Abstract
Background
COVID-19 is spreading rapidly in India and other parts of the world. Despite the Indian Government's efforts to contain the disease in the affected districts, cases have been reported in 627 (98%) of 640 districts. There is a need to devise a tool for district-level planning and prioritisation and effective allocation of resources. Based on publicly available data, this study reports a vulnerability index for identification of vulnerable regions in India on the basis of population and infrastructural characteristics.
Methods
We computed a composite index of vulnerability at the state and district levels based on 15 indicators across the following five domains: socioeconomic, demographic, housing and hygiene, epidemiological, and health system. We used a percentile ranking method to compute both domain-specific and overall vulnerability and presented results spatially with number of positive COVID-19 cases in districts.
Findings
A number of districts in nine large states—Bihar, Madhya Pradesh, Telangana, Jharkhand, Uttar Pradesh, Maharashtra, West Bengal, Odisha, and Gujarat—located in every region of the country except the northeast, were found to have high overall vulnerability (index value more than 0·75). These states also had high vulnerability according to most of the five domains. Although our intention was not to predict the risk of infection for a district or a state, we observed similarities between vulnerability and the current concentration of COVID-19 cases at the state level. However, this relationship was not clear at the district level.
Interpretation
The vulnerability index presented in this paper identified a number of vulnerable districts in India, which currently do not have large numbers of COVID-19 cases but could be strongly impacted by the epidemic. Our index aims to help planners and policy makers effectively prioritise regions for resource allocation and adopt risk mitigation strategies for better preparedness and responses to the COVID-19 epidemic.
Funding
None.
Introduction
Widely believed to have originated in the Hubei province in China in November, 2019, COVID-19, the infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is spreading fast across the world and was declared a pandemic by WHO on March 11, 2020.1 As of July 5, 2020, the number of confirmed cases of COVID-19 worldwide stood at more than 11·2 million, with more than 529 000 deaths.2 213 countries and territories have reported confirmed cases of coronavirus. In India, the first case was reported on Jan 30, 2020, among a group of students who arrived in the southern state of Kerala from Wuhan, the epicentre of the outbreak at that time. As of July 5, 2020, in India, more than 648 300 confirmed cases have been reported, of which around 235 433 (36%) were active, 394 227 (61%) recovered, and 18 655 (3%) died.2 These cases were spread over 35 (97%) of 36 states and union territories and 627 (98%) of 640 districts of the country.
Walker and colleagues3 expressed concern about the spread of COVID-19 and its potential to cause more than 1·7 billion infections and 7·6 million deaths in south Asia alone if action is not taken. India is the world's second most populous country and the largest in south Asia, with a population of nearly 1·4 billion, therefore, it is at risk of having the largest share of these potential infections and deaths. Realising the gravity of the threat, the Indian Government put in place several measures, including stopping all international passenger flights (effective March 22, 2020), implementing a 40-day strict nationwide lockdown (from March 25, 2020), which was extended by 8 more weeks with some relaxation,4 steps towards boosting health infrastructure, and a large mass media campaign on the importance of social distancing and personal hygiene measures.
India faces the threat of a serious COVID-19 outbreak that would have far reaching consequences due to its large population but also for other reasons, including challenges in practicing social distancing, densely populated urban areas, non-universal access to water and soap for handwashing,5 a large number of people with chronic morbidities,6 a substantial proportion of the population living below the poverty line,7 and a large number of migrant workers who move from one state to another for their livelihoods.8 According to data from the Indian Government, more than 80% of confirmed cases in India are asymptomatic,9 making the population vulnerable to community spread of the virus. Although the epidemic appears to be concentrated in more affluent and industrialised districts,10 with millions of migrant workers from these areas moving to their home districts after the lockdown eased,11 it is only a matter of time before the virus spreads to the rural hinterlands of India. The question arises over whether these districts are ready for the virus and its consequences.
Research in context.
Evidence before this study
Application of social vulnerability indices in disaster management and identification of vulnerable people and regions are not novel. There have been several studies globally and a small number in India that proposed social vulnerability indices while tackling a climatic disaster. In the era of COVID-19, we found one study in the USA that developed a vulnerability index with specific application to COVID-19. In this study, by the Surgo Foundation, a COVID-19 community vulnerability index (CCVI) was computed by improvisation on the existing social vulnerability index used by the US Centers for Disease Control and Prevention by adding indicators relevant to the novel coronavirus pandemic. The index was calculated using US census track-level data for identification of vulnerable regions and to help prepare local-level responses and risk mitigation strategies. Although not a full-scale study, an editorial in The Lancet posed questions on so called one-size-fit-all strategies and recommended local-level planning based on specific vulnerabilities of population groups or regions. To understand and forecast the economic repercussions of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak, work has been done to measure an index of economic resilience of communities. We searched web-based coverage of the SARS-CoV-2 outbreak and PubMed and Google Scholar for peer reviewed publications on the outbreak and vulnerability indices published between Jan 1 and April 30, 2020. We used the search terms “Corona virus outbreak”, “Covid-19 vulnerability index”, “social vulnerability”, “economic vulnerability”, and “social distancing” separately and in combinations. We did not find any relevant literature on construction of a district-level vulnerability index in an Indian context that captured how vulnerable different regions are in their ability to mitigate and respond to the COVID-19 epidemic.
Added value of this study
To our knowledge, our study is the first to develop a composite measure of community-level vulnerability concerning the COVID-19 situation in India. We defined vulnerability through five domains that are important when preparing for, mitigating, and reducing the consequences of the coronavirus epidemic. Our operationalisation of the vulnerability index considered the risk of consequences of coronavirus infection to a population, rather than the risk of infection (or susceptibility) itself. The main value of our study is the state and district ranking provided to policy makers to prioritise resource allocation and devise effective mitigation and reconstruction strategies for affected populations. Although we applied our methods to states and districts of India, we believe that they can be used in other countries that are at different stages of the epidemic and have the required indicators available.
Implications of all the available evidence
To contain the outbreak of COVID-19, the Indian Government imposed a countrywide lockdown for 40 days initially, and extended this by 8 weeks with gradual relaxation. The government has started phased lifting of the lockdown restrictions by assessing the current situation based on the incidence of positive cases, the doubling rate, and several other factors. Our findings could help the government identify the regions that might have potential severe consequences of the COVID-19 outbreak, which is particularly important because of the risk of reintroduction of the virus posed by millions of returnee migrant workers. Both the domain-specific and overall vulnerability index will help prioritise resource allocation in the face of constrained resources during the epidemic.
To control the epidemic, the Indian Government has enacted the National Disaster Management Act (2005),12 equating the COVID-19 epidemic to a national disaster, laying down the policies, plans, and guidelines for management of the epidemic and ensuring a timely and effective response to the disaster, for example, nature of lockdown measures, disease containment plans, guidelines on social distancing, testing strategies, and contact tracing and isolation strategies. Centrally coordinated local-level planning is essential for mitigating both the short-term and long-term devastating effects of the epidemic on economic, health, and social wellbeing in the affected areas and their populations.
In disaster management, risk is often described as a function of hazard and vulnerability, where risk is defined as the ability of a population to absorb and ultimately recover from the effects of a hazard, that is, the exposure to an event that might present a grave threat to its people and economy, given the level of vulnerability of the population and the resources they have to mitigate the hazard.13 Mathematically, risk is often expressed as hazard × (vulnerability – resources).
Although disaster management deals mostly with physical hazards, the vulnerability of a population is frequently considered in the literature to mean their geographical location or other physical vulnerabilities, rather than their social vulnerability. The manner in which hazards might affect the population must be of foremost importance, but understanding how and where vulnerable communities might be impacted can greatly help with effective allocation of resources during the different disaster management phases—prevention, preparedness, response, mitigation, recovery, and reconstruction.
Vulnerability in the era of COVID-19 is more than the risk of contracting the disease. As articulated in The Lancet,14 vulnerability in the present context is a dynamic concept—a person or a group might not be vulnerable at the beginning of the pandemic, but could subsequently become vulnerable depending on the government response. Beyond the groups who are epidemiologically vulnerable to COVID-19 (eg, older people and individuals with comorbidities), there might be people from diverse socioeconomic backgrounds who are vulnerable as they struggle to cope with the crisis in various ways—financially, mentally, or even physically.14 Thus, to appropriately respond to and manage the COVID-19 pandemic, knowledge and understanding of social and other community vulnerabilities is critical. The most vulnerable communities could be those who are at the receiving end of short-term and long-term effects of the pandemic, but whose needs might not have been sufficiently considered in the planning of local responses and relief.
The concept of using vulnerability indices in times of disaster is not novel. The US Centers for Disease Control and Prevention (CDC) uses a social vulnerability index to measure the resilience of communities when faced with natural or manmade disasters. Globally, several studies have proposed variations of social vulnerability indices for use mostly in the context of disaster management, and only a small number for management of pandemics.15 A recent review by Fatemi and colleagues16 provided an extensive account of such studies. In India, little literature is available on use of social vulnerability indices, and mostly in relation to disastrous climatic events.17, 18 Our study attempts to fill the gap in the literature on social vulnerability indices in India.
In this context, we attempted to provide a tool for district-level planning and responses to the COVID-19 epidemic in India. We computed a set of indices to rank each district of India under five domains—socioeconomic, demographic, hygiene, health system, and epidemiological—which make them vulnerable to a natural disaster in general, as well as the COVID-19 epidemic.
Methods
Study design
Although social, demographic, economic, health, and epidemiological data are available in India, district-level data are scarce. We used the following data sources in this paper, as these indicators are available at the district level from these sources: National Family Health Survey 2015–16,6 Census of India 2011,19 Rural Health Statistics 2018,20 and National Health Profile 2019.21
We used similar methodology to that developed by Flanagan and colleagues,22 used by the CDC to compute social vulnerability indices for each census track in the USA. Flanagan's social vulnerability index includes four domains—socioeconomic status (comprising income, poverty, employment, and education variables), household composition and disability (comprising age, single parenting, and disability variables), minority status and language (comprising race, ethnicity, and English language proficiency variables), and housing and transportation (comprising housing structure, crowding, and vehicle access variables). We expanded the concept and computed vulnerability under different thematic domains, extending beyond social vulnerability to accommodate vulnerability related to the COVID-19 pandemic.
We considered the following five domains, which are important in the context of the COVID-19 epidemic in India, particularly for management and mitigation of COVID-19 infection in the community: socioeconomic condition, demographic composition, housing and hygiene condition, availability of health-care facilities, and COVID-19-related epidemiological factors (table 1 ). Details of the rationale for including each domain in the vulnerability index are described in the appendix (pp 1–3).
Table 1.
Domains of vulnerability and variables within
| Variable description | Source | |
|---|---|---|
| Socioeconomic | ||
| Scheduled tribe or caste households | Calculated as proportion of households belonging to scheduled caste or tribe | National Family Health Survey-4 (Household file), India (2015–16)6 |
| Education level in population | Calculated as proportion of population who completed secondary or higher level of education | National Family Health Survey-4 (Person file), India (2015–16)6 |
| Poor households | An asset deprivation indicator was computed as the proportion of households that did not have any of the following: a motorised vehicle (a two-wheeler, car or truck, or tractor), television, computer, bicycle, refrigerator, thresher, or air-conditioner or cooler | National Family Health Survey-4 (Household file), India (2015–16)6 |
| Demographic | ||
| Elderly population | Calculated as proportion of individuals in the population aged 60 years or older | National Family Health Survey-4 (Person file), India (2015–16)6 |
| Urbanisation | Calculated as proportion of urban households among all households | National Family Health Survey-4 (Household file), India (2015–16)6 |
| Population density | Calculated as a ratio of population of a unit (district or state) and its area in km2 | Area data: 2011 census;19 population data: linearly projected population for 2019 using growth rate calculated for each district based on 2001 and 2011 census |
| Housing and hygiene condition | ||
| People per room | Calculated as the mean number of people residing per room used for sleeping in a household | National Family Health Survey-4 (Household file), India (2015–16)6 |
| Households with no toilet facility | Calculated as proportion of households reporting no availability of toilet facility within premises | National Family Health Survey-4 (Household file), India (2015–16)6 |
| Households with no hand-hygiene facility | Calculated as percent households with no availability of water and soap or detergent at place of handwashing | National Family Health Survey-4 (Household file), India (2015–16)6 |
| Availability of health care | ||
| Households with health insurance | Calculated as proportion of households with at least one member covered under any health insurance scheme | National Family Health Survey-4 (Household file), India (2015–16)6 |
| Households without easy access to public health facility | Calculated as proportion of households reported having no nearby public health facility | National Family Health Survey-4 (Household file), India (2015–16)6 |
| Availability of public hospitals (at district level) | Calculated as number of public hospitals (primary health centre and above) per 100 000 population | Rural health statistics 2018 and linearly projected population for 2019 using growth rate calculated for each district based on 2001 and 2011 census20 |
| Availability of hospital beds (at state level) | Calculated as number of public or private hospital beds per 1000 population | National health profile 201921 |
| Epidemiological | ||
| Men with any chronic morbidity | Calculated as proportion of men aged 40–54 years with chronic health conditions, such as cardiovascular disease, diabetes, asthma, or cancer | National Family Health Survey-4 (Men's file), 2015–166 |
| Men who smoke | Calculated as proportion of men who smoke tobacco | National Family Health Survey-4 (Men's file), 2015–166 |
| Women with any chronic morbidity | Calculated as proportion of women aged 40–49 years with chronic health conditions, such as cardiovascular disease, diabetes, asthma, or cancer | National Family Health Survey-4 (Women's file), 2015–166 |
Socioeconomic vulnerability
The social and economic repercussions of the COVID-19 epidemic might be far reaching and will be felt long after it is over. Epidemic-induced economic shock will be felt mostly by the poorest section of society,23 hence it is important to consider the socioeconomic condition of a population when creating a vulnerability index. We used the following three indicators to define socioeconomic vulnerability: the proportion of the population belonging to scheduled castes and tribes (to represent socially marginalised groups in India), the proportion of the population with secondary or higher education (to represent education level in the population), and the proportion of the population who did not have any of certain assets (motorised vehicle, television, computer, bicycle, refrigerator, thresher, and air conditioner or cooler) as a proxy for poverty.
Demographic vulnerability
The nature of the COVID-19 epidemic is such that both the pace of transmission and mortality due to infection depend on the demographic composition of the population, hence demography should be part of a vulnerability index. We considered the following three indicators to represent the demographic composition of a population in the context of COVID-19: the proportion of the population aged 60 years and older, the proportion of the population living in urban areas, and population density.
Housing and hygiene conditions
Housing conditions, particularly intrahousehold crowding, sanitation, and hand hygiene, are important factors in COVID-19 transmission and thus constitute an important domain of vulnerability. We considered the following three indicators for this purpose: the mean number of people sharing a room in a household for sleeping, the proportion of households having their own toilet, and the proportion of households having soap and water available for handwashing.
Availability of health care
The management of an epidemic and the treatment seeking ability of a population depend on easy and affordable access to well capacitated health-care systems and health security, and thus should be included in the vulnerability index. We chose the following three variables to represent health security, accessibility of affordable health care and health-care system capacity: the proportion of households with health insurance, the proportion of households who reported no nearby public health facility, and the number of public hospitals per 100 000 population (for district level) and number of hospital beds per 1000 population (for state or union territory level).
Epidemiological factors
There are several known epidemiological factors that might put a population at risk of higher morbidity and mortality by COVID-19 infection and thus merit inclusion in the vulnerability index. Because of the paucity of data on the prevalence of comorbidities in older people (aged 60 years and over) we captured epidemiological factors through the following three variables: the proportion of men (aged 40–54 years) and women (aged 40–49 years) who reported having any of cardiovascular disease, diabetes, asthma, or cancer, and the proportion of men who smoked tobacco.
Construction of the vulnerability index
15 indicators were used to define vulnerability across five domains at both the district and state level. First, each of these indicators were computed from the respective data sources to arrive at district-level indicators. The mean of all the districts in a state was then computed to arrive at state-level indicators.
Within the district (or state) datafile, each indicator was arranged in increasing or decreasing order of prevalence in such a way that the higher the value of the indicator the higher the vulnerability. Ranks were then assigned to districts (or states). In case of ties, the lowest rank value in the string of ties was assigned to each tied case. After assigning a rank to the district (or state) the percentile rank was calculated. The percentile rank was the percentage of districts (or states) at or below that rank score. The following formula was used to calculate the percentile rank of each indicator for each district or state: P=(rank – 1)/(N – 1), where P is the percentile rank and N is the total number of districts or states.
A higher percentile rank denoted greater relative vulnerability, with 1·0 being the most vulnerable and 0·0 being the least vulnerable. The relative vulnerability of any district or state was estimated by calculating the percentile rank at three stages—first at the indicator level, then the domain level by summing the percentile ranks of all indicators constituting the domain, and finally at the overall level by summing the percentile ranks of all five domains. In absence of a rationale for using any weighting scheme, equal weights were assigned to each indicator for calculating domain vulnerability. Similarly, equal weights were given to each domain at the time of calculating the overall vulnerability index. This method is the same as that used by Flanagan and colleagues22 for calculating the social vulnerability index.
We computed the vulnerability index for both states and union territories and districts of India separately. At the time of the 2011 census, India had 640 districts in 29 states and six union territories.17 In 2014, the state of Andhra Pradesh was divided into two states—Andhra Pradesh and Telangana—meaning there were now 30 states and six union territories. Although there are currently 736 districts in India because large districts have been split into new districts for ease of administration, since the data required for this paper were not available for the newly defined districts, we considered only the 640 districts that had administrative boundaries defined in the 2011 census. To measure reliability of the index, we computed Chronbach's α for the overall vulnerability index. We also computed Pearson's correlation between domain vulnerability indices and overall vulnerability index. All analyses were done using Stata version 16.0.
We generated choropleth maps at district and state levels to show the spatial distribution of domain-specific and overall vulnerability. The number of COVID-19 cases (as of June 17, 2020) in each district was plotted over these maps to show the spatial distribution of confirmed coronavirus cases in contrast to their relative vulnerability. 2011 census shape files at district and state levels were used and the Stata spmap command was implemented to construct the maps.
Role of the funding source
There was no funding source for this study. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
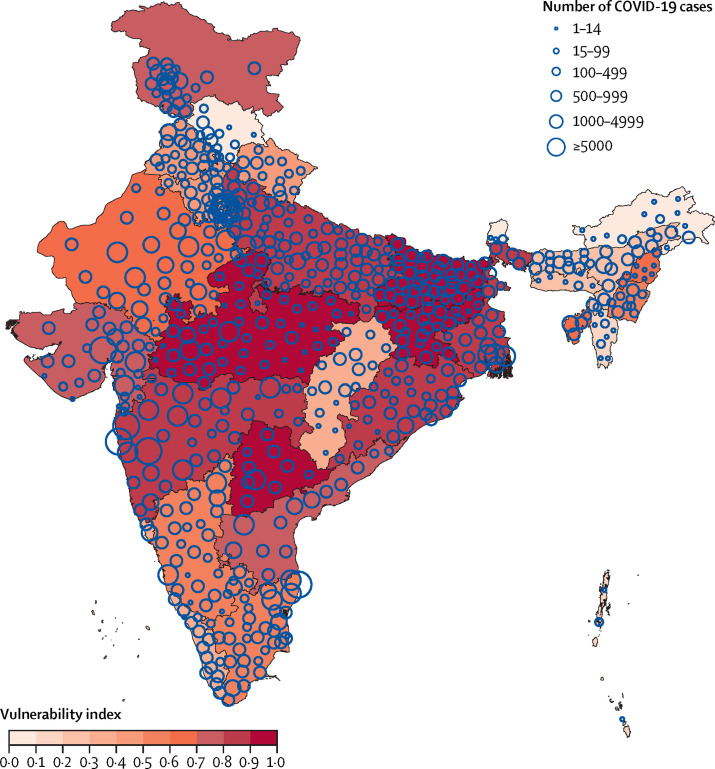
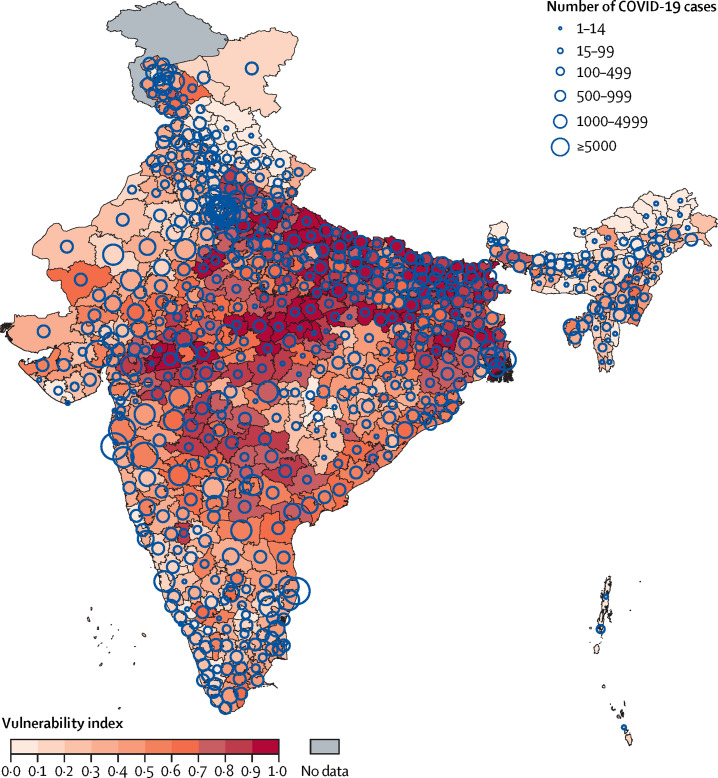
We computed vulnerability indices for 30 Indian states, six union territories, and 640 districts (Table 2, Table 3, Table 4 ; appendix pp 14–23). For brevity, only the 20 districts each with lowest and highest vulnerability in the country are presented in Table 3, Table 4. Data for all 640 districts are presented in the appendix (pp 14–23). We also mapped state-level and district-level overall vulnerability (Figure 1, Figure 2 ) and individual domain vulnerability (appendix pp 4–13). Reliability of the overall vulnerability index (Chronbach's α) computed from five domain vulnerability indices was 0·6. Our findings showed patterns of different vulnerabilities across the country.
Table 2.
Domain-wise and overall COVID-19 vulnerability index by state (in order of increasing overall vulnerability)
| Socioeconomic vulnerability | Demographic vulnerability | Vulnerability due to housing and hygiene condition | Vulnerability due to non-availability of health care | Epidemiological vulnerability | Overall vulnerability | |
|---|---|---|---|---|---|---|
| Sikkim | 0·457 | 0·086 | 0·000 | 0·029 | 0·029 | 0·000 |
| Arunachal Pradesh | 0·971 | 0·000 | 0·371 | 0·057 | 0·114 | 0·029 |
| Himachal Pradesh | 0·314 | 0·257 | 0·486 | 0·229 | 0·229 | 0·057 |
| Chandigarh | 0·086 | 0·943 | 0·143 | 0·286 | 0·314 | 0·086 |
| Daman and Diu | 0·143 | 0·800 | 0·429 | 0·429 | 0·000 | 0·114 |
| Andaman and Nicobar Islands | 0·257 | 0·057 | 0·200 | 0·314 | 1·000 | 0·143 |
| Mizoram | 0·714 | 0·257 | 0·229 | 0·000 | 0·629 | 0·143 |
| Puducherry | 0·029 | 0·943 | 0·286 | 0·114 | 0·743 | 0·200 |
| Lakshadweep | 0·286 | 1·000 | 0·029 | 0·229 | 0·571 | 0·200 |
| Assam | 0·486 | 0·114 | 0·457 | 0·743 | 0·371 | 0·257 |
| Meghalaya | 1·000 | 0·000 | 0·086 | 0·143 | 0·971 | 0·286 |
| Chhattisgarh | 0·657 | 0·114 | 0·857 | 0·457 | 0·143 | 0·314 |
| Kerala | 0·000 | 0·914 | 0·057 | 0·371 | 0·886 | 0·314 |
| Goa | 0·057 | 0·886 | 0·229 | 0·514 | 0·543 | 0·314 |
| Haryana | 0·200 | 0·600 | 0·400 | 0·914 | 0·143 | 0·400 |
| Punjab | 0·229 | 0·857 | 0·171 | 0·800 | 0·257 | 0·429 |
| Uttarakhand | 0·343 | 0·514 | 0·486 | 0·600 | 0·371 | 0·429 |
| Dadra and Nagar Haveli | 0·714 | 0·543 | 0·857 | 0·171 | 0·086 | 0·486 |
| Delhi | 0·114 | 0·743 | 0·343 | 0·543 | 0·743 | 0·514 |
| Manipur | 0·714 | 0·200 | 0·314 | 0·686 | 0·714 | 0·543 |
| Tamil Nadu | 0·171 | 0·771 | 0·657 | 0·200 | 0·857 | 0·571 |
| Karnataka | 0·429 | 0·657 | 0·743 | 0·486 | 0·343 | 0·571 |
| Tripura | 0·829 | 0·314 | 0·543 | 0·057 | 0·943 | 0·629 |
| Nagaland | 0·943 | 0·429 | 0·114 | 0·771 | 0·457 | 0·657 |
| Rajasthan | 0·886 | 0·371 | 0·857 | 0·629 | 0·057 | 0·686 |
| Jammu and Kashmir | 0·629 | 0·171 | 0·571 | 0·686 | 0·829 | 0·714 |
| Andhra Pradesh | 0·343 | 0·629 | 0·686 | 0·571 | 0·657 | 0·714 |
| Gujarat | 0·543 | 0·571 | 0·800 | 0·800 | 0·286 | 0·771 |
| Odisha | 0·686 | 0·343 | 0·971 | 0·371 | 0·657 | 0·800 |
| Maharashtra | 0·400 | 0·800 | 0·600 | 0·886 | 0·429 | 0·829 |
| West Bengal | 0·486 | 0·686 | 0·714 | 0·314 | 0·914 | 0·829 |
| Uttar Pradesh | 0·571 | 0·457 | 0·771 | 0·971 | 0·514 | 0·886 |
| Jharkhand | 0·857 | 0·371 | 0·943 | 0·943 | 0·200 | 0·914 |
| Telangana | 0·571 | 0·714 | 0·629 | 0·657 | 0·800 | 0·943 |
| Bihar | 0·714 | 0·486 | 0·800 | 0·971 | 0·486 | 0·971 |
| Madhya Pradesh | 0·886 | 0·200 | 0·971 | 0·857 | 0·600 | 1·000 |
Table 3.
Domain-wise and overall COVID-19 vulnerability index by district (20 least vulnerable districts)
| District | Socioeconomic vulnerability | Demographic vulnerability | Vulnerability due to housing and hygiene condition | Vulnerability due to non-availability of health care | Epidemiological vulnerability | Overall vulnerability | |
|---|---|---|---|---|---|---|---|
| Sikkim | South district | 0·311 | 0·103 | 0·000 | 0·063 | 0·009 | 0·000 |
| Sikkim | North district | 0·642 | 0·008 | 0·003 | 0·036 | 0·034 | 0·002 |
| Sikkim | West district | 0·628 | 0·033 | 0·000 | 0·064 | 0·116 | 0·003 |
| Assam | Jorhat | 0·059 | 0·302 | 0·155 | 0·252 | 0·164 | 0·005 |
| Himachal Pradesh | Kangra | 0·039 | 0·357 | 0·210 | 0·180 | 0·166 | 0·006 |
| Uttarakhand | Rudraprayag | 0·297 | 0·224 | 0·185 | 0·260 | 0·033 | 0·008 |
| Arunachal Pradesh | Dibang valley | 0·876 | 0·094 | 0·017 | 0·025 | 0·063 | 0·009 |
| Arunachal Pradesh | Lower Subansiri | 0·775 | 0·025 | 0·097 | 0·011 | 0·172 | 0·011 |
| Himachal Pradesh | Lahul and Spiti | 0·601 | 0·186 | 0·219 | 0·066 | 0·023 | 0·013 |
| Himachal Pradesh | Shimla | 0·153 | 0·433 | 0·228 | 0·042 | 0·286 | 0·014 |
| Arunachal Pradesh | West Siang | 0·753 | 0·053 | 0·014 | 0·005 | 0·326 | 0·016 |
| Arunachal Pradesh | Upper Siang | 0·847 | 0·049 | 0·105 | 0·003 | 0·166 | 0·017 |
| Himachal Pradesh | Mandi | 0·258 | 0·377 | 0·280 | 0·049 | 0·216 | 0·019 |
| Assam | Golaghat | 0·127 | 0·080 | 0·171 | 0·462 | 0·354 | 0·020 |
| Assam | Nalbari | 0·111 | 0·227 | 0·045 | 0·235 | 0·576 | 0·022 |
| Himachal Pradesh | Chamba | 0·560 | 0·138 | 0·360 | 0·039 | 0·103 | 0·023 |
| Jammu and Kashmir | Baramula | 0·261 | 0·189 | 0·039 | 0·383 | 0·338 | 0·025 |
| Arunachal Pradesh | East Siang | 0·520 | 0·116 | 0·088 | 0·000 | 0·562 | 0·027 |
| Haryana | Panchkula | 0·013 | 0·814 | 0·078 | 0·391 | 0·008 | 0·028 |
| Arunachal Pradesh | Kurung Kumey | 0·995 | 0·002 | 0·282 | 0·009 | 0·019 | 0·030 |
Table 4.
Domain-wise and overall COVID-19 vulnerability index by district (20 most vulnerable districts)
| District | Socioeconomic vulnerability | Demographic vulnerability | Vulnerability due to housing and hygiene condition | Vulnerability due to non-availability of health care | Epidemiological vulnerability | Overall vulnerability | |
|---|---|---|---|---|---|---|---|
| Madhya Pradesh | Satna | 0·679 | 0·568 | 0·792 | 0·612 | 0·987 | 0·970 |
| Bihar | Khagaria | 0·732 | 0·368 | 0·879 | 0·926 | 0·739 | 0·972 |
| Rajasthan | Karauli | 0·942 | 0·383 | 0·964 | 0·435 | 0·926 | 0·973 |
| Uttar Pradesh | Sant Kabir Nagar | 0·656 | 0·391 | 0·818 | 0·886 | 0·919 | 0·975 |
| Uttar Pradesh | Chitrakoot | 0·803 | 0·272 | 0·997 | 0·892 | 0·726 | 0·977 |
| Bihar | Munger | 0·513 | 0·923 | 0·646 | 0·801 | 0·814 | 0·978 |
| Uttar Pradesh | Hardoi | 0·793 | 0·336 | 0·834 | 0·936 | 0·804 | 0·980 |
| Uttar Pradesh | Bara Banki | 0·759 | 0·311 | 0·870 | 0·950 | 0·826 | 0·981 |
| Madhya Pradesh | Alirajpur | 0·992 | 0·036 | 0·989 | 0·743 | 0·959 | 0·983 |
| Madhya Pradesh | Sagar | 0·765 | 0·344 | 0·837 | 0·793 | 0·981 | 0·984 |
| Jharkhand | Deoghar | 0·618 | 0·620 | 0·937 | 0·959 | 0·615 | 0·986 |
| Uttar Pradesh | Balrampur | 0·681 | 0·293 | 0·890 | 0·967 | 0·928 | 0·987 |
| Bihar | Saharsa | 0·740 | 0·457 | 0·917 | 0·867 | 0·793 | 0·989 |
| Bihar | Vaishali | 0·706 | 0·635 | 0·681 | 0·790 | 0·977 | 0·991 |
| Madhya Pradesh | Jhabua | 0·998 | 0·061 | 0·995 | 0·798 | 0·978 | 0·992 |
| Bihar | Sheohar | 0·862 | 0·689 | 0·781 | 0·823 | 0·759 | 0·994 |
| Bihar | Saran | 0·603 | 0·704 | 0·761 | 0·930 | 0·920 | 0·995 |
| Bihar | Samastipur | 0·820 | 0·448 | 0·870 | 0·905 | 0·878 | 0·997 |
| Uttar Pradesh | Sitapur | 0·806 | 0·372 | 0·879 | 0·973 | 0·944 | 0·998 |
| Bihar | Darbhanga | 0·879 | 0·588 | 0·903 | 0·833 | 0·800 | 1·000 |
Figure 1.
Overall COVID-19 vulnerability index in states and union territories of India and number of confirmed cases as of June 17, 2020
This map does not reflect changes made in Jammu and Kashmir state (now union territory) in August, 2019.
Figure 2.
Overall COVID-19 vulnerability index in districts of India and number of confirmed cases as of June 17, 2020
This map does not reflect changes made in Jammu and Kashmir state (now union territory) in August, 2019.
Nine states with an overall vulnerability index more than 0·75 mostly ran through the centre of the country, from West Bengal in the east to Gujarat in the west, covering Bihar, Odisha, Jharkhand, Uttar Pradesh, Madhya Pradesh, Telangana, and Maharashtra (table 2, figure 1). These nine states represent most regions of the country, except for the northeast. Most of these states have high vulnerability according to several individual domains. As many as 14 states and union territories had a vulnerability index lower than 0·4, one from the north (Himachal Pradesh), five union territories (Chandigarh, Daman and Diu, Andaman and Nicobar Islands, Puducherry, and Lakshadweep), five from the northeast region (Sikkim, Arunachal Pradesh, Mizoram, Assam, and Meghalaya), one from the west (Goa), one from the south (Kerala), and Chhattisgarh from the central region.
Although our intention was not to predict the risk of infection for a district or a state, we observed similarities between vulnerability and the current concentration of COVID-19 cases at the state level (figure 1). As of June 17, 2020, there are eight states in India that have contributed to over 80% of the confirmed COVID-19 cases in the country—Maharashtra (115 650 [33%]), Delhi (50 278 [14%]), Tamil Nadu (47 366 [13%]), Gujarat (25 577 [5%]), Rajasthan (16 799 [7%]), Uttar Pradesh (14 229 [4%]) West Bengal (12 127 [3%]), and Madhya Pradesh (10 751 [3%]). Of these eight states, five states had a high overall vulnerability index value (ranging from 0·771 to 1·000) and the remaining three had medium vulnerability (ranging from 0·514 to 0·686; table 2).
We recorded the districts with confirmed cases of coronavirus infection as of June 17, 2020, and their relative overall vulnerability, which did not always align with each other (figure 2). For example, the districts of Delhi and Haryana were among those with low overall vulnerability, but currently have concentrated clusters of infections. When further investigating the domain-specific vulnerability in these districts, we observed an increased level of vulnerability due to demographic and epidemiological factors in many of these districts. Furthermore, Delhi is a national and international transport hub and is thus highly susceptible to importation of positive cases from outside the state.
Domain vulnerability indices also revealed different patterns. Several states and union territories that had very low overall vulnerability (eg, Daman and Diu, Chandigarh, Puducherry, Lakshadweep, Goa, and Kerala) have high vulnerability in terms of their demography (index value ranged from 0·800 to 1·000; table 2). Similarly, if we consider district-level vulnerability, Mumbai had low overall vulnerability (0·394) but high vulnerability in terms of demographic (0·951) and epidemiological (0·609) factors (appendix p 17). As of June 17, 2020, Mumbai has reported around 17% (61 665 cases) of all confirmed COVID-19 cases in India.
Among the five domains, housing and hygiene condition and availability of health-care facility correlated most strongly with overall vulnerability (R values of 0·70 and 0·68, respectively), followed by socioeconomic factors (R=0·41) and epidemiological factors (R=0·39). However, demographic factors had low correlation with overall vulnerability (appendix p 23).
Most of the northeast, much of the south and western parts of India, and the hilly region of the north were found to have relatively low vulnerability compared with districts from the north, east, and central regions of the country (figure 2; appendix pp 14–23).
Discussion
Mitigation efforts to contain the COVID-19 epidemic and manage24 its far-reaching consequences need effective planning25 and require the right kind of data. In this study, we report a state-level and district-level vulnerability index that is designed to aid government efforts to effectively respond to the fast-developing COVID-19 epidemic in India. These data are meant to be used by planners to target vulnerable populations and support them to prepare for, and to mitigate and reduce, health and socioeconomic consequences of COVID-19.
The results of our study show that districts in nine of 30 large states—Bihar, Madhya Pradesh, Telangana, Jharkhand, Uttar Pradesh, Maharashtra, West Bengal, Odisha, and Gujarat—have high overall vulnerability. These states also have high vulnerability according to many of the five domains that we considered. Districts in nine states and five union territories have relatively low vulnerability, and states in the northeast dominate those with low vulnerability.
With no vaccine or effective treatment available, some form of the epidemic will continue to affect life across the world, including having a severe impact on the economy. In India, after a steady beginning the epidemic has more recently shown exponential growth. Thus, the country is dealing with a large increase in new cases over a short period of time. During the 6 week period beginning on May 2, 2020, the number of districts with confirmed cases increased from 359 (or 56% of all districts) to 627 (98% of all districts).
India has a huge number of low wage workers who move around the country. Because of a halt in almost all economic activities during national lockdown, the country is seeing millions of these migrant workers returning to their origin districts as lockdown restrictions are eased. In the first 3 weeks of May, Indian railways alone ferried around 4 million migrant workers to their states of origin.26 Most of these people travelled to Uttar Pradesh and Bihar, followed by Madhya Pradesh, Punjab, Rajasthan, Uttarakhand, Jammu and Kashmir, and West Bengal and, indeed, we observed that these are some of most vulnerable states according to the vulnerability indices. Another important issue is that most of these migrant workers are returning from states with a high burden (in terms of active cases; eg, Delhi, Maharashtra, Tamil Nadu, Gujarat, Andhra Pradesh, and Kerala) to lower-burden but highly vulnerable districts in their own states, possibly carrying back infections. Our vulnerability index and data on migration might help local authorities prepare for and better mitigate the increasing threat of virus spreading in their districts.
The domain-specific and overall vulnerability index presented here can also be combined with other available information, such as disease transmission, case fatality rate, the proportion of cases needing hospitalisation, intensive care unit admissions, or ventilator support to heighten the preparedness of a district or state, as well as planning and executing the response.
Several aspects of the vulnerability index should be discussed. First, there is an apparent conflation between the concepts of susceptibility and vulnerability. In the context of COVID-19, susceptibility means the risks of getting infected by the virus, which are determined by several epidemiological factors, individual hygiene practices, and the ability to maintain physical distance from others. By contrast, vulnerability means the risk of consequences of infection, including spread, morbidity and mortality, and social and economic consequences. Our vulnerability index includes demographic indicators that might represent both susceptibility and vulnerability. For example, although a dense urban area is susceptible to COVID-19 infection, older people who live in that population are vulnerable to severe mortality and morbidity. Second, being based on ranking of districts (or states) for 15 indicators, our vulnerability index provides a relative position of a district (or a state) compared with other districts (or states) in the country, rather than being an absolute score. We believe that an absolute vulnerability score is less useful to planners and managers of an epidemic than a relative index, as they need to allocate available resources on a priority basis. Third, the vulnerability index proposed in this study is simple and additive and has a reliability of 0·6 (Chronbach's α). However, we were unable to test the external validity of our vulnerability index as there is no known measure of comparison. Fourth, our index uses equal weights to combine individual indicators and domains, but researchers have argued that all the domains are not equally important and hence should not be given equal weight. However, alternatives such as using factor weights (based on an exploratory factor analysis of components) are problematic as they are sensitive to data and do not have easy interpretability. A simple equally weighted index is easy to comprehend, interpret, and replicate. Finally, although overall vulnerability is a handy summary, we recommend the use of an overall index alongside domain-specific vulnerability indices. For example, while planning to protect older citizens from infection, a demographic vulnerability index should be used to identify priority regions. Often, overall vulnerability masks the domain-specific vulnerability of a population, and users of our index should be mindful of this.
Despite the usefulness of the index, there are some limitations. Ideally, it would be possible to calculate the index at a sub-district level. However, several important variables used to define vulnerability were not available at a sub-district level. Hence, this analysis is restricted to the district level. Furthermore, at present, major planning and financing of the Indian Government response to the epidemic is concentrated at the state and district levels, meaning it makes sense to provide vulnerability data to these policy makers at district and state levels. Finally, data used in this study are 2–5 years old and might not have captured vulnerability well in districts in which rapid changes have occurred up to the present day.
In conclusion, the vulnerability indices reported in this study are intended to spatially identify vulnerable regions in India according to five different domains of vulnerability and help the community prepare for, mitigate, respond to, and recover from the epidemic. The fact that we were unable to study sub-district data to provide results for small-area planning calls for an overhaul of India's data ecosystem. We recommend a national micro-level data framework for effective management of such disasters in the future.
This online publication has been corrected. The corrected version first appeared at thelancet.com/lancetgh on Aug 19, 2020
Data sharing
We used publicly available data and have referenced the sources in the paper.
Acknowledgments
Acknowledgments
We are grateful to Niranjan Saggurti and Arupendra Mozumdar and anonymous referees for their helpful comments on an earlier draft.
Editorial note: the Lancet Group takes a neutral position with respect to territorial claims in published maps and tables.
Contributors
RA conceptualised the manuscript. AP and RA did the literature search, collected data from public sources, and did all statistical analyses. RA mainly wrote the manuscript with contributions from AP. Both authors reviewed the manuscript and RA finalised it.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.WHO Rolling updates on coronavirus disease. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
- 2.Johns Hopkins Center for Systems Science and Engineering Coronavirus resource center: COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) https://coronavirus.jhu.edu/map.html
- 3.Walker P, Whittaker C, Watser O. The global impact of COVID-19 and strategies for mitigation and suppression. March 26, 2020. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-Global-Impact-26-03-2020.pdf
- 4.Government of India Ministry of Information and Broadcasting. India's response to COVID outbreak. https://pib.gov.in/PressReleasePage.aspx?PRID=1608727
- 5.Khan MI, Abraham A. No ‘room’ for social distancing: a look at India's housing and sanitation conditions. Econ Polit Wkly. 2020;55 [Google Scholar]
- 6.International Institute for Population Sciences and ICF . IIPS; Mumbai: 2017. National Family Health Survey (NFHS-4), 2015–16: India. [Google Scholar]
- 7.Government of India Ministry of Social Justice and Empowerment. State-wise percentage of population below poverty line by social groups, 2004–05. http://socialjustice.nic.in/UserView/index?mid=76672
- 8.Tumbe C. A million migrations: journeys in search of jobs. Livemint. Jan 17, 2019. https://www.livemint.com/Politics/8WPPsZygqR7Mu6e3Fgy55N/A-million-migrations-Journeys-in-search-of-jobs.html
- 9.Reddy KS. India's high number of asymptomatic cases worrying, and herd immunity is far off. The Print. April 24, 2020. https://theprint.in/opinion/indias-high-number-of-asymptomatic-cases-worrying-and-herd-immunity-is-far-off/407931/
- 10.Bhatia S, Devulapalli S. Mapped: the spread of coronavirus across India's districts. Livemint. April 19, 2020. https://www.livemint.com/news/india/mapped-the-spread-of-coronavirus-across-india-s-districts-11587179250870.html
- 11.Chatterjee P, Dey S, Jain S. Lives and livelihood: an exit strategy from lockdown for India. SSRN. 2020 doi: 10.2139/ssrn.3582497. published online April 18. (preprint) [DOI] [Google Scholar]
- 12.Ministry of Law and Justice The Disaster Management Act. 2005. https://www.ndmindia.nic.in/images/The%20Disaster%20Management%20Act,%202005.pdf
- 13.Dwyer A, Zoppou C, Nielsen O, Day S, Roberts S. Commonwealth of Australia; Canberra: 2004. Quantifying social vulnerability: a methodology for identifying those at risk to natural hazards. [Google Scholar]
- 14.The Lancet Redefining vulnerability in the era of COVID-19. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Handel MM, Rose CE, Hallisey EJ. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. J Acquir Immune Defic Syndr. 2016;73:323–331. doi: 10.1097/QAI.0000000000001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fatemi F, Ardalan A, Aguirre B, Mansouri N, Mohammadfam I. Social vulnerability indicators in disasters: findings from a systematic review. Int J Disaster Risk Reduct. 2017;22:219–227. [Google Scholar]
- 17.Vittal H, Karmakar S. In: Climate change signals and response. Venkataraman C, Mishra T, Ghosh S, Karmakar S, editors. Springer Singapore; Singapore: 2019. A comprehensive social vulnerability analysis at a national scale; pp. 163–176. [Google Scholar]
- 18.Kumar D, Bhattacharjya RK. Study of integrated social vulnerability index SoVIint of Hilly Region of Uttarakhand, India. Environ Clim Technol. 2020;24:105–122. [Google Scholar]
- 19.Office of the Registrar General & Census Commissioner, India 2011 Census data. http://censusindia.gov.in/2011-Common/CensusData2011.html
- 20.Government of India Open government data platform. Rural health statistics. https://data.gov.in/dataset-group-name/rural-health-statistics
- 21.Central Bureau of Health Intelligence. Ministry of Health and Family Welfare 2019 National Health Profile. New Delhi. Government of India. https://www.cbhidghs.nic.in/showfile.php?lid=1147
- 22.Flanagan B, Gregory E, Hallisey E, Heitgerd J, Lewis B. A social vulnerability index for disaster management. J Homel Secur Emerg Manag. 2011;8 [Google Scholar]
- 23.UNDP . United Nations Development Programme; Bangkok: 2020. The social and economic impact of COVID-19 in the Asia-Pacific region. Position note prepared by UNDP regional bureau for Asia and the Pacific. [Google Scholar]
- 24.Wiles S. The three phases of Covid-19—and how we can make it manageable. The Spinoff. March 9, 2020. https://thespinoff.co.nz/society/09-03-2020/the-three-phases-of-covid-19-and-how-we-can-make-it-manageable/
- 25.Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Press trust of India 3060 special trains ferried around 40 Lakh migrants since May 1: railways. NDTV India. May 26, 2020. https://www.ndtv.com/india-news/coronavirus-lockdown-indian-railways-says-3-060-shramik-special-trains-ferried-around-40-lakh-migrants-since-may-1-2235039
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
We used publicly available data and have referenced the sources in the paper.