Abstract
Globally, about one in four people develop a psychiatric disorder during their lifetime. Specifically, the lifetime prevalence of schizophrenia is about 0.48%, and schizophrenia can have detrimental effects on a patient’s life. Therefore, estimating the economic burden of schizophrenia is important. We investigated the cost-of-illness trend of schizophrenia in South Korea from 2006 to 2016. The cost-of-illness trend was estimated from a societal perspective using a prevalence-based approach for direct costs and a human capital approach for indirect costs. We utilized information from the following sources: 1) National Health Insurance Service, 2) Korean Statistical Information Service, Statistics Korea, 3) the National Survey of Persons with Disabilities, 4) Budget and Fund Operation Plan, Ministry of Justice, 5) Budget and Fund Operation Plan, Ministry of Health and Welfare, and 6) annual reports from the National Mental Health Welfare Commission. Direct healthcare costs, direct non-healthcare costs, and indirect costs by sex and age group were calculated along with sensitivity analyses of the estimates. The cost-of-illness of schizophrenia in Korea steadily increased from 2006 to 2016, with most costs being indirect costs. Individuals in their 40s and 50s accounted for most of the direct and indirect costs. Among indirect costs, the costs due to unemployment were most prevalent. Our estimation implies that schizophrenia is associated with a vast cost-of-illness in Korea. Policymakers, researchers, and physicians need to put effort into shortening the duration of untreated psychosis, guide patients to receive community-care-based services rather than hospital-based services and empower lay people to learn about schizophrenia.
Introduction
Many individuals have mental disorders globally, and one in four people will develop a mental disorder during their lifetime [1]. Specifically, the lifetime and 12-month prevalence rate of having any psychiatric disorder in South Korea (Korea from hereon) is 25.4% and 11.9%, respectively [2]. Moreover, the global burden of mental disorders comprises about 30% of years lived with disability and 15% of disability-adjusted life years [3]. These numbers indicate that improving mental health is a major aspect of increasing one’s wellbeing.
Schizophrenia is a psychiatric disorder that includes symptoms such as delusions, hallucinations, and disorganized speech and behavior [4]. According to a systematic literature review [5], the median 12-month and lifetime prevalence rate of schizophrenia is 0.33% (interquartile range = 0.26%–0.51%) and 0.48% (interquartile range = 0.34–0.85%), respectively. Despite the low prevalence rate, schizophrenia has detrimental effects on patients’ lives, and it places tremendous health, social, and economic burdens on patients, families, caregivers, and society [6]. For instance, patients with schizophrenia have low quality of life [7], impeded employment [8], can be involved in violence [9], have a high risk of acquiring physical diseases (e.g., cardiovascular disease) [10], and have a reduced life expectancy [11]. Consequently, it is no surprise that schizophrenia is in the top 15 (of 328) of diseases and injuries included in the “leading cause of years lived with disability” [12].
Notably, the Korean government has increased the national health expenditures allocated to mental health [13]. Despite the increase, only 2.6% of the total expenditures was allocated to mental health in 2014 [14]. Moreover, the amount is only about 2% of what the U.S. allocates to mental health [15]. Accordingly, it is important to determine what area requires more funding.
Korea provides universal healthcare through National Health Insurance (NHI) and Medical Aid programs. The NHI covers about 97% of the population and the rest is covered by Medical Aid [16]. Consequently, it is possible to construct a health insurance database that contains key data such as health records, prescriptions, etc. Moreover, the NHI Service (NHIS) provide these data to researchers for research purposes.
Investigating the cost-of-illness (COI) of schizophrenia is needed to establish proper and effective healthcare policy and intervention [17]. However, scant studies have investigated the economic burden of schizophrenia in Korea. A previous study [18] regarding the economic burden of schizophrenia (estimated from a societal perspective) in Korea is dated, and other studies [19,20] utilized disability-adjusted life years when estimating the economic cost. Moreover, no study has investigated the economic burden trend regarding schizophrenia in Korea. Therefore, from a societal perspective, we examined the COI trend of schizophrenia in Korea from 2006 to 2016.
Materials and methods
Study design
COI studies estimate the direct and indirect costs intertwined with a specific disease [16]. Direct costs are disease-related payments, which are divided into two parts: direct healthcare costs and direct non-healthcare costs. Indirect costs account for resources that are lost owing to the disease. Therefore, we calculated the cost for three main categories: direct healthcare costs, direct non-healthcare costs, and indirect costs related to those being treated for schizophrenia in Korea. When converting Korean Won to U.S. dollars, we used the average exchange rate of each year. The prevalence approach was utilized for direct costs, and the human capital approach was used for indirect costs.
The requirement for written, informed consent was waived. This study was approved by the institutional review board of the National Center for Mental Health, Korea (no. 116271-2017-10).
We utilized the following sources: 1) claims data and a medical expense survey from the NHIS [21]; 2) Korean Statistical Information Service, Statistics Korea [22]; 3) the National Survey of Persons with Disabilities [23,24]; 4) Budget and Fund Operation Plan, Ministry of Justice [25]; 5) Budget and Fund Operation Plan, Ministry of Health and Welfare [26]; and 6) annual reports of the National Mental Health Welfare Commission [27].
Direct healthcare costs
Direct healthcare costs are defined as medical care costs, which include inpatient care costs, outpatient treatment costs, pharmacy costs, and non-covered care costs. The information regarding inpatient treatment costs, outpatient treatment costs, and pharmacy costs were obtained from the NHIS claims data from 2006 to 2016 [21]. However, the non-covered medical expenses were not retrievable from NHIS; therefore, these were estimated by the proportion of the non-covered care costs (i.e., 4.3% for inpatient and 2.3% for outpatient care) regarding mental health from the 2009 medical expense survey [28].
Direct non-healthcare costs
Direct non-healthcare costs are defined as costs that are associated with patient management, other than direct healthcare costs. We included the following direct non-healthcare costs in this study: incarceration costs, community mental healthcare center costs, sanatoria costs, rehabilitation facility costs, and transport costs [2]. Patients with schizophrenia are involved in crime (mediated by substance use comorbidity) (mediated by substance use comorbidity) more so than is the general population [9]. Accordingly, there are various costs that are related to this issue such as policing and prosecution costs. However, those specific data were not available. Instead, we focused on costs that are retrievable—incarceration cost. Incarceration cost was calculated based on the Budget and Fund Operation Plan, Ministry of Justice [25]. Patients do not receive a diagnosis or prescription at a community mental health center; rather, patients visit community mental healthcare centers for rehabilitation purposes. In addition, most community mental healthcare costs are covered by the government, not by the individual. Therefore, community mental healthcare center costs were considered as direct non-healthcare costs.
Community mental healthcare center costs were estimated using information included in the budget of the local mental health centers [27]. The cost for sanatoria was based on the Budget and Fund Operation Plan, Ministry of Health and Welfare [26]. Psychiatric rehabilitation is vital for treatment as it assists patients with reaching their optimal level of functioning [29]. Therefore, the costs for rehabilitation facilities were also estimated through the Budget and Fund Operation Plan, Ministry of Health and Welfare [26]. The community mental healthcare center costs, sanatoria costs, and psychiatric rehabilitation costs were estimated by the annual operating costs from each report (e.g., annual operating cost of community mental healthcare center by local mental health centers in 2007 * treated prevalence rate of schizophrenia in 2007). We estimated the transport cost by multiplying the total number of hospital visits by the mean return fare [18].
Indirect costs
Indirect costs included productivity loss due to unemployment, workplace productivity loss due to morbidity, premature death costs, and caregiving costs. Information regarding indirect costs was retrieved from Statistics Korea [22], the NHIS [21], and the National Survey of Persons with Disabilities [23,24]. There has been a shift with caregiving responsibility of those with mental disorders—from hospital-based to family- or caregiver-based [30]. Therefore, it is important to estimate the caregiving costs associated with schizophrenia. The information regarding caregiving costs was estimated by information provided by Statistics Korea [22], the National Survey of Persons with Disabilities [23,24], and the NHIS [21]. For the exact equations for indirect costs, see S1 Table.
Sensitivity analyses
Some costs were not attributable directly (e.g., non-covered medical expenses). Therefore, we conducted a sensitivity analysis to evaluate the robustness of the estimated costs utilizing the lowest (11%) and highest (20%) proportion of non-covered medical expenses reported by NHIS [31]. In addition, the discount rates (0% and 5%) of expected future earnings and the productivity costs due to premature mortality (using the friction-cost method for 1 month, 3 months, and 6 months) were calculated. A more-detailed description of the method regarding sensitivity analyses can be found elsewhere [18]. All statistical analyses were performed with SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Treated prevalence of schizophrenia in Korea from 2006 to 2016
The numbers of patients who were treated for schizophrenia, those registered as having a mental disability, and those who died from schizophrenia (i.e., cause of death was schizophrenia) or committed suicide each year from 2006 to 2016 are presented in Table 1. The treated prevalence rate has increased from 0.33% to 0.40% during this period. In total, 448,490 patients (when duplicates were removed) were treated for schizophrenia from 2006 to 2016 in Korea. Additionally, 109,306 individuals (when duplicates were removed) were classified as having mental disability among those treated for schizophrenia during that period. Moreover, about 1,000 people each year died from schizophrenia or committed suicide.
Table 1. Individuals treated for schizophrenia, registered as having a mental disability, or who died from schizophrenia/committed suicide from 2006 to 2016 in Korea.
| Treated for schizophrenia | Determined to have a mental disability | Died from schizophrenia or suicide | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 2006 | 160,157 | 0.33 | 32,300 | 0.20 | 631 | 0.00 |
| 2007 | 165,544 | 0.34 | 48,536 | 0.29 | 926 | 0.01 |
| 2008 | 171,663 | 0.35 | 58,168 | 0.34 | 1,008 | 0.01 |
| 2009 | 175,230 | 0.35 | 64,824 | 0.37 | 1,054 | 0.01 |
| 2010 | 174,492 | 0.35 | 69,468 | 0.40 | 1,066 | 0.01 |
| 2011 | 179,254 | 0.36 | 73,664 | 0.41 | 1,122 | 0.01 |
| 2012 | 187,390 | 0.37 | 76,548 | 0.41 | 1,091 | 0.01 |
| 2013 | 189,961 | 0.38 | 78,260 | 0.41 | 1,093 | 0.01 |
| 2014 | 191,502 | 0.38 | 79,694 | 0.42 | 1,063 | 0.01 |
| 2015 | 199,743 | 0.39 | 82,058 | 0.41 | 1,138 | 0.01 |
| 2016 | 202,345 | 0.40 | 82,976 | 0.41 | 1,110 | 0.01 |
COI of schizophrenia each year by each category
The total COI of schizophrenia and specific costs for each category—direct healthcare costs, direct non-healthcare costs, and indirect costs—are presented in Table 2. The total direct healthcare cost was about 451 billion Won in 2006 and rose to approximately 868 billion Won in 2016. The direct non-healthcare cost rose from about 135 billion Won in 2006 to 244 billion Won in 2016. The total indirect cost was 3.09 trillion Won in 2006 and increased to 5.79 trillion Won in 2016. Moreover, the direct healthcare cost, direct non-healthcare cost, and indirect cost accounted for about 12–14%, 3–4%, and 83–85% of the total COI of schizophrenia during this period, respectively.
Table 2. Overall cost of schizophrenia in Korea from 2006 to 2016.
| Cost type | 2006 | % | 2007 | % | 2008 | % | 2009 | % | 2010 | % | 2011 | % | 2012 | % | 2013 | % | 2014 | % | 2015 | % | 2016 | % | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Direct cost | Direct healthcare | Inpatient care costs | 325,324 | 75% | 361,527 | 75% | 399,306 | 76% | 486,348 | 78% | 528,291 | 78% | 567,542 | 79% | 598,032 | 80% | 619,228 | 80% | 633,385 | 81% | 660,052 | 81% | 674,963 | 81% |
| uncovered inpatient care cost | 13,289 | 14,646 | 15,926 | 20,033 | 21,977 | 23,617 | 24,829 | 25,743 | 26,334 | 27,375 | 27,950 | |||||||||||||
| Outpatient care costs | 93,095 | 21% | 101,722 | 21% | 109,056 | 20% | 118,553 | 19% | 125,385 | 18% | 128,384 | 18% | 126,982 | 17% | 132,692 | 17% | 134,319 | 17% | 136,327 | 16% | 140,672 | 17% | ||
| uncovered outpatient care cost | 1,825 | 1,994 | 2,148 | 2,425 | 2,605 | 2,674 | 2,629 | 2,741 | 2,779 | 2,805 | 2,887 | |||||||||||||
| Pharmacy costs | 17,583 | 4% | 19,807 | 4% | 21,677 | 4% | 23,075 | 4% | 23,831 | 3% | 23,895 | 3% | 23,845 | 3% | 23,535 | 3% | 21,955 | 3% | 22,078 | 3% | 22,221 | 3% | ||
| Total | 451,116 | 12% | 499,695 | 12% | 548,114 | 12% | 650,434 | 13% | 702,089 | 14% | 746,111 | 14% | 776,316 | 13% | 803,939 | 13% | 818,772 | 13% | 848,637 | 13% | 868,693 | 13% | ||
| Direct non-healthcare | Incarceration | 1,223 | 1% | 1,261 | 1% | 1,540 | 1% | 1,545 | 1% | 1,901 | 1% | 1,813 | 1% | 2,023 | 1% | 2,530 | 1% | 2,673 | 1% | 3,471 | 1% | 3,969 | 2% | |
| Community mental healthcare centers | 4,149 | 3% | 3,966 | 3% | 4,347 | 3% | 4,738 | 3% | 4,657 | 3% | 5,033 | 3% | 5,357 | 3% | 6,065 | 3% | 6,537 | 3% | 17,113 | 7% | 16,902 | 7% | ||
| Sanatoria | 81,443 | 60% | 84,847 | 60% | 86,254 | 59% | 89,653 | 59% | 92,319 | 59% | 95,507 | 59% | 129,532 | 63% | 115,482 | 57% | 118,509 | 56% | 122,238 | 52% | 126,006 | 52% | ||
| Rehabilitation facilities | 40,580 | 30% | 41,835 | 30% | 43,129 | 29% | 44,463 | 29% | 45,838 | 29% | 47,256 | 29% | 54,136 | 26% | 61,310 | 30% | 67,380 | 32% | 76,888 | 33% | 80,116 | 33% | ||
| Transport costs | 8,028 | 6% | 9,541 | 7% | 11,153 | 8% | 11,738 | 8% | 12,262 | 8% | 13,281 | 8% | 14,971 | 7% | 15,636 | 8% | 16,061 | 8% | 16,692 | 7% | 17,055 | 7% | ||
| Total | 135,423 | 4% | 141,450 | 3% | 146,424 | 3% | 152,137 | 3% | 156,977 | 3% | 162,891 | 3% | 206,019 | 4% | 201,023 | 3% | 211,160 | 3% | 236,402 | 4% | 244,048 | 4% | ||
| Direct cost total | 586,539 | 16% | 641,145 | 15% | 694,537 | 15% | 802,572 | 17% | 859,066 | 17% | 909,002 | 17% | 982,335 | 17% | 1,004,962 | 16% | 1,029,932 | 16% | 1,085,039 | 16% | 1,112,741 | 16% | ||
| Indirect Cost | Unemployment | 2,100,191 | 68% | 2,276,720 | 63% | 2,491,115 | 62% | 2,493,093 | 62% | 2,569,126 | 62% | 2,912,681 | 64% | 3,104,954 | 64% | 3,288,018 | 64% | 3,516,994 | 65% | 3,658,302 | 65% | 3,773,508 | 65% | |
| Reduced productivity at work | 455,272 | 15% | 491,123 | 14% | 537,121 | 13% | 546,017 | 14% | 558,917 | 13% | 524,470 | 11% | 559,134 | 12% | 623,497 | 12% | 622,725 | 12% | 650,899 | 12% | 674,513 | 12% | ||
| Premature mortality | 335,560 | 11% | 510,854 | 14% | 582,374 | 15% | 593,426 | 15% | 585,936 | 14% | 634,954 | 14% | 621,983 | 13% | 659,451 | 13% | 637,711 | 12% | 684,832 | 12% | 682,256 | 12% | ||
| Caregiver productivity loss | 202,672 | 7% | 315,775 | 9% | 396,035 | 10% | 410,914 | 10% | 446,588 | 11% | 505,304 | 11% | 546,587 | 11% | 583,560 | 11% | 614,523 | 11% | 637,921 | 11% | 663,570 | 11% | ||
| Indirect cost total | 3,093,695 | 84% | 3,594,472 | 85% | 4,006,646 | 85% | 4,043,449 | 83% | 4,160,567 | 83% | 4,577,408 | 83% | 4,832,658 | 83% | 5,154,527 | 84% | 5,391,954 | 84% | 5,631,954 | 84% | 5,793,848 | 84% | ||
| Total cost | 3,680,234 | 4,235,617 | 4,701,183 | 4,846,021 | 5,019,633 | 5,486,410 | 5,814,993 | 6,159,489 | 6,421,886 | 6,716,993 | 6,906,589 | |||||||||||||
Total direct and indirect cost of schizophrenia per sex and age group
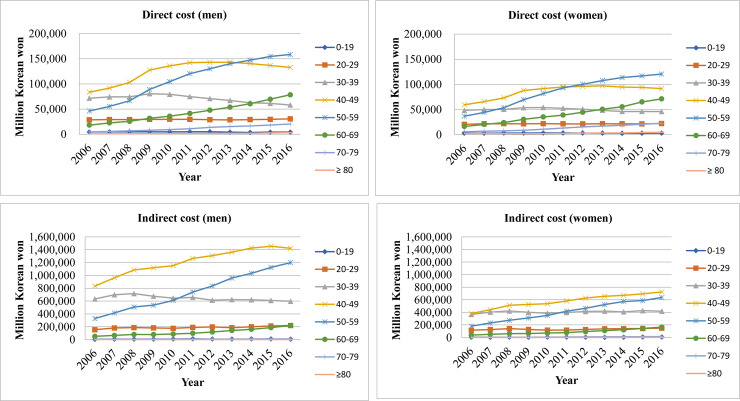
Fig 1 displays the direct and indirect cost trend of different age groups per sex. The direct healthcare costs of those in their 40s and 50s (both men and women) showed the highest proportion among different age groups. Especially, the direct cost attributable to those in their 50s was the highest among the different age groups since 2014 for men and since 2012 for women. Moreover, individuals who were younger than 20 years and those in their 20s had a much lower proportion of cost compared to those in their 30s, 40s, and 50s.
Fig 1. Direct and indirect cost of men and women by different age groups.
The indirect cost for all age groups showed a similar pattern for men and women. However, costs attributable to men were higher than among women—especially those in their 40s and 50s. The highest indirect cost was attributable to those in their 40s for both men and women.
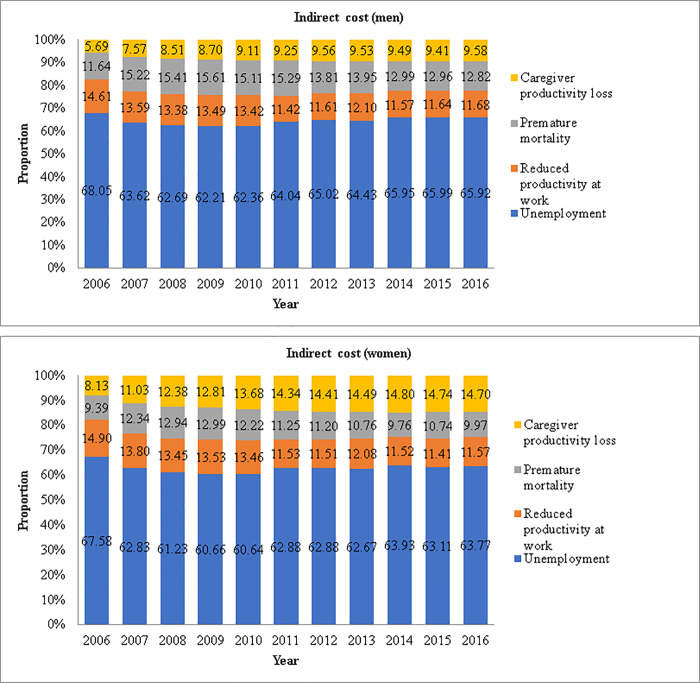
Trend of indirect cost of men and women for each category
Fig 2 shows the trend of indirect cost for men and women per the three cost categories. For both men and women, most of the cost was due to unemployment (about 65% each year). Men showed much higher economic cost due to unemployment than did women. For example, cost due to unemployment for men in 2016 was about 2.42 trillion Won; however, for women, it was 1.35 trillion Won.
Fig 2. Indirect cost of men and women by specific costs.
COI trend of schizophrenia in Korea from 2006 to 2016
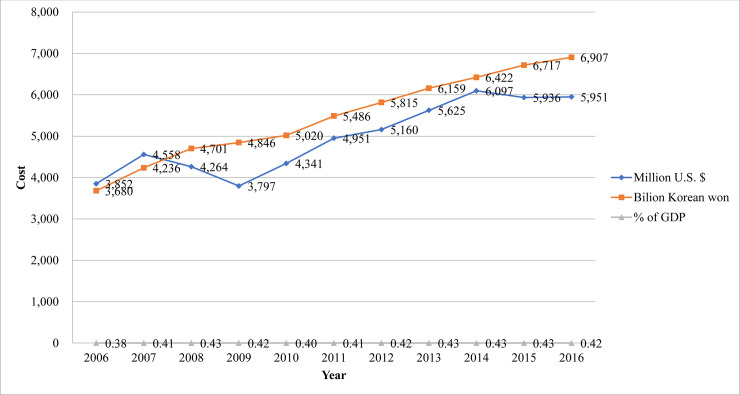
The COI of treated schizophrenia in South Korea from 2006 to 2016 is presented in Fig 3. The COI of schizophrenia in Korea was 3.68 trillion Won in 2006 and 6.90 trillion Won in 2016, showing a steady increase. Compared to 2006, the treated prevalence and the socioeconomic cost of schizophrenia increased by 1.26-fold and 1.88-fold, respectively (whereas Korea’s gross domestic product has increased by 1.70-fold) [32]. The COI of schizophrenia in 2016 was 0.42% of Korea’s total gross domestic product.
Fig 3. Economic burden of schizophrenia in Korea from 2006–2016.
Sensitivity analysis
The base case COI estimates and the sensitivity analysis results from 2006 to 2016 are shown in Table 3. The COI in 2016 was 6.97 and 7.06 trillion Won when non-covered payments were estimated to be 11% and 20%, respectively. When 0% and 5% discount rates were utilized, the COI of schizophrenia increased to 7.27 trillion Won and decreased to 6.77 trillion Won, respectively.
Table 3. Sensitivity analysis on key burden of illness assumptions.
| Assumption | Cost | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | ||
| Base case | 3,680,233,795,244 | 4,235,617,109,128 | 4,701,182,922,976 | 4,846,020,781,817 | 5,019,633,100,110 | 5,486,410,086,705 | 5,814,992,976,769 | 6,159,488,759,051 | 6,421,885,598,523 | 6,716,992,852,444 | 6,906,588,614,709 | |
| Self-payment cost due to exclusion | 11% | 3,711,257,139,215 | 4,269,731,656,007 | 4,738,196,072,152 | 4,891,400,747,236 | 5,069,180,707,246 | 5,539,122,026,917 | 5,869,633,553,680 | 6,216,208,548,882 | 6,479,799,073,198 | 6,776,839,043,580 | 6,967,790,505,589 |
| 20% | 3,758,443,405,139 | 4,321,639,376,898 | 4,794,535,810,751 | 4,960,780,852,854 | 5,144,995,017,811 | 5,619,920,613,540 | 5,953,597,774,746 | 6,303,349,096,437 | 6,568,803,055,861 | 6,868,910,792,248 | 7,061,921,021,206 | |
| Discount rate | 0% | 3,874,440,653,050 | 4,536,378,779,999 | 5,036,764,090,884 | 5,184,696,012,249 | 5,348,497,726,623 | 5,841,530,537,553 | 6,156,700,946,741 | 6,518,794,425,616 | 6,763,938,237,563 | 7,097,991,969,143 | 7,265,716,631,374 |
| 5% | 3,608,316,562,974 | 4,124,713,574,902 | 4,576,781,509,309 | 4,719,882,859,041 | 4,896,913,092,329 | 5,353,699,002,535 | 5,686,672,763,369 | 6,024,025,376,641 | 6,292,603,171,235 | 6,574,780,651,454 | 6,770,256,188,743 | |
| Friction period for worker replacement | 1 mo. | 3,346,061,583,850 | 3,726,839,993,401 | 4,121,236,220,694 | 4,255,075,036,749 | 4,436,206,798,623 | 4,854,178,186,053 | 5,195,726,556,241 | 5,502,927,031,116 | 5,787,023,551,063 | 6,035,133,811,143 | 6,227,442,843,374 |
| 3 mo. | 3,348,836,444,680 | 3,730,993,735,545 | 4,126,091,147,815 | 4,260,034,765,749 | 4,441,227,022,623 | 4,859,621,923,053 | 5,201,159,455,241 | 5,508,706,562,116 | 5,792,721,578,063 | 6,041,078,895,143 | 6,233,663,267,374 | |
| 6 mo. | 3,352,998,735,925 | 3,737,224,348,761 | 4,133,373,538,496 | 4,267,474,359,249 | 4,448,757,358,623 | 4,867,787,528,553 | 5,209,308,803,741 | 5,517,375,858,616 | 5,801,268,618,563 | 6,049,996,521,143 | 6,242,993,903,374 | |
mo. = month
Discussion
From a societal perspective, we estimated the COI trend of schizophrenia in Korea from 2006 to 2016. The overall economic burden of schizophrenia has increased steadily from 2006, and the cost trend is similar to that of a previous study that utilized data from 2005 [18].
The increased treatment prevalence could be attributable to Korea’s efforts to alleviate stigma against schizophrenia, which led some patients to actively seek help for their symptoms. The term for schizophrenia in Korean was originally “jungshinbunyeolbyung,” which translates to “mind-split disorder.” To reduce stigma, in 2012, the Korean Neuropsychiatric Association changed the term to “johyeonbyung,” which translates to “attunement disorder.” According to a Korean study [33], changing the term had a significant effect on reducing stigma toward schizophrenia.
Despite the increased treatment prevalence, there is much room for improvement. Among the general population, about 10% received help by a mental health professional (e.g., psychiatrists, other medical doctors, other mental health professionals, nurses, etc.) for mental health problems in Korea [2]. Moreover, only about 20% among those diagnosed with a mental disorder received help from a mental health professional [2], which is much lower than the rate observed in New Zealand (38.9%), the U.S. (43.1%), Spain (35.5%), Belgium (39.5%), and Australia (34.9%) [34–36]. Moreover, a previous study [37] emphasized the need for education on etiology and treatment regarding schizophrenia in Korea to guide patients to use mental health services. Further, sex and personality traits should be considered when providing education to promote help-seeking behavior [38]. Researchers and practitioners thus need to work to raise public awareness concerning schizophrenia to promote patients’ help-seeking behavior.
Based on our estimation, inpatient care comprised most of the direct healthcare costs. The inpatient care cost was 75% of the direct healthcare cost in 2006, and this increased to 81% in 2016. The number of admissions into mental hospitals decreased in developed countries [39]; however, Korea shows an opposite trend. The numbers of psychiatric beds have continuously increased and the length of stay at a psychiatric hospital remains long (i.e., 116 days)—in fact, the longest among Organization for Economic Cooperation and Development countries [40]. This could be explained by the payment system in Korea. About 97% of the total population in Korea is supported by the NHIS, and the remaining 3% are supported by Medical Aid. The zero co-payment for those who receive Medical Aid may provoke those to stay longer at a psychiatric hospital. In fact, only 3% of the total population receives Medical Aid; however, about 50% and 60% of the psychiatric admissions and total long-term admissions, respectively, are by those who receive Medical Aid [41]. The government needs to guide these patients to receive treatment from a community-based facility rather than obtaining hospital-based treatment.
Further, the Mental Health Act could account for the high inpatient care costs. Korea has a very high rate (i.e., 80%) of involuntary admissions, which is regulated by the Mental Health Act. This high rate of involuntary admissions is higher than other countries [42]. According to Article XXIV of the Mental Health Act, an institution can involuntarily hospitalize a patient when a psychiatrist judges that he or she needs hospitalization [43]. However, a stricter regulation regarding involuntary admissions and a shorter period before being able to be discharged have been applied owing to the revised Mental Health Act in 2016 [44]. Based on this revision, it is expected that inpatient costs will decrease, and outpatient costs and non-healthcare costs will increase.
Of the different age groups, those in their 40s and 50s accounted for most of the direct costs. Those in their 20s and younger had much lower direct healthcare costs comparatively. The onset of schizophrenia typically occurs in late adolescence [45]. However, our data showed that adolescents and those in their 20s are not actively being treated for schizophrenia. In fact, Korea has a higher duration of untreated psychosis (DUP; i.e., 840 days) compared to Western countries [46]. This indicates that patients are not being treated during the most critical period. Since there is an association between longer DUP and worse outcomes among patients with a psychosis [47], researchers and policymakers need to provide ways to promote patients to seek help when they notice their first psychotic symptom. Especially, an integrated community program is needed to improve outcomes and to raise intervention efficiency [48].
Most direct non-healthcare costs were for sanatoria and rehabilitation facility costs, which accounts for about 90% when combined. This shows that most of the burden from schizophrenia concerns long-term care, which is consistent with previous studies [18,49]. It seems that Korean patients miss the chance for early intervention owing to a high DUP [46], which leads to a poor prognosis [47] and patients requiring inpatient care. Incarceration accounts for about 1% of the direct non-healthcare costs. However, considering the severity of the matter, efforts to prevent violence that is associated with schizophrenia are needed. A meta-analysis [9] that investigated the association between schizophrenia and violence stated that substance abuse comorbidity mediates the association between schizophrenia and violence. Therefore, experts need to consider preventing substance abuse among patients with schizophrenia.
The cost due to unemployment was the highest among all indirect costs, regardless of sex. However, the cost was much higher for men, which may be attributable to the income difference between men and women in Korea [22]. Moreover, cost due to premature mortality was the second highest for men. This is consistent with previous research showing that men have a higher suicide completion rate than do women [50]. Therefore, suicide prevention interventions are required for men with schizophrenia. For women, the second highest cost among indirect costs was due to caregiver productivity loss since 2010.
Overall, the COI of schizophrenia in Korea has been steadily increasing since 2006. The Korean government has made strides concerning citizens’ mental health. The most prominent change is the revised Mental Health Act in 2016 [44]. Through this revision, the unnecessarily long and involuntary admissions of psychiatric patients are expected to decrease. Moreover, the government, researchers, and policymakers need to focus on guiding patients to receive treatment, especially at a community-based facility. Future study is needed to determine how the COI in Korea changes owing to the revision of the Mental Health Act and other efforts the Korean government has implemented.
Despite its importance, this study had some limitations. First, we utilized the treated prevalence rate. Therefore, we did not acquire information about those who have schizophrenia but are not being treated. However, rather than using self-report data, we utilized actual claim data from the NHIS. Second, the costs, especially the indirect costs, are estimated values; the indirect costs could be underestimated or overestimated. For example, the budget for the central government was considered when estimating costs for community centers and specific proportions of budget allocated in each local government to community center were not regarded. Despite these limitations, we tried to use exact numbers when the information was retrievable. For instance, the numbers concerning those with a mental disability, suicide, and mortality were exact numbers rather than estimates.
Conclusions
The current study estimated the COI trend of schizophrenia in South Korea from 2006 to 2016. This study was based on a societal perspective and we employed a prevalence-based approach for direct costs and a human capital approach for indirect costs. We also utilized information from various sources. The results indicated that more patients with schizophrenia are seeking help; however, there is still room for improvement. Most costs were attributed from indirect costs, and those in their 40s and 50s accounted for most of the COI of schizophrenia in Korea. Our results also imply that community-based care, instead of hospital care, is needed in Korea. Future studies need to examine how the Mental Health Act in 2016 has changed the COI of schizophrenia in Korea.
Supporting information
(DOCX)
Data Availability
There are ethical and legal restrictions (i.e., data contains potentially sensitive information and personally identifiable information) since the data contains sensitive patient information. However, the data is available from NHIS (National Health Insurance System) upon request to the ‘Information analysis department in Big data operation room’. Researchers who may wish to get access to the data could contact the Bid data operation room (+82-33-736-2432). Also, the url for the website is: https://nhiss.nhis.or.kr/bd/ab/bdaba000eng.do;jsessionid=cK18Qv01aQU6z3lIVw344vo AFGSXalRxAdKkU8XvPL1E2XK9y0CdK1BRwzPwbhzQ.primrose2_servlet_engine1 Future researchers who wish to get access to the data we have utilized could request the 2006-2016 claims data of those with schizophrenia (F20, ICD-10 code).
Funding Statement
This study was supported by an intramural grant(No 2019-06) from the National Center for Mental Health, Republic of Korea.
References
- 1.Ginn S, Horder J. “One in four” with mental health problem: the anatomy of a statistic. BMJ. 2012;344(e1302): 1–2. [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Health and Welfare. The survey of mental disorders in Korea; 2016.
- 3.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness Lancet Psychiatry. 2016;3: 171–178. 10.1016/S2215-0366(15)00505-2 [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual disorders 5th ed Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 5.Simeone JC, Ward AJ, Rotella P, Collins J, Windisch R. An evaluation of variation in published estimates of schizophrenia prevalence from 1990–2013: a systematic literature review. BMC Psychiatry. 2015;15(193): 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou C, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatric Dis Treat. 2016;12: 357–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bobes J, Garcia-Portilla MP, Bascaran MT, Saiz PA, Bousono M. Quality of life in schizophrenia patients. Dialogues Clin Neurosci. 2007;9(2): 215–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, Perkins D, et al. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163: 411–417. 10.1176/appi.ajp.163.3.411 [DOI] [PubMed] [Google Scholar]
- 9.Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. 2009;6(8): e1000120 10.1371/journal.pmed.1000120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cunningham R, Poppe K, Peterson D, Every-Palmer S, Soosay I, Jackson R. Prediction of cardiovascular disease risk among people with severe mental illness: a cohort study. PLoS One. 2009;-14(9): e0221521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Ann Rev Clin Psychol. 2014;10: 425–448. [DOI] [PubMed] [Google Scholar]
- 12.Vos T, Abajobir AA, Abbafati C, Abbas KM, Abate KH, Abd-Allah F, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100): 1211–1259. 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roh S, Lee S-U, Soh M, Ryu V, Kim H, Jang JW, et al. Mental health services and R&D in South Korea. Int J Ment Health Syst. 2016;10: 45 10.1186/s13033-016-0077-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ministry of Health and Welfare. An overview of MOHW budget and fund operation plan 2010–2014. Ministry of Health and Welfare; 2010. –2014. [Google Scholar]
- 15.Hong SC. Recent status of national expenditure for mental health improvement in Korea. J Budget Pol. 2012;1(1): 67–102. [Google Scholar]
- 16.National Health Insurance System. National Health Insurance System of Korea; 2015.
- 17.Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20(4): 327–337. 10.3350/cmh.2014.20.4.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang SM, Cho S-J, Jeon HJ, Hahm B-J, Lee HJ, Park J-I, et al. Economic burden of schizophrenia in South Korea. J Korean Med Sci. 2008;23(2): 167–175. 10.3346/jkms.2008.23.2.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim D, Lee WK, Park H. Disability-adjusted life years (DALYs) for mental and substance use disorders in the Korean Burden of Disease Study 2012. J Korean Med Sci. 2016;31: 191–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park J-H, Yoon S-J, Lee H-Y, Cho H-S, Lee J-Y, Eun S-J, et al. Estimating the burden of psychiatric disorder in Korea. J Prevent Med Public Health 2006;39(1): 39–45. [PubMed] [Google Scholar]
- 21.National Health Insurance System. National Health Insurance Sharing System 2006–2016. Available from: https://nhiss.nhis.or.kr/bd/ab/bdaba013eng.do
- 22.Statistics Korea. Korean Statistical Information System: Korean National Statistical Office; 2006–2016. Available from: http://kostat.go.kr/portal/korea/index.action
- 23.Ministry of Health and Welfare, Korea Institute for Health and Social Affairs. National Survey of Persons with Disabilities. Sejong, Korea; 2014.
- 24.Ministry of Health and Welfare, Korea Institute for Health and Social Affairs. National Survey of Persons with Disabilities. Sejong, Korea; 2011.
- 25.Ministry of Justice. Budget and Fund Operation Plan. Gwacheon-si, Korea: Ministry of Justice 2006–2016.
- 26.Ministry of Health and Welfare. Budget and Fund Operation Plan. Sejong, Korea; 2006–2016.
- 27.The National Mental Health Welfare Commission. The National Mental Health Welfare Commission Annual Report. Seoul, Korea; 2006–2016.
- 28.Choi YS, Baek SJ, Lim ES, Lee HY, Chang HJ. 2009 Medical expense survey of health insurance patients. Seoul: National Health Insurance System; 2009. [Google Scholar]
- 29.Glynn SM. Psychiatric rehabilitation in schizophrenia: advances and challenges. Clini Neurosci Res. 2003;3(1–2): 23–33. [Google Scholar]
- 30.Thompson EH, Doll W. The burden of families coping with the mental ill: An invisible crisis. Fam Relat. 1982;31(3): 379–388. [Google Scholar]
- 31.Jeong HS. Public financing in total health expenditure and coverage by National Health Insurance in Korea: including comparison with other OECD countries. Korean J Health Econ Pol. 2004;10: 95. [Google Scholar]
- 32.Economic Statistics System. Gross Domestic Product of Korea: Bank of Korea; 2019 Available from: http://ecos.bok.or.kr/
- 33.Kim SW, Chang JE, Kim JM, Shin IS, Ban DH, Choi BS, et al. Comparison of stigma according to the term used for schizophrenia: split-mind disorder vs. attunement disorder. J Korean Neuropsychiatr Assoc. 2012;51: 210–217. [Google Scholar]
- 34.Kessler RC, Ustun TB. The WHO World Mental Health Survey: global perspectives on the epidemiology of mental disorders. New York, USA: Cambridge University Press; 2008. [Google Scholar]
- 35.Slade T, Johnston A, Oakley Browne MA, Andrews G, Whiteford HA. 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Australian and New Zealand Journal of Psychiatry. 2009;43: 594–605. 10.1080/00048670902970882 [DOI] [PubMed] [Google Scholar]
- 36.Center for Behavioral Health Statistics and Quality. 2015 national survey on drug use and health: detailed tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 37.Park S, Lee M, Furnham A, Jeon M, Ko Y-M. Lay beliefs about the causes and cures of schizophrenia. Int J Soc Psychiatry. 2017;63(6): 518–524. 10.1177/0020764017717283 [DOI] [PubMed] [Google Scholar]
- 38.Park S, Jeon M, Lee Y, Ko Y-M, Kim CE. Influencing factors of attitudes toward seeking professional help for mental illness among Korean adults. Int J Soc Psychiatry. 2018;64(3): 286–292. 10.1177/0020764018760952 [DOI] [PubMed] [Google Scholar]
- 39.Organization of Economic Co-operation and Development. Psychiatric care beds per 1000 population. Paris: Organization of Economic Co-operation and Development; 2014. [Google Scholar]
- 40.Organization of Economic Co-operation and Development. Korea’s increase in suicides and psychiatric bed numbers is worrying, says OECD. Paris: Organization of Economic Co-operation and Development; 2014. [Google Scholar]
- 41.Park JI, Chang HS, Lee JS, Lee MS. Structural factors for maintaining long-term admission. Human Rights of Mentally Disabled Survey 2008. Seoul: National Human Rights Commission of Korea; 2009. [Google Scholar]
- 42.World Health Organization and Ministry of Health and Welfare. WHO-AIMS Report on Mental Health System in Republic of Korea. Korea: Gwacheon City: World Health Organization; 2007. [Google Scholar]
- 43.Constitutional Court of Korea. Article XXIIII of Mental Health Act; 2011.
- 44.Constitutional Court of Korea. Decision on the constitutionality of paragraph 1 et cetera of Article XXIIII of the Mental Health Act Seoul: Constitutional Court of Korea; 2016 Available from: http://search.ccourt.go.kr/ths/pr/ths_pr0103_P1.do?seq=0&cname=%EA%B3%B5%EB%B3%B4&eventNum=41196&eventNo=2014%ED%97%8C%EA%B0%809&pubFlag=0&cId=010200&page=&qrylist=2014%ED%97%8C%EA%B0%809%7C2014%ED%97%8C%EA%B0%809&selectFont
- 45.Harrop C, Trower P. Why does schizophrenia develop at late adolescence? Clin Psychol Rev. 2001;21(2): 241–266. 10.1016/s0272-7358(99)00047-1 [DOI] [PubMed] [Google Scholar]
- 46.Yoo JM, Ahn SR, Cho YS, Lee MS. A study of duration of untreated psychosis (DUP) for first episode psychosis. Ment Health. 2011;2: 12–16. [Google Scholar]
- 47.Penttilä M, Jääskeläinen E, Hirvonen N, Isohanni M, Miettunen J. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2014;205: 88–94. 10.1192/bjp.bp.113.127753 [DOI] [PubMed] [Google Scholar]
- 48.Lee MS, Ahn SR. The analysis of community-based identification, assessment and allocation system for early psychosis. Korean J Schizophr Res. 2013;16(1): 32–37. [Google Scholar]
- 49.Kim A, M. Why do psychiatric patients in Korea stay longer in hospital? Int J Ment Health Syst. 2017;11(2): 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim M, Jung-Choi K, Jun H, Kawachi I. Socioeconomic inequalities in suicidal ideation, parasuicides, and completed suicides in South Korea. Soc Sci Med. 2010;70(8): 1254–1261. 10.1016/j.socscimed.2010.01.004 [DOI] [PubMed] [Google Scholar]