Abstract
Background
Cannabis use is more common among nicotine users than non-users. This study characterized concurrent use of nicotine and cannabis (“co-use”) among 12,064 youth aged 16–19 residing in Canada, the United States, and England in 2017.
Methods
Data were from the ITC Youth Tobacco & Vaping Survey (Wave 1). Seven modes of cannabis delivery (MOD) were characterized by country of residence and past 30-day use of combusted tobacco and electronic cigarettes. Weighted multivariable regression models were fitted to assess correlates of co-use and each cannabis MOD.
Results
Seventy-percent of cannabis users reported nicotine use. Co-users exhibited behavioral and demographic differences compared to exclusive users of either substance. “Smoking cannabis without tobacco” was the most popular form of use (78%). Use of nicotine-containing e-cigarettes was associated with “using an e-cigarette to vape cannabis oil/liquid” (aOR:4.96, 95%CI: 2.23–11.06). Combustible tobacco use was associated with “smoking cannabis with tobacco in a joint/blunt” (aOR:2.93, 95%CI: 1.89–4.56). Country-level differences were detected.
Conclusions
Nicotine use is substantial among cannabis users, and associations exist between modes of delivery for both drugs. Results underscore the importance of studying cannabis and nicotine use concurrently, and the need to address use of both substances in developing interventions for youth users.
Keywords: Cannabis, Nicotine, Youth, Vaping, Co-use, Modes of delivery
Introduction
Use of cannabis and nicotine among youth presents a substantial global public health burden, with an estimated 13.8 million youth aged 15–16 years reporting past-year use of cannabis in 2016, and approximately 25 million youth reporting current use of cigarettes or smokeless tobacco.1 Youth commonly experiment with these substances, which may present elevated health harms related to brain development and risks of developing substance use disorders.2,3 In many high-income countries, rates of youth cigarette smoking are declining, while youth trial and use of electronic cigarettes (“e-cigarettes”) and electronic vapor products is increasing.4–6 In tandem, changes in cannabis policies have contributed to considerable expansion of the cannabis market in recent years, with a greater diversity of products and modes of delivery in both ‘illegal’ and ‘legal’ markets.7
Use of cannabis and nicotine are often studied in isolation with respect to the other substance. However, concurrent use (“co-use”) of cannabis and nicotine is common, with estimates showing 5.4% of youth reporting co-use in the United States, compared with 2.2% reporting exclusive cannabis use, and 3.9% reporting exclusive nicotine use.8 Prior research suggests there are a number of problems related to co-use, including heavier nicotine and cannabis use, greater dependence on both substances, difficulty in quitting cannabis use, linkage to problematic use of alcohol and other illicit drugs, increased likelihood of experiencing psychotic symptoms later in life, and elevated exposure risks for smoke-related toxicants.9–13 Commonalities in the primary route of administration for both substances (i.e., inhalation) have been posited as reinforcing mechanisms of co-use, which may serve to further compound related health harms.14 The significant overlap between the modes of delivery used to administer cannabis and nicotine may also contribute to emerging co-use patterns. Many tobacco products can be used for cannabis administration (i.e., flavored rolling papers, blunts),15,16 and vaporized modes of delivery are available for both substances.17,18
Cross-national differences in cannabis and nicotine modes of delivery exist, yet often remain unexamined through the lens of co-use. Smoking remains the predominant form of cannabis delivery, but specific practices related to cannabis smoking are regionally and culturally determined.19 For example, mixing cannabis and tobacco in “spliffs”/”mulled cigarettes” (i.e., joints that mix tobacco with cannabis) or “blunts” (i.e., cigars that have been hollowed out and filled with cannabis) are common co-administration practices, with spliff use being far more common in Western European countries, and blunt use occurring more frequently in North American countries.19–21 Further, countries with different regulatory treatment of e-cigarettes and vaping products display differences in public perceptions of these products, and their subsequent adoption and use.22 For example, in England, authorities place substantial restrictions on e-cigarette advertising, promotion, and allowable nicotine content in the products, which have been largely normalized for the purpose of tobacco smoking cessation.23 A recent cross-national study showed that past 30-day nicotine vaping was less common among youth in England compared to youth in the United States and Canada.24 It is possible that cultural contexts specific to nicotine products could influence cannabis use behaviors, and vice versa.
Characterizations of co-use in light of diversifying modes of delivery remain sparse,25,26 and have not been examined in a cross-national context. The primary objective of this study was to characterize cannabis and nicotine co-use patterns among youth aged 16–19 years in three countries, based on their past-30 day use of different modes of cannabis and nicotine delivery. Secondary objectives aimed to assess correlates of co-use, and specific cannabis modes of delivery.
Methods
Data source
Data are from Wave 1 of the International Tobacco Control Policy Evaluation Youth Tobacco and Vaping Survey, conducted in July/August 2017 among 12,064 youth aged 16–19 years, in Canada (CA; n = 4,008), England (EN; n = 3,970), and the United States (US; n = 4,086). Participants were recruited through Nielsen’s Consumer Insights Global Panel and affiliated partners using a blend of probability and non-probability-based sampling strategies. After eligibility screening, and obtaining parental consent and youth assent (where applicable), participants completed a 15-minute survey consisting of sociodemographic measures, questions on e-cigarette and tobacco use, and questions on other health behaviors, including cannabis use. Participants were compensated according to their panel’s standard incentive structure (e.g., points or cash remuneration, inclusion in prize raffles.) Additional data on recruitment and data collection methods are available elsewhere.27,28 Institutional review boards at the University of Waterloo and King’s College London provided ethics approval for the project, which was sufficient to allow the study to be undertaken at all sites. At the time of data collection, non-medical use of cannabis was prohibited by all three nations at the Federal/national level. Participants’ identifying information (i.e., names, addresses, and/or telephone numbers) were unavailable to the research team. Data ascertained during the survey was kept anonymous and used exclusively in aggregate form during analyses.29
Measures
Cannabis use & modes of delivery
Cannabis use was assessed using the following question: “When was the last time you used marijuana/cannabis?” (response options: “I have never used cannabis”; “Earlier today”; “Not today but sometime in the past week”; “Not in the past week but sometime in the past month”; “Not in the past month but sometime in the past 6 months”; “Not in the past 6 months but sometime in the past year”; “1 to 4 years ago”; “5 or more years ago”). Participants who responded “earlier today”; “not today but sometime in the past week”; or “not in the past week but sometime in the past month” were classified as past 30-day cannabis users. Past 30-day cannabis users were asked to report on their use of seven different modes of delivery: “In the last 30 days, did you…”: (a) “smoke cannabis without tobacco”; (b) “smoke cannabis with tobacco in a joint or blunt”; (c) “use a waterpipe or bong to smoke cannabis”; (d) “use a vaporizer to heat dried cannabis leaves or herb”; (e) “use an e-cigarette to vape cannabis oil or liquid”; (f) “eat or drink cannabis in a food or beverage”; (g) “use cannabis extracts, including oil, wax or shatter” (response options for each: Yes, No).
Nicotine use & modes of delivery
All respondents answered the following questions: “Have you ever tried a cigarette, even one or two puffs?”; “Have you ever tried an e-cigarette, even one or two puffs?”. Participants who responded “Yes” were successively asked: “When was the last time you used a… [cigarette/ e-cigarette]?”. Youth selected from the following answers: (a) “Earlier today”; (b) “Not today but sometime in the past 7 days”; (c) “Not in the past 7 days but sometime in the past 30 days”; (d) “Not in the past 30 days but sometime in the past 6 months”; (e) “Not in the past 6 months but sometime in the past year”; (f) “1 to 4 years ago”; and (g) “5 or more years ago”. Additionally, participants responded to a yes/no checklist pertaining to past 30-day use of other tobacco products (“In the past 30 days, have you used any of the following?”: (a) little cigars or cigarillos; (b) cigars; (c) bidis; (d) smokeless tobacco; (e) nicotine patches/ gum/ lozenges; (f) waterpipe to smoke shisha).
Mutually exclusive categories were developed in accordance with combustible tobacco and nicotine e-cigarette use: (a) respondents who reported no past 30-day use of nicotine products were defined as non-nicotine users; (b) participants reporting past 30-day use of a single combustible product (cigarette, little cigar/cigarillo, cigar, bidis, waterpipe/shisha) and no past 30-day e-cigarette were designated as exclusive single-combustible nicotine users; (c) past 30-day e-cigarette users who were not past 30-day combustible tobacco users were designated as exclusive nicotine e-cigarette users; (d) simultaneous past 30-day use of multiple nicotine products (combusted tobacco and/or e-cigarettes) were designated as dual/poly-nicotine users.
Other covariates
Socio-demographic measures assessed at baseline included sex, age, race-ethnicity (White vs. Non-white), and country of residence (CA, US, EN). Household income was approximated by assessing the number of computers in a participant’s home.30,31 Additional psychosocial control variables included past month measures of depression and anxiety (range: 0 “not at all” to 9 “severe”), alcohol use (never vs. ever), and harm perceptions regarding smoked cannabis use (“How much do you think people harm themselves when they smoke marijuana/cannabis?”: (a) “No harm”; (b) “Little harm”; (c) “Some harm”; (d) “A lot of harm”).
Statistical Analysis
Analyses were approached using available-case methods and were conducted using PROCSURVEY commands in SAS v.9.4. All analyses were weighted. Survey weights were constructed using a raking algorithm (details available at: http://davidhammond.ca/projects/tobacco-control/itc-youth-tobacco-ecig/). Univariate and bivariate analyses were conducted to assess the distributions and initial associations between variables of interest. Differences across sample subgroups were initially assessed with Rao-Scott χ2 tests of independence (categorical variables) and one-way analysis of variance (continuous variables). Multivariable logistic regression models were employed to examine correlates of exclusive nicotine or cannabis use versus co-use, and correlates of reporting use of each cannabis mode of delivery within the past 30 days. Exploratory analyses were conducted to test whether country of residence moderated associations between nicotine modes of delivery and cannabis modes of delivery among past 30-day users; cross-product interaction terms were included in secondary models examining cannabis mode of delivery outcomes. Statistical significance was determined based on p-values < 0.05.
Results
Prevalence of cannabis and nicotine use
Demographic characteristics and prevalence of past 30-day cannabis use among Wave 1 ITC Tobacco and Youth Vaping Survey respondents have been reported elsewhere.27,28 Respondents from each country primarily identified as white (US: 79.2%; CA: 63.9%; EN: 79.0%), had a mean age of 17.5 years, and were slightly more often male than female (US: 53.3%; CA: 51.6%; EN: 55.3%). Prevalence of past 30-day cannabis use was highest in the US (14.4%), followed by CA (12.7%) and EN (10.3%). Among past 30-day cannabis users, 82.4% reported still being enrolled in school, versus 90.6% of the overall sample. Estimates of nicotine and cannabis co-use are presented in Table 1. Overall, 74.5% of respondents reported no use of nicotine or cannabis products, 13.1% reported only nicotine use, 3.8% reported only cannabis use, and 8.7% reported co-use of nicotine and cannabis. These proportions differed according to country of residence (χ2 p < 0.001); the prevalence of nicotine and cannabis co-use was 8.8% in CA, 9.7% in the US, and 7.6% in EN. Among past 30-day nicotine users, 39.9% reported past 30-day cannabis use (CA: 49.8%; US: 41.6%; EN: 31.0% [χ2 p < 0.001]), while 69.7% of past 30-day cannabis users reported past 30-day nicotine use (CA: 69.1%; US: 67.3%; EN: 73.8% [χ2 p < 0.001]).
Table 1.
Past 30-day nicotine and cannabis use patterns among a sample of youth residing in the United States, Canada, and England.
| Overall |
Canada |
United States |
England |
Rao-Scott χ2 p value | |
|---|---|---|---|---|---|
| % weighted (95% CI) | % weighted (95% CI) | % weighted (95% CI) | % weighted (95% CI) | ||
| All Participants | n=12,064 | n=4,008 | n=4,086 | n=3,970 | |
|
| |||||
| No nicotine or cannabis use | 74.5 (73.4–75.6) | 78.5 (76.5–80.4) | 72.1 (70.3–73.9) | 72.8 (70.9–74.8) | < 0.001 |
| Only nicotine use | 13.1 (12.2–14.0) | 8.8 (7.4–10.2) | 13.5 (12.1–15.0) | 16.9 (15.2–18.6) | |
| Only cannabis use | 3.8 (3.4–4.2) | 3.9 (3.2–4.7) | 4.7 (4.0–5.4) | 2.7 (2.1–3.3) | |
| Nicotine and cannabis co-use | 8.7 (7.9–9.5) | 8.8 (7.3–10.2) | 9.7 (8.4–10.9) | 7.6 (6.3–8.9) | |
|
| |||||
| Cannabis users | n=1,310 | n=475 | n=499 | n=336 | |
|
| |||||
| No nicotine use | 30.3 (27.3–33.4) | 30.9 (25.4–36.4) | 32.7 (28.1–37.3) | 26.2 (20.5–31.9) | < 0.001 |
| Exclusive nicotine e-cigarette use | 4.9 (3.6–6.2) | 3.9 (2.0–5.7) | 6.7 (4.3–9.1) | 3.7 (1.5–5.9) | |
| Exclusive single-combustible use | 24.2 (20.9–27.5) | 27.7 (21.1–34.3) | 16.1 (12.3–20.0) | 31.4 (24.6–38.2) | |
| Dual/poly nicotine use | 40.6 (36.8–44.3) | 37.6 (30.8–44.3) | 44.5 (38.9–50.0) | 38.7 (31.4–46.1) | |
|
| |||||
| Nicotine users | n=2,172 | n=614 | n=737 | n=821 | |
|
| |||||
| No cannabis use | 60.1 (57.2–63.0) | 50.2 (44.1–56.3) | 58.4 (53.9–62.9) | 69.0 (64.5–73.5) | < 0.001 |
| Cannabis use | 39.9 (37.0–42.8) | 49.8 (43.7–55.9) | 41.6 (37.1–46.1) | 31.0 (26.5–35.5) | |
%weighted= weighted percentage; CI=confidence interval.
Correlates of co-use
Multivariable adjusted odds of engaging in past 30-day co-use of nicotine and cannabis can be viewed in Table 2. Among all past 30-day nicotine product users, co-use was positively associated with ever use of alcohol, use of multiple nicotine products, and with residing in CA. Additionally, co-use was associated with lower harm perceptions of smoked cannabis, and was about half as likely to occur among exclusive nicotine e-cigarette users versus exclusive users of a single combusted tobacco product. Among all past 30-day cannabis users, co-users had greater odds of identifying as White, residing in EN, and reporting symptoms of depression; past 30-day co-users had lower odds of residing in a home with multiple computers present.
Table 2.
Correlates of exclusive versus concurrent past 30-day nicotine and cannabis use among youth aged 16–19 residing in the United States, Canada, and England
| Odds of concurrent use vs. exclusive nicotine use n=1,928 | Odds of concurrent use vs. exclusive cannabis use n=1,080 | |
|---|---|---|
|
| ||
| aOR (95% CI)* | aOR (95% CI)† | |
| Age | 1.10 (0.96–1.27) | 1.04 (0.89–1.23) |
| Sex | ||
| Female | 1.00 (ref) | 1.00 (ref) |
| Male | 0.90 (0.68–1.19) | 1.34 (0.97–1.86) |
| Race-ethnicity | ||
| Non-white | 1.00 (ref) | 1.00 (ref) |
| White | 0.81 (0.59–1.11) | 1.49 (1.07–2.09) |
| Country of residence | ||
| USA | 1.00 (ref) | 1.00 (ref) |
| Canada | 1.68 (1.16–2.44) | 1.01 (0.70–1.46) |
| England | 0.84 (0.60–1.17) | 1.68 (1.12–2.51) |
| No. of computers | 0.99 (0.90–1.09) | 0.86 (0.78–0.95) |
| Depression | 1.03 (0.95–1.11) | 1.10 (1.01–1.19) |
| Anxiety | 1.04 (0.96–1.12) | 0.99 (0.91–1.08) |
| Alcohol use | ||
| Never | 1.00 (ref) | 1.00 (ref) |
| Ever | 2.71 (1.73–4.26) | 1.42 (0.81–2.48) |
| Harm perception of smoked cannabis | 0.52 (0.45–0.60) | 0.84 (0.70–1.02) |
| Past 30-day nicotine use | ||
| Exclusive single-combustible use | 1.00 (ref) | --- |
| Exclusive nicotine e-cigarette use | 0.55 (0.37–0.83) | --- |
| Dual/poly nicotine use | 1.89 (1.38–2.58) | --- |
Bold values denote statistically significant findings (p<0.05).
Adjusted for age, sex, race-ethnicity, country of residence, number of computers, depression, anxiety, alcohol use, harm perceptions of smoked cannabis, & past 30-day nicotine use.
Adjusted for age, sex, race-ethnicity, country of residence, number of computers, depression, anxiety, alcohol use, & harm perceptions of smoked cannabis.
Age, no. of computers, depression, anxiety and harm perceptions of smoked cannabis were modeled as continuous variables.
Modes of cannabis delivery
Among all past 30-day cannabis users, “smoking cannabis without tobacco” was the dominant mode of delivery (77.6%), followed by “using a waterpipe or bong to smoke cannabis” (51.7%), “smoking cannabis with tobacco in a joint or blunt” (49.8%), “eating or drinking cannabis in a food or beverage” (26.7%), “using cannabis extracts, including oil, wax, or shatter” (20.7%), “using an e-cigarette to vape cannabis oil or liquid” (17.1%), and “using a vaporizer to heat dried cannabis leaves or herb” (16.6%). Nearly three-quarters (73%) of past 30-day cannabis users reported using more than one cannabis mode of delivery within the past month (Mean = 2.7, SE = 0.07). Among youth reporting multiple modes of cannabis use, the top three cannabis use combinations were: (a) “smoking cannabis without tobacco” + “using a waterpipe or bong to smoke cannabis” (44.1%); (b) “smoking cannabis without tobacco” + “smoking cannabis with tobacco in a joint or blunt” (32.3%); and (c) “smoking cannabis with tobacco in a joint or blunt” + “using a waterpipe or bong to smoke cannabis” (27.3%).
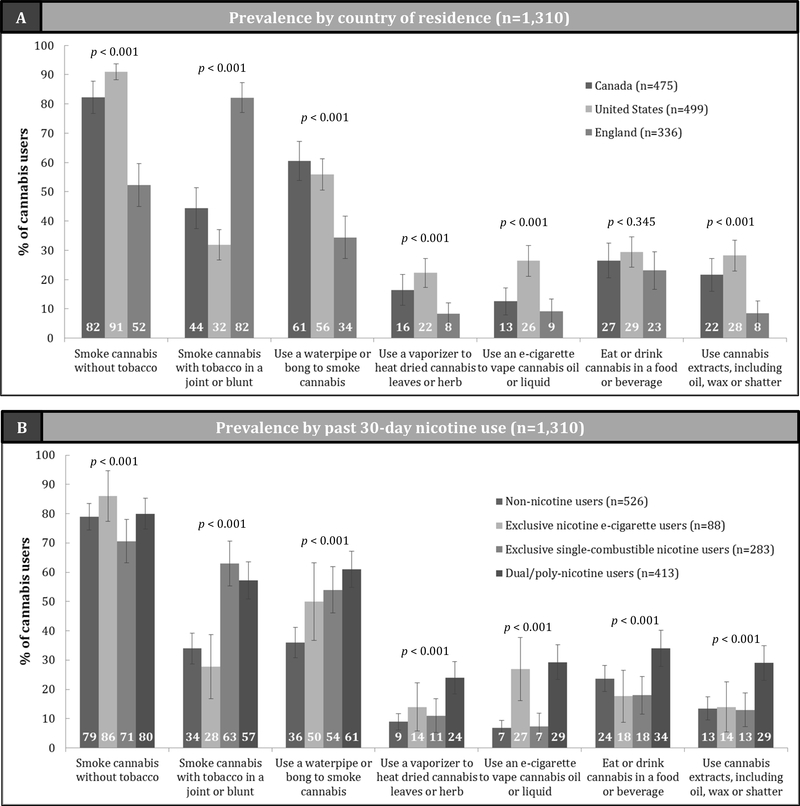
Differences in the prevalence of each cannabis MOD according to (a) country of residence and (b) past 30-day nicotine use are further detailed in Figure 1. “Smoking cannabis without tobacco” was most prevalent among youth cannabis users in CA and the US (χ2 p < 0.001), while youth cannabis users residing in EN more frequently reported “smoking cannabis with tobacco” (χ2 p < 0.001). “Smoking cannabis with tobacco” was most prevalent among exclusive single-combustible nicotine users and dual/poly-tobacco users, while “using an e-cigarette to vape cannabis oil or liquid” was most frequently reported by past 30-day exclusive e-cigarette users and by dual/poly-tobacco users (χ2 p < 0.001).
Figure 1:
Modes of cannabis delivery (MOD) used by past 30-day youth cannabis users aged 16–19, according to (A) country of residence, and (B) past 30-day nicotine use.
Error bars note 95% confidence intervals for estimates. P-values denote statistically significant associations between endorsed cannabis mode of delivery and (A) country of residence, or (B) past 30-day tobacco use status (Rao-Scott χ2 test, p<0.05). Percentages indicate endorsement of cannabis MOD within each group, users were allowed to endorse multiple modes of delivery. Therefore, percentages may add up to more than 100%.
Correlates of modes of cannabis delivery
Findings from multivariable logistic regression models suggested differences in the associations between select cannabis modes of delivery and country of residence, and by past 30-day nicotine use (Table 3). Compared to youth in the US, youth in CA and EN had lower odds of reporting “smoking cannabis without tobacco”, and “using an e-cigarette to vape cannabis oil or liquid”. Youth in EN also exhibited reduced odds of “using a waterpipe or bong to smoke cannabis”, “using a vaporizer to heat dried cannabis leaves or herb”, and “using cannabis extracts, including oil, wax, or shatter”. Conversely, EN youth had 10.6 fold greater odds, and youth in CA had 1.7 fold greater odds of “smoking cannabis with tobacco in a joint or blunt” compared to US youth. Odds of “smoking cannabis with tobacco in a joint or blunt” and “using a waterpipe or bong to smoke cannabis” were significantly higher among past 30-day exclusive single combustible nicotine users and dual/poly-nicotine users relative to non-nicotine users. Past 30-day exclusive nicotine e-cigarette users had approximately five-fold greater odds of “using an e-cigarette to vape cannabis oil or liquid”; a similar association was observed among dual/poly-nicotine users. Dual/poly-nicotine users also exhibited greater odds of “using a vaporizer to heat dried cannabis leaves or herb”, “eating or drinking cannabis in a food or beverage”, and “using cannabis extracts including oil, wax, or shatter” compared to past 30-day cannabis users that did not use any nicotine products. Results from models including cross-product terms for country of residence and past 30-day nicotine use revealed no statistically significant results.
Table 3.
Correlates of reporting past 30-day use of seven modes of cannabis delivery (MOD), among all past 30-day users of cannabis
| Smoke cannabis without tobacco (n=1,219) | Smoke cannabis with tobacco in a joint or blunt (n=1,224) | Use a waterpipe/bong to smoke cannabis (n=1,232) | Use a vaporizer to heat dried cannabis leaves or herb (n=1,229) | Use an e-cigarette to vape cannabis oil or liquid (n=1,231) | Eat or drink cannabis in a food or beverage (n=1,239) | Use cannabis extracts, including oil, wax, or shatter (n=1,234) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Age | 1.23 (0.99–1.53) | 0.98 (0.82–1.18) | 1.14 (0.96–1.36) | 1.58 (1.21–2.05) | 1.19 (0.94–1.50) | 1.30 (1.08–1.56) | 1.28 (1.02–1.60) |
| Sex | |||||||
| Female | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Male | 1.72 (1.13–2.63) | 1.39 (0.97–2.00) | 1.46 (1.05–2.04) | 1.38 (0.84–2.28) | 1.68 (1.03–2.74) | 1.18 (0.81–1.73) | 1.29 (0.85–1.95) |
| Race-ethnicity | |||||||
| Non-white | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| White | 0.93 (0.60–1.45) | 0.64 (0.45–0.92) | 1.10 (0.78–1.56) | 0.73 (0.46–1.15) | 0.77 (0.49–1.22) | 0.81 (0.56–1.18) | 0.94 (0.61–1.44) |
| Country of residence | |||||||
| USA | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Canada | 0.36 (0.21–0.60) | 1.65 (1.12–2.45) | 1.09 (0.75–1.60) | 0.71 (0.42–1.21) | 0.38 (0.22–0.65) | 0.82 (0.54–1.24) | 0.68 (0.44–1.07) |
| England | 0.07 (0.05–0.12) | 10.58 (6.69–16.76) | 0.34 (0.22–0.52) | 0.31 (0.17–0.58) | 0.26 (0.14–0.49) | 0.77 (0.49–1.22) | 0.23 (0.12–0.45) |
| No. of computers | 1.13 (0.99–1.28) | 0.97 (0.86–1.08) | 0.91 (0.82–1.01) | 1.00 (0.86–1.18) | 1.04 (0.88–1.23) | 0.98 (0.87–1.11) | 0.97 (0.86–1.10) |
| Depression | 0.98 (0.89–1.07) | 1.03 (0.95–1.13) | 1.02 (0.93–1.11) | 0.98 (0.88–1.10) | 1.08 (0.97–1.20) | 1.07 (0.97–1.17) | 1.01 (0.91–1.12) |
| Anxiety | 1.06 (0.96–1.16) | 1.03 (0.94–1.13) | 1.09 (0.99–1.18) | 1.02 (0.92–1.14) | 1.04 (0.93–1.17) | 1.02 (0.92–1.12) | 1.13 (1.02–1.25) |
| Alcohol use | |||||||
| Never | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Ever | 3.06 (1.53–6.14) | 1.21 (0.64–2.29) | 1.24 (0.68–2.26) | 0.74 (0.34–1.61) | 0.54 (0.27–1.08) | 1.12 (0.61–2.05) | 0.71 (0.39–1.31) |
| Harm perception of smoked cannabis | 1.01 (0.99–1.03) | 1.01 (0.99–1.02) | 1.00 (0.98–1.01) | 1.01 (0.99–1.03) | 1.00 (0.99–1.02) | 1.00 (0.98–1.01) | 1.00 (0.98–1.02) |
| Past 30-day nicotine use | |||||||
| No past 30-day use | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Exclusive nicotine e-cigarette use | 1.02 (0.42–2.48) | 0.82 (0.38–1.77) | 1.60 (0.83–3.09) | 1.71 (0.73–4.01) | 4.96 (2.23–11.06) | 0.63 (0.31–1.28) | 1.12 (0.48–2.62) |
| Exclusive single-combustible use | 0.70 (0.43–1.15) | 2.93 (1.89–4.56) | 2.14 (1.38–3.32) | 1.60 (0.81–3.15) | 1.38 (0.61–3.12) | 0.70 (0.42–1.17) | 1.15 (0.60–2.21) |
| Dual/poly nicotine use | 0.98 (0.59–1.62) | 2.81 (1.90–4.16) | 2.82 (1.92–4.14) | 3.45 (2.13–5.57) | 5.47 (3.40–8.79) | 1.62 (1.11–2.36) | 2.87 (1.76–4.65) |
Bold values denote statistically significant findings (p<0.05).
Results adjusted for age, sex, race-ethnicity, country of residence, number of computers, depression, anxiety, alcohol use, harm perceptions of smoked cannabis, & past 30-day nicotine use.
Age, no. of computers, depression, anxiety and harm perceptions of smoked cannabis were modeled as continuous variables.
Discussion
Our results indicate that a majority of youth cannabis users also co-use nicotine, and co-users of both substances differ from exclusive users on important risk-related variables, such as use of alcohol and multiple nicotine-containing products. Modes of cannabis delivery used by youth were diverse, though smoked forms of cannabis were the most common. Co-users’ affinity for certain modes of delivery differed according to country of residence and their nicotine use, and associations were detected between smoked and vaped forms of cannabis and nicotine delivery. These findings emphasize the need to consider concurrent cannabis and nicotine use in developing interventions for youth, particularly youth at greater risk for substance-use related harms.
Findings imply youth who report use of cannabis are very likely to use nicotine in some form, which is linked to other risky health-related behaviors among co-using youth. As depicted in Table 1, almost three-quarters of past 30-day youth cannabis users reported past 30-day use of nicotine, and about 40% of nicotine users reported past 30-day cannabis use. This is important to consider in light of recent information from other studies stating that youth cannabis use exceeds use of nicotine.32 While all youth use of nicotine and cannabis is illegal, this asymmetrical distribution of co-use may be indicative of a subset of nicotine users who are more willing to engage in illicit behaviors. This is in line with our finding that co-using youth exhibited several additional markers of risky behavior, including alcohol use and poly- nicotine use, lower socioeconomic status, and reporting symptoms of depression. As cannabis use becomes increasingly permitted in these nations, high rates of co-use should be considered in developing salient prevention and harm reduction interventions for youth substance use. This consideration may prove to be beneficial in targeting youth who engage in higher-risk health behaviors, and are more challenging to reach through traditional youth-prevention approaches.33
Our findings displayed in Figure 1 also point toward substantial variability in the ways youth use cannabis within different countries, which was associated with certain forms of nicotine use. This indicates that the regulatory and cultural contexts under which these behaviors take place are important to consider when addressing prevention needs related to youth nicotine use, and vice versa. For example, youth in England were more likely to “smoke cannabis with tobacco” and were less likely to report using other MODs than youth in other nations; while youth in North America exhibited more variability in their chosen cannabis MODs. Mulling (i.e., adding tobacco to cannabis smoked as joints) is a traditional cannabis consumption practice among adults in Western Europe, even among those who do not identify as tobacco users; this use practice appears to translate to youth.19–21 Conversely, youth in the U.S. and Canada reside in countries with some of the highest cannabis use rates in the world, which correlate with liberalized cannabis policies.34 Liberalization of cannabis is linked to greater use of non-smoked modes of use.35 Additionally, vaping cannabis oil in an e-cigarette was more commonly reported among U.S. youth compared with youth in England and Canada. This is important to consider in light of recent reports by the U.S. Surgeon General and others noting increases in past 30-day vaping among U.S. high school students,4,36 as well as recent outbreaks of acute vaping-related respiratory illnesses occurring in this population.37,38 In combination with existing information on cross-national differences in youth use of nicotine in e-cigarettes,24 our findings suggest there is a factor unique to the U.S. sociocultural environment that could be underlying youth vaping behaviors relative to other countries. While we did not detect statistically significant interactions examining respondent nicotine e-cigarette use by country of residence, small samples sizes resulting from these stratifications may have contributed to a lack of statistical power to detect such effects. Cross-national differences in co-use practices should continue to be monitored in order to provide accurate and effective information that can target problematic co-use behaviors among youth.
The results from this study also point to the need for concurrent study of youth use of nicotine and cannabis, which can ensure accurate measurement related to individual and concurrent use of these substances moving forward. We found that 34% of cannabis users reported smoking cannabis with tobacco, but did not self-report current tobacco or nicotine use. The phenomenon of misclassification in tobacco use based on mulling practices (i.e., mulled cigarette users often identify as “non-smokers”) has been found in other studies, and should be monitored in the context of youth substance use.21 Along these same lines, many common measures of youth vaping behavior do not differentiate between vaping nicotine or vaping cannabis, which may introduce error into estimates of youth “vaping”.39,40 While many national surveys are beginning to address this issue,4,17,32 researchers working within these domains should be aware of the need to specify the substances being smoked and/or vaped by youth, and be aware of common co-use practices that could result in misclassified estimates to obtain accurate estimates in their own assessments.
This study benefits from a large sample size spanning three countries with different policies and norms related to cannabis and nicotine use. While the sample was not obtained using a strict probability-based sampling method, the findings are consistent with those from similar studies,8,18,41 which lend credibility to both the results and the data collection approach. Limitations of the present work include the cross-sectional design and potential underreporting of cannabis use by youth, due to its illicit status.42 Further, an absence of measurements for nicotine product and cannabis use quantity and frequency specific to each mode of delivery, and other product-level measures (i.e., use of flavored cannabis oils, method of concentrate use, cannabis product potency) may further influence specific patterns of co-use, which should be explored in future studies. For instance, examinations of daily/near daily use, versus past 30-day use can provide useful information on co-use patterns that pose more or less risk to youth users, especially considering the links between daily/near-daily nicotine and cannabis use, and risks of dependence.2 Additionally, frequency of use will also vary across modes of cannabis that contain different cannabis product formulations (i.e., cannabis flower, oils, concentrates), which have a wide range of potencies that can lead to increased risk of cannabis dependence.2 Despite these limitations, the findings provide important contributions to understanding youth who use both nicotine products and cannabis, and international differences in co-use.
Conclusions
This study demonstrates that youth use cannabis through a diverse range of modes of delivery, which are most commonly delivered through smoking. Further, the majority of youth cannabis users also co-use nicotine products, and associations between modes of delivery for administering cannabis and nicotine exist. Given the existing literature on the health effects stemming from co-use, 9–13 studies are needed to bi-directionally examine initiation into co-use, evaluate potential co-use behavioral reinforcement as it pertains to vaping and e-cigarette use, and the impact of these issues on use escalation, heaviness of nicotine product use, and cessation among youth users. Results underscore the importance of studying cannabis and nicotine use concurrently, and the need to address use of both substances in developing interventions for youth users.
Acknowledgments
FUNDING: The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. This work was supported by National Institute of Health (NIH) Grants 1-P01CA200512–01 and 1-P30CA16056.
Footnotes
DECLARATIONS OF INTEREST: MLG receives fees for serving on an advisory board from Johnson & Johnson and grant support from Pfizer. The other authors have no conflicts of interest to declare.
References
- 1.United Nations Office on Drugs and Crime. World Drug Report 2018: Drugs and Age - Drugs and associated issues among young people and older people. Vienna, Austria, 2019. [Google Scholar]
- 2.National Academies of Science, Engineering, and Medicine. The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. Washington D.C.2017. [PubMed] [Google Scholar]
- 3.Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J Physiol. 2015;593(16):3397–3412.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gentzke AS, Creamer M, Cullen KA, et al. Vital Signs: Tobacco Product Use Among Middle and High School Students - United States, 2011–2018. MMWR Morb Mortal Wkly Rep. 2019;68(6):157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reid JLHD, Tariq U, Burkhalter R, Rynard VL, Douglas O. Tobacco Use in Canada: Patterns and Trends, 2019 Edition. Waterloo, ON2019. [Google Scholar]
- 6.Bauld L, MacKintosh AM, Eastwood B, et al. Young People’s Use of E-Cigarettes across the United Kingdom: Findings from Five Surveys 2015–2017. Int J Environ Res Public Health. 2017;14(9):973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marijuana Business Daily. Marijuana Industry Statistics, Data and Charts. 2019; https://mjbizdaily.com/category/charts/.Accessed May 18, 2019.
- 8.Schauer GL, Peters EN. Correlates and trends in youth co-use of marijuana and tobacco in the United States, 2005–2014. Drug Alcohol Depend. 2018;185:238–244. [DOI] [PubMed] [Google Scholar]
- 9.Meier E, Hatsukami DK. A review of the additive health risk of cannabis and tobacco co-use. Drug Alcohol Depend. 2016;166:6–12. [DOI] [PubMed] [Google Scholar]
- 10.Peters EN, Schwartz RP, Wang S, O’Grady KE, Blanco C. Psychiatric, psychosocial, and physical health correlates of co-occurring cannabis use disorders and nicotine dependence. Drug Alcohol Depend. 2014;134:228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramo DE, Liu H, Prochaska JJ. Tobacco and marijuana use among adolescents and young adults: a systematic review of their co-use. Clin Psychol Rev. 2012;32(2):105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones HJ, Gage SH, Heron J, et al. Association of Combined Patterns of Tobacco and Cannabis Use in Adolescence With Psychotic Experiences. JAMA psychiatry. 2018;75(3):240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith DM, O’Connor RJ, Wei B, Travers M, Hyland A, Goniewicz ML. Nicotine and Toxicant Exposure among Concurrent Users (“Co-users”) of Tobacco and Cannabis. Nicotine Tob Res. 2019. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agrawal A, Budney AJ, Lynskey MT. The co-occurring use and misuse of cannabis and tobacco: a review. Addiction. 2012;107(7):1221–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giovenco DP, Miller Lo EJ, Lewis MJ, Delnevo CD. “They’re Pretty Much Made for Blunts”: Product Features That Facilitate Marijuana Use Among Young Adult Cigarillo Users in the United States. Nicotine Tob Res. 2017;19(11):1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kong G, Bold KW, Simon P, Camenga DR, Cavallo DA, Krishnan-Sarin S. Reasons for Cigarillo Initiation and Cigarillo Manipulation Methods among Adolescents. Tob Regul Sci. 2017;3(2 Suppl 1):S48–S58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trivers KF, Phillips E, Gentzke AS, Tynan MA, Neff LJ. Prevalence of cannabis use in electronic cigarettes among us youth. JAMA Pediatrics. 2018;172(11):1097–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S. High School Students’ Use of Electronic Cigarettes to Vaporize Cannabis. Pediatrics. 2015;136(4):611–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Russell C, Rueda S, Room R, Tyndall M, Fischer B. Routes of administration for cannabis use - basic prevalence and related health outcomes: A scoping review and synthesis. Int J. Drug Policy. 2018;52:87–96. [DOI] [PubMed] [Google Scholar]
- 20.Belanger RE, Akre C, Kuntsche E, Gmel G, Suris JC. Adding tobacco to cannabis--its frequency and likely implications. Nicotine Tob Res. 2011;13(8):746–750. [DOI] [PubMed] [Google Scholar]
- 21.Fix BV, Smith DM, O’Connor R, et al. Cannabis use among a nationally representative cross-sectional sample of smokers and non-smokers in the Netherlands: results from the 2015 ITC Netherlands Gold Magic Survey. BMJ Open. 2019;9(3):E024497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yong H-H, Hitchman SC, Cummings KM, et al. Does the Regulatory Environment for E-Cigarettes Influence the Effectiveness of E-Cigarettes for Smoking Cessation?: Longitudinal Findings From the ITC Four Country Survey. Nicotine Tob Res. 2017;19(11):1268–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McNeill A, Brose LS, Calder R, Hitchman SC, Hajek P, H M. E-cigarettes: an evidence update. A report commissioned by Public Health England. 2015. [Google Scholar]
- 24.Hammond D, Reid JL, Rynard VL, et al. Prevalence of vaping and smoking among adolescents in Canada, England, and the United States: repeat national cross sectional surveys. BMJ (Clinical research ed). 2019;365:l2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohn AM, Abudayyeh H, Perreras L, Peters EN. Patterns and correlates of the co-use of marijuana with any tobacco and individual tobacco products in young adults from Wave 2 of the PATH Study. Addict Behav. 2019;92:122–127. [DOI] [PubMed] [Google Scholar]
- 26.Peters EN, Bae D, Barrington-Trimis JL, Jarvis BP, Leventhal AM. Prevalence and Sociodemographic Correlates of Adolescent Use and Polyuse of Combustible, Vaporized, and Edible Cannabis Products. JAMA Netw Open. 2018;1(5):e182765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wadsworth E, Hammond D. Differences in patterns of cannabis use among youth: Prevalence, perceptions of harm and driving under the influence in the USA where non-medical cannabis markets have been established, proposed and prohibited. Drug Alcohol Rev. 2018;37(7):903–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wadsworth E, Hammond D. International differences in patterns of cannabis use among youth: Prevalence, perceptions of harm, and driving under the influence in Canada, England & United States. Addict Behav. 2019;90:171–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammond D, Reid JL, White CM, C B. ITC Youth Tobacco And E-Cigarette Survey: Technical Report – Wave 1 (2017). University of Waterloo; March20182017. [Google Scholar]
- 30.Hartley JE, Levin K, Currie C. A new version of the HBSC Family Affluence Scale - FAS III: Scottish Qualitative Findings from the International FAS Development Study. Child Indic Res. 2016;9:233–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torsheim T, Cavallo F, Levin KA, et al. Psychometric Validation of the Revised Family Affluence Scale: a Latent Variable Approach. Child Indic Res. 2016;9:771–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnston L, Miech R, O’Malley P, Bachman J, Schulenberg J, Patrick M. 2018 Overview: Key Findings on Adolescent Drug Use. Ann Arbor, Michigan: Institute for Social Research, University of Michigan, 2019. [Google Scholar]
- 33.Frankford ER. Changing service systems for high-risk youth using state-level strategies. American journal of public health. 2007;97(4):594–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hall W, Stjepanović D, Caulkins J, et al. Public health implications of legalising the production and sale of cannabis for medicinal and recreational use. Lancet. 2019;394:1580–90. [DOI] [PubMed] [Google Scholar]
- 35.Borodovsky JT, Crosier BS, Lee DC, Sargent JD, Budney AJ. Smoking, vaping, eating: Is legalization impacting the way people use cannabis? International Journal of Drug Policy. 2016;36:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.United States Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults. A Report of the Surgeon General. Atlanta GA, 2016. [Google Scholar]
- 37.Layden JE, Ghinai I, Pray I, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin — Preliminary Report. New England Journal of Medicine. 2019. [DOI] [PubMed] [Google Scholar]
- 38.United States Centers for Disease Control and Prevention. Outbreak of Lung Disease Associated with E-Cigarette Use, or Vaping. 2019; https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html#latest-outbreak-information.Accessed September 13, 2019.
- 39.McDonald EA, Popova L, Ling PM. Traversing the triangulum: the intersection of tobacco, legalised marijuana and electronic vaporisers in Denver, Colorado. Tobacco Control. 2016;25(Suppl 1):i96–i102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Popova L, McDonald EA, Sidhu S, et al. Perceived harms and benefits of tobacco, marijuana, and electronic vaporizers among young adults in Colorado: implications for health education and research. Addiction. 2017;112(10):1821–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Knapp AA, Lee DC, Borodovsky JT, Auty SG, Gabrielli J, Budney AJ. Emerging Trends in Cannabis Administration Among Adolescent Cannabis Users. J Adolesc Health. 2019;64(4):487–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boykan R, Messina CR, Chateau G, Eliscu A, Tolentino J, Goniewicz ML. Self-Reported Use of Tobacco, E-cigarettes, and Marijuana Versus Urinary Biomarkers. Pediatrics. 2019;143(5). [DOI] [PubMed] [Google Scholar]