The American Heart Association (AHA) Get With The Guidelines Coronary Artery Disease Advisory Work Group, and the Acute Care and Interventional Science Subcommittees of the AHA Council on Clinical Cardiology, are responding to the call of concern on ideal ST-segment–elevation myocardial infarction (STEMI) Systems of Care during the coronavirus disease 2019 (COVID-19) pandemic. Emergency interim guidance is being provided, pivoting from the conventional AHA evidence-based meticulous peer review process. This statement addresses STEMI Systems of Care issues throughout the pandemic, to ensure that patients with STEMI continue to receive life-saving treatments while maintaining patient and healthcare worker safety.
COVID-19 and STEMI
Mission: Lifeline is the American Heart Association’s national initiative to advance the systems of care for patients with STEMI.1 Under normal operative conditions, a STEMI system of care requires constant oversight and data review to manage continuous quality improvement. As a result of the COVID-19 pandemic, disruptions in the most refined systems of care have occurred.
Delays are anticipated across the continuum of STEMI care. US hospitals are reporting substantial declines in patients presenting by emergency medical services (EMS) or by direct presentation with STEMI.2 Patients and family members may be less likely to call 911 for cardiac symptoms because of fear of exposure to the coronavirus. It is also plausible that there is a protective effect of sheltering, improved behaviors, and increased family support. More EMS-transported patients are expected to be critically ill requiring mechanical ventilation. EMS may need to transport patients to temporary facilities or directly to the most appropriate facility based on local resources. Fleet resources may become limited while ambulances are being decontaminated and restocked with supplies. Appropriate delays in EMS first medical contact are to be expected as essential precautionary measures are required to minimize COVID-19 exposure and transmission. Necessary delays after hospital arrival occur related to new triage protocols requiring personal travel history, additional detailed sign and symptom screening, thoughtful patient assignment based on suspicion of being COVID-19 positive, and new catheterization laboratory preparations/readiness treating patients in full personal protective equipment (PPE).
Interim Emergency STEMI Systems of Care Guidance
Public Awareness/Call 911
Although the United States is in the midst of the coronavirus crisis, public awareness campaigns are needed to remind individuals of the signs and symptoms of heart attack, with an added emphasis on calling 911 as soon as possible. Patients must be reassured that appropriate precautions are being taken to protect them and healthcare workers from COVID-19. Earlier entry into the system of care will help offset the expected delays in care.
Prehospital/Emergency Medical Services
In attempts to mitigate exposure, the Centers for Disease Control and Prevention recommend Emergency Medical Dispatch centers or 911 Public Safety Answering Points dispatchers triage callers, utilizing a series of questions to identify patients (and anyone in the home) who may be experiencing coronavirus signs and symptoms and share this information with prehospital first responders.3
Before arrival at the scene, EMS should don the appropriate PPE that must be available to all EMS personnel. Once on scene, the EMS provider should screen the patient again to identify high-risk features. If possible, limiting the number of EMS providers evaluating the patient is recommended. EMS should assume that all patients, regardless of dispatch complaint, may have COVID-19. Minimum recommended PPE for all patient encounters is a surgical mask, eye protection, and gloves. For patients who are deemed to be at high risk for COVID-19, additional PPE is warranted.
Once EMS has made rapid but safe and protected contact with the patient, acquisition of the 12-lead ECG should be expedited with subsequent interpretation and prompt notification of findings (and likelihood of COVID-19 infection) to the emergency department. For diagnostic ST elevation, prehospital catheterization laboratory activation should occur immediately. However, often prehospital activation requires more thoughtfulness, coordination, and judgment with particular attention to possible STEMI mimics and duration of symptoms.
Emergency Department
For patients presenting through EMS from the field, there should be a standard brief stop in the receiving hospital emergency department before proceeding to the catheterization laboratory, with clear communication between the emergency department physician and the interventional cardiologist. Patients should be triaged for consideration of placement to COVID-positive or suspect and COVID-negative areas. Testing for COVID-19 should not delay primary percutaneous coronary intervention (PCI) for those with clear STEMI. Point-of-care ultrasound use may be helpful to delineate left ventricular wall motion abnormality and pulmonary pathology, particularly in suspected STEMI mimics. Patients who require mechanical ventilation should be intubated before transport to the catheterization laboratory with a lower than usual threshold to avoid aerosol spread of respiratory secretions.
Fibrinolytic administration for patients with true STEMI who cannot receive PCI and coronary reperfusion within 120 minutes when transferred from a STEMI referring-hospital should be considered, consistent with guideline recommendations.4 Absent significant system resource constraints, PCI should remain the primary and preferred reperfusion strategy for patients with classic STEMI based on superior outcomes with PCI including preservation of left ventricular function and lower rates of reinfarction, stroke, and death and in view of the higher prevalence of STEMI mimics.
Catheterization Laboratory
Consideration should be given to options to safely increase catheterization laboratory readiness to accept patients with STEMI more quickly from the field and emergency department once screened for coronavirus. Designation of 1 laboratory for patients who have tested positive for COVID-19, stocked only with the essential equipment needed for all procedures, may be helpful. Consideration should be given to use of a negative pressure room, limiting staff in the room, and terminal cleaning with possibly a longer 4- to 6-hour clean. Because 25% to 50% of patients infected with SARS-CoV-2 are asymptomatic,5 catheterization laboratory personnel should assume that all patients are COVID-19 positive, particularly in high prevalence areas, and don appropriate PPE.
Postreperfusion Hospital Care
Triaging patients to proper units after primary PCI is important. In uncomplicated cases, disposition to a noncritical care bed should be considered to conserve critical care beds for patients with COVID-19 requiring mechanical ventilation or critical care unit care. Patients should receive the usual care after myocardial infarction including adherence to guideline directed medical therapy and post–myocardial infarction assessment of left ventricular function with echocardiography. When hospital beds are in extreme demand, early discharge between 24 to 48 hours after PCI in patients with uncomplicated STEMI may be considered.
STEMI System of Care Guideline Adherence
The American College of Cardiology (ACC)/AHA STEMI Guideline recommendations continue to provide the foundation of our evidence-based therapies and efforts to meet time-sensitive goals should continue.4 However, during this COVID-19 pandemic, the inherent delays should be considered as nonsystem delays in the context of reporting measures.
Postdischarge Care
Telemedicine
Because of the COVID-19 crisis, the value of telemedicine can surge in (STEMI) heart attack systems of care consultation and management. Coordination of care between STEMI receiving centers, with EMS, and with STEMI referring hospitals may benefit from telemedicine capabilities. Telemedicine can also help with family communications for patients with STEMI, as many family members are prohibited from entering the hospital.
Cardiac Rehabilitation
Stay-at-home orders and social distancing guidelines have and will continue to have an effect on cardiac rehabilitation opportunities. Cardiac rehabilitation can be attended in a healthcare facility–based program or a home health or virtual model, and referral should still be made to a program to facilitate enrollment at a later date.
Summary
Despite the effect of the COVID-19 pandemic on STEMI Systems of Care (Figure), evidence-based cardiac care and the tenets of our collective systems of care success should not be abandoned. Regionalization of STEMI care is perhaps more important than ever. Communication between hospitals and EMS and interfacility transport providers in a region, sharing protocols, resources, data, and experiences may prove critically important. Usual monthly review meetings should continue through the pandemic, in a virtual format, to review regional performance and opportunities for improvement.
Figure.
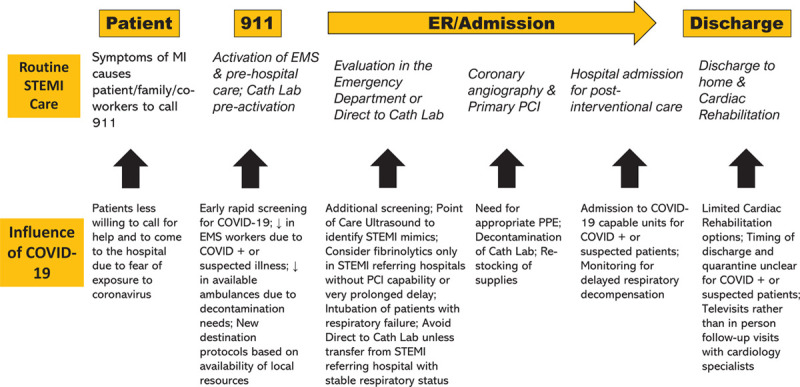
Potential Effect of the COVID-19 Pandemic on STEMI Systems of Care EMS indicates emergency medical services; ER, emergency room; COVID-19, coronavirus disease 2019; MI, myocardial infarction; PCI, percutaneous coronary intervention; PPE, personal protective equipment; STEMI, ST-segment–elevation myocardial infarction.
Disclosures
The Get With The Guidelines Coronary Artery Disease (GWTG-CAD) program is provided by the American Heart Association. GWTG-CAD is sponsored, in part, by Novartis, Edwards, and Amgen Cardiovascular. Dr Bieniarz reports consulting for Terumo and Abiomed, and consulting and speakers bureau for Amgen. Dr Fonarow reports consulting for Abbott, Amgen, AstraZeneca, Bayer, Edwards, Janssen, Medtronic, Merck, and Novartis. Dr Granger reports no conflicts relevant to the current work. Dr Jacobs is a site principal investigator for a trial by Abbott Vascular. Dr Zègre-Hemsey receives funding through the US National Institutes of Health. Drs Ali, Best, Cohen, Goyal, Henry, Hollowell, Jneid, Jollis, Katz, Mason, Menon, Redlener, and Tamis-Holland have no relevant relationships to disclose.
Appendix
Alice K. Jacobs, MD; Murtuza Ali, MD; Patricia J. Best, MD; Mark Bieniarz, MD; Mauricio G. Cohen, MD; William J. French, MD; Gregg C. Fonarow, MD; Christopher B. Granger, MD; Abhinav Goyal, MD; Timothy D. Henry, MD; Lori Hollowell, RN, MHIT; Hani Jneid, MD; James G. Jollis, MD; Jason N. Katz, MD, MHS; Peter Mason, MD, MPH; Venu Menon, MD; Michael Redlener, MD; Jacqueline E. Tamis-Holland, MD; Jessica Zegre-Hemsey, PhD, RN; On behalf of the American Heart Association’s Mission: Lifeline and Get With The Guidelines Coronary Artery Disease Advisory Work Group and the Council on Clinical Cardiology’s Committees on Acute Cardiac Care and General Cardiology and Interventional Cardiovascular Care.*
Footnotes
Endorsed by the AHA Council on Clinical Cardiology
The opinions expressed in this article are not necessarily those of the editors.
Contributor Information
Collaborators: Alice K. Jacobs, Murtuza Ali, Patricia J. Best, Mark Bieniarz, Mauricio G. Cohen, William J. French, Gregg C. Fonarow, Christopher B. Granger, Abhinav Goyal, Timothy D. Henry, Lori Hollowell, Hani Jneid, James G. Jollis, Jason N. Katz, Peter Mason, Venu Menon, Michael Redlener, Jacqueline E. Tamis-Holland, and Jessica Zegre-Hemsey
References
- 1.Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation 2007116217–230doi: 10.1161/CIRCULATIONAHA.107.184043 [DOI] [PubMed] [Google Scholar]
- 2.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020752871–2872doi: 10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Interim Guidance for Emergency Medical Services (EMS) Systems and 911 Public Safety Answering Points (PSAPs) for COVID-19 in the United States. Updated March 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-for-ems.html. Accessed April 11, 2020.
- 4.O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, et al. ; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013127e362–e425doi: 10.1161/CIR.0b013e3182742cf6 [DOI] [PubMed] [Google Scholar]
- 5.Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, Taylor J, Spicer K, Bardossy AC, Oakley LP, et al. ; Public Health–Seattle and King County and CDC COVID-19 Investigation Team Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med 20203822081–2090doi: 10.1056/NEJMoa2008457 [DOI] [PMC free article] [PubMed] [Google Scholar]


