Abstract
Purpose
Understanding factors associated with reaching the contemplative stage of readiness to initiate osteoporosis treatment may inform the design of behavioral interventions to improve osteoporosis treatment uptake in women at high risk for fracture.
Methods
We measured readiness to initiate osteoporosis treatment using a modified form of the Weinstein Precaution Adoption Process Model (PAPM) among 2,684 women at high risk of fracture from the Activating Patients at Risk for OsteoPOroSis (APROPOS) clinical trial. Pre-contemplative participants were those who self-classified in the unaware and unengaged stages of PAPM (stages 1 and 2). Contemplative participants were those in the undecided, decided not to act, or decided to act stages of PAPM (stages 3, 4 and 5). Using multivariable logistic regression, we evaluated participant characteristics associated with levels of readiness to initiate osteoporosis treatment.
Results
Overall, 24% (N=412) self-classified in the contemplative stage of readiness to initiate osteoporosis treatment. After adjusting for age, race, education, health literacy, and major osteoporotic fracture in the past 12 months, contemplative women were more likely to report previously being told they had osteoporosis or osteopenia [adjusted odds ratio [aOR] (95% CI) 11.8 (7.8-17.9) and 3.8 (2.5-5.6), respectively], acknowledge concern about osteoporosis [aOR 3.5 (2.5-4.9)] and disclose prior osteoporosis treatment [aOR 4.5 (3.3-6.3)] than women who self-classified as pre-contemplative.
Conclusions
For women at high risk for future fractures, ensuring women’s recognition of their diagnosis of osteoporosis/osteopenia and addressing their concerns about osteoporosis are critical components to consider when attempting to influence stage of behavior transitions in osteoporosis treatment.
Keywords: Osteoporosis, Fracture, Behavioral changes, Precaution Adoption Process Model
Summary
We investigated the factors associated with readiness for initiating osteoporosis treatment in women at high risk of fracture. We found that women in the contemplative stage were more likely to report previously being told having osteoporosis or osteopenia, acknowledge concern about osteoporosis and disclose prior osteoporosis treatment.
Introduction
The majority of patients who experience a fragility fracture do not receive adequate treatment [1, 2]. Population-based studies demonstrate a temporal decline in the uptake of osteoporosis treatment, in particular bisphosphonates [3], the most commonly prescribed osteoporosis medications [4]. Osteoporosis treatment initiation is a multi-step, complex process that involves interactions between patients and their health care team and hinges on a patient`s awareness of the need for the medication. Most often patients become aware of the need to initiate osteoporosis medications once they are diagnosed by their provider as having osteoporosis.
Patient-centered strategies may help overcome barriers to osteoporosis treatment [5-9] (e.g., patients` fear of medication adverse events and inadequate knowledge of osteoporosis). Theoretical models of behavior change such as Weinstein’s Precaution Adoption Process Model (PAPM) [10] have been used to understand a patient’s readiness to initiate health behaviors, including medication initiation. Previously, our group showed that a patient-centered video intervention using storytelling improved participants’ readiness for initiating osteoporosis treatment 6 months after a patient-directed behavioral intervention [11]. However, our previous study did not dive further into understanding the factors associated with the readiness for initiating osteoporosis treatment; doing so can inform the design of future interventions to improve osteoporosis treatment uptake.
Thus, the objectives of the present study were to examine the factors associated with readiness for initiating osteoporosis treatment in women at high risk for fracture.
Methods
Study Design and Participants
We conducted a cross-sectional analysis of baseline data from women who participated in the Activating Patients at Risk for OsteoPOroSis (APROPOS) randomized controlled clinical trial, which was nested within the Global Longitudinal Study of Osteoporosis in Women (GLOW) observational study as previously described [5]. Patients provided explicit consent for participation in APROPOS. A total of 2,684 US women from the seven GLOW U.S. sites (Birmingham, AL; Los Angeles, CA; Worcester, MA; New York, NY; Cincinnati, OH; Pittsburgh, PA; Seattle, WA) at high risk for future fracture were included. We defined a high risk of future fracture based on self-reported: (1) history of a prior fracture after age of 45 in prior GLOW surveys, and (2) no reported current use of osteoporosis medication with the exception of estrogen treatments [11].
Determining the contemplative stage of readiness to initiate osteoporosis treatment
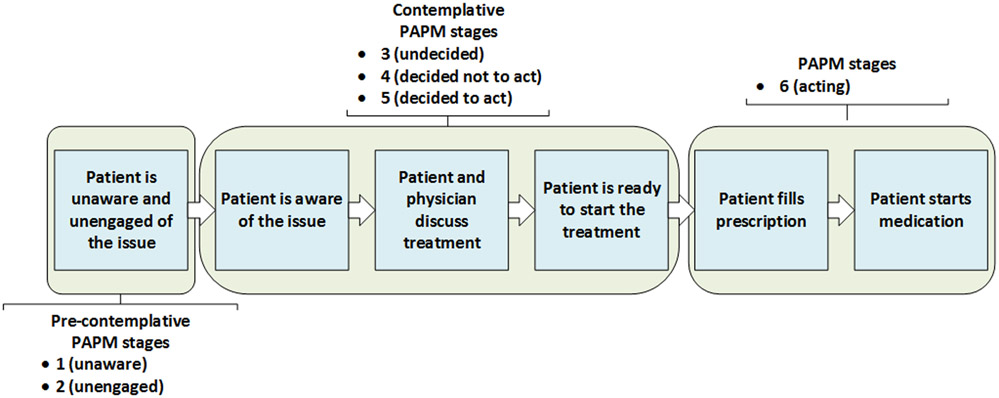
Overall, we measured the participant’s readiness to initiate osteoporosis treatment using a modified form of the Weinstein PAPM [10]. According to the PAPM theoretical model of behavior change, at any point, a person is in one of the seven stages of decision making about initiating osteoporosis treatment (Figure 1). The PAPM seven stages of behavior change can be then grouped into three main categories: 1)pre-contemplative stage in which individuals are not aware of a health problem and/or the behavior change needed to address it; 2) contemplative stage in which individuals are aware of the health problem and classify in the undecided, decided not to act, and decided to act stages of PAPM, and 3) action stage in which individuals already are engaged in the new behavior (Figure 1). In this study, we defined pre-contemplative participants as women who self-classified in the first and second stages of PAPM. Contemplative participants were those who self-classified in the third, fourth and fifth stages of PAPM.
Figure 1.
Multi-step process in osteoporosis treatment initiation illustrated using the Precaution Adoption Process Model (PAPM) stages of decision making.*
*PAPM stage 7 (maintenance stage) is not included in the figure
Factors associated with initiating treatment
We included the following independent variables as factors associated with initiating osteoporosis treatment: sociodemographic variables (age, race) [12], health literacy (based answers to a multiple choice screening question regarding respondents’ confidence about filling out medical forms by themselves, with “quite a bit” or “extremely” choices denoting “adequate” health literacy while responses of “somewhat,” “a little bit,” and “not at all” were denoting “not adequate” health literacy) [13], education level (“some college or more” or “high school graduate or less”) [14], self-reported history of depression and dementia (“yes” or “no”) [15], previous treatment for osteoporosis (“present” or “absent”) [16], whether participants had been told they had osteoporosis or osteopenia (“yes” or “no”, the two conditions were mutually exclusive) [16], whether participants had a major osteoporotic fracture in the past 12 months (hip, humerus, wrist, spine) (“yes” or “no”), and whether they had concerns about osteoporosis when they thought about their health (“yes” or “no”) [16].
Statistical analysis
We calculated the mean (SD) for continuous variables and frequencies and proportions to describe categorical variables. We then evaluated the association between the independent variables and the contemplative stage of readiness to initiate osteoporosis treatment (defined as pre-contemplative vs contemplative) using bivariate analyses. Forward selection multivariable analyses were used to determine the best and most parsimonious set of variables associated with the contemplative stage of readiness to initiate osteoporosis treatment. We entered variables of interest into a logistic regression model if the p values were less than 0.1 and retained in the final model only significant variables with p values less than 0.05 or variables considered clinically important (e.g., age, race, education, health literacy, major osteoporotic fracture in the past year, and current use of estrogen).We report unadjusted and adjusted odds ratios (ORs/aORs) and corresponding 95% confidence intervals (CIs) to express the strength of the association between independent variables and readiness for behavioral change. Given prior research [17], we report three multivariable models to account for potential collinearity between education level and health literacy. One model included both education and health literacy while the remaining two models included either education or health literacy. We also performed a sensitivity analysis to determine whether there were differences in the factors associated with contemplative stage of readiness to initiate osteoporosis treatment, or the strength of their association, based on history of major osteoporotic fracture in the past 12 months, including fracture of hip, spine, humerus and wrist. All analyses were conducted using SAS Version 9.3 (SAS Institute, Inc, Cary, NC, Enterprise Guide v4.3). The study was governed by the University of Alabama at Birmingham institutional review board (IRB).
Results
Out of 2,684 women at high risk of fracture enrolled in APROPOS, we excluded the 86 (3%) who reported being in the action stage of PAMP. In order to run a complete case analysis, we subsequently excluded an additional 872 (34%) women due to missing baseline survey data. Those with missing data had were more likely to be of Caucasian race, were younger, more educated and have higher health literacy. They were less likely to report an osteoporosis diagnosis or osteoporotic fracture in the past year, yet more likely to report a diagnosis of osteopenia (data not shown). Thus, our analysis included a total of 1,726 women, of which 412 (24.0%) were in contemplative and 1314 (76.0%) were in pre-contemplative stages of PAMP. Participants were 96% Caucasian, with a mean (SD) age 73.9 (7.6) years and 81% had some college education or more. The characteristics by stage of readiness to initiate osteoporosis treatment (pre-contemplative vs. contemplative) are summarized in Table 1.
Table 1.
Characteristics of APROPOS participants by level of readiness of behavioral change defined using Precaution Adoption Process Model (PAPM).
| Variable | Contemplative n = 412 (24%) |
Pre-contemplative n = 1,314 (76%) |
p-value | |||
|---|---|---|---|---|---|---|
| Age at baseline, years, mean (SD) | 74.5 (7.7) | 73.7 (7.6) | 0.08 | |||
| n | % | n | % | |||
| Age categories, years | 0.14 | |||||
| ≤70 | 130 | 31.6 | 462 | 35.2 | ||
| 70 - <80 | 172 | 41.8 | 558 | 42.7 | ||
| 80 - <90 | 97 | 23.5 | 271 | 20.6 | ||
| ≤90 | 13 | 3.2 | 23 | 1.8 | ||
| Race: White | 399 | 96.8 | 1,257 | 95.7 | 0.29 | |
| Education level: Some college or more | 339 | 82.3 | 1,060 | 80.7 | 0.47 | |
| Health literacy: Adequate | 360 | 87.4 | 1,193 | 90.8 | 0.04 | |
| Told they have osteoporosis | 217 | 54.3 | 174 | 13.4 | <0.0001 | |
| Told they have osteopenia (n = 1,304) | 147 | 80.3 | 420 | 37.5 | <0.0001 | |
| Being concerned about osteoporosis, yes | 358 | 86.9 | 634 | 48.3 | <0.0001 | |
| Prior osteoporosis treatment, yes | 353 | 85.7 | 633 | 48.2 | <0.0001 | |
| Current estrogen therapy, yes | 15 | 3.6 | 96 | 7.3 | 0.008 | |
| Major osteoporotic fracture in the past year (hip, humerus, wrist, spine) | 15 | 3.6 | 20 | 1.5 | 0.008 | |
Contemplative phase comprises women who self-classified in the in the third, fourth and fifth stages of PAPM. Pre-contemplative phase comprises women who self-classified in the first and second stages of PAPM. Having been told they have osteoporosis and having been told they have osteoporosis are mutually exclusive. Adequate health literacy category includes women who responded “quite a bit” or “extremely” when asked about their confidence about filling out medical forms by themselves.
Bivariate Analysis
We found that self-report of being concerned about osteoporosis [Odds Ratio [OR] (95% CI) 7.1 (95% CI 5.2-9.7)], having had prior osteoporosis treatment [OR 6.4 (95% CI 4.8-8.7)], having been told they have osteoporosis [OR 7.6 (95% CI 5.9-9.8)], or having been told they have osteopenia [OR 6.8 (95% CI 4.6-10.0)] were the major factors associated with being in the contemplative stage of behavior change. Having had a prior major osteoporotic fracture in the precedent year was a factor associated with being in the contemplative stage [OR 2.4 (95% CI 1.2-4.8)]. Women reporting current estrogen treatment were less likely to be in the contemplative stage [OR 0.5 (95% CI 0.3-0.8)]. Characteristics of APROPOS participants by level of readiness of behavioral change using Precaution Adoption Process Model (PAPM) are shown in Table 1.
Multivariable Analysis
After adjusting for age, race, education, health literacy, history of major osteoporotic fracture in the past 12 months and current estrogen treatment (C-statistic for the multivariable model was 0.85, Hosmer and Lemeshow Goodness-of-Fit was 0.6), contemplative women had a 3.5 fold higher odds of being concerned about osteoporosis [adjusted OR [aOR] 3.5 (95% CI 2.5-4.9) and 4.5 fold higher odds to report prior osteoporosis treatment [aOR 4.5 (95% CI 3.3-6.3)] compared with women who self-classified as pre-contemplative. Participants who were told they had osteoporosis had an 11.8-fold odds to be in the contemplative group (95% CI 7.8-17.8), while those who were told they had osteopenia had 3.8 fold odds to be in the contemplative group (95% CI 2.5-5.6) (Table 2). In multivariable models adjusting for age and race and which included either education level or health literacy as covariates, our findings did not change from what was observed when both variables were included in the model (Table 2).
Table 2.
Factors associated with contemplative level of readiness of behavior change using Precaution Adoption Process Model (PAPM) among all women included in the study (n = 1,726).
| Characteristics | Odds ratio (95% CI) Bivariate |
Adjusted Odds Ratio (95% CI) Multivariable model |
Adjusted Odds Ratio (95% CI) Multivariable model adjusted for age, race, education level |
Adjusted Odds Ratio (95% CI) Multivariable model adjusted for age, race, health literacy |
|---|---|---|---|---|
| Age (continuous) | 1.0 (1.0 - 1.0) | 1.0 (1.0 - 1.0) | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) |
| Race (white vs other) | 1.4 (0.8 - 2.6) | 1.2 (0.6 - 2.6) | 1.2 (0.6, 2.4) | 1.3 (0.6, 2.6) |
| Education level (some college or more vs high school graduate or less) | 1.1 (0.8 - 1.5) | 1.3 (0.9 - 1.9) | 1.3 (0.9, 1.8) | / |
| Health literacy (adequate vs not adequate) | 0.7 (0.5 - 1.0) | 0.9 (0.6 - 1.4) | / | 1.0 (0.7, 1.5) |
| Major osteoporotic fracture in the past 12 months (hip, humerus, wrist, spine) (yes vs no) | 2.4 (1.2 - 4.8) | 2.0 (0.9 - 4.7) | / | / |
| Current estrogen treatment | 0.5 (0.3 - 0.8) | 0.9 (0.5 - 1.8) | / | / |
| Prior osteoporosis treatment | 6.4 (4.8 - 8.7) | 4.5 (3.3 - 6.3) | 4.6 (3.4, 6.3) | 4.9 (3.6, 6.7) |
| Concerns about osteoporosis | 7.1 (5.2 - 9.7) | 3.5 (2.5 - 4.9) | 3.3 (2.4, 4.5) | 3.3 (2.4, 4.5) |
| Having been told they have osteoporosis | 7.6 (5.9 - 9.8) | 11.8 (7.8 - 17.8) | 11.3 (7.7, 16.6) | 11.3 (7.6, 16.7) |
| Having been told they have osteopenia | 6.8 (4.6 - 10.0) | 3.8 (2.5 - 5.6) | 3.7 (2.5, 5.3) | 3.8 (2.6, 5.6) |
Contemplative group comprises women who self-classified in the in the third, fourth and fifth stages of PAPM. Pre-contemplative group comprises women who self-classified in the first and second stages of PAPM. Having been told they have osteoporosis and having been told they have osteopenia are mutually exclusive, p<0.05 in italics.
We obtained similar results, albeit slightly attenuated, in a sensitivity analysis, which included only women who reported previous major osteoporotic fractures including fractures of hip, spine, humerus, and wrist (N=775, 27% contemplative) (Table 3).
Table 3.
Factors associated with contemplative level of readiness of behavior change using Precaution Adoption Process Model (PAPM) among women with major osteoporosis fracture (hip, spine, humerus, and wrist).
| Characteristics | Odds ratio (95% CI) Bivariate |
Adjusted Odds ratio (95% CI) Multivariable, Full Model |
|---|---|---|
| Age (continuous) | 1.0 (1.0 - 1.0) | 1.0 (1.0 - 1.0) |
| Race (white vs other) | 2.7 (0.9 - 7.8) | 2.6 (0.7 - 8.9) |
| Education (some college or more vs high school graduate or less) | 1.3 (0.9 - 1.9) | 1.6 (0.9 - 2.6) |
| Adequate health literacy (yes vs no) | 0.7 (0.4 - 1.1) | 0.8 (0.5 - 1.5) |
| Major osteoporotic fracture in the past 12 motnhs (hip, humerus, wrist, spine) (yes vs no) | 2.1 (1.1 - 4.2) | 1.9 (0.8 - 4.5) |
| Current estrogen treatment | 0.3 (0.1 - 0.9) | 0.9 (0.3 - 2.8) |
| Prior osteoporosis treatment | 6.3 (4.1 - 9.4) | 4.6 (2.9 - 7.3) |
| Concerns about osteoporosis | 5.3 (3.4 - 8.1) | 3.0 (1.8 - 4.9) |
| Having been told they have osteoporosis | 6.5 (4.6 - 9.3) | 10.0 (5.5 - 17.9) |
| Having been told they have osteopenia | 5.6 (3.2 - 9.8) | 3.3 (1.8 - 5.8) |
Contemplative phase comprises women who self-classified in the in the third, fourth and fifth stages of PAPM. Pre-contemplative phase comprises women who self-classified in the first and second stages of PAPM. Having been told they have osteoporosis and having been told they have osteopenia are mutually exclusive, p < 0.05 in italics.
Discussion
We identified the patient factors associated with contemplative stage of readiness of initiating osteoporosis treatment. We found that among women with a high risk of future fracture, only a quarter were contemplating whether or not to initiate osteoporosis therapy. Participants who had been previously told they had osteoporosis had approximately twelve-fold odds of being in this contemplative group, while those who had been told they had osteopenia had about four fold odds of being in the contemplative group. In addition, women who reported prior osteoporosis treatment and those who reported being concerned about osteoporosis were also more likely to be in the contemplative group. Knowledge of the characteristics influencing where a patient is in the process of considering and deciding about osteoporosis medication is clinically useful and might inform the design of future clinical interventions aimed at improving osteoporosis medication adherence at the point of care.
Our findings that the vast majority of women who had self-reported fractures after age 45, regardless of type (e.g., major osteoporotic fracture or other types of fracture) can be classified as pre-contemplative are similar to the results of previous studies that found that majority of women with fragility fractures were in the pre-contemplative phase of behavior change regarding osteoporosis treatment [18-20]. The proportion of individuals who were pre-contemplative in these studies varied between 65%-91%, with the difference attributable to individual characteristics (e.g., age, sex, education level) of the population being studied and the eligibility criteria for those studies. Similar to our observations, in studies with smaller sample sizes, the investigators found that a previous diagnosis of osteoporosis was associated with the contemplative stage of behavior change [18-20]. Taken together, these findings reveal a lack of awareness of the link between fractures and osteoporosis even among persons who have experienced fractures, thus underscoring the role of healthcare professionals in facilitating how patients advance through stages of contemplation regarding osteoporosis treatment.
The finding that the diagnosis of having osteoporosis is strongly associated with the contemplative stage reflects both the medical care contact and dependent patient stages of illness experience [21]. This reinforces the idea that receiving a diagnosis of osteoporosis legitimizes the illness and produces a fundamental shift in an individual’s understanding of their health state subsequently becomes a “patient” in need of osteoporosis treatment. Providing a diagnosis of osteoporosis or osteopenia for a patient should represent a catalyst of change and a “teaching moment”, where healthcare professionals and patients take the time to discuss osteoporosis consequences and treatment strategies. This conversation is essential because it has been shown that without receiving reliable information about the consequences of osteoporosis and available therapeutic options, patients may underestimate their risk of fractures and overestimate the risk of adverse events from medication [22-24]. However, understanding changes in human behavior is a complex topic and a difficult phenomenon to study. Indeed, there are several factors that play a role in whether an individual ultimately decides to change behavior. For example, self-efficacy, that reflects individuals` judgement of their ability to successfully perform a behavior and producing a favorable outcome (e.g., initiate osteoporosis medication) is an important determinant of behavioral change [25, 26].
Our study adds to the body of literature showing that women who classify in the pre-contemplative phase of behavior change differ in some characteristics compared to those who classify as contemplative. For example, a previous study showed that women from the general population in the pre-contemplative stage for initiating calcium supplements exhibit less knowledge of osteoporosis and report fewer expected benefits than women in contemplative stage [27]. However, while data provide further evidence that the awareness of osteoporosis is low among general population [28, 29], for conditions widely recognized as dangerous by the public such as hyperlipidemia, fewer individuals are in the pre-contemplative category. In a study of 404 individuals with elevated serum cholesterol, 35.6% were in the pre-contemplative stage of behavior change for initiating lipid lowering treatment [30], a proportion that was significantly lower than we and others have found among individuals with fractures and/or osteoporosis [18-20]. These data emphasize the need for more education of the general public on bone health, and particularly on the relationship between osteoporosis and fragility fractures. The most important risk factor of having a fragility fracture is having had a previous fracture [31]. Thus, improving patients’ awareness about the implications of experiencing a fragility fracture and its direct link to osteoporosis is a public health priority. Indeed, has been shown that promoting awareness and knowledge of patients with osteoporosis improved medication uptake and optimized osteoporosis care [32]. In the present analysis, we did not observe an association between health literacy or the level of education and the contemplative stage readiness to initiate osteoporosis treatment. However, the vast majority of the APROPOS cohort had an adequate health literacy and college education.
Our study results need to be interpreted in light of some limitations. This study was a secondary analysis of data collected as part of the APROPOS clinical trial. However, the large sample of women at high risk for fractures enrolled in APROPOS provided a valuable population resource to evaluate factors associated with readiness for behavior change regarding osteoporosis treatment. Because most women enrolled in our study were Caucasian and had higher health literacy and education levels compared to the general US population, the generalizability of our findings is limited. In addition, we collected information about osteoporosis or osteopenia diagnosis using surveys, and it is unclear whether women’s self-report of being told of an osteoporosis or osteopenia diagnosis is limited by patient recall bias. Some of the women who reported a fracture in GLOW had relatively minor events with limited sequelae (i.e. fractures that are not typically considered due to osteoporosis). The strong association between osteoporosis diagnosis and greater odds of moving to a more advanced stage of behavior change may reflect this partial misclassification. However, even when we restricted our analysis to those persons with more typical osteoporosis fractures, the main findings of our study were largely preserved.
In summary, we examined the factors associated with the contemplative stage of readiness to initiate osteoporosis treatment, and found that among women with high risk of future fracture, having been told by a health care provider that they had osteoporosis/osteopenia was independently associated with contemplating treatment for osteoporosis. Our findings may help in the design of future behavioral interventions to improve the uptake of osteoporosis treatment by increasing patient knowledge and awareness about bone health. The findings also highlight the likely importance of providing clear and consistent chronic disease diagnoses, such as osteoporosis, to our patients and should drive healthcare professionals, including bone specialists and primary care practitioners, to take the time to discuss osteoporosis consequences and treatment. More research is needed to understand the optimal strategies for motivating patients to transition to higher stages of decision making about initiating osteoporosis treatment.
Acknowledgements:
Trial registration: clinicaltrials.gov, identifier NCT01907269. This work was supported by R01 AR060240 (KGS) from the NIAMS/NIH. MID was supported by a K23 AR062100 award from NIAMS/NIH. NCW is supported by grant number K12HS023009 from the Agency for Healthcare Research and Quality. The NIAMS/NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflict of Interest
Giovanni Adami, Amy S. Mudano, Elizabeth J. Rahn, Ryan C. Outman, Susan L. Greenspan, Andrea Z. LaCroix, Jeri W. Nieves, Ethel S. Siris, Michael J. Miller, Sigrid Ladores, Maria I. Danila declare that they have no conflict of interest related to the present manuscript. The following authors declare the following conflicts of interest. Kenneth G. Saag - Amgen, Gilead, Radius (Consultant), Amgen (Research Grant); Nicole C. Wright - Amgen (Grants), Pfizer/Norton Rose/Fulbright (Expert Witness); Stuart L. Silverman- Radius, Amgen, Lilly (Speaker), Amgen (Grants), Amgen, Radius, Lilly (Advisory Board member); Nelson B. Watts - Amgen (Consultant, Speaker), Radius (Speaker); Jeffrey R. Curtis - Amgen/Radius (Consultant, Teaching);
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Giangregorio L, Papaioannou A, Cranney A, et al. (2006) Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum 35:293–305. 10.1016/j.semarthrit.2005.11.001 [DOI] [PubMed] [Google Scholar]
- 2.Solomon DH, Johnston SS, Boytsov NN, et al. (2014) Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res 29:1929–1937. 10.1002/jbmr.2202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wysowski DK, Greene P (2013) Trends in osteoporosis treatment with oral and intravenous bisphosphonates in the United States, 2002-2012. Bone 57:423–428. https://doi.Org/10.1016/j.bone.2013.09.008 [DOI] [PubMed] [Google Scholar]
- 4.Black DM, Rosen CJ (2016) Clinical Practice. Postmenopausal Osteoporosis. N Engl J Med 374:254–262. 10.1056/NEJMcp1513724 [DOI] [PubMed] [Google Scholar]
- 5.Danila MI, Outman RC, Rahn EJ, et al. (2016) A multi-modal intervention for Activating Patients at Risk for Osteoporosis (APROPOS): Rationale, design, and uptake of online study intervention material. Contemp Clin Trials Commun 4:14–24. https://doi.Org/10.1016/j.conctc.2016.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yood RA, Mazor KM, Andrade SE, et al. (2008) Patient Decision to Initiate Therapy for Osteoporosis: The Influence of Knowledge and Beliefs. J GEN INTERN MED 23:1815 10.1007/s11606-008-0772-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gadkari AS, McHomey CA (2010) Medication nonfulfillment rates and reasons: narrative systematic review. Curr Med Res Opin 26:683–705. 10.1185/03007990903550586 [DOI] [PubMed] [Google Scholar]
- 8.McHomey CA, Spain CV (2011) Frequency of and reasons for medication non-fulfillment and non persistence among American adults with chronic disease in 2008. Health Expect 14:307–320. https://doi.Org/10.1111/j.1369-7625.2010.00619.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu J, Brenneman SK, Sazonov V, Modi A (2015) Reasons for not initiating osteoporosis therapy among a managed care population. Patient Prefer Adherence 9:821–830. 10.2147/PPA.S81963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinstein ND (1988) The precaution adoption process. Health Psychol 7:355–386 [DOI] [PubMed] [Google Scholar]
- 11.Danila MI, Outman RC, Rahn EJ, et al. (2018) Evaluation of a Multi-modal, Direct-to-Patient Educational Intervention Targeting Barriers to Osteoporosis Care: A Randomized Clinical Trial. J Bone Miner Res 33:763–772. 10.1002/jbmr.3395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. The Lancet 359:1761–1767. 10.1016/S0140-6736(02)08657-9 [DOI] [PubMed] [Google Scholar]
- 13.Morris NS, MacLean CD, Chew LD, Littenberg B (2006) The Single Item Literacy Screener: Evaluation of a brief instrument to identify limited reading ability. BMC Family Practice 7:21 10.1186/1471-2296-7-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heidari B, Hosseini R, Javadian Y, et al. (2015) Factors affecting bone mineral density in postmenopausal women. Arch Osteoporos 10:15 10.1007/s11657-015-0217-4 [DOI] [PubMed] [Google Scholar]
- 15.Amouzougan A, Lafaie L, Marotte H, et al. (2017) High prevalence of dementia in women with osteoporosis. Joint Bone Spine 84:611–614. 10.1016/j.jbspin.2016.08.002 [DOI] [PubMed] [Google Scholar]
- 16.Yeam CT, Chia S, Tan HCC, et al. (2018) A systematic review of factors affecting medication adherence among patients with osteoporosis. Osteoporos Int. 10.1007/s00198-018-4759-3 [DOI] [PubMed] [Google Scholar]
- 17.Schmitt M, Miller M, Harrison D, et al. (2011) Communicating non-steroidal anti-inflammatory drug risks: Verbal counseling, written medicine information, and patients’ risk awareness. Patient Educ Couns June;83(3):391–7. https://doi.Org/10.1016/j.pec.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 18.Sujic R, Beaton DE, Bogoch ER (2016) Patient acceptance of osteoporosis treatment: Application of the stages of change model. Maturitas 88:70–75. https://doi.Org/10.1016/j.maturitas.2016.03.021 [DOI] [PubMed] [Google Scholar]
- 19.Mauck KF, Cuddihy MT, Trousdale RT, et al. (2002) The decision to accept treatment for osteoporosis following hip fracture: exploring the woman’s perspective using a stage-of-change model. Osteoporos Int 13:560–564. 10.1007/s001980200073 [DOI] [PubMed] [Google Scholar]
- 20.Escott B, Elliot-Gibson V, Bogoch E, Beaton D (2007) Stage-of-Change Model Applied to Osteoporosis Medication Use at the Time of Fragility Fracture. ASBMR Honolulu, Hawaii, September 16 - 19, 2007. J Bone Miner Res 22 (Suppl. 1) s203 (Abstract): [Google Scholar]
- 21.Suchman EA (1965) Stages of Illness and Medical Care. Journal of Health and Human Behavior 6:114–128. 10.2307/2948694 [DOI] [PubMed] [Google Scholar]
- 22.Rothmann MJ, Ammentorp J, Bech M, et al. (2015) Self-perceived facture risk: factors underlying women’s perception of risk for osteoporotic fractures: the Risk-Stratified Osteoporosis Strategy Evaluation study (ROSE). Osteoporos Int 26:689–697. 10.1007/s00198-014-2936-6 [DOI] [PubMed] [Google Scholar]
- 23.Gerend MA, Aiken LS, West SG, Erchull MJ (2004) Beyond medical risk: investigating the psychological factors underlying women’s perceptions of susceptibility to breast cancer, heart disease, and osteoporosis. Health Psychol 23:247–258. https://doi.Org/10.1037/0278-6133.23.3.247 [DOI] [PubMed] [Google Scholar]
- 24.Giangregorio L, Dolovich L, Cranney A, et al. (2009) Osteoporosis risk perceptions among patients who have sustained a fragility fracture. Patient Educ Couns 74:213–220. https://doi.Org/10.1016/j.pec.2008.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solimeo SL, Nguyen V-TT, Edmonds SW, et al. (2019) Sex differences in osteoporosis self-efficacy among community-residing older adults presenting for DXA. Osteoporos Int. 10.1007/s00198-019-04854-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhu S, Nahm E-S, Resnick B, et al. (2017) The Moderated Mediating Effect of Self-Efficacy on Exercise Among Older Adults in an Online Bone Health Intervention Study: A Parallel Process Latent Growth Curve Model. J Aging Phys Act 25:378–386. 10.1123/japa.2016-0216 [DOI] [PubMed] [Google Scholar]
- 27.Blalock SJ (2007) Predictors of calcium intake patterns: a longitudinal analysis. Health Psychol 26:251–258. https://doi.Org/10.1037/0278-6133.26.3.251 [DOI] [PubMed] [Google Scholar]
- 28.Wright NC, Melton ME, Sohail M, et al. (2019) Race Plays a Role in the Knowledge, Attitudes, and Beliefs of Women with Osteoporosis. J Racial Ethn Health Disparities. 10.1007/s40615-019-00569-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noel SE, Mangano KM, Griffith JL, et al. (2018) Prevalence of Osteoporosis and Low Bone Mass Among Puerto Rican Older Adults. J Bone Miner Res 33:396–403. 10.1002/jbmr.3315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson SS, Driskell M-M, Johnson JL, et al. (2006) Transtheoretical Model Intervention for Adherence to Lipid-Lowering Drugs. Disease Management 9:102–114. https://doi.Org/10.1089/dis.2006.9.102 [DOI] [PubMed] [Google Scholar]
- 31.Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297:387–394. https://doi.Org/10.1001/jama.297.4.387 [DOI] [PubMed] [Google Scholar]
- 32.Jaleel A, Saag KG, Danila MI (2018) Improving drug adherence in osteoporosis: an update on more recent studies. Ther Adv Musculoskelet Dis 10:141–149. 10.1177/1759720X18785539 [DOI] [PMC free article] [PubMed] [Google Scholar]