Abstract
Objectives
Due to recent developments and the wide application of percutaneous transforaminal discectomy (PTED) in China, we herein compare its clinical effects with microendoscopic discectomy (MED) for the treatment of lumbar disc herniation in terms of recurrence and revision rates.
Methods
Six databases, namely, PubMed, EMBASE, Cochrane Library, Ovid, China National Knowledge Infrastructure and Wanfang, were searched by computer. The literature was screened according to inclusion and exclusion criteria, and the quality of the included literature was evaluated. After extracting the data from the papers, Review Manager 5.2 software (Cochrane Collaboration, Oxford, UK) was applied to analyze these data. Finally, sensitivity and publication bias analyses of the results were conducted.
Results
A total of 12 studies consisting of 2400 patients were included in this meta-analysis. A comparison of PTED with MED revealed higher postoperative recurrence and postoperative revision rates for PTED (odds ratio [OR] recurrence, 1.60; 95% confidence interval [CI], 1.01 to 2.53; p=0.05 and OR revision, 1.77; 95% CI, 1.18 to 2.64, p=0.006).
Conclusion
PTED has a number of advantages because it is a minimally invasive surgery, but its recurrence and revision rates are higher than MED. Therefore, MED should not be completely replaced by PTED.
Keywords: Herniated disc, Microendoscopic discectomy, Percutaneous transforaminal discectomy, Reoperation, Recurrence, Meta-analysis
INTRODUCTION
Lumbar disc herniation (LDH) and related diseases are public health problems that negatively impact people’s health. Waist and leg pains caused by this condition have long affected the work and daily lives of people from all walks of life [23]. The basic treatment principle for LDH is that surgical treatment is required in the case of no obvious improvement after conservative treatment [1]. Traditional open surgery causes great damage to the normal tissue structure of patients [28]; thus, it is not the preferred treatment at present. In recent years, the idea of minimally invasive surgery in the spine has advanced. The two most common types of surgery are microendoscopic discectomy (MED) and percutaneous transforaminal discectomy (PTED). MED uses a working channel to extract abnormal nucleus pulposus under endoscopic vision to achieve the purpose of treatment [10,24], research has shown that MED has a significant effect in the treatment of LDH, with excellent and good rates of surgery reaching 97% [9]. It was once considered the “gold standard” for the treatment of LDH [35]. At present, many medical institutions at home and abroad are still vigorously developing this technology.
Compared with MED, a more minimally invasive technique is PTED, which originated in Europe and America [27,37] and has been further developed in east Asia. Due to the large number of patients with LDH in China, the new medical technology is easy to be popularized and applied. Meanwhile, Chinese people have a deep traditional concept and are unwilling to accept traditional open surgery with greater trauma, so PTED is developing rapidly in China. Compared with open surgery, its intraoperative trauma is small and largely maintains the stability of the lumbar spine [7], and its postoperative recovery is fast. Compared with MED, its operating channel enters into the protruding vertebral space through the natural orifice, thus greatly reducing the related complications of nerve traction. Although the minimally invasive advantages of PTED are obvious, and its efficacy is similar to that of MED, its disadvantages cannot be ignored. For example, the steep learning curve is not suitable for inexperienced physicians [14]. Additionally, it has a high intraoperative radiation exposure rate [2,8]. Recently, some studies have found that another fatal defect of PTED is that its postoperative recurrence and revision rates are much higher than those of other discectomy techniques [6,30]. Therefore, is it truly appropriate to replace MED with PTED as the standard minimally invasive operation for the treatment of LDH?
In this meta-analysis, we retrieved relevant studies to compare the two surgical methods, which are currently widely used, in terms of postoperative recurrence and revision rates. The advantages and disadvantages of various surgical methods were examined from different angles to explore whether the current treatment of LDH can be completely replaced with PTED to provide a better basis for guiding clinicians’ learning and patients’ treatment choices.
MATERIALS AND METHODS
Protocol and registration
This systematic review and meta-analysis was registered with the International Prospective Register of Systematic Reviews (PROSPERO 2018: CRD42018094890, http://crd.york.ac.uk/PROSPERO).
Inclusion criteria
Inclusion criteria : 1) type of study : all randomized controlled trials comparing PTED and MED for LDH, prospective or retrospective controlled studies; 2) treatment object : patients diagnosed with LDH; 3) intervention measures : PTED and MED as well as other interventions, but the premise is that these interventions are consistent between the groups; and 4) outcome indicators : the included studies must contain indicators of recurrence and revision rates.
Exclusion criteria
Exclusion criteria : 1) studies such as meeting summaries, reviews or meta-analyses; 2) no control group in the study, such as case series; and 3) other diseases in the study that affected the efficacy, such as spondylolisthesis and intervertebral disc calcification.
Search strategy
The PubMed, EMBASE, Cochrane Library, Ovid, China National Knowledge Infrastructure, and Wanfang databases were searched by computer without language restrictions until October 2018. According to the principles of evidence-based medical literature retrieval [26], the following were the main search terms : LDH, PTED, MED, recurrence rate, residual rate, revision rate and synonyms, etc. For some literature that was of high value and had an influence on research results but could not be obtained, relevant researchers were contacted to obtain the data.
Literature selection and quality evaluation
Two reviewers (X.Z. and L.L.) screened the literature from the database according to inclusion and exclusion criteria. After that, two other researchers (Q.Y. and Y.S.) evaluated the quality of the literature, and if their opinions were inconsistent, they discussed their opinions with each other or another researcher (Y.Z.) to make a final decision. The specific evaluation methods for the quality of the literature are listed below.
For randomized controlled trials, the modified Jadad scale was used [32]. The total score was 7, and the literature with a score of >4 was of high quality. For retrospective studies, the Newcastle-Ottawa (NOS) scale was applied [31]. The total score was 9, and the literature with a score of >6 was of high quality.
Data extraction
The included experimental data were extracted into a spreadsheet, including 1) baseline information of the included literature (author, year of publication, type of study, surgical method, number of participants, follow-up time, and included evaluation indexes) and 2) analysis indicators, namely, recurrence and residual rates and revision rate of surgery. According to the unified design table, two researchers (X.Z. and L.L.) independently extracted the data needed for the study from the included literature and exchanged the data collected for strict verification. When encountering doubts and when data indicators had different evaluation standards, another independent researcher (Q.Y.) made a decision. If missing data or incomplete indicators in the literature were beneficial to the study, the person conducting the experiment tried to communicate with the author(s) to obtain the data required for the study.
Statistical methods
The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for the counting data (postoperative recurrence and revision rates). The chi-squared test was used to compare the heterogeneity between data sets, and the test level was set as p<0.1. When p<0.1 and I2 >50%, high heterogeneity was observed. The random effect model was applied for metaanalysis, and its source was further discussed by subgroup analysis. If the heterogeneity was not significant (p>0.1, I2 <50%), the fixed-effect model was used instead. The jackknife method [22] was used for sensitivity analysis of the comprehensive analysis results of evaluation indexes, and low-quality literature and literature with too large or too small a sample size were removed successively to further investigate the stability of the obtained results. Finally, funnel plots were used to roughly judge the publication bias degree of the indexes studied according to the scatter distribution. All data were input into Review Manager 5.2 software (Cochrane Collaboration, Oxford, UK) for sorting, synthesis and analysis.
RESULTS
Literature search and quality evaluation
A total of 365 relevant studies were searched according to all methods and reference retrieval strategies formulated. After double checking with tools, 78 duplicates were removed. After reading the title and abstract, 255 studies inconsistent with the purpose, object and intervention measures of the systematic evaluation were excluded. After reading the full texts of the remaining 32 articles, 20 articles that did not meet the inclusion criteria and were not detailed in the results were excluded. The 12 remaining studies were analyzed again, and four randomized controlled trials (RCTs) were ultimately included, along with eight retrospective studies. Among them, there were seven studies from mainland China and five from Europe, America, Japan, and South Korea. There were a total of 2400 research subjects, including 1048 in the PTED group and 1352 in the MED group. The document retrieval process chart is shown in Fig. 1, the basic research information is shown in Table 1, and the quality evaluation of the research documents is detailed in Tables 2 and 3.
Fig. 1.
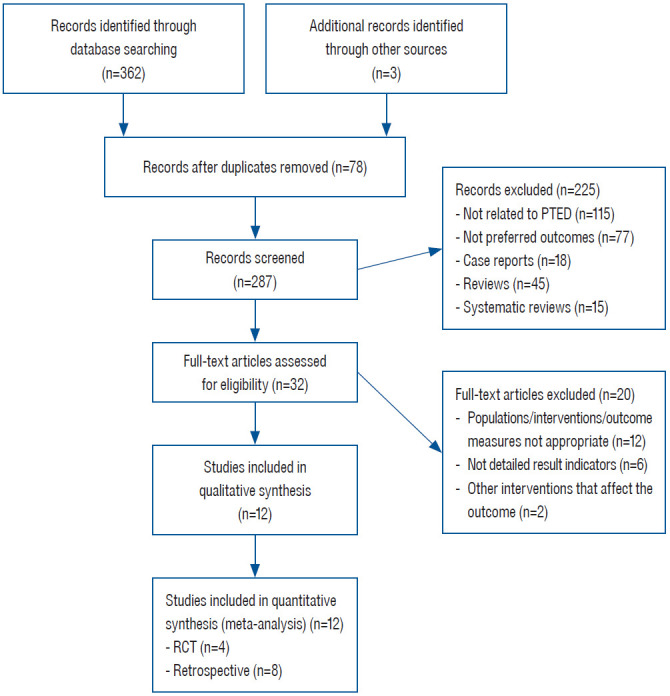
Flow chart of study selection. PTED : percutaneous transforaminal discectomy, RCT : randomized controlled trial.
Table 1.
Basic information of the studies
| Study | Number of patients |
Age (years) |
Follow-up time (months) |
Study type | Outcome | |||
|---|---|---|---|---|---|---|---|---|
| PTED | MED | PTED | MED | PTED | MED | |||
| Chen et al. [5] | 80 | 73 | 40±11.4 | 40.7±11.1 | 12 | 12 | RCT | ①, ② |
| Liu et al. [20] | 60 | 63 | 36.2±5.9 | 33.1±6.7 | 28.2±2.5 | 29.6±3.7 | Retro | ① |
| Hsu et al. [13] | 57 | 66 | 44.2 | 50.4 | 20.4 (12-24) | 20.4 (12-24) | Retro | ①, ② |
| Qu et al. [25] | 40 | 40 | 39.05±6.82 | 38.45±7.04 | 15.43±3.12 | 16.34±3.74 | RCT | ① |
| Li et al. [17] | 48 | 30 | 18.96±1.99 | 19.40±1.50 | 43.9±11.6 | 46.1±13.2 | Retro | ① |
| Choi et al. [7] | 20 | 23 | 33.9±11.1 | 27.5±5.7 | 27.5±5.7 | 27.5±5.7 | Retro | ①, ② |
| Kim et al. [16] | 301 | 614 | 34.9 | 44.9 | 23.6 (18-36) | 23.6 (18-36) | Retro | ①, ② |
| Yang et al. [36] | 82 | 57 | 48.43±0.21 | 47.95±0.22 | 3 | 3 | Retro | ① |
| Wang et al. [33] | 25 | 80 | 17.9±1.9 | 17.9±1.9 | No disicussion | No disicussion | Retro | ① |
| Gibson et al. [11] | 70 | 70 | 42±9 | 39±9 | 24 | 24 | RCT | ② |
| Zhao et al. [38] | 245 | 216 | 56.2±5.9 | 56.2±5.9 | No disicussion | No disicussion | Retro | ①, ② |
| Mayer and Brock [21] | 20 | 20 | 39.8±10.4 | 42.7±10 | 24 | 24 | RCT | ①, ② |
PTED : percutaneous transforaminal discectomy, MED : microendoscopic discectomy, RCT : randomized controlled clinical trial, ① : incidence of recurrence, ② : revision rate, Retro : retrospective study
Table 2.
Quality evaluation of retrospective clinical studies
| Included study | Study type | Rated items |
Quality score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Selection (4) |
Comparability (2) |
Outcomes (3) |
||||||||
| ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | |||
| Liu et al. [20] (2018) | Retrospective | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 (Hi-Q) |
| Hsu et al. [13] (2013) | Retrospective | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 (Hi-Q) |
| Yang et al. [36] (2015) | Retrospective | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 (Hi-Q) |
| Li et al. [17] (2018) | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Zhao et al. [38] (2012) | Retrospective | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 (Hi-Q) |
| Choi et al. [7] (2016) | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Kim et al. [16] (2007) | Retrospective | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 (Hi-Q) |
| Wang et al. [33] (2013) | Retrospective | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 (Hi-Q) |
① : case definition, ② : representativenes, ③ : control selection, ④ : control definition, ⑤ : A/B : the comparability of cases and controls in design and statistical analysis, ⑥ : ascertainment of exposure, ⑦ : same method of ascertainment for cases and controls, ⑧ : non-response rate
Table 3.
Quality evaluation of randomized controlled clinical trials
| Study | Study type | Randomization (2) | Concealment of allocation (2) | Double blinding (2) | Withdrawals and dropouts (1) | Quality evaluation |
|---|---|---|---|---|---|---|
| Chen et al. [5] (2018) | RCT | 2 | 2 | 2 | 1 | High quality |
| Gibson et al. [11] (2017) | RCT | 2 | 2 | 1 | 1 | High quality |
| Qu et al. [25] (2017) | RCT | 2 | 1 | 0 | 1 | High quality |
| Mayer and Brock [21] (1993) | RCT | 2 | 1 | 0 | 1 | High quality |
RCT : randomized controlled clinical trial
Outcomes
Recurrence rates of surgery
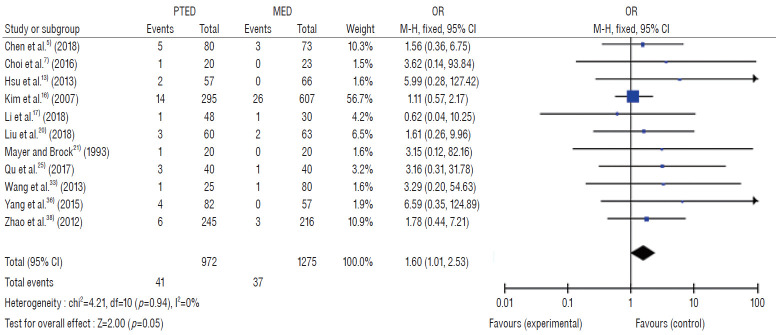
The recurrence rates of the PTED and MED groups were reported in 11 references [5,7,13,16,17,20,21,25,33,38], including 972 in the PTED group and 1275 in the MED group, with no obvious heterogeneity between groups (p=0.94, I2=0%), and a fixed effects model was applied. The results showed that the recurrence and residual rates after PTED were high, and the differences were statistically significant (OR recurrence, 1.60; 95% CI, 1.01 to 2.53; p=0.05) (Fig. 2).
Fig. 2.
Meta-analysis for recurrence rate between PTED and MED. PTED : percutaneous transforaminal discectomy, MED : microendoscopic discectomy, OR : odds ratio, M-H : mantel-hensel test, CI : confidence interval.
Revision rate of surgery
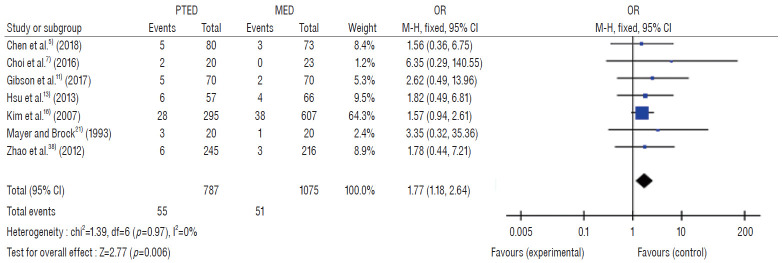
The revision rates of the PTED and MED groups were reported in seven references [5,7,11,13,16,21,38], including 787 in the PTED group and 1075 in the MED group, with no obvious heterogeneity between groups (p=0.97, I2=0%), and a fixed effects model was applied. The results showed that the revision rates after PTED were high, and the differences were statistically significant (OR, 1.77; 95% CI, 1.18 to 2.64; p=0.006) (Fig. 3).
Fig. 3.
Meta-analysis for revision rate between PTED and MED. PTED : percutaneous transforaminal discectomy, MED : microendoscopic discectomy, OR : odds ratio, M-H : mantel-hensel test, CI : confidence interval.
Publication bias analysis
To evaluate the degree of publication bias, the funnel plot method was used. An inverted funnel plot corresponding to each index was observed, and the results of the recurrence and revision rates were mainly distributed on the right side of the funnel plot, with visual asymmetry on the left and right sides, suggesting the possibility of publication bias in this study. Different surgeons had different levels of surgical proficiency; no specific distinction was made for the orifice approach; the randomization method of RCTs was unknown; and the differences in language and in year of publication all had certain effects on publication bias (Figs. 4 and 5).
Fig. 4.
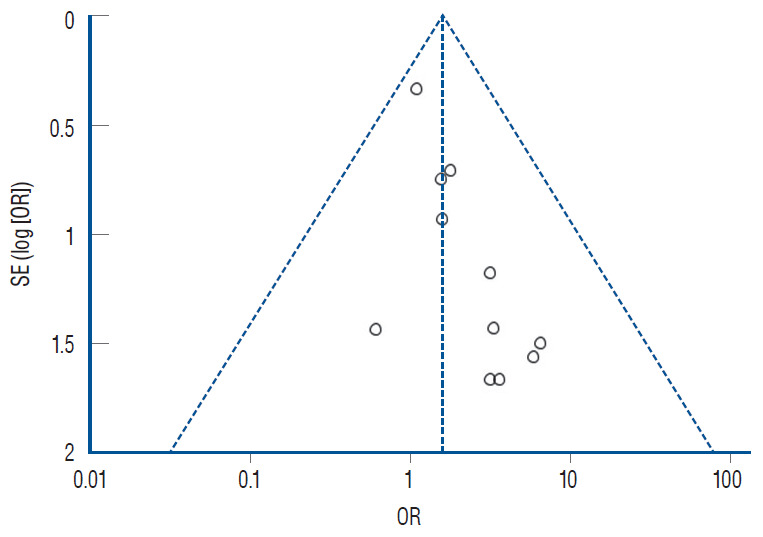
Funnel plot of PTED and MED for recurrence rate. SE : standard error, OR : odds ratio, PTED : percutaneous transforaminal discectomy, MED : microendoscopic discectomy.
Fig. 5.
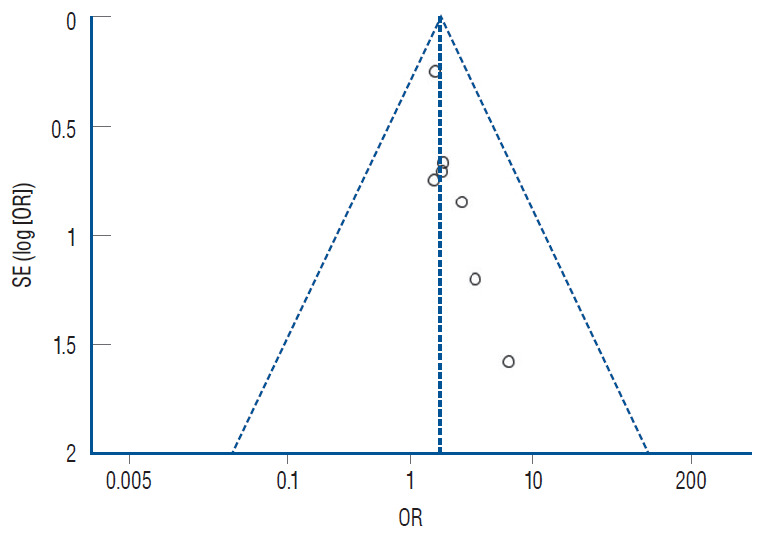
Funnel plot of PTED and MED for revision rate. SE : standard error, OR : odds ratio, PTED : percutaneous transforaminal discectomy, MED : microendoscopic discectomy.
Sensitivity analysis
To ensure the stability of the conclusion, sensitivity analysis was adopted to exclude those with a large sample size (n>200), small sample size (n<20), and low literature quality (NOS<6). It was found that the literature quality level was relatively high, two references had a large sample size [16,38], and no study had a small sample size. After exclusion, the recurrence and revision rates of PTED were still higher than those of MED (OR recurrence, 2.38; 95% CI, 1.11 to 5.10; p=0.03) (OR revision, 2.23; 95% CI, 1.04 to 4.78; p=0.04). There was no significant difference between the evaluation index and the previous combined results, indicating that the meta-analysis results were relatively stable and reliable.
DISCUSSION
In recent years, due to the great advantages of the minimally invasive PTED, domestic hospitals have begun to strongly advocate PTED, and its indications have been gradually relaxed. Relevant studies have shown [7,28,34] that PTED has limitations in the treatment of disc herniation, and its surgical efficacy and safety are the same as that of traditional surgery. However, from the perspective of recurrence and revision rates, its long-term efficacy is not better than other methods of disc surgery. Therefore, is it reasonable to blindly consider the use of PTED, the emerging minimally invasive surgery, as a complete replacement for MED?
Different from previous studies, this meta-analysis abandoned a variety of minimally invasive indicators, such as incision size, intraoperative blood loss, postoperative recovery time, etc. (relevant meta-analysis mainly discussed the minimally invasive advantages of PTED, and most agreed that PTED was the mainstream minimally invasive surgical method for the treatment of LDH). In this meta-analysis, comparative studies on the treatment of LDH by PTED and MED were searched in terms of postoperative recurrence and revision rates. A comprehensive analysis of big data clinical studies further confirmed the conclusions of other studies. It was found that the recurrence and revision rates of PTED were higher than those of MED (OR recurrence, 1.60; 95% CI, 1.01 to 2.53; p=0.05) (OR revision, 1.77; 95% CI, 1.18 to 2.64; p=0.006). This finding is a wake-up call for our current blind use of minimally invasive PTED surgery and provides an improved direction for the future treatment of LDH.
Both PTED and MED are minimally invasive methods for the treatment of LDH. They represent the development and progress of endoscopy in spine surgery in the 21st century, and each has its unique advantages. MED is a combination of microscopy and traditional fenestration, which is actually a minimally invasive approach to traditional surgery, largely compensating for the defects of open surgery. At the same time, the subsequent microscopy approach is operated under direct vision, inheriting the advantages of traditional fenestration surgery. This approach gives the surgeon a clear understanding of the anatomical structure, allowing more complete removal of the herniated disc tissue. In addition, the learning curve is short, meaning that this procedure is also suitable for unskilled physicians to learn and apply widely.
PTED is performed under local anesthesia. It is conducted through the natural orifice, which greatly reduces a series of complications caused by the pulling of the dural sac and nerve root, and it maximally protects the surrounding bone structure and soft tissue [7]. Under local anesthesia, patients with slight pain and numbness can be timely fed back to the surgeon, making the decompression of nerve roots safer and avoiding the risk of iatrogenic injury to a great extent. At the same time, after decompression of the intervertebral disc, patients can feel significant relief of lumbar and leg pain during the operation [18], and the straight leg elevation test can be tested during the surgery, which is helpful for doctors to make a better judgment on the thoroughness of surgical decompression. In addition, an 8-mm minimally invasive incision, blunt tissue separation and intraoperative bipolar radiofrequency hemostasis significantly reduce intraoperative blood loss as well as postoperative scarring and adhesion. The postoperative infection rate is low [12], with a short postoperative time to ambulation, and the total length of hospitalization is significantly reduced [15].
For various discectomy, there are many reasons for recurrence and revision, including incomplete removal of nucleus pulposus, preoperative lumbar instability, high degree of lumbar disc degeneration, incorrect postoperative rehabilitation training, intraoperative rupture of annulus fibrosus, etc. However, numerous studies have shown [4,34] that the most common cause is incomplete intraoperative clearance of herniated disc tissue. After surgery, there may be more or less residual nucleus pulposus, which may result in reherniation of the disc tissue at the initial lesion segment, leading to symptom recurrence. Conservative treatment failed and revision surgery had to be performed again. We can see from the results of this study that MED has certain advantages over PTED, whose recurrence and renovation rates are higher than those of MED. From the technical aspects of these two surgical methods, the main reason is that PTED is performed under nondirect vision. The difficulty of instrument operation combined with the blind field makes it difficult to fully expose the hidden structures in the spinal canal. During the operation, the operator needs to constantly change the channels to comprehensively identify various anatomical structures to prevent damage to nerve roots and the dural sac, resulting in incomplete resection of the herniated intervertebral disc tissue [3]. At the same time, undetected nucleus pulposus is one of the reasons for recurrence in patients with nucleus pulposus protruding upward or downward or even dissociating [19]. However, for MED, posterior approach microscopy is a direct vision operation, which can clearly expose the anatomical structures of each layer. To a large extent, the surgeon is able to completely remove the disc. However, the annulus fibrosus incurs a great deal of damage during poroscopy. Once the annulus fibrosus is ruptured, the healing scar tissue at the wound will become relatively weak, making the residual nucleus pulposus easy to be highlighted from the weak spot. In addition, the learning curve of PTED is steeper than that of MED due to it being a nondirect vision operation [29]. Although the preoperative exposure and postoperative suture processes do not require much time, the difference in anatomical structure and the narrow operating space require doctors with many years of open surgical expertise to carry out it easily. Study has shown that there is a close relationship between the recurrence rate of PTED in the early postoperative period (within half a year) and the surgical skills level of the surgeon. Unskilled doctors are inexperienced and have poorer spatial and stereoscopic thinking abilities, making it difficult to deal with various types of complications during the operation, leading to fewer successful surgeries. In addition, study [4] has found that when the nucleus pulposus is not completely removed, the increase in postoperative activity can lead to the re-herniation of residual nucleus pulposus, thus increasing the risk of recurrence. Compared with MED, the earlier time of getting out of bed, and the early and incorrect rehabilitation training may also have something to do with the high recurrence rate of PTED. All of the above reasons may underlie the increase in the recurrence and revision rates of PTED compared with MED.
This study has the following shortcomings : 1) as postoperative recurrence is one of the reasons leading to surgical revision, the postoperative recurrence rate and revision rate in this study are overlapped to a certain extent. 2) Due to the limited control experiments on the intervertebral foraminoscope and other surgical methods in the database, relatively few studies were included in this meta-analysis, and most of them were small, with the exception of a few large-sample studies. 3) As for the criteria of postoperative recurrence rate, this study did not make a unified definition, which may lead to different recurrence rates among different literatures and have certain influence on the results. 4) The average follow-up times of the included studies were mostly in the range of 1–2 years; a longer follow-up time is needed to determine the long-term efficacy of the two surgical methods. And 5) the application of completely randomized controlled trials in the field of surgery is relatively difficult, meaning that several retrospective studies and few RCTs were included in this study; and the randomization methods were not detailed, and whether blind methods were used was not reported, which may have caused bias in the research results.
CONCLUSION
In summary, compared with MED, the postoperative recurrence and revision rates of PTED are higher than those of MED, despite its minimally invasive advantages to some extent. This is closely related to the incomplete resection of intervertebral disc tissue by PTED and is also a general indication that we need to further develop and improve the surgical methods of PTED at present. Therefore, in conclusion, the advantage of PTED is that it is minimally invasive; however, its disadvantages also stem from its minimally invasive nature.
Acknowledgments
This study was supported by grants (No. 81371987) from the National Natural Science Foundation of China and also by 2016 Clinical Research Special Award of Xi’an Jiaotong University, China (No. XJTU1AF-CRF-2016T-15).
Footnotes
No potential conflict of interest relevant to this article was reported.
INFORMED CONSENT
Informed consent was obtained from all individual participants included in this study.
AUTHOR CONTRIBUTIONS
Conceptualization : XZ
Data curation : QY, LL
Formal analysis : QY
Funding acquisition : XZ, LL
Methodology : YS
Project administration : YZ
Visualization : XZ, LL
Writing - original draft : XZ
Writing - review & editing : XZ
References
- 1.Ahn SS, Kim SH, Kim DW, Lee BH. Comparison of outcomes of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for young adults: a retrospective matched cohort study. World Neurosurg. 2016;86:250–258. doi: 10.1016/j.wneu.2015.09.047. [DOI] [PubMed] [Google Scholar]
- 2.Ahn Y, Kim CH, Lee JH, Lee SH, Kim JS. Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine (Phila Pa 1976) 2013;38:617–625. doi: 10.1097/BRS.0b013e318275ca58. [DOI] [PubMed] [Google Scholar]
- 3.Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976) 2004;29:E326–E332. doi: 10.1097/01.brs.0000134591.32462.98. [DOI] [PubMed] [Google Scholar]
- 4.Chen GY, Xie E, Zhang ZX, Hao DJ, Fan Y, Li FH. Multiple factors influencing the postoperative recurrence of lumbar disc herniation treated with lumbar discectomy. Chin J Bone Joint. 2018;6:437–441. [Google Scholar]
- 5.Chen Z, Zhang L, Dong J, Xie P, Liu B, Wang Q, et al. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J Neurosurg Spine. 2018;28:300–310. doi: 10.3171/2017.7.SPINE161434. [DOI] [PubMed] [Google Scholar]
- 6.Choi G, Kang HY, Modi HN, Prada N, Nicolau RJ, Joh JY, et al. Risk of developing seizure after percutaneous endoscopic lumbar discectomy. J Spinal Disord Tech. 2011;24:83–92. doi: 10.1097/BSD.0b013e3181ddf124. [DOI] [PubMed] [Google Scholar]
- 7.Choi KC, Kim JS, Park CK. Percutaneous endoscopic lumbar discectomy as an alternative to open lumbar microdiscectomy for large lumbar disc herniation. Pain Physician. 2016;19:E291–E300. [PubMed] [Google Scholar]
- 8.Farace DJ, Frantzen J. Perspectives on the design and transfer of scientific and technical information : third international conference on grey literature; 1997 November 13-14; Luxembourg. Amsterdam. Grey Literature Network Service; 1998. Mar, p. 294. [Google Scholar]
- 9.Fontanella A. Endoscopic microsurgery in herniated cervical discs. Neurol Res. 1999;21:31–38. doi: 10.1080/01616412.1999.11740888. [DOI] [PubMed] [Google Scholar]
- 10.Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong) 2011;19:30–34. doi: 10.1177/230949901101900107. [DOI] [PubMed] [Google Scholar]
- 11.Gibson JNA, Subramanian AS, Scott CEH. A randomised controlled trial of transforaminal endoscopic discectomy vs microdiscectomy. Eur Spine J. 2017;26:847–856. doi: 10.1007/s00586-016-4885-6. [DOI] [PubMed] [Google Scholar]
- 12.Hou KD, Liu ZS, Zhu SR. A long-term follow-up study of the remote result of lumbar discectomy versus conservative treatment for single-level lumbar disc herniation. Med J Chin PLA. 2012;37:727–730. [Google Scholar]
- 13.Hsu HT, Chang SJ, Yang SS, Chai CL. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J. 2013;22:727–733. doi: 10.1007/s00586-012-2540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kafadar A, Kahraman S, Akbörü M. Percutaneous endoscopic transforaminal lumbar discectomy: a critical appraisal. Minim Invasive Neurosurg. 2006;49:74–79. doi: 10.1055/s-2006-932184. [DOI] [PubMed] [Google Scholar]
- 15.Kim CH, Chung CK, Park CS, Choi B, Kim MJ, Park BJ. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nationwide cohort study. Spine (Phila Pa 1976) 2013;38:581–590. doi: 10.1097/BRS.0b013e318274f9a7. [DOI] [PubMed] [Google Scholar]
- 16.Kim MJ, Lee SH, Jung ES, Son BG, Choi ES, Shin JH, et al. Targeted percutaneous transforaminal endoscopic diskectomy in 295 patients: comparison with results of microscopic diskectomy. Surg Neurol. 2007;68:623–631. doi: 10.1016/j.surneu.2006.12.051. [DOI] [PubMed] [Google Scholar]
- 17.Li H, Jiang C, Mu X, Lan W, Zhou Y, Li C. Comparison of MED and PELD in the treatment of adolescent lumbar disc herniation: a 5-year retrospective follow-up. World Neurosurg. 2018;112:e255–e260. doi: 10.1016/j.wneu.2018.01.030. [DOI] [PubMed] [Google Scholar]
- 18.Liu C, Chu L, Yong HC, Chen L, Deng ZL. Percutaneous endoscopic lumbar discectomy for highly migrated lumbar disc herniation. Pain Physician. 2017;20:E75–E84. [PubMed] [Google Scholar]
- 19.Liu HN, Lin X, Yan JZ, Wang L, Cui W, Zeng Z. A comparison of preliminary surgical resu lts between percutaneous transforaminal endoscopic discectomy and microsurgical lumbar disc ectomy for lumbar disc herniation. Chin J Bone Joint. 2013;2:30–35. [Google Scholar]
- 20.Liu X, Yuan S, Tian Y, Wang L, Gong L, Zheng Y, et al. Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: minimum 2-year follow-up results. J Neurosurg Spine. 2018;28:317–325. doi: 10.3171/2017.6.SPINE172. [DOI] [PubMed] [Google Scholar]
- 21.Mayer HM, Brock M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–225. doi: 10.3171/jns.1993.78.2.0216. [DOI] [PubMed] [Google Scholar]
- 22.Miller RG. The jackknife-a review. Biometrika. 1974;61:1–15. [Google Scholar]
- 23.Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. New Eng J Med. 1934;211:210–215. [Google Scholar]
- 24.Perez-Cruet MJ, Foley KT, Isaacs RE, Rice-Wyllie L, Wellington R, Smith MM, et al. Microendoscopic lumbar discectomy: technical note. Neurosurgery. 2002;51(5 Suppl):S129–S136. [PubMed] [Google Scholar]
- 25.Qu JX, Li QZ, Chen M. Comparative study of PTED and MED for monosegment lumbar disc herniation. Chin J Bone Joint Inj. 2017;32:70–71. [Google Scholar]
- 26.Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123:A12–A13. [PubMed] [Google Scholar]
- 27.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931–939. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 28.Schoeggl A, Maier H, Saringer W, Reddy M, Matula C. Outcome after chronic sciatica as the only reason for lumbar microdiscectomy. J Spinal Disord Tech. 2002;15:415–419. doi: 10.1097/00024720-200210000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res. 2014;472:1711–1717. doi: 10.1007/s11999-014-3495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sinkemani A, Hong X, Gao ZX, Zhuang SY, Jiang ZL, Zhang SD, et al. Outcomes of microendoscopic discectomy and percutaneous transforaminal endoscopic discectomy for the treatment of lumbar disc herniation: a comparative retrospective study. Asian Spine J. 2015;9:833–840. doi: 10.4184/asj.2015.9.6.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 32.van Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review Group Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976) 2003;28:1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 33.Wang H, Cheng J, Xiao H, Li C, Zhou Y. Adolescent lumbar disc herniation: experience from a large minimally invasive treatment centre for lumbar degenerative disease in Chongqing, China. Clin Neurol Neurosurg. 2013;115:1415–1419. doi: 10.1016/j.clineuro.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 34.Wei B. Analysis on the risk factors of recurrence of lumbar disk herniation in patients after intervertebral foramen surgery. J Pediatr Orthop. 2019;25:101-104, 116. [Google Scholar]
- 35.Williams RW. Microlumbar discectomy: a conservative surgical approach to the virgin herniated lumbar disc. Spine (Phila Pa 1976) 1978;3:175–182. [PubMed] [Google Scholar]
- 36.Yang L, Liao XQ, Zhao XJ, Zeng ZC, Wu RH, Guan HY, et al. Comparision of surgical outcomes between percutaneous transforaminal endoscopic discectomy and micro-endoscopic discectomy for lumbar disc herniation. China J Endosc. 2015;21:962–965. [Google Scholar]
- 37.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722–731. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 38.Zhao W, Li CQ, Zhou Y, Wang J, Zheng WJ. Surgical treatment of the lumbar disc herniated discs using transforaminal endoscopic surgery system. Orthop J China. 2012;20:1191–1195. [Google Scholar]