacking is required. The resulting deep inspiration can be measured using the lung insufflation capacity (LIC). To measure LIC, a mechanical ventilator, a mechanical insufflation–exsufflation (MI-E) device, or a special lung volume recruitment bag (LVRB) with a built-in one-way valve is used.2) The components of a LVRB are similar to those of the LIC measurement technique that uses a one-way valve proposed by Bach et al. in 2008,4) as well as the Artificial External Glottic Device (AEGD) presented by Kim et al. in 2011.5) However, these devices were not commercialized and were used only in research institutions and in a handful of medical institutions; furthermore, until recently, there were no approved medical devices for performing LIC in Japan. Moreover, the risk management of lung injury resulting from positive pressure was a challenge when using the LVRB. Consequently, we developed LIC TRAINER (LT) as a medical device, and received approval for it in 2016. At present, it is possible to measure LIC in ALS patients in Japan using LT. However, LT is not well known internationally.
The objective of this study was to retrospectively analyze the measured values of vital capacity (VC), MIC, and LIC in ALS patients, and to validate the usefulness of respiratory function assessment based on LIC using the LT that we developed.
METHODS
LT Product Description and Operation
Form and Structure
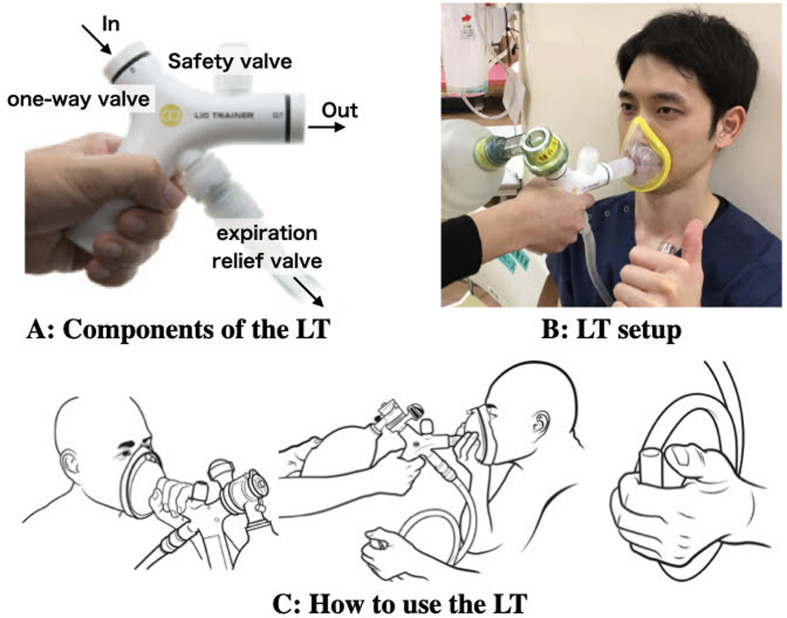
The LT is a device that is airtight and includes a one-way valve, a safety valve, and an expiration relief valve (Fig. 1A).
Fig. 1.
The LIC TRAINER (LT) (components from Cater Technologies, Japan). (A) The LT comprises a one-way valve, a safety valve, and an expiration relief valve. (B) LT setup: the BVM is attached to the primary port (IN) of the LT. The mask is attached to the secondary port (OUT) of the LT. (C) Operation of the LT: the patient’s nose and mouth are covered by the mask. The patient holds the expiration relief valve in their hand. The assistant slowly applies pressure several times with the BVM. The patient inhales as much as they can tolerate, before releasing their thumb from the expiration relief valve and exhaling deeply.
LT Setup
A BVM is attached to the primary port (IN) of the LT, and a mask is attached to the secondary port (OUT) of the LT. For tracheostomy patients, a flexible tracheostomy tube is attached to the OUT port. When measuring LIC, a Wright respirometer is attached between the OUT port of the LT and the mask or flex tube, and an expiration relief valve is attached to the LT (Fig. 1B).
Use of the LT
The patient’s nose and mouth are covered with the mask. The patient holds the expiration relief valve in the hand and operates the valve with his/her thumb. The assistant slowly applies air pressure several times with the BVM. At this point, the patient inhales slowly and deeply. After inhaling as much as the patient can tolerate, the patient releases his/her thumb from the expiration relief valve and exhales deeply. If the patient cannot operate the expiration relief valve by himself/herself, the assistant operates the valve. The attached Wright respirometer measures LIC (Fig. 1C).
Specifications of the LT
The LT, co-developed by our hospital and Cater Technologies (Saitama, Japan), has an LIC function and, in addition to LVRB and AEGD functions, it has a built-in safety valve to prevent lung injury. Specifically, when a pressure of 60 cmH2O or greater is applied, the safety valve is activated for automatic de-aeration. Additionally, there is an expiration relief valve that patients can operate themselves with their thumb. This device can be used in respiratory therapy and, by connecting a Wright respirometer, it can be used to measure LIC. In 2016, the LT was approved for sale in Japan as a medical device (medical device registration number, 11B3X10044000001; patent pending, patent application 2016–109754).
Participants
The current study was approved by the Ethics Committee of the National Center of Neurology and Psychiatry (A2014-025). The participants were 20 ALS patients who underwent respiratory therapy at our hospital between April 1, 2014, and December 2017, either as hospitalized patients or as outpatients. All patients were diagnosed as having ALS. After receiving a full explanation of the study, all participants provided informed consent for retrieval of their medical records.
Design and Outcome Measures
For the measurement of VC, all subjects were asked to take a deep breath and then exhale the maximum volume of air into the Wright spirometer with a mask. Tracheostomy patients undergoing positive pressure ventilation (TPPV) were asked to measure VC from their tracheal cannula by using a Wright spirometer. For the measurement of MIC, which is done on exhalation using a Wright spirometer, air stacking was carried out with a BVM that was consecutively pressurized, and breath was held by glottic closure until no more air could be retained.
The measured values of VC, MIC, and LIC obtained during respiratory therapy training were retrospectively extracted from the patients’ medical records. Data on age, duration of disease, Oral Secretions Scale (OSS) scores, Mini-Mental State Examination (MMSE) scores, and revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R) scores were obtained from the patients’ medical records. For each item, the same physical therapist made measurements three times, and the highest value was used as the measured value. Patients were divided into three groups: group A, VC could not be measured; group B, VC could be measured, but MIC was less than VC; and group C, MIC was larger than VC. LIC could be measures in all members of all groups. The inability to measure VC meant no spontaneous breathing, and the inability to measure MIC meant that more ventilation volume than VC could not be obtained.
Data Analysis
Group C consisted of patients in whom both MIC and LIC could be measured. To investigate whether there was a significant difference in insufflation volumes obtained by different methods, a paired t-test was used after confirming the normality of MIC and LIC values. Analysis of covariance (Fisher r-to-z transformation) was performed to determine the associations between measured ventilation volumes (VC, MIC, and LIC) and age, duration of disease, OSS, MMSE, and ALSFRS-R. IBM SPSS version 25 was used as the statistical software, and p<0.05 was considered significant.
RESULTS
All 20 study patients (11 men, 9 women; mean age 61.4±12.2 years) had “probable ALS,” according to the El Escorial revised criteria. The initial disease involved the upper limbs (n=9), the lower limbs (n=7), bulbar palsy (n=3), and respiratory muscle paralysis (n=1). At the start of respiratory therapy, the disease duration was 36.0±24.4 months, VC was 1659±1013 ml, the ALSFRS-R score was 30.1±12.2, the OSS score was 9.75±5.2, and the MMSE score was 26.8±4.3 [values expressed as mean ± standard deviation (SD)]. A non-invasive mechanical ventilator (NIV) was used in five patients, and TPPV was used in five patients (Table 1) .
Table 1. Patient characteristics (n=20).
| Parameter | Number or median value | IQR |
| Sex, male:female (n) | 11:09 | |
| Age (years) | 61.5 | 41–78 |
| Types UE:LE:Bulbar:RMP (n) | 9:7:3:1 | |
| Disease duration (months) | 29 | 5–100 |
| MMSE (points)* | 29 | 16–30 |
| ALSFRS-R total score | 32.5 | 16–46 |
| OSS | 10 | 0–16 |
| NIV user | 5 | |
| TPPV user | 5 |
*MMSE n=19 (1 patient was unable to complete the test).
IQR, interquartile range; UE, upper extremity paralysis; LE, lower extremity paralysis; Bulbar, bulbar palsy; RMP, respiratory muscle paralysis.
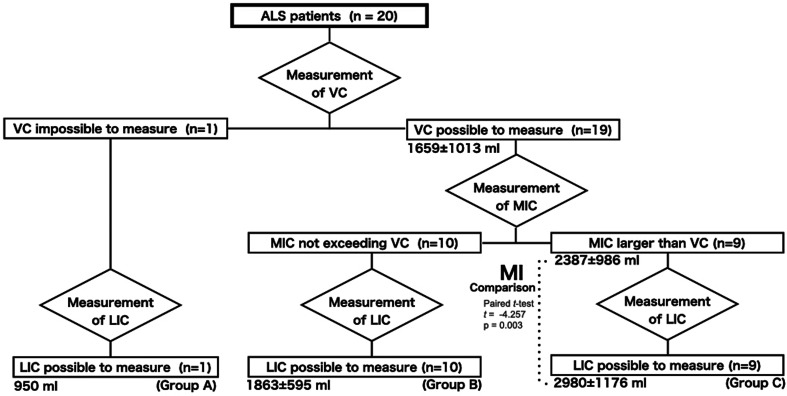
VC could be measured in 19 of 20 patients, and its mean value was 1659±1013 ml. LIC was 950 ml, 1863±595 ml, and 2980±1176 ml in groups A (n=1), B (n=10), and C (n=9), respectively (Fig. 2). LIC could be measured in all three groups, and its mean (range) ±SD value was 2366 (850–5100) ±1020 ml. In the nine patients whose MIC and LIC could be measured, LIC was significantly greater than MIC (t=–4.257, p=0.003). All patients using LT could exhale by operating the relief valve, and the safety valve did not operate. Analysis of the associations between ventilation volume and each assessment variable showed a positive correlation between LIC and MMSE (r=0.402, p<0.05).
Fig. 2.
Measurement of VC, MIC, and LIC in the present study. Patients were divided into three groups: group A, VC could not be measured; group B, VC could be measured, but MIC was less than VC; and group C, MIC was larger than VC. LIC could be measured in all members of all groups. In group C, LIC was significantly greater than MIC (t=–4.257, p=0.003).
DISCUSSION
Respiratory disorders in ALS patients cause restrictive ventilatory impairment because of the decreased strength of the respiratory muscles such as the diaphragm. When deep inspirations become difficult, hypoventilation leads to hypercapnia. Moreover, when the symptoms of bulbar palsy are also present, further decreases in coughing strength result in a condition likely to cause suffocation or aspiration pneumonia.6)
Treatments for respiratory disorders in ALS include ventilatory support with an NIV and a TPPV. Compared to those receiving no ventilatory support, the lifespan of ALS patients can be prolonged by using an NIV; compared to the use of an NIV, lifespan can be extended even further by using a TPPV. Therefore, ventilatory support can extend life under long-term medical treatment beyond the point of respiratory failure. Furthermore, in respiratory care that requires ventilatory support, maintaining airway clearance by regularly performing oral care, endotracheal aspiration, and MI-E is indispensable for maintaining a stable condition. However, when hypoventilation occurs as a result of progressive respiratory muscle impairment, the flexibility of the thorax is lost. Moreover, mechanical ventilator support is not powerful enough to maximally expand the thorax, and this eventually restricts the mobility of the thorax. In patients on long-term TPPV, decreased LIC is directly linked to the elevation in airway pressure, leading to poor airway clearance.
In this study, the airway clearance techniques recommended above could not be used to measure the MIC because the ALS patients who had bulbar palsy or had undergone tracheostomy could not perform air-stacking. However, even in such cases, it was shown that LT could be used to quantitatively evaluate LIC.
To obtain LIC using a mechanical ventilator, it is necessary to use the volume control ventilation setting, or it is necessary to make special changes with the inspiratory phase, such as the lung insufflation assist maneuver, intermittent positive pressure breathing, or the recruitment maneuver. These settings are difficult to apply with home mechanical ventilation. To measure LIC with an MI-E, a setting other than the setting for the coughing aid is required, and the operation of this setting procedure is quite complex because it is performed while manually maintaining the extension in the inspiratory phase. Additionally, in Japan, MI-E is covered by the medical insurance system only for patients with a home mechanical ventilator; therefore, MI-E cannot be used in patients with early-stage disease, patients who do not wish to be on a mechanical ventilator, or inpatients. To resolve this issue, we developed the LT.
The advantage of LIC is that it facilitates deep inspiration when air stacking is difficult in patients with severe respiratory failure.2,4,5) In the present study, MIC was 2387 (800–4000) ±986 ml (mean (range)±SD), and LIC using the LT in all patients was 2366 (850–5100) ±1020 ml, similar to previous studies.4) However, in group C, where both MIC and LIC could be determined, LIC was 2980±1176 ml, which is larger than the values found in previous studies (Table 2). To measure LIC, Bach et al. used a BVM and ventilator, and Kim et al. used the AEGD; however, in both studies, the operator, not the patient, released the expiration relief valve.4,5) With the LT used in the present study, the patients themselves could control the expiration relief valve, indicating that self-control, rather than third-person control, of the expiration relief valve may achieve the largest possible inspiratory volume. Moreover, since there is a built-in safety valve in the LT, LVR can be safely performed by the patients themselves or by an operator while managing the risk of lung injury. Therefore, this method may be more clinically effective than the conventional method of LVR for measuring LIC. Furthermore, LIC could be measured in patients whose VC and MIC could not be measured, thereby supporting the findings of Bach et al. who stated that MIC minus VC has a negative correlation with LIC minus MIC.4)
Table 2. The results of previous research and of the present study.
| Bach7) | Kim8) | Present study | ||||
| Group A | Group B | Group C | Total | |||
| ALS (n) | 76 | 23 (all bulbar) | 1 | 10 | 9 | 20 (bulbar type: 3 patients) |
| Mean age (years) | 57 (27–82)±13 | 52.2±11 | 64 | 63.1 (43–76)±10.1 | 61.4 (44–78)±13.1 | 61.4 (41–78)±12.2 |
| Mean VC (ml) | 1371 (20–3480)±789 | 823.8±316.5 | — | 1095±533.4 | 2286±1074 | 1659 (550–4500)±1013* |
| Mean MIC (ml) | 1939 (150–5100)±1080 | MIC possible to measure in 6 patients |
— | — | 2387 (800–4000)±986 | 2387 (800–4000)±986** |
| Mean LIC (ml) | 2409 (780–5400)±989 | 1543.9±437.8 | 950 | 1863 (900–2650)±595 | 2980 (850–5100)±1176 | 2366 (850–5100)±1020 |
| Without NIV (n) | 22 | 0 | 0 | 5 | 5 | 10 |
| Tracheostomy (n) | 0 | 12 | 1 | 4 | 0 | 5 |
Data are mean (range) ±SD or number of patients.
*VC could be measured in 19 patients (groups B and C).
**MIC was larger than VC in 9 patients (group C).
In group C, which consisted of patients in whom both MIC (requiring self-air breath holding) and LIC (not requiring breath holding) could be performed, LIC was significantly greater than MIC. These findings are consistent with previous studies and indicate that a passive control mechanism that does not require self-air stacking may be more effective than an active control mechanism that requires self-air stacking in maintaining the flexibility of the lungs and thorax. Therefore, with respect to the respiratory disorders in ALS, LIC using LT may be more useful in the passive expansion of the lungs than MIC. Moreover, because LVR can be performed easily by using the LT without a mechanical ventilator or MI-E, this method represents a versatile everyday technique of respiratory therapy because it can conveniently maintain lung volume, thoracic range of motion, and lung compliance.
Although Kim et al.5) reported that AEGD can measure cough peak flow in addition to LIC, this approach presents challenges because it requires two operators, and precision measurement is hard to maintain because of the system complexity and the requirement of momentary air stacking. In contrast to AEGD, the LT uses a Wright respirometer and ventilator mask for measuring VC; LT can also prevent the potential risk of lung injury thanks to its built-in safety valve. Consequently, the LT is a more convenient device and is therefore superior to the AEGD or LVRB. From the perspective of the cost of performing airway clearance techniques, as well as the amount of aid required, as reported by Toussaint et al., MIC and LIC are less expensive and require less aid than methods that use MI-E or manually assisted coughing.7) Unlike AEGD and LVRB, compared to MI-E, LT does not require several additional mechanisms such as the provision of negative pressure for exsufflation, automatic controllers, or batteries. Furthermore, the LT can be purchased as a medical device in Japan for 27,000 yen (~250 USD), which is significantly less expensive than purchasing an MI-E device. Moreover, whereas MI-E devices require an external or internal battery, the LT is versatile, because it is portable and does not require a power source.
Because some ALS patients have dementia,8) the present investigation also examined the patients’ cognitive function. According to the MMSE scores, decreased cognitive function was not observed in 16 patients. However, because LIC was associated with MMSE, we consider it desirable to use LT in patients with early-stage ALS or in those without cognitive impairment who can fully understand how to use the device and can take full advantage of its beneficial characteristics.
McKim and Bédard stated that a greater difference between the passive inspiratory volume and VC is associated with a better prognosis for survival, and that it should be a goal to maintain this difference, since the difference is known to disappear with disease progression as the patient suffers respiratory muscle impairment.9) Therefore, because LIC measurement and training become feasible with LVR using the LT, even when MIC is difficult, this could be a potential airway clearance technique. LVR with LT has the added advantage that it allows the evaluation, maintenance, and expansion of thoracic mobility as a method to attain LVR in ALS patients. Bach et al. stated that both MIC and LIC increase with training4); therefore, the effects of practicing LVR using the LT need to be investigated in the future.
Study Limitations
There are several limitations to this study. First, this was a retrospective study, so the expiratory maximum airway pressure at which the patient experienced limitation in LVR was not verified. Second, in LIC, the self-operation of the expiration relief valve could not be confirmed from the description in the medical records, and this may have led to the difference in MIC and LIC measurements. Third, subjective symptoms, immediate effects, and short-term effects of LT could not be ascertained. Fourth, it will be necessary to standardize the level of experience of the therapist who operates the LT to ensure familiarity with and mastery of the device.
The current challenge is to elucidate the reliability and validity of LIC evaluations using the LT in terms of inter-rater reliability. In the future, in ALS patients using the LT, it will be necessary to investigate the effects on ventilation efficiency and oxygenation as an outcome of LVR and LIC measurement. Furthermore, validation of whether LVR using the LT prevents decreased respiratory function or microatelectasis will be needed. It is hoped that LVR with LT will prove effective as a technique for standard respiratory care for all stages of ALS, including the respiratory failure stage and home mechanical ventilation.
Conclusion
LIC could be quantitatively assessed using the LT. Because the LT can be used conveniently to obtain LIC values, it may be a useful method for performing respiratory therapy in ALS patients.
ACKNOWLEDGMENTS
A summary of this study was presented by the same authors at the 29th ALS/MND International Symposium in Glasgow, United Kingdom, December 13, 2018. This study was funded by an NCNP Grant-in-Aid for Promoting Research (86–3).
Footnotes
CONFLICTS OF INTEREST: The LT was co-developed by our hospital and Cater Technologies (Saitama, Japan). The authors state that they have no other conflicts of interest.
REFERENCES
- 1.Haverkamp LJ,Appel V,Appel SH: Natural history of amyotrophic lateral sclerosis in a database population. Validation of a scoring system and a model for survival prediction. Brain 1995;118:707–719. 10.1093/brain/118.3.707 [DOI] [PubMed] [Google Scholar]
- 2.Chatwin M,Toussaint M,Gonçalves MR,Sheers N,Mellies U,Gonzales-Bermejo J,Sancho J,Fauroux B,Andersen T,Hov B,Nygren-Bonnier M,Lacombe M,Pernet K,Kampelmacher M,Devaux C,Kinnett K,Sheehan D,Rao F,Villanova M,Berlowitz D,Morrow BM: Airway clearance techniques in neuromuscular disorders: a state of the art review. Respir Med 2018;136:98–110. 10.1016/j.rmed.2018.01.012 [DOI] [PubMed] [Google Scholar]
- 3.Finder JD,Birnkrant D,Carl J,Farber HJ,Gozal D,Iannaccone ST,Kovesi T,Kravitz RM,Panitch H,Schramm C,Schroth M,Sharma G,Sievers L,Silvestri JM,Sterni L, American Thoracic Society: Respiratory care of the patient with Duchenne muscular dystrophy: ATS consensus statement. Am J Respir Crit Care Med 2004;170:456–465. 10.1164/rccm.200307-885ST [DOI] [PubMed] [Google Scholar]
- 4.Bach JR,Mahajan K,Lipa B,Saporito L,Goncalves M,Komaroff E: Lung insufflation capacity in neuromuscular disease. Am J Phys Med Rehabil 2008;87:720–725. 10.1097/PHM.0b013e31817fb26f [DOI] [PubMed] [Google Scholar]
- 5.Kim DH,Kang SW,Park YG,Choi WA,Lee HR: Artificial external glottic device for passive lung insufflation. Yonsei Med J 2011;52:972–976. 10.3349/ymj.2011.52.6.972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vandenberghe N,Vallet AE,Petitjean T,Le Cam P,Peysson S,Guérin C,Dailler F,Jay S,Cadiergue V,Bouhour F,Court-Fortune I,Camdessanche JP,Antoine JC,Philit F,Beuret P,Bin-Dorel S,Vial C,Broussolle E: Absence of airway secretion accumulation predicts tolerance of noninvasive ventilation in subjects with amyotrophic lateral sclerosis. Respir Care 2013;58:1424–1432. 10.4187/respcare.02103 [DOI] [PubMed] [Google Scholar]
- 7.Toussaint M,Chatwin M,Gonzales J,Berlowitz DJ,Toussaint M,Chatwin M,Gonzales J,Berlowitz D,Lacombe M,Goncalves M,Bonnier MN,Sheers N,Andersen T,Sancho J,Fauroux B,Pernet K,Hov B,Kampelmacher M,Villanova M,Rao F,Morrow B,Sheehan DW,Devaux C,Kinnett K,Chaulet J, ENMC Respiratory Therapy Consortium: 228th ENMC International Workshop: Airway clearance techniques in neuromuscular disorders – Naarden, The Netherlands, 3-5 March, 2017. Neuromuscul Disord 2018;28:289–298. 10.1016/j.nmd.2017.10.008 [DOI] [PubMed] [Google Scholar]
- 8.Chen-Plotkin AS,Lee VM,Trojanowski JQ: TAR DNA-binding protein 43 in neurodegenerative disease. Nat Rev Neurol 2010;6:211–220. 10.1038/nrneurol.2010.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bédard ME,McKim DA: Daytime mouthpiece for continuous noninvasive ventilation in individuals with amyotrophic lateral sclerosis. Respir Care 2016;61:1341–1348. 10.4187/respcare.04309 [DOI] [PubMed] [Google Scholar]