Abstract
• PURPOSE:
To assess the long-term stability of sutured scleral-fixated posterior chamber intraocular lenses (PCIOLs) performed in combination with pars plana vitrectomy.
• DESIGN:
Retrospective, consecutive, interventional case series.
• METHODS:
Retrospective single-surgeon study of 118 eyes of 111 patients seen at Retina Consultants of Hawaii, who underwent sutured scleral fixation of at least 1 haptic of a posterior chamber intraocular lens with 10–0 polypropylene combined with a pars plana vitrectomy. The fixation knot-tying technique required 2 separate 10–0 polypropylene sutures tied into 1 combined knot—1 suture closed the fixation sclerotomy and created the scleral fixation, and 1 suture looped together around the haptic of the PCIOL, securing the haptic to the scleral fixation site. The primary outcomes were position of the PCIOL at last follow-up, dislocation of either 1 or both haptics of the PCIOL, and breakage of the 10–0 polypropylene fixation suture.
• RESULTS:
PCIOLs remained well stabilized and positioned at last follow-up in 116 of 118 eyes (98.3%), with a mean follow-up of 6.0 years. The maximum stable follow-up with 2 intact fixation sutures was 24.75 years. There were 4 cases of redislocation (3.4%), but 2 cases were owing to unstable residual capsular support. There was 1 case of suture breakage in 214 fixation sutures (0.47%) and 1 case of haptic breakage.
• CONCLUSIONS:
Scleral fixation sutures with 10–0 polypropylene provide excellent long-term fixation of PCIOLs, with a less than 0.5% incidence of suture breakage and documented suture stability for up to 24+ years.
WHEN THERE IS ABSENT OR INADEQUATE capsular support, there are many options for alternative means of support for an intraocular lens (IOL).1–9 Successful techniques have included using an anterior chamber IOL, preferably with an open-loop haptic configuration; iris fixation of posterior chamber IOL (PCIOL) with sutures, and scleral fixation of PCIOL. Anterior chamber IOLs, even with an open-loop configuration, still may be associated with a variety of complications, including corneal endothelial cell loss, glaucoma, hyphema, inflammation, and cystoid macular edema.10,11 Because of these risks, scleral fixation of PCIOLs remains a widely used technique around the world in eyes with inadequate residual capsular support for PCIOL implantation. Placement of the IOL in the posterior chamber has many benefits, including minimizing aniseikonia and positioning the lens further away from anterior segment structures such as the corneal endothelium and the trabecular meshwork, minimizing the risk of bullous keratopathy and glaucoma.10,11
Scleral fixation of PCIOLs with sutures continues to be a widely used option for management of dislocated PCIOLs, especially in Asia and Latin America, where in 2015 it was still the most prevalent technique in the 2015 American Society of Retina Specialists Survey.12 However, there is controversy on the stability of 10–0 polypropylene sutures for scleral fixation of PCIOLs. In 2006, Vote and associates reported 61 eyes with scleral fixation of PCIOLs using 10–0 polypropylene sutures with a 26.2% suture breakage rate, and multiple suture breakages in 3 eyes.13 In 2007, Bading and associates reported on a similar series of 63 patients with scleral-fixated PCIOLs using a 2-knot technique with 1 suture attached to the haptic and 1 suture attached to the sclera underneath the scleral flap. Suture breaks were rare, occurring at 15 and 54 months, with a 3.2% rate of suture breakage.14
Other methods of scleral fixation of the haptics of PCIOLs have now been innovatively developed, including the use of scleral tunnels,15 the use of a flanged intrascleral technique,16 the use of biologic glue to seal the haptics intrasclerally,17 and the use of alternative sutures, such as Gore-tex (W.L. Gore & Associates, Elkton, Maryland, USA)18 or 9–0 polypropylene sutures.19 These fixation techniques are promising, but there is not long-term follow-up for most of these procedures.
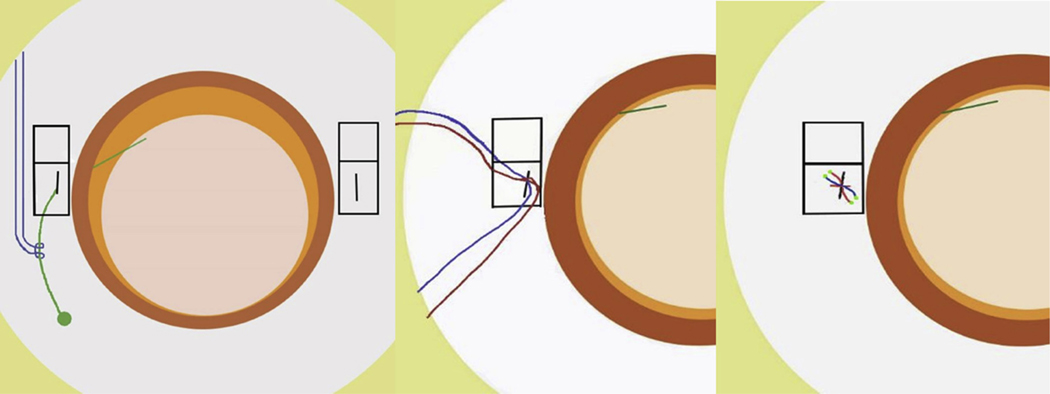
In order to reevaluate the stability and long-term results of 10–0 polypropylene sutures for scleral fixation of PCIOLs, herein we report a retrospective study of scleral-fixated PCIOLs with follow-up up to 24.75 years. A suture knot technique involving 2 separate sutures tied together in 1 knot was used after externalization of the haptic through a clear corneal incision2,8 or through a fixation sclerotomy site.3 The haptic is defined as the part of the PCIOL that provides support for fixation of the optic of the PCIOL, and can be made of the same flexible material as the optic (foldable PCIOL), a different material (polypropylene), or the less flexible polymethylmethacrylate (PMMA) support structures with a nonfoldable PMMA optic. Externalization procedures bring the haptic outside of the eye, allowing placement of the sutures around the haptic by direct visualization.2,3,8,9 One suture was looped securely around the haptic with a strap hitch knot, commonly used to attach luggage tags, or a cow hitch knot (Figure, Left, blue suture). The haptic with the attached strap hitch knot is then reimplanted behind the iris. A separate 10–0 polypropylene suture on a short curved needle is used to close the fixation sclerotomy site with 1 triple-throw knot (red suture, Figure) and to create the fixation to the sclera. Then the sutures attached to the haptic with a strap hitch are tied together in 1 knot to the 10–0 polypropylene sutures, closing the fixation sclerotomy. This 1 knot involves 1 triple-throw knot with 2 subsequent single-throw knots to create the fixation suture. The suture ends are melted using a low-temperature cautery to create a bulb on the ends of the 10–0 polypropylene sutures. This is then covered with a scleral flap with closure with 10–0 black nylon sutures. In this study, we evaluate the long-term stability of 10–0 polypropylene scleral-fixation sutures for the fixation of scleral-fixated PCIOLs using this suture knot placed after haptic externalization.
FIGURE.
Suture-tying technique used for 10–0 polypropylene fixation suture knot around the haptic of a posterior chamber intraocular lens. (Left) Haptic has been externalized through the fixation sclerotomy made 2 mm posterior to the surgical limbus. The 10–0 polypropylene loop (blue suture) has been attached to the haptic using a strap hitch. An inferior based rectangular scleral flap has been dissected to cover each fixation suture knot. (Middle) The haptic is then reimplanted into the eye through the fixation sclerotomy with the strap hitch (blue suture) attached to the haptic. A separate 10–0 polypropylene suture is then placed across the fixation sclerotomy (red suture) to both close the sclerotomy and create the scleral fixation. (Right) The 2 separate 10–0 polypropylene sutures (red and blue) are tied together in 1 secure 3-1-1 knot, creating the scleral fixation. The ends of the suture have been melted to a bulb to minimize the risk of being exposed through the scleral flap or through the conjunctiva. The scleral flap is then tacked down using 10–0 nylon sutures to cover the fixation suture knot.
METHODS
A RETROSPECTIVE, CONSECUTIVE, INTERVENTIONAL CASE series study was performed at the Hawaii Macula and Retina Institute and Retina Consultants of Hawaii in Honolulu, Hawaii, involving 111 patients who underwent pars plana vitrectomy with sutured scleral fixation of a PCIOL by a single surgeon (G.T.K.) from January 25, 1990 to October 18, 2012. This retrospective study was deemed exempt from institutional review board approval by the Western Institutional Review Board (#1-860649-1). This study conformed to the guidelines of the Health Insurance Portability and Accountability Act (HIPAA) and of the Declaration of Helsinki. Inclusion criteria for this retrospective study were at least 2 years of follow-up after vitrectomy with placement of a 10–0 polypropylene suture to scleral-fixate at least 1 haptic of a PCIOL by a single surgeon (G.T.K.).
The charts of 111 patients (118 eyes) were reviewed in this case series. Each patient was examined at baseline and postoperatively by a vitreoretinal specialist (G.T.K.). Preoperative examination was particularly important to determine the amount of capsular support and the integrity of the zonules. The preoperative data recorded were preoperative diagnosis, indication for surgery, age, sex, Snellen best-corrected visual acuity (BCVA), and lens status. Dislocated IOL was defined as an IOL with the optic out of the visual axis. Subluxated IOL was defined as an IOL out of position but with the optic still in the visual axis. In-the-bag IOL dislocations are the most common presentation of IOL dislocations and are attributable to the entire PCIOL and capsular bag complex dislocating owing to weakness of zonular support. Intraoperative data collected included the date of the surgery, operated eye, procedure performed, distance of the scleral fixation sutures posterior to the limbus, and number and location of scleral fixation sutures. Postoperative data included BCVA at last follow-up, length of follow-up period, complications, the stability and position of the PCIOL, the development of any fixation suture breakage, and reoperation for any complications or any recurrent dislocated PCIOL. The primary outcomes at last follow-up were position of the PCIOL, dislocation of either 1 or both haptics of the sutured PCIOL, and evidence of suture breakage.
SURGICAL TECHNIQUE: Scleral fixation of the PCIOLs was performed using a haptic externalization technique. The haptic was externalized through a fixation sclerotomy or through a clear corneal incision. Once the 10–0 polypropylene suture was looped around the haptic in a strap hitch (Figure, Left, blue suture), the haptic with the suture loop attached was then reimplanted into the ciliary sulcus. This was performed as previously described in the literature, either through a clear corneal incision2 or through a fixation sclerotomy.3 Prior to surgery the type of dislocated PCIOL was noted and the amount of residual capsular support was assessed. If there was capsular support of 180 degrees or more, then capsular fixation was considered for 1 haptic. If there was poor and inadequate capsular support, then a scleral fixation suture was planned for both haptics, and residual capsule was removed during vitrectomy. Inferiorly based scleral flaps were dissected at the site of future scleral fixation, which were usually centered at the 2 o’clock and 8 o’clock positions, if 2 fixation sutures were performed. The location of the fixation sclerotomy posterior to the limbus and within the bed of the scleral flap was marked at the appropriate measured distance from the limbus—usually 1.0–2.0 mm posterior to the limbus during the course of this study. When sclerotomy externalization was used, the 20 gauge sclerotomy within the bed of the scleral flap was made using a 20 gauge vitrectomy surgical blade, which is large enough to allow the haptic to be externalized with a straight horizontal forceps grasping the very tip of the haptic. If a clear corneal externalization was performed, a 15-degree blade was used to create a paracentesis to externalize the haptic, which then allowed direct visualization for placement of the 10–0 polypropylene suture loop around the haptic (Figure, Left, blue suture). Following vitrectomy the dislocated IOL was stabilized in the vitreous cavity to allow the visualization of the very tip of the haptic, which was then grasped and externalized through the fixation sclerotomy3 or through the clear corneal incision.2 Externalization of the haptic through the sclerotomy minimizes surgical maneuvers, but it has the disadvantage of the externalization technique occurring blindly behind the iris, and haptic damage can occur. Externalization of the haptic through the clear cornea allows direct visualization of the haptic during the externalization procedure, but it requires manipulation in the anterior segment with risk of iris and corneal damage. If the haptic is grasped at its very tip during externalization of the haptic through the fixation sclerotomy, then the risk of haptic damage can be minimized. The fixation suture knot is the same regardless of what externalization technique is used. The haptic was cauterized at the end to prevent fixation suture knot slippage and to minimize risk of future suture knot exposure of sharp ends through the conjunctiva. The 10–0 polypropylene suture was attached in a long loop with both ends attached to a PC9 needle (Alcon Laboratories, Fort Worth, Texas, USA) or to 2 separate CIF-4 needles (Ethicon, Johnson and Johnson, Somerville, New Jersey, USA). The 10–0 polypropylene was lassoed around the haptic and tightened. The haptic with the tightened 10–0 polypropylene loop was then reimplanted into the eye through the fixation sclerotomy or through the clear corneal incision. This suture around the haptic was then tied together in 1 knot with a separate 10–0 polypropylene suture placed through the sclera to close the fixation sclerotomy.2 If the haptic suture fixation was planned for 2 haptics, a similar procedure was performed 180 degrees away from the first fixation sclerotomy. If there was felt to be enough residual capsular support, then the other haptic was placed in the ciliary sulcus over residual capsule. To close the scleral flap, 10–0 black nylon sutures were used to cover the fixation suture knot.
RESULTS
IN THIS STUDY 118 EYES OF 111 PATIENTS REQUIRED scleral fixation with 10–0 prolene sutures to stabilize the position of the intraocular lens. The average patient age was 67 years (range 27–92 years) and there were 68 (61%) male and 43 (39%) female patients. The operative eye was the right eye in 54 cases (45.8%) and the left eye in 64 cases (54.2%). Preoperative diagnosis was dislocated or subluxated PCIOLs in 72 eyes (61.0%), in-the-bag PCIOL dislocations in 29 eyes (24.6%), crystalline lens dislocations or subluxations in 11 eyes (9.3%), anterior chamber IOL complications in 2 eyes (1.7%), and aphakia in 4 eyes (3.4%).
All patients had follow-up of at least 2 years, with a mean follow-up of 6.0 years (range 2.0–24.75 years). Mean preoperative vision was 20/270, which improved to 20/100 postoperatively for 118 eyes. Sixty-nine eyes (58.5%) had improvements of 2 lines in visual acuity, 29 eyes (24.6%) remained stable, and 20 eyes (16.9%) had a decrease of 2 lines in visual acuity. Of those 20 eyes, 3 experienced corneal edema; 2 had retinal detachments, which occurred 8 and 13 months after scleral-fixation surgery; 6 had advanced glaucoma and optic atrophy; 4 had macular scarring and fibrosis; 1 had epiretinal membrane; 1 had neovascular glaucoma, which occurred 4 years after scleral-fixation surgery; 1 had acute retinal necrosis; and 2 had unknown causes for decreased vision.
The operative procedure performed was repositioning of an IOL with scleral fixation in 77 eyes (65.2%), intraocular lens implant exchange for a sutured PCIOL in 25 eyes (21.2%), and pars plana lensectomy with scleral-fixated PCIOL in 16 eyes (13.6%). In 21 eyes (17.8%) only 1 haptic required scleral fixation because of use of residual capsular support for fixation of the other haptic. The majority of eyes, 96 eyes (81.4%), required sutured scleral fixation of both haptics. One case was a reoperation case in which a previous scleral fixation suture placed elsewhere was removed and replaced with the suture knot and repositioning technique used in this study. A total of 214 scleral fixation sutures were placed for haptic fixation to the sclera out of 236 haptics in this study. Sutures were placed 1.00 mm posterior to the limbus in 5 eyes (4.24%), 1.25 mm posterior to the limbus in 46 eyes (38.98%), 1.33 mm posterior to the surgical limbus in 8 eyes (6.78%), 1.50 mm posterior to the surgical limbus in 16 eyes (13.56%), 1.75 mm posterior to the surgical limbus in 10 eyes (8.47%), 2.00 mm posterior to the surgical limbus in 20 eyes (16.95%), and an unknown distance in 13 eyes (11.02%).
The optic was postoperatively in good position in 116 out of 118 eyes. There were 2 decentered PCIOLs that did not undergo repositioning because the visual prognosis was poor and the patient elected not to pursue further surgery. One lens dislocated after 2.5 months and the other subluxated after 12.4 months. In both cases, only 1 haptic was secured with a scleral fixation suture while the other haptic was placed over residual capsule. Both PCIOLs dislocated owing to slippage of the haptic out of position from the residual capsule support, as the implant remained fixated at the site of the scleral fixation suture. Of the 116 well-centered implants, 1 eye required reoperation after 4.98 years owing to an apparent broken fixation suture. Intraoperatively, in this case 1 scleral fixation suture was noted to be missing around an intact PCIOL, suggesting that suture breakage had occurred. In 1 case at 21 years there was redislocation owing to instability of 1 haptic. Intraoperatively, the fixation suture was intact, but the haptic had broken from its fixated portion. This damaged dislocated PCIOL required removal and exchange for a new scleral-fixated PCIOL. Out of the 214 fixation sutures evaluated in this study, there was only 1 sutured scleral fixation suture (0.47%) that was noted to be broken, with a minimum follow-up of 2 years, a mean follow-up of 6.0 years, a median follow-up of 5.0 years, and a maximal follow-up without breakage of 24.75 years. The length of follow-up was less than 5 years in 59 eyes (50.0%), 5–10 years in 45 eyes (38.1%), and more than 10 years in 14 eyes (11.9%). The redislocation rate was 3.4% (4/118 eyes), of which 2 redislocations were owing to loss of capsular support for 1 haptic, 1 was owing to suture breakage as noted above, and 1 was because of haptic breakage at 21 years with both scleral fixation sutures intact. In this case during the repositioning surgery, both scleral fixation sutures were intact, and there was a broken haptic, which caused the redislocation after 21 years. The fixation suture was directly visualized as being intact and holding the broken piece of the haptic in place.
The conjunctiva and scleral flap coverage of all fixation sutures was carefully assessed through follow-up evaluations. To decrease the risk of the sharp edge of the polypropylene suture poking through the conjunctiva, a bulb was created at the end of the fixation sutures by melting the end of the sutures with a low-temperature cautery. There were 6 fixation suture exposures in this study. In each case graft material was used to cover the fixation suture. Pericardial grafts were used in 4 eyes, bank sclera was used in 1 eye, and bank corneal tissue was used in 1 eye. There were no cases of recurrent exposure. There were no cases of endophthalmitis related to an exposed fixation suture.
DISCUSSION
SCLERAL FIXATION OF PCIOLS IS A WIDELY USED METHOD OF fixation throughout the world in the absence of capsular support. Polypropylene sutures have been reported in sutured scleral fixation of PCIOLs since 1988.20 The stability of sutured scleral-fixated IOLs depends on a number of factors, including fixation technique, suture type, and knot stability. This study supports the long-term stability of 10–0 polypropylene sutures as a fixation suture for dislocated PCIOLs or secondary scleral-fixated PCIOLs. To our knowledge this is the largest study of sutured scleral-fixated PCIOLs and there was a fixation suture breakage rate of less than 0.5% in 118 eyes. This study also involved a single surgeon with a consistent method of knot tying for the 10–0 polypropylene fixation sutures. The longest stable fixated PCIOLs with intact 10–0 polypropylene sutures in this series were 21 years and 24.75 years. To our knowledge this is the longest follow-up to date in the literature on sutured scleral-fixated PCIOLs. In 1 case at 21 years there was redislocation, but the IOL haptic had broken, and both 10–0 polypropylene sutures were found to be intact intraoperatively. The broken haptic end was still attached to the 10–0 polypropylene scleral fixation suture in the ciliary sulcus. This PCIOL was exchanged for a new PCIOL with 10–0 polypropylene fixation sutures, once the old fixation suture knots were cut and removed.
Concern about the long-term stability of 10–0 polypropylene fixation sutures was raised by a report by Vote and associates with a 26.2% fixation suture breakage rate and multiple cases of recurrent dislocations. In their report, the suture was either tied to the haptic directly with a single knot or looped around the haptic with a girth hitch and then tied by a single external knot underneath a scleral flap.13 The authors attributed the redislocations to suture breakage. However, this was a multiple-surgeon series, and failing fixation sutures could also be attributable to knot instability, as well as suture stability. Another large retrospective series, by Bading and associates, did not show a high rate of suture breakage. In a series of 63 eyes with scleral-fixated PCIOLs only 2 cases developed suture breakage (3.2%) resulting in redislocation.14 This breakage occurred 15 and 54 months after suture fixation. Two different knot techniques were used in this study, with 1 requiring just 1 knot and the other, similar to our technique, requiring 2 separate sutures in 1 knot. Other causes of PCIOL malposition included 1 case of traumatic dislocation and 1 case in which the knot was in position but the haptic had slipped out of the knot.13 The authors concluded that 10–0 polypropylene fixation sutures were still adequate to correct aphakia surgically, even in younger patients.
Histopathologic studies of polypropylene sutures have shown superficial surface wrinkling, mild cracking of only 6 mm in thickness, and flaking, but this is of uncertain clinical significance in regard to suture breakage.21 In a clinicopathologic study the suture of an iris-fixated PCIOL with 10–0 polypropylene sutures was evaluated after placement had been made through the positioning holes of the PCIOL and then through the iris. The suture was recovered 11.5 years after placement, when the iris-fixated PCIOL redislocated. The 10–0 polypropylene suture was retrieved and evaluated with scanning electron microscopy. There was no evidence of cracking, wrinkling, or flaking of the 10–0 polypropylene suture. There was evidence of a cut edge of the 10–0 polypropylene suture, which was felt to be caused by the sharp edge of the positioning hole of the PCIOL (Cilco MC71CM) cutting through the iris-fixation suture.22 This sharp edge of the positioning hole was also imaged by scanning electron microscopy. Price and associates used regular light microscopy to analyze 10–0 polypropylene sutures.19 These studies noted transverse cracking on the surface of the 10–0 polyproplylene suture, but it is uncertain what impact these superficial changes have on the strength of the suture.
The stability of suture knots depends on a number of factors, including fixation technique, knot-tying technique, trauma to suture during manipulation, and long-term suture stability. Fixation techniques are markedly varied in the literature, and often include a suture loop around a haptic tied together with 1 square knot on the outside of the eye. Other techniques include a tightened cow hitch or strap hitch around the haptic, which is tied together with a separate intrascleral suture closing the fixation sclerotomy, as in this series (Figure). McAllister and Hirst used a single-knot technique and reported suture breakage in 5 of 82 patients (6.1%) 4.9 years after surgery.23 Possible differences in study results could be related to knot technique. Other factors could include different suture manufacturers than the sutures used in this study (Alcon or Ethicon 10–0 polypropylene sutures). Polypropylene is a synthetic, monofilament, nonabsorbable suture that is durable and is the mainstay of sutures used in vascular anastomosis in cardiovascular and vascular surgery. Polypropylene suture is more difficult to handle than other sutures owing to suture memory with more rebound, and more slippery handling characteristics, which could affect knot stability. Muffly and associates note that knot security is dependent on suture type, suture gauge, and knot configuration.24 Gore-tex is a potential long-term fixation suture, as it is a soft microporous monofilament suture that is soft, flexible, and compressible. These characteristics could allow improved and more secure knot-tying ability, but the follow-up of Gore-Tex PCIOL fixation sutures is much shorter than for 10–0 polypropylene sutures.
Many large retrospective studies have now reported a low rate of redislocation with 10–0 polypropylene sutures. In a large study of 284 eyes by Kim and associates, the incidence of redislocation was 6%.7 In our study of 118 eyes with follow-up ranging from 2 to 24.75 years, there was a redislocation rate of 3.4%. However, only 1 case was owing to suture breakage (0.47%); in 2 cases loss of capsular support resulted in redislocation; and in the other case the haptic had broken and both haptics were still fixated with the fixation sutures. In the study by Bading and associates there was a 6.3% redislocation rate, but only 2 were related to suture breakage (3.2% suture breakage rate).14 With 3 large studies showing a redislocation rate of 6% or less, this supports that pars plana vitrectomy with placement of sutured scleral-fixated PCIOLs remains an effective and long-term procedure to manage situations with poor capsular support. In addition, the incidence of suture breakage is very low, especially considering that the longest reported stable sutured fixation of a PCIOL was documented at 21 years and 24.75 years in 2 separate cases in this study. Their series had a different mix of patients, with 43% of cases involving Marfan syndrome, whereas the Moorfield series included 25% with complicated cataract surgery and 24% with pseudoexfoliation. However, it is uncertain if these varying indications would affect fixation suture stability.
The surgical technique used in this study is a modification of the haptic externalization techniques through the fixation sclerotomy as described by Chanin19923 or the haptic externalization technique through a clear corneal incision reported by Kokame and associates.2 The advantage of haptic externalization is that it allows direct visualization for placement and tightening of the suture loop around the haptic. The benefit of the knot technique used in this study is that it incorporates 2 separate 10–0 polypropylene sutures in 1 knot. One suture is securely looped and tightened in a strap hitch or cow hitch around the haptic.2 The other 10–0 Polypropylene suture is used to close the fixations clerotomy site, where the haptic was externalized.2 The 2 10–0 polypropylene sutures are then tied together in 1 knot to create the scleral fixation. The fixation sclerotomies were placed 1.0–2.0 mm posterior to the limbus within the bed of the scleral flap, but we now place all fixation sclerotomies 2 mm or more posterior to the limbus, owing to the risk of optic capture, iris chafing, glaucoma, and uveitis.
Pars plana vitrectomy with placement of sutured scleral-fixated PCIOLs remains a widely used treatment option in the management of dislocated PCIOLs or for PCIOL placement in the absence of capsular or zonular support.4,12 This study supports the stability and long-term clinical efficacy of 10–0 polypropylene scleral fixation sutures. There are many promising approaches to fixation of IOLs in the absence of capsular support. Alternative options of scleral fixation include intrascleral fixation of PCIOL haptics with flanged haptics,16 scleral tunnels,15 Gore-tex sutures,18 and sutureless haptic fixation with fibrin glue,17 but length of follow-up is limited compared to the follow-up available for sutured PCIOLs with 10–0 polypropylene. In this study suture breakage with 10–0 polypropylene was very low at 1 breakage in 247 fixation sutures (0.47%), and this 1 case was successfully managed with a repeat 10–0 polypropylene fixation suture with stable positioning for more than 7 years after the second procedure. Suture fixation of PCIOLs with 10–0 polypropylene can provide long-term successful scleral fixation for dislocated PCIOLs and for secondary placement of PCIOLs in aphakic eyes without capsular support.
Acknowledgments
FUNDING/SUPPORT: NO FUNDING OR GRANT SUPPORT. FINANCIAL DISCLOSURES: GREGG T. KOKAME: RESEARCH SUPPORT: Genentech, Regeneron; Consultant: Genentech, Santen, Regeneron, Bayer, Bausch & Lomb, Zeiss, Allergan; Speaker: Regeneron, Bayer, Second Sight, Bausch and Lomb. Jessica G. Shantha: Consultant: Santen. The following authors have no financial disclosures: Ryan T. Yanagihara and Kyle N. Kaneko. The authors attest that they meet the current ICMJE criteria for authorship.
Other Acknowledgments: The authors acknowledge the editorial assistance of Maria Won, research coordinator at Hawaii Macula and Retina Institute, Aiea, Hawaii.
Footnotes
Supplemental Material available at AJO.com.
Contributor Information
GREGG T. KOKAME, Division of Ophthalmology, Department of Surgery, University of Hawaii School of Medicine, Honolulu, Hawaii The Retina Center at Pali Momi, Aiea, Hawaii; Retina Consultants of Hawaii, Aiea, Hawaii; Hawaii Macula and Retina Institute, Aiea, Hawaii.
RYAN T. YANAGIHARA, The Retina Center at Pali Momi, Aiea, Hawaii Retina Consultants of Hawaii, Aiea, Hawaii; Hawaii Macula and Retina Institute, Aiea, Hawaii; University of Hawaii John A. Burns School of Medicine, Honolulu, Hawaii.
JESSICA G. SHANTHA, The Retina Center at Pali Momi, Aiea, Hawaii Retina Consultants of Hawaii, Aiea, Hawaii; Hawaii Macula and Retina Institute, Aiea, Hawaii.
KYLE N. KANEKO, The Retina Center at Pali Momi, Aiea, Hawaii Retina Consultants of Hawaii, Aiea, Hawaii; Hawaii Macula and Retina Institute, Aiea, Hawaii.
REFERENCES
- 1.Por YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv Ophthalmol 2005;50(5):429–462. [DOI] [PubMed] [Google Scholar]
- 2.Kokame GT, Yamamoto I, Mandel H. Scleral fixation of dislocated posterior chamber intraocular lenses: temporary haptic externalization through a clear corneal incision. J Cataract Refract Surg 2004;30(5):1049–1056. [DOI] [PubMed] [Google Scholar]
- 3.Chan CK. An improved technique for management of dislocated posterior chamber implants. Ophthalmology 1992;99(1):51–57. [DOI] [PubMed] [Google Scholar]
- 4.Dajee KP, Abbey AM, Williams GA. Management of dislocated intraocular lenses in eyes with insufficient capsular support. Curr Opin Ophthalmol 2016;27(3):191–195. [DOI] [PubMed] [Google Scholar]
- 5.Smiddy WE, Flynn HW Jr. Needle-assisted scleral fixation suture technique for relocating posteriorly dislocated IOLs. Arch Ophthalmol 1993;111(2):161–162. [DOI] [PubMed] [Google Scholar]
- 6.Lawrence FC II, Hubbard WA. “Lens lasso” repositioning of dislocated posterior chamber intraocular lenses. Retina 1994;14(1):47–50. [PubMed] [Google Scholar]
- 7.Kim SS, Smiddy WE, Feuer W, Shi W. Management of dislocated intraocular lenses. Ophthalmology 2008;115(10): 1699–1704. [DOI] [PubMed] [Google Scholar]
- 8.Kokame GT, Atebara NH, Bennett MD. Modified technique of haptic externalization for scleral fixation of dislocated posterior chamber lens implants. Am J Ophthalmol 2001;131(1):129–131. [DOI] [PubMed] [Google Scholar]
- 9.Chan CK, Agarwal A, Agarwal S, Agarwal A. Management of dislocated intraocular implants. Ophthalmol Clin North Am 2001;14(4):681–693. [DOI] [PubMed] [Google Scholar]
- 10.Numa A, Nakamura J, Takashima M, Kani K. Long-term corneal endothelial changes after intraocular lens implantation. Anterior vs posterior chamber lenses. Jpn J Ophthalmol 1993;37(1):78–87. [PubMed] [Google Scholar]
- 11.Huang YS, Xie LX, Wu XM, Han DS. Long-term follow-up of flexible open-loop anterior chamber intraocular lenses implantation. Zhonghua Yan Ke Za Zhi 2006;42(5):391–395 [in Chinese]. [PubMed] [Google Scholar]
- 12.Rezeai KA, Stone TW, eds. 2015 Global Trends in Retina Survey. Chicago, Illinois: American Society of Retina Specialists; 2015. [Google Scholar]
- 13.Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol 2006;141(2):308–312. [DOI] [PubMed] [Google Scholar]
- 14.Bading G, Hillenkamp J, Sachs HG, Gabel VP, Framme C. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol 2007;144(3):371–377. [DOI] [PubMed] [Google Scholar]
- 15.Prenner JL, Feiner L, Wheatley HM, Connors D. A novel approach for posterior chamber intraocular lens placement or rescue via a sutureless scleral fixation technique. Retina 2012;32(4):853–855. [DOI] [PubMed] [Google Scholar]
- 16.Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology 2017;124(8):1136–1142. [DOI] [PubMed] [Google Scholar]
- 17.Agarwal A, Kumar DA, Jacob S, Bald C, Agarwar A, Srinivasan S. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation with deficient posterior capsules. J Cataract Refract Surg 2008;34(9):1433–1438. [DOI] [PubMed] [Google Scholar]
- 18.Khan MA, Gerstenblith AT, Dolin ML, Omesh P, Spirn MJ. Scleral fixation of posterior chamber intraocular lenses using Gore-tex suture with concurrent 23 gauge pars plana vitrectomy. Retina 2014;34(7):1477–1480. [DOI] [PubMed] [Google Scholar]
- 19.Price MO, Price FW, Werner L, Berlie C, Mamalis N. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg 2005;31(7):1320–1326. [DOI] [PubMed] [Google Scholar]
- 20.Hu BV, Shin DH, Gibbs KA, Hong YJ. Implantation of posterior chamber lens in the absence of zonular and capsular support. Arch Ophthalmol 1988;106(3): 416–420. [DOI] [PubMed] [Google Scholar]
- 21.Drews RC. Polypropylene in the human eye. J Am Intraocul Implant Soc 1983;9:137–142. [DOI] [PubMed] [Google Scholar]
- 22.Parekh P, Green WR, Stark WJ, Akpek EK. Subluxation of suture-fixated posterior chamber intraocular lenses a clinicopathologic study. Ophthalmology 2007;114(2): 232–237. [DOI] [PubMed] [Google Scholar]
- 23.McAllister AS, Hirst LW. Visual outcomes and complications of scleral-fixation posterior chamber intraocular lenses. J Cataract Refract Surg 2011;37(7):1263–1269. [DOI] [PubMed] [Google Scholar]
- 24.Muffly TM, Kow N, Iqbal I, Barber MD. Minimum number of throws needed for knot security. J Surg Educ 2011;68(2): 130–133. [DOI] [PubMed] [Google Scholar]