Abstract
OBJECTIVE:
Disparities exist between population subgroups in the use of gynecologic oncologists and high-volume hospitals. The objectives of this study were to explore the experiences of black women obtaining ovarian cancer (OC) care at a high-volume center (HVC) and to identify patient-, provider-, and systems-related factors affecting their access to and use of this level of care.
MATERIALS AND METHODS:
Twenty-one semistructured interviews were conducted as part of an institutional review board–approved protocol with women who self-identified as black or African American, treated for OC at a single HVC from January 2013 to May 2017. Recurring themes were identified in transcribed interviews through the process of independent and collaborative thematic content analysis.
RESULTS:
Five themes were identified: (1) internal attributes contributing to black women’s ability/desire to be treated at an HVC, (2) pathways to high- and low-volume centers, (3) obstacles to obtaining care, (4) potential barriers for black women interested in treatment at an HVC, and (5) suggestions for improving HVC use by black women. Study participants who successfully accessed care were comfortable navigating the health care system, understood the importance of self-advocacy, and valued the expertise of an HVC. Barriers to obtaining care at an HVC included lack of knowledge about the HVC, lack of referral, transportation difficulties, and lack of insurance coverage.
CONCLUSION:
In this qualitative study, black women treated at an HVC shared attributes and experiences that helped them access care. There is a need to collaborate with black communities and establish interventions to reduce barriers, facilitate access, and disseminate information about the value of receiving care for OC at an HVC.
INTRODUCTION
Despite growing evidence that ovarian cancer outcomes are improved at tertiary care centers, disparities among population subgroups in using and accessing high-volume providers and high-volume centers (HVCs) persist.1-3 This holds true regardless of insurance status, comorbidities, cancer stage, or tumor grade. Women treated for ovarian cancer at HVCs are more likely to be white and have higher household incomes and private health insurance.4 Black women with ovarian cancer are less likely to use HVCs; consequently, they are less likely to receive optimal surgery, adjuvant chemotherapy, and care adherent to National Comprehensive Cancer Network guidelines.5-8 As a population, black women have lower overall survival rates.9 However, studies also show that with equal use of expert care, the differences in treatment and survival dissipate.10-12
There is a dearth of published literature on the experiences of black patients with ovarian cancer accessing HVCs. Previous research has prioritized identification of disparities using national, statewide, and hospital-based databases, demonstrating that black women have poorer outcomes and less access.6,7,10,13-22 Hypotheses regarding why such disparities exist have been extrapolated from these retrospective population-based studies.
Currently, there is no validated tool to assess the experiences of patients with cancer attempting to use the health care system. Qualitative research methodology serves to explore beliefs and attitudes, is a useful research approach in understudied areas, and is ideal for gathering new information on recurring phenomena. There are more than 50 qualitative studies in ovarian cancer research, but to our knowledge, no prior study comprehensively has investigated the experiences of black women accessing care. Because racial disparities in access exist regardless of insurance status, the patient population at our HVC offers a unique opportunity to explore the experiences of black patients. With respect to racial disparities, patients’ experiences in obtaining this level of care and perceived barriers to accessing care are of specific interest. The objectives of this study were to investigate the experiences of black women obtaining ovarian cancer care at a single HVC and to identify patient-, provider-, and systems-related factors affecting their ability to access and use this care.
MATERIALS AND METHODS
We conducted semistructured interviews with patients treated at a National Cancer Institute–designated comprehensive cancer center (Memorial Sloan Kettering Cancer Center). After approval of this study by the Memorial Sloan Kettering Cancer Center Institutional Review Board, research personnel used a prospectively managed database to identify all living women diagnosed with ovarian, fallopian tube, or peritoneal cancer older than 18 years of age, who self-identified as black or African American treated at our institution (starting in 2017, working back in time to 2013). We used the electronic medical record to confirm the demographic and treatment information of eligible women. We excluded women who were cognitively impaired or did not speak English.
A recruitment letter was sent to eligible participants, who were subsequently contacted by phone (in reverse chronologic order). Some were also approached during clinic visits. We purposely oversampled patients with advanced disease. Figure 1 depicts the patient flowchart. Patients who agreed to participate provided verbal consent by telephone or in person before their interview; consent included permission to audio-record the interviews.
Fig 1.
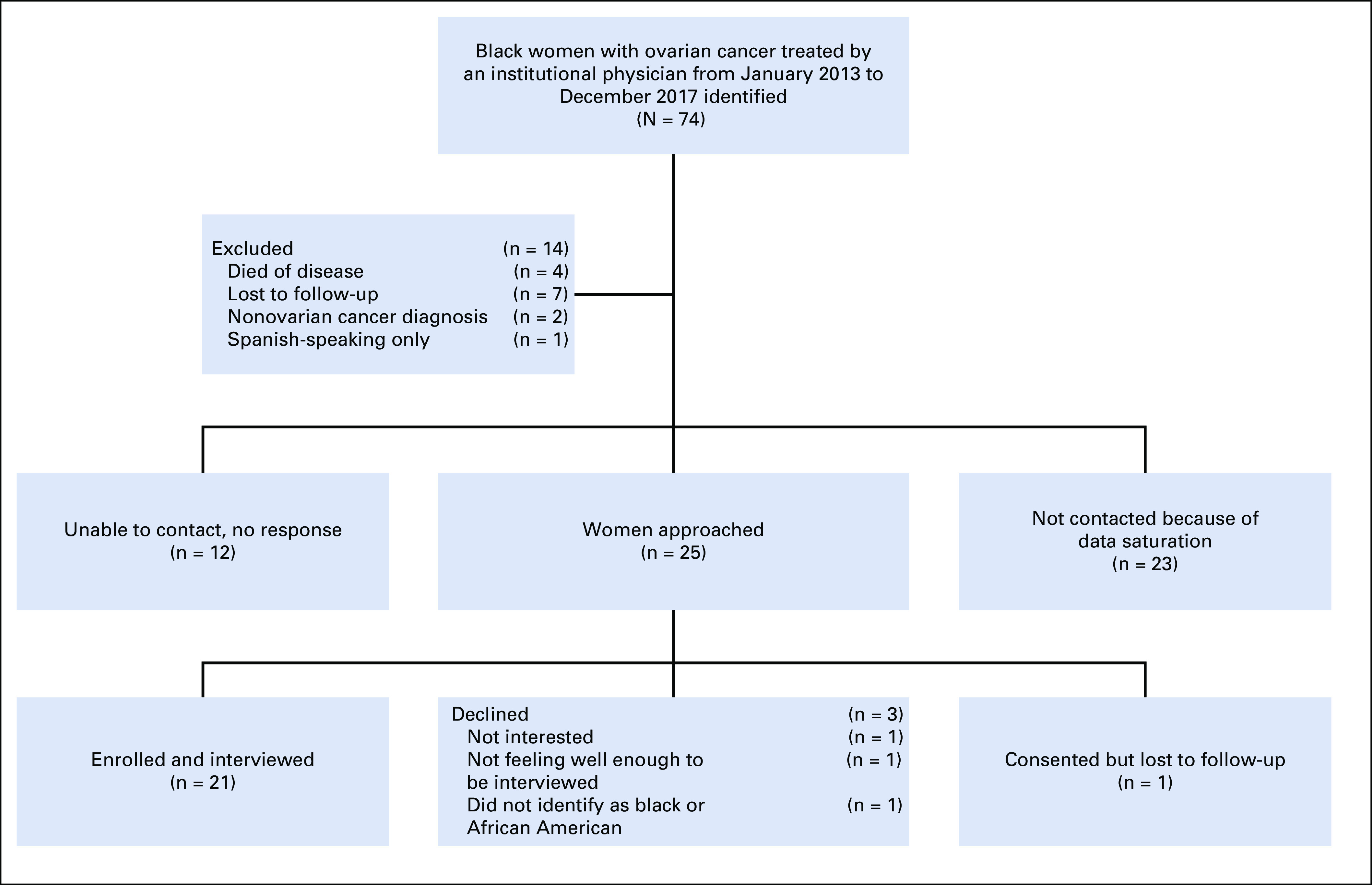
Patient flowchart showing how patients were accrued to the study. An institutional database was used to identify eligible participants. We sent a recruitment letter to the women who had been diagnosed with advanced disease and subsequently contacted them by phone in reverse chronologic order to seek their participation. To expedite accrual, some participants were also approached during medical oncology clinic visits.
After a review of the literature, a semistructured interview guide was developed with a qualitative methods specialist (E.S.) from the Behavioral Research Methods Core Facility and reviewed by coauthors for content, clarity, and relevance. The interview included open-ended questions in five domains, detailed in the Data Supplement.
Individual interviews were conducted by phone or in person. Interviews were recorded and transcribed. One author who has formal training in qualitative research methodology (R.A.C.) conducted all the interviews. Participants were able to interpret questions independently and respond freely. The interviewer used the conversation as an opportunity to explore previously unidentified areas of inquiry if she determined they were relevant to the research objectives. This interview format is the one most commonly used by qualitative researchers.23
Transcripts were coded by three trained authors (R.A.C., E.S., M.B.) using grounded theory.24 The authors reviewed and coded transcripts through independent and collaborative thematic content analysis24-27 using ATLAS.ti (ATLAS.ti Scientific Software Development, Berlin, Germany), a qualitative data analysis software package.28 During the first stage of content analysis, each coder independently read five transcripts (20% of total proposed sample), identifying key narrative content, creating codes, assigning relevant codes to content, and developing a codebook. The team met weekly to discuss differences in interpretation and reach consensus. After completion of coding, the team engaged in a secondary analysis in which they synthesized coded narrative content and described recurring themes. As is ideal for most qualitative studies, thematic analysis was performed in parallel with patient accrual. This allowed the investigators to develop a better understanding of the research question as study enrollment continued. By coding interviews as they were completed, data saturation was determined.23,29
Recent qualitative studies conducted in a comparable population have reported on data derived from seven to 28 participants.30-34 The Behavioral Research Methods Core Facility has expertise in this area and estimated that a reasonable goal was 25 participants (although data saturation among a relatively homogenous group often occurs within the first 12 interviews).35 In this study, data saturation was achieved after 21 patients were interviewed and enrolled.
RESULTS
Participant Cohort
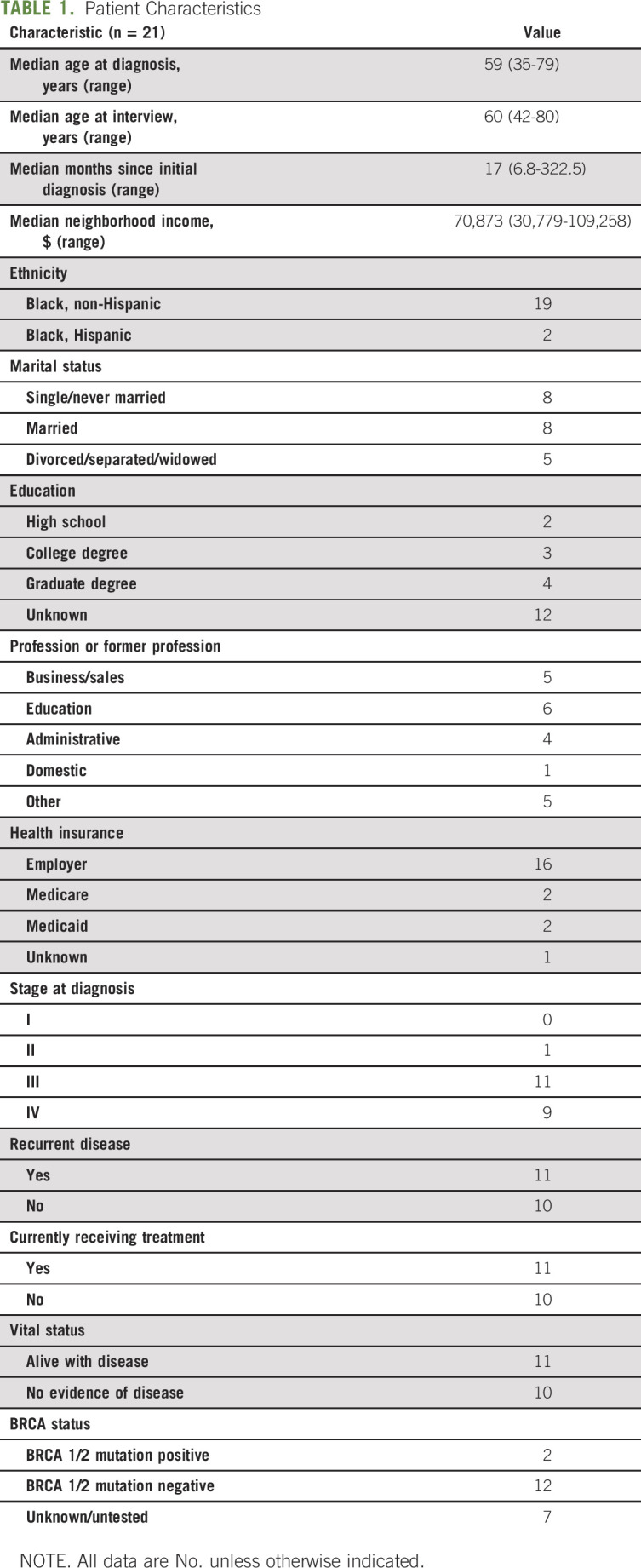
Twenty-one women were interviewed. Median age at diagnosis was 59 years (range, 35 to 79 years). Median time from date of diagnosis to date of interview was 17 months (range, 6 to 322 months). Twenty participants were initially diagnosed with advanced-stage disease; 11 had evidence of disease and were undergoing treatment at the time of their interviews. Most received all their care at this HVC; two patients had surgeries at outside hospitals (OSHs), three initiated chemotherapy at OSHs, and three had been treated at an OSH at the time of initial diagnosis but transferred to our institution when diagnosed with a recurrence.
The neighborhood median income for the cohort was $70,873 (range, $30,779 to $109,258). According to 2014 Census data, seven of 21 participants (33%) lived in zip codes with a median income below the national average. Sixteen (76%) had employer-sponsored insurance, and four (19%) had government safety-net insurance. Table 1 lists demographic information.
TABLE 1.
Patient Characteristics
Thematic Findings
In the following sections and the Data Supplement, we summarize five main themes and representative quotes from the analysis.
Theme 1: Common characteristics.
Many interviewees described character traits that made them more likely to seek care at an HVC. The most commonly described traits were health literacy, persistence, self-advocacy, and perceived value in expert/specialty care.
Participants characterized as health literate had a baseline understanding of the health care and/or insurance system and how to navigate it:
So I sat down at my computer, and I had not accessed my records through my primary doctor because I hadn’t been going there that long.…And on the very first page, the very first test result was the CA 125 high….So when I saw that, I immediately called my oncologist and asked for an appointment….I also downloaded all the test results that the primary care doctor had done.
Several women discussed having to advocate for themselves. They described scenarios in which they had to be patient and persistent to get an appointment.
I kept calling them. Can I get this appointment? Well, Ms T, you have to get the paperwork and so I made sure to keep following through and following up until I got my appointment. And made sure I faxed and did the necessary steps that were asked.
Many participants perceived additional value in undergoing treatment at a cancer specialty hospital. They expressed hope that they would have a better outcome by going to an HVC. One woman compared specialty hospitals with specialty restaurants:
When you want an authentic experience—let's say you like Korean food, right? You're going to go to House of Seoul for Korean food. You're not going to go to Beni's Trattoria Italiano for Korean food. They may have one night that they serve great Korean, but then they go back to selling pizza every day. My philosophy is I want to go to a place that has experts in cancer, that that's all they do, that's all they know, that's what they're trained to do.
Theme 2: Journey to our institution.
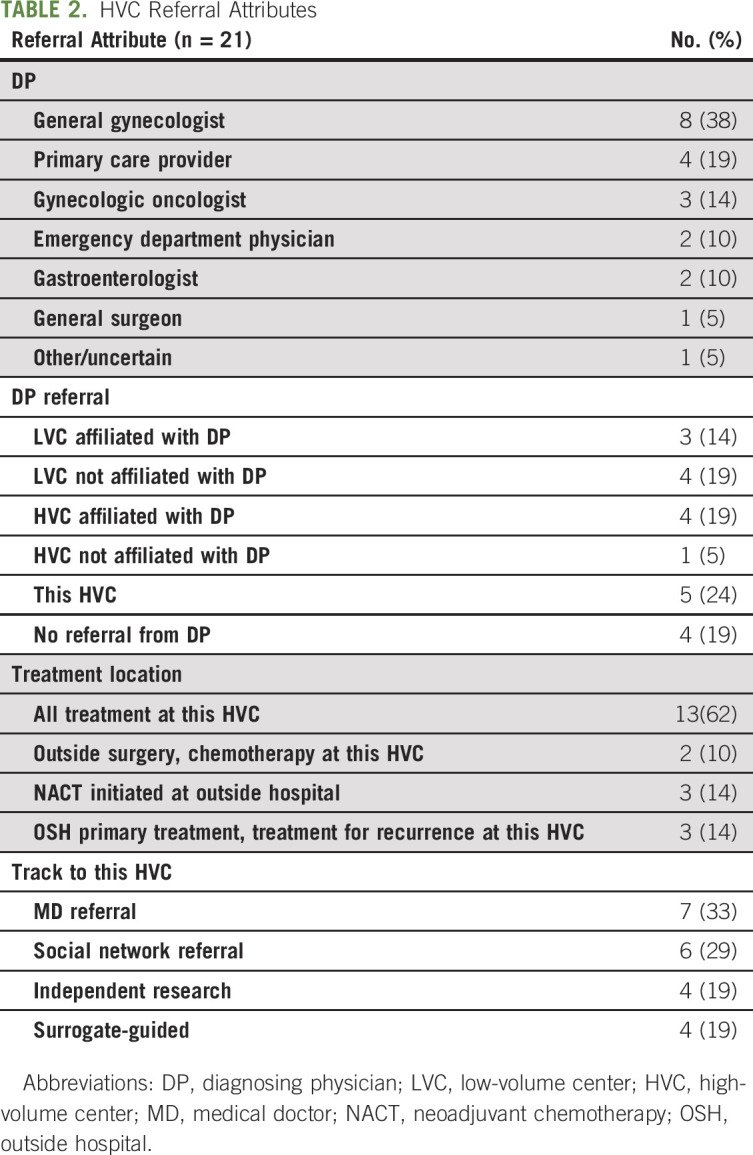
Participants were asked to share stories of how they came to our institution for treatment. They were most often diagnosed by a general gynecologist (38%), primary care physician (19%), or gynecologic oncologist (14%; Table 2). Diagnosing physicians either referred these women directly to our institution (24%), to another HVC they were affiliated with (19%), to another HVC they were not affiliated with (5%), to a low-volume center (LVC) they were affiliated with (14%), or to an LVC they were not affiliated with (19%). Several patients reported that they had never received a referral from their diagnosing physician (19%). Four general paths to our institution emerged: (1) patients were referred by the physician who diagnosed them or by another external physician (33%); (2) they were referred by a member of their social network, such as a friend, family member, or coworker (29%); (3) they did their own research, usually on the Internet, and determined that our institution was the best place for treatment (19%); and (4) someone, usually a child or sibling, served as a medical surrogate and dictated where their treatment should take place (19%). Participants who lacked the traits and values that emerged in theme 1 often had another person involved in their medical decision making who directed their care.
TABLE 2.
HVC Referral Attributes
Theme 3: Obstacles.
Many of the interviewees faced potential barriers to initiating care at this HVC, such as unfamiliarity with the facility, lack of referral, limited access (ie, transportation difficulties, financial obstacles, insurance issues, and so on); however, these obstacles were overcome by internal character traits or external support from social networks. Patients referred to LVCs spoke about having to advocate for referral to an HVC or having a member of their social network suggest seeking another opinion. Several women, who may have lacked health literacy, described not knowing that cancer centers existed or feeling that they did not belong to the appropriate sociodemographic for a specialty center:
I had an idea of [this hospital] but my idea was probably just a private hospital and I couldn’t afford it. So I wasn’t going to explore it but [my son] went online and then I called and when I called they asked me the type of insurance I had and then I gave it to them and they accepted it.
We hypothesized that some participants may have seen race as a potential barrier to accessing HVC care. However, when asked, 20 of the participants (95%) responded “No,” and one said she was uncertain whether race had played a role.
Theme 4: Why don’t more black women come to our institution?
Participants were asked to share their views on why more black women do not use our institution for ovarian cancer treatment. Reflecting on their own experiences, many concluded that there was a lack of knowledge in the black community about the potential for care at an HVC. They also described the importance of the trusting relationship that exists between patients and diagnosing physicians, and hypothesized that if diagnosing physicians do not refer black patients to our institution, few of their patients will seek care here for themselves. Numerous participants brought up the fact that this HVC does not accept certain forms of insurance and the difficulties posed by traveling to our institution for treatment as possible obstacles to initiating care here. There was significant overlap in these subthemes, described in the following quotation and in the Data Supplement:
I think the difference is simply in the sense of information and access. And believing that you deserve the best. It's those three things—information, then access, which comes from the information. And that the end for you to believe that, you know, you deserve the best care that you can get.…So I feel that they don't come here because of the lack of information….And also…many of them don't believe that they can, you see since they are poor…they are a minority, you know, because of their prior experiences in the society.
Theme 5: How can we encourage more black women to use our services?
Several interviewees had suggestions for improving black women’s use of our institution. Lack of knowledge about this HVC was frequently cited as a potential barrier. They suggested addressing this through outreach to patients, their social networks, and diagnosing providers. In addition, participants felt there was a lack of diverse patient-directed marketing. Some had seen commercials highlighting the research conducted at our institution but would have preferred ad campaigns focusing on high-quality patient care:
Patient 74: Going into the community is the way you get the work done….Go to the churches on Sundays in various places, start with Harlem. Go to Spanish Harlem, you know, go to the Bronx. Go to Brooklyn, Queens, you know, and even Staten Island you see because one place to find these people is in the church.
Daughter: Since you started your care here, I noticed that there has been a series of ad campaigns. But those ad campaigns have always been focused on, like...
Patient 74: Science.
Daughter: And finding a cure. Right. And maybe the same way that you can focus on having an ad campaign advertising that [this HVC] is doing the research to find a cure, there should also be, like, an ad campaign saying, you can come here.
DISCUSSION
As novel treatments improve survival outcomes, the elimination of health care disparities remains a priority.36,37 To comprehend the complexities of disparities in provider preference and use, we must understand patients’ experiences. This study fills a gap in our understanding of the factors associated with use of an HVC by black women with ovarian cancer. Our results indicate that black women treated at this HVC have overlapping attributes that led them to seek and obtain treatment here. They also have shared perceptions about the potential barriers faced by other black women and how those can be overcome.
A 2014 qualitative study on the perceptions of investigators, research staff, and referring clinicians regarding barriers to and facilitators of minority recruitment for clinical trials at five National Cancer Institute–designated cancer centers reported similar observations. Although the authors did not assess the opinions of minority patients directly, they found that many stakeholders thought developing a rapport with minority communities and external physicians would be a primary facilitator for increasing minority participation in clinical cancer trials.38 Although our focus was not clinical trial enrollment, those sentiments were echoed by our participants with respect to increasing black patients’ use of HVCs. Thirty-three percent of our participants were referred by their diagnosing physicians to hospitals that did not have expertise in ovarian cancer treatment. More than half of the diagnosing physicians who referred patients to LVCs were not affiliated with said LVCs. Of note, these patients either had Medicare insurance or were employed in blue-collar jobs. This highlights the potential age-related and financial obstacles to seeking expert treatment. Developing a rapport with diagnosing physicians and educating all providers on the benefits of ovarian cancer care at HVCs could shunt a large group of eligible black women into HVC systems.
A 2003 survey of a sample of US residents examined how patients choose physicians.39 The authors found that race and ethnicity were strong determinants, even after controlling for health and insurance status; black patients were less likely than their white counterparts to seek information from social networks and more likely to use formal sources, such as referring physicians. Although a large portion of our cohort did rely on their social networks for recommendations, more were referred by a diagnosing physician. Lack of physician referral emerged as a potential barrier (but a modifiable barrier) for other black women seeking care.
Another key component in accessing an HVC is the phone call. In our cohort, the phone call to initiate care was most often made by participants themselves; however, surrogates and diagnosing physicians may also call and make appointments. Admittedly, all HVCs cannot accommodate all patients. Currently, this is a systems-related barrier, not modifiable at the provider or patient level. Preferably, patients who cannot be seen at one HVC because of insurance issues can be referred to HVCs that accept their insurance. When no other options exist, a patient may be referred to an LVC. However, this should seldom occur in the patient population we serve because this state is home to more than 100 gynecologic oncologists and only two low-access counties in which only 1% of the state’s female population lives.40
As with most qualitative studies, ours was a small convenience sample. It may be representative of black women at an urban cancer center but not of all black women in other settings. Although our results lack generalizability, they do provide a basis for future studies and interventions. The combination of phone and in-person interviews was particularly helpful, allowing us to sample a diverse group of women at various stages of their journey through treatment. Because we depended on patient reporting, there may have been elements of recall and selection bias. The process of accessing care may have seemed easier to some patients in hindsight.
Despite these limitations, this study fills a critical gap by interviewing black women about their experiences accessing and using care for ovarian cancer. Our findings provide a template and conceptual framework for research at both HVCs and LVCs. Future research should explore the experiences of black women who do not use expert care.
This study identifies a need for collaboration with black communities and educational interventions for the general population. Our findings suggest that if black patients know that treatment at an HVC is associated with improved survival outcomes and that access to this type of care is available to them, they will use it. As a community of providers and researchers, it is our responsibility to provide patients with as much information as possible so that they can make optimal health care decisions. Clinical practice should offer relevant information so that treatment decisions are aligned with the individual patient’s needs. Regardless of affiliation, it is important that diagnosing physicians refer patients with suspected advanced ovarian cancer to HVCs.
ACKNOWLEDGMENT
Supported in part through the National Institutes of Health/National Cancer Institute Support Grant No. P30 CA008748. Presented in part as a poster at the 49th Society of Gynecologic Oncology Annual Meeting on Women’s Cancer, New Orleans, LA, March 24 to 27, 2018.
AUTHOR CONTRIBUTIONS
Conception and design: Renee A. Cowan, Dennis S. Chi, Carla Boutin-Foster, Carol L. Brown, Kara Long Roche
Provision of study materials or patients: Nadeem R. Abu-Rustum, Dennis S. Chi, Carol L. Brown, Kara Long Roche
Collection and assembly of data: Renee A. Cowan, Maureen Byrne, Kara Long Roche
Data analysis and interpretation: Renee A. Cowan, Elyse Shuk, Maureen Byrne, Nadeem R. Abu-Rustum, Carla Boutin-Foster, Kara Long Roche
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Factors Associated With Use of a High-Volume Cancer Center by Black Women With Ovarian Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Nadeem R. Abu-Rustum
Honoraria: Prime Oncology
Research Funding: Stryker/Novadaq (Inst), Olympus (Inst), Grail (Inst)
Travel, Accommodations, Expenses: Prime Oncology
Dennis S. Chi
Leadership: C Surgeries
Stock and Other Ownership Interests: Bovie Medical, Verthermia, Intuitive Surgical, TransEnterix
Consulting or Advisory Role: Bovie Medical, Verthemia
Kara Long Roche
Travel, Accommodations, Expenses: Intuitive Surgical
No other potential conflicts of interest were reported.
REFERENCES
- 1.Bristow RE, Palis BE, Chi DS, et al. The National Cancer Database report on advanced-stage epithelial ovarian cancer: Impact of hospital surgical case volume on overall survival and surgical treatment paradigm. Gynecol Oncol. 2010;118:262–267. doi: 10.1016/j.ygyno.2010.05.025. [DOI] [PubMed] [Google Scholar]
- 2.Cliby WA, Powell MA, Al-Hammadi N, et al. Ovarian cancer in the United States: Contemporary patterns of care associated with improved survival. Gynecol Oncol. 2015;136:11–17. doi: 10.1016/j.ygyno.2014.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bristow RE, Chang J, Ziogas A, et al. High-volume ovarian cancer care: Survival impact and disparities in access for advanced-stage disease. Gynecol Oncol. 2014;132:403–410. doi: 10.1016/j.ygyno.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 4.Wright JD, Herzog TJ, Siddiq Z, et al. Failure to rescue as a source of variation in hospital mortality for ovarian cancer. J Clin Oncol. 2012;30:3976–3982. doi: 10.1200/JCO.2012.43.2906. [DOI] [PubMed] [Google Scholar]
- 5.Chan JK, Zhang M, Hu JM, et al. Racial disparities in surgical treatment and survival of epithelial ovarian cancer in United States. J Surg Oncol. 2008;97:103–107. doi: 10.1002/jso.20932. [DOI] [PubMed] [Google Scholar]
- 6.Williams VL, Stockwell HG, Hoffman MS, et al. Racial differences in treatment modalities among female residents of Florida diagnosed with epithelial ovarian cancer. J Gynecol Surg. 2010;26:15–22. [Google Scholar]
- 7.Aranda MA, McGory M, Sekeris E, et al. Do racial/ethnic disparities exist in the utilization of high-volume surgeons for women with ovarian cancer? Gynecol Oncol. 2008;111:166–172. doi: 10.1016/j.ygyno.2008.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boyd LR, Novetsky AP, Curtin JP. Ovarian cancer care for the underserved: Are surgical patterns of care different in a public hospital setting? Cancer. 2011;117:777–783. doi: 10.1002/cncr.25490. [DOI] [PubMed] [Google Scholar]
- 9.Brewer KC, Peterson CE, Davis FG, et al. The influence of neighborhood socioeconomic status and race on survival from ovarian cancer: A population-based analysis of Cook County, Illinois. Ann Epidemiol. 2015;25:556–563. doi: 10.1016/j.annepidem.2015.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bristow RE, Ueda S, Gerardi MA, et al. Analysis of racial disparities in stage IIIC epithelial ovarian cancer care and outcomes in a tertiary gynecologic oncology referral center. Gynecol Oncol. 2011;122:319–323. doi: 10.1016/j.ygyno.2011.04.047. [DOI] [PubMed] [Google Scholar]
- 11.Terplan M, Temkin S, Tergas A, et al. Does equal treatment yield equal outcomes? The impact of race on survival in epithelial ovarian cancer. Gynecol Oncol. 2008;111:173–178. doi: 10.1016/j.ygyno.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bristow RE, Chang J, Ziogas A, et al. Sociodemographic disparities in advanced ovarian cancer survival and adherence to treatment guidelines. Obstet Gynecol. 2015;125:833–842. doi: 10.1097/AOG.0000000000000643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McGuire V, Jesser CA, Whittemore AS. Survival among U.S. women with invasive epithelial ovarian cancer. Gynecol Oncol. 2002;84:399–403. doi: 10.1006/gyno.2001.6536. [DOI] [PubMed] [Google Scholar]
- 14.Nelson A. Unequal treatment: Confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94:666–668. [PMC free article] [PubMed] [Google Scholar]
- 15.Harlan LC, Clegg LX, Trimble EL. Trends in surgery and chemotherapy for women diagnosed with ovarian cancer in the United States. J Clin Oncol. 2003;21:3488–3494. doi: 10.1200/JCO.2003.01.061. [DOI] [PubMed] [Google Scholar]
- 16.Liu JH, Zingmond DS, McGory ML, et al. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA. 2006;296:1973–1980. doi: 10.1001/jama.296.16.1973. [DOI] [PubMed] [Google Scholar]
- 17.Farley J, Risinger JI, Rose GS, et al. Racial disparities in blacks with gynecologic cancers. Cancer. 2007;110:234–243. doi: 10.1002/cncr.22797. [DOI] [PubMed] [Google Scholar]
- 18.Bristow RE, Zahurak ML, Ibeanu OA. Racial disparities in ovarian cancer surgical care: A population-based analysis. Gynecol Oncol. 2011;121:364–368. doi: 10.1016/j.ygyno.2010.12.347. [DOI] [PubMed] [Google Scholar]
- 19.Chase DM, Fedewa S, Chou TS, et al. Disparities in the allocation of treatment in advanced ovarian cancer: Are there certain patient characteristics associated with nonstandard therapy? Obstet Gynecol. 2012;119:68–77. doi: 10.1097/AOG.0b013e31823d4006. [DOI] [PubMed] [Google Scholar]
- 20.Terplan M, Schluterman N, McNamara EJ, et al. Have racial disparities in ovarian cancer increased over time? An analysis of SEER data. Gynecol Oncol. 2012;125:19–24. doi: 10.1016/j.ygyno.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 21.Bristow RE, Powell MA, Al-Hammadi N, et al. Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. J Natl Cancer Inst. 2013;105:823–832. doi: 10.1093/jnci/djt065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Howell EA, Egorova N, Hayes MP, et al. Racial disparities in the treatment of advanced epithelial ovarian cancer. Obstet Gynecol. 2013;122:1025–1032. doi: 10.1097/AOG.0b013e3182a92011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dicicco-Bloom B, Crabtree BF. The qualitative research interview. Med Educ. 2006;40:314–321. doi: 10.1111/j.1365-2929.2006.02418.x. [DOI] [PubMed] [Google Scholar]
- 24. Green J, Thorogood N: Qualitative Methods for Health Research (ed 3). London, United Kingdom, Sage Publications, 2013. [Google Scholar]
- 25.Miles MB, Huberman AM, Saldana J: Qualitative Data Analysis: A Methods Sourcebook (ed 3). Thousand Oaks, CA, Sage Publications; 2013. [Google Scholar]
- 26.Quinn Patton M.Qualitative interviewing, in Laughton CD, Axelsen DE, Peterson K.Qualitative Research & Evaluation Methods (ed 3) Thousand Oaks, CA: Sage Publications; 2002339–428. [Google Scholar]
- 27. Saldaña J: The Coding Manual for Qualitative Researchers (ed 3). London, United Kingdom, Sage Publications, 2015. [Google Scholar]
- 28. Friese S: Qualitative Data Analysis With ATLAS.ti (ed 2). London, United Kingdom, Sage Publications, 2014. [Google Scholar]
- 29.Glaser BG. The constant comparative method of qualitative analysis. Soc Probl. 1965;12:436–445. [Google Scholar]
- 30.Bellinger JD, Millegan W, Abdalla AE. “I’m not ashamed to talk on it!”: African-American women’s decisions about cervical cancer prevention and control in South Carolina. Womens Health Issues. 2015;25:120–127. doi: 10.1016/j.whi.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 31.Brunstrom K, Murray A, McAllister M. Experiences of women who underwent predictive BRCA 1/2 mutation testing before the age of 30. J Genet Couns. 2016;25:90–100. doi: 10.1007/s10897-015-9845-5. [DOI] [PubMed] [Google Scholar]
- 32.Cox A, Faithfull S. Aiding a reassertion of self: A qualitative study of the views and experiences of women with ovarian cancer receiving long-term nurse-led telephone follow-up. Support Care Cancer. 2015;23:2357–2364. doi: 10.1007/s00520-014-2578-4. [DOI] [PubMed] [Google Scholar]
- 33.Curmi C, Peters K, Salamonson Y. Barriers to cervical cancer screening experienced by lesbian women: A qualitative study. J Clin Nurs. 2016;25:3643–3651. doi: 10.1111/jocn.12947. [DOI] [PubMed] [Google Scholar]
- 34.Wells AA, Shon EJ, McGowan K, et al. Perspectives of low-income African-American Women non-adherent to mammography screening: The importance of information, behavioral skills, and motivation. J Cancer Educ. 2017;32:328–334. doi: 10.1007/s13187-015-0947-4. [DOI] [PubMed] [Google Scholar]
- 35.Guest G, Bunce A, Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. 2006;18:59–82. [Google Scholar]
- 36.J Oncol Pract. 2009;5:315–317. doi: 10.1200/JOP.091015. ASCO announces new program designed to increase workforce diversity and reduce cancer care disparities. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Collins Y, Holcomb K, Chapman-Davis E, et al. Gynecologic cancer disparities: A report from the Health Disparities Taskforce of the Society of Gynecologic Oncology. Gynecol Oncol. 2014;133:353–361. doi: 10.1016/j.ygyno.2013.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Durant RW, Wenzel JA, Scarinci IC, et al. Perspectives on barriers and facilitators to minority recruitment for clinical trials among cancer center leaders, investigators, research staff, and referring clinicians: Enhancing minority participation in clinical trials (EMPaCT) Cancer. 2014;120(suppl 7):1097–1105. doi: 10.1002/cncr.28574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harris KM. How do patients choose physicians? Evidence from a national survey of enrollees in employment-related health plans. Health Serv Res. 2003;38:711–732. doi: 10.1111/1475-6773.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shalowitz DI, Vinograd AM, Giuntoli RL., II Geographic access to gynecologic cancer care in the United States. Gynecol Oncol. 2015;138:115–120. doi: 10.1016/j.ygyno.2015.04.025. [DOI] [PubMed] [Google Scholar]


