Abstract
Purpose:
To characterize performance among ED sites participating in the Emergency Quality Network (E-QUAL) Avoidable Imaging Initiative for clinical targets on the American College of Emergency Physicians Choosing Wisely list.
Methods:
This was an observational study of quality improvement (QI) data collected from hospital-based ED sites in 2017–2018. Participating EDs reported imaging utilization rates (UR) and common QI practices for three Choosing Wisely targets: Atraumatic Low Back Pain, Syncope, or Minor Head Injury.
Results:
305 ED sites participated in the initiative. Among all ED sites, the mean imaging UR for Atraumatic Low Back Pain was 34.7% (IQR 26.3%−42.6%) for XR, 19.1% (IQR 11.4%24.9%) for CT, and 0.09% (IQR 0%−0.9%) for MRI. The mean CT UR for Syncope was 50.0% (IQR 38.0%−61.4%). The mean CT UR for Minor Head Injury was 72.6% (IQR 65.6%−81.7%). ED sites with sustained participation showed significant decreases in CT UR in 2017 compared to 2018 for Syncope (56.4% vs 48.0%; 95% CI: −12.7%, −4.1%) and Minor Head Injury (76.3% vs 72.1%; 95% CI: −7.3%, −1.1%). There was no significant change in imaging UR for Atraumatic Back Pain for XR (36.0% vs 33.3%; 95% CI: −5.9%, −0;5%), CT (20.1% vs 17.7%; 95% CI: −5.1%, −0.4%) or MRI (0.8% vs 0.7%; 95% CI: −0.4%, −0.3%).
Conclusions:
Early data from the E-QUAL Avoidable Imaging Initiative suggests QI interventions could potentially improve imaging stewardship and reduce low-value care. Further efforts to translate the Choosing Wisely recommendations into practice should promote data-driven benchmarking and learning collaboratives to achieve sustained practice improvement.
Keywords: Quality Improvement, Benchmarking, Diagnostic Imaging, Emergency Department
1. INTRODUCTION
1.1. Background
The Choosing Wisely campaign was launched by the American Board of Internal Medicine Foundation in 2012 to promote physician stewardship of healthcare resources by encouraging specialty societies to develop “Top Five” lists of low-value care practices amenable to avoidance. By 2014, the American College of Emergency Physicians (ACEP) had published ten evidence-based Choosing Wisely recommendations to promote resource stewardship and reduce low-value care in the emergency department (ED).1 Five of the ten items identified by ACEP were focused on the use of advanced imaging.2 These recommendations were based on research demonstrating the potential overuse of imaging for several indications despite evidence-based guidelines to direct practice. One large national study demonstrated a 330% increase in CT utilization in the ED between 1996 and 2007 without improving diagnostic yield, and a study of Medicare beneficiaries found that the low-value services targeted by the Choosing Wisely initiative may contribute over $8.5 billion a year to annual health care costs in the Medicare program alone.3–5
1.2. Importance
Since the inception of Choosing Wisely, emergency departments (EDs) across the country have initiated quality improvement (QI) efforts to implement recommendations in concert with national “Top Five” lists. These efforts are highly varied and include clinical pathways, computerized decision support tools, physician audit and feedback, and shared-decision making. While they showed promise in reducing potentially avoidable imaging within local contexts, efforts to identify and disseminate best practices have been limited and mostly confined to academic settings.6,7 EDs that engaged in performance improvement initiatives to reduce imaging utilization also have few national benchmarks for comparison.8 Finally, studies showed that while most ED physicians acknowledge overimaging as a problem, they are unaware of their own overutilization and continue to perform low value services.9–11 Clinicians continue to be vulnerable to the “therapeutic illusion” of believing that their diagnostic tools are more effective than they actually are, resulting in unnecessary or costly care.12
To address these gaps, The American College of Emergency Physicians (ACEP) Emergency Quality Network (E-QUAL) created the Avoidable Imaging Initiative in 2016.13 This initiative aims to establish national benchmarking data for imaging utilization using a large sample of hospital-based community EDs, disseminate common QI interventions, share best practices to reduce avoidable imaging, and report performance variation and improvement trends.
1.3. Objectives
We sought to characterize imaging utilization performance and variation for QI efforts to reduce potentially avoidable imaging for Atraumatic Low Back Pain, Syncope, and Minor Head injury among ED sites participating in the ACEP E-QUAL Avoidable Imaging Initiative. We also sought to characterize top-performing ED sites to identify specific benchmarks for improvement and best practices associated with high performance.
2. METHODS
2.1. Study Design
This was an observational study of QI data obtained from a national learning network. Demographic, benchmarking, and survey data were collected from the E-QUAL database for all ED sites participating in the E-QUAL Avoidable Imaging Initiative in either 2017 or 2018, with data collected between December 2016 and December 2018. We focused on three clinical targets for imaging reduction within the initiative based on the ACEP Choosing Wisely list: Atraumatic Low Back Pain, Syncope, and Minor Head Injury (see Appendix 1).
2.2. Ethical Approval
This QI study did not include protected health information (PHI) and was not considered human subjects research by our institutional review board.
2.3. Study Population
A total of 334 hospital-based ED sites in the United States were recruited to participate in the E-QUAL Avoidable Imaging Initiative on an annual basis in 2017 and/or 2018. Participation was voluntary with EDs recruited nationally by the American College of Emergency Physicians (ACEP) for enrollment in the Emergency Quality Network. Enrollment was offered over a 3-month period prior to each calendar year and advertised at national and state meetings and through electronic channels such as email blasts, as well as direct engagement of large emergency medicine staffing organizations. Of all the recruited EDs sites, 29 (8.7%) were excluded due to missing data for QI benchmarking metrics, leaving 305 ED sites in our study group.
2.4. Study Protocol and Measurements
We collected demographic, imaging utilization, and quality survey data from all participating ED sites using a standardized web-based submission portal. Demographic data included annual ED volume, group size, and ZIP code. We categorized EDs by volume as Small (<20K annual visits), Medium (20–60K), or Large (>60K). We stratified group size as groups staffing a single ED versus multiple EDs. Imaging utilization data is described in detail below. EDs were classified as rural or urban based on the Rural-Urban Commuting Area Code for each ED site ZIP code. Survey data included participation in eleven QI activities, implementation of best practices, and qualitative comments from success stories at top-performing ED sites. See Appendix 2 for the complete survey questionnaire for the 2018 E-QUAL Avoidable Imaging Initiative.
2.5. Outcome Measures
The primary outcome measure for this study was indication-specific imaging utilization rates based on E-QUAL measure definitions (see Appendix 3). The E-QUAL Avoidable Imaging Workgroup developed and approved nine imaging utilization measures to translate the clinical practice statements of the ACEP Choosing Wisely list into proportional and quantifiable metrics for QI purposes. For example, the ACEP Choosing Wisely recommendation “avoid computed tomography (CT) scans of the head in emergency department patients with minor head injury who are at low risk based on validated decision rules” was represented by the E-QUAL imaging utilization measure “Head CT Utilization for Minor Head Trauma.” The denominator for each measure was the total number of cases with diagnostic codes for the clinical target (Atraumatic Low Back Pain, Syncope, or Minor Head Injury), and the numerator was the total number of imaging orders by modality (XR, CT, or MRI). Adult patients >18 years old were included in the measures for 2017 and adult patients 18–65 years old were included in 2018. Secondary outcome measures included engagement rates in QI activities.
2.6. Data Analysis
Descriptive statistics were calculated for all imaging utilization measures in 2017, 2018, and both years for all participating ED sites. Interquartile ranges (IQR) were calculated to describe performance variation. In addition, we separately defined performance at the extremes to better characterize “top” and “bottom” performers for benchmarking purposes, since the utilization rates of “top performers” could serve as potential performance targets. To describe top and bottom performers for each imaging utilization measure, we calculated a binomial proportion confidence interval for each ED site based on its numerator and denominator for the measure using a Bayesian likelihood method. “Top” performance refers to lower utilization rates and “bottom” performance refers to higher utilization rates. For each clinical target and imaging modality, we defined a top performer as any ED site with a utilization rate upper confidence interval below the overall mean score for all participating ED sites. Conversely, we defined a bottom performer as any ED site with a utilization rate lower confidence interval above the overall mean score for all participating ED sites. See Supplemental Figure 1 for a graphical representation of these definitions. This approach is similar to that used by the Center for Medicare and Medicaid Services (CMS) to calculate measures for Hospital Compare.14 We described the change in performance from 2017 to 2018 for ED sites with sustained participation in both years and compared imaging utilization rates in 2017 versus 2018 using t-tests. Finally, we calculated the correlation between imaging modalities for Atraumatic Low Back Pain using Pearson correlation coefficients. We used R (version 3.6.0; R Core Team, Vienna, Austria) for all analyses.
3. RESULTS
3.1. Characteristics of Study Subjects
The characteristics of all participating ED sites are shown in Table 1. A total of 305 hospital-based EDs participated in the E-QUAL Avoidable Imaging Initiative in 2017 or 2018. Of these, 76 (25%) were small volume with <20K annual visits, 157 (51%) were medium volume with 2060K annual visits, and 44 (14%) were large volume with >60K annual visits. A total of 208 EDs (68%) were urban and 69 (23%) were rural. Only 1 ED group (0.3%) staffed a single ED, while 304 ED groups (99.7%) were part of larger organizations that staffed multiple EDs. There were no notable differences in the distribution of ED volume, group size, or urban vs rural setting for participating ED sites within each of the clinical targets (Atraumatic Low Back Pain, Syncope, or Minor Head Injury).
Table 1.
ED Site Demographics
| 2017–2018 n (%) | 2017 Only n (%) | 2018 Only n (%) | |
|---|---|---|---|
| ALL TARGETS | |||
| TOTAL | 305 (100%) | 143 (100%) | 272 (100%) |
| Volume | |||
| Small (<20K) | 76 (25%) | 26 (18%) | 76 (28%) |
| Medium (20–60K) | 157 (51%) | 74 (52%) | 153 (56%) |
| Large (>60K) | 44 (14%) | 15 (10%) | 43 (16%) |
| Unknown | 28 (9%) | 28 (20%) | 0 (0%) |
| Region | |||
| Urban | 208 (68%) | 87 (61%) | 203 (75%) |
| Rural | 69 (23%) | 28 (20%) | 69 (25%) |
| Unknown | 28 (9%) | 28 (20%) | 0 (0%) |
| ATRAUMATIC LOW BACK PAIN | |||
| TOTAL | 280 (100%) | 127 (100%) | 257 (100%) |
| Volume | |||
| Small (<20K) | 75 (27%) | 26 (20%) | 75 (29%) |
| Medium (20–60K) | 144 (51%) | 67 (53%) | 143 (56%) |
| Large (>60K) | 39 (14%) | 12 (9%) | 39 (15%) |
| Unknown | 22 (8%) | 22 (17%) | 0 (0%) |
| Region | |||
| Urban | 191 (68%) | 78 (61%) | 190 (74%) |
| Rural | 67 (24%) | 27 (21%) | 67 (26%) |
| Unknown | 22 (8%) | 22 (17%) | 0 (0%) |
| SYNCOPE | |||
| TOTAL | 278 (100%) | 127 (100%) | 259 (100%) |
| Volume | |||
| Small (<20K) | 73 (26%) | 26 (20%) | 73 (28%) |
| Medium (20–60K) | 148 (53%) | 72 (57%) | 145 (56%) |
| Large (>60K) | 41 (15%) | 13 (10%) | 41 (16%) |
| Unknown | 16 (6%) | 16 (13%) | 0 (0%) |
| Region | |||
| Urban | 197 (71%) | 83 (65%) | 194 (75%) |
| Rural | 65 (23%) | 28 (22%) | 65 (25%) |
| Unknown | 16 (6%) | 16 (13%) | 0 (0%) |
| MINOR HEAD INJURY | |||
| TOTAL | 280 (100%) | 123 (100%) | 259 (100%) |
| Volume | |||
| Small (<20K) | 74 (26%) | 25 (20%) | 74 (29%) |
| Medium (20–60K) | 147 (53%) | 66 (54%) | 145 (56%) |
| Large (>60K) | 41 (15%) | 14 (11%) | 40 (15%) |
| Unknown | 18 (6%) | 18 (15%) | 0 (0%) |
| Region | |||
| Urban | 195 (70%) | 79 (64%) | 192 (74%) |
| Rural | 67 (24%) | 26 (21%) | 67 (26%) |
| Unknown | 18 (6%) | 18 (15%) | 0 (0%) |
3.2. Main Results
Overall imaging utilization rates are shown in Figure 1, with descriptive statistics summarized in Supplemental Table 1. Across all participating ED sites (n=305) for 2017–2018, the national average imaging utilization rates for Atraumatic Low Back Pain were 34.7% (IQR 26.3%−42.6%) for XR, 19.1% (IQR 11.4%−24.9%) for CT, and 0.09% (IQR 0%−0.9%) for MRI. The national average CT utilization rate for Syncope was 50.0% (IQR 38.0%−61.4%). The national average CT utilization rate for Minor Head Injury was 72.6% (IQR 65.6%−81.7%).
Figure 1.
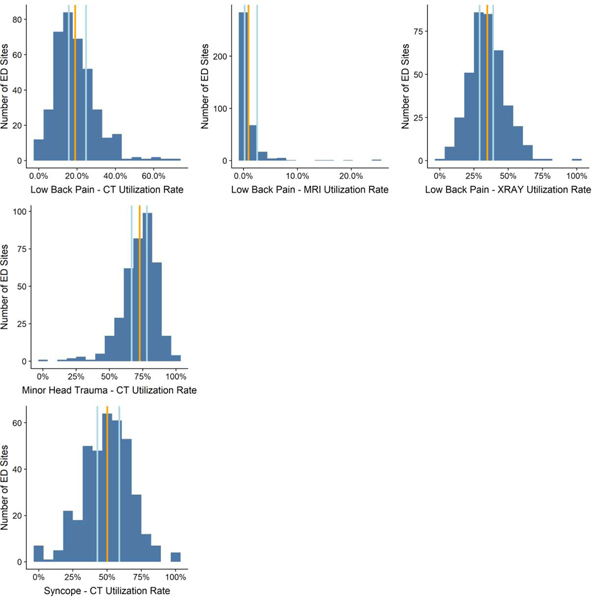
Utilization Rates for Atraumatic Low Back Pain, Syncope and Minor Head Injury in 2017–2018*
Orange Line = Overall Mean; Lower Blue Line = Lower Confidence Line; Upper Blue Line = Upper Confidence Line
* This figure includes all ED sites that participated in the initiative in 2017 or 2018.
** n values represent the total number of data points for each measure, not the number of unique ED sites. For instance, if an ED site reported a data point in 2017 and a data point in 2018, this would be counted as 2 data points. As a result, the n values for these measures exceed the total number of unique ED sites in our sample (n=305).
For XR utilization in Atraumatic Low Back Pain, a total of 89 ED sites (23.2%) were considered top-performers for reporting utilization rates below the national average (mean top-performing score 19.6%) and 84 ED sites (21.9%) were considered bottom-performers for reporting rates above the national average (mean bottom-performing score 50.3%). For CT utilization in Atraumatic Low Back Pain, a total of 99 ED sites (25.8%) were considered top-performers for reporting rates below the national average (mean top-performing score 8.7%) and 79 ED sites (20.6%) were considered bottom-performers for reporting rates above the national average (mean bottom-performing score 34.6%). For MRI utilization in Atraumatic Low Back Pain, a total of 4 ED sites (mean score 1.0%) were considered top-performers for reporting rates below the national average and 32 ED sites (8.3%) were considered bottom-performers for reporting rates above the national average (mean bottom performing score 6.7%).
For CT utilization in Syncope, a total of 66 ED sites (17.0%) were considered top-performers (mean score 28.7%) and 57 ED sites (14.7%) were considered bottom-performers (mean score 71.9%). Finally, for CT utilization in Minor Head Injury, a total of 57 ED sites (15.0%) were considered top-performers (mean score 52.6%) and 87 ED sites (22.8%) were considered bottom-performers (mean score 86.3%).
The change in imaging utilization rates for 2017 vs 2018 are reported in Table 2 with the corresponding graphs in Supplemental Figure 2. Of all participating ED sites (n=305), only some consistently participated in the initiative in both 2017 and 2018 for Atraumatic Low Back Pain (n=104), Syncope (n=103), and Minor Head Injury (n=102). There was no significant change in XR, CT, or MRI utilization for Atraumatic Low Back Pain between the two years. There was significant performance improvement in CT utilization for Syncope in 2017 compared to 2018 (56.4% vs 48.0%; 95% CI: −12.7%, −4.1%), as well as significant performance improvement in CT utilization for Minor Head Injury (76.3% vs 72.1%; 95% CI: −7.3%, −1.1%). There was no significant change in imaging utilization rates for Atraumatic Back Pain over this time period for XR (36.0% vs 33.3%; 95% CI: −5.9%, −0;5%), CT (20.1% vs 17.7%; 95% CI: −5.1%, −0.4%) or MRI (0.8% vs 0.7%; 95% CI: −0.4%, −0.3%).
Table 2.
Comparison of Imaging Utilization Rates in 2017 vs 2018 for ED Sites Participating in Both Years*
| 2017 Mean Utilization Rate (n ED Sites) | 2018 Mean Utilization Rate (n ED Sites) | 2017 vs 2018 Difference in Mean UR (95% CI) P-Value | |
|---|---|---|---|
| ATRAUMATIC LOW BACK PAIN | |||
| XR | 36% (n = 104) | 33.3% (n = 104) | −2.7% (−5.9%, −0.5%) p=0.095 |
| CT | 20.1% (n = 104) | 17.7% (n = 104) | −2.4% (−5.1%, −0.4%) p=0.09 |
| MRI | 0.8% (n = 104) | 0.7% (n = 104) | −0.1% (−0.4%, −0.3%) p=0.777 |
| SYNCOPE | |||
| CT | 56.4% (n = 103) | 48.0% (n = 103) | −8.4% (−12.7%, −4.1%) p<0.001 |
| MINOR HEAD INJURY | |||
| CT | 76.3% (n = 102) | 72.1% (n = 102) | −4.2% (−7.3%, −1.1%) p=0.008 |
This table only includes ED sites that participated in the initiative in both 2017 and 2018 (not 2017 or 2018).
Participating ED sites showed high levels of engagement in QI Activities in the E-QUAL Avoidable Imaging Initiative across all three clinical targets. In 2017, 96.1% of all participating ED sites completed all E-QUAL QI activities for Atraumatic Low Back Pain, 95.9% completed all activities for Syncope, and 96.9% completed all activities for Minor Head Trauma. In 2018, participation improved to 98.8%, 99.6%, and 98.8%, respectively, among all sites.
Several QI Activities were widely and consistently implemented at participating ED sites in both 2017 and 2018, regardless of the clinical target. These included: 1) Adoption of a Departmental Protocol or Guideline (99%); 2) Collaboration with Radiology (92–99%); and 3) Engagement with Leadership (97–100%).
Qualitative survey comments including success stories and lessons learned are shown in Table 3. Multiple EDs cited the difficulty of changing provider practice patterns as their main challenge. Common success themes included using evidence-based education and clinical decision rules to change physician behaviors, implementing both patient education and provider re-education, and involving radiology decision-support.
Table 3.
Success Stories from Top-Performing ED Sites
| ATRAUMATIC LOW BACK PAIN | “Our challenge was educating the staff that not all patients with back pain need imaging. Also, obtaining good data was and remains a challenge. Finally, it can be challenging to get providers to change their practice patterns and it can be difficult, even in the age of the EMR to get reliable data. We believe we were able to reduce the utilization of imaging in patients with atraumatic back pain. If we were to do this project over again, I believe that it would have been easier if we worked with IT to generate baseline data and then provide post- education data.” - ED Medical Director (Large Volume, Urban ED) |
| SYNCOPE | “The biggest challenge was changing practice behaviors in those who have been practicing for many years and are used to doing [things] a certain way. Another challenge is that they may not have kept up with the current literature on this topic. We were able to change ordering patterns in our clinicians with respect to this category of patients. In the moment, discussions as well as radiology decision support helped move the needle on this. Continued reminders and frequent re-education is necessary to change practice. If we were going to do this project over again, we would implement more frequent updates.” - ED Residency Program Director (Medium Volume, Urban ED) |
| MINOR HEAD INJURY |
“Our challenge at first was educating staff (docs and nurses) that not necessarily all patients with head injury need CT. Our baseline numbers were actually better than I expected, and department-wide education was well-received. If we were going to do this project over again, we would have reading material for patients at the outset, perhaps to read as they are waiting for a provider.” - ED Medical Director (Small Volume, Rural ED) “Our group learned that instituting a validated clinical decision rule such as the Canadian Head CT Rule successfully decreased our imaging rates and increased our diagnostic yield. By knowing and having the literature to support our decisions, we were able to engage patients and their families in discussions about imaging and it’s risks and successfully avoid imaging in patients that expected to have a head CT after their minor head injury. If we were going to do this project over again, we would present our project and goals at the resident didactic conference in order to address as many residents as possible. With several residents rotating through the ED each month, it was difficult to discuss this initiative with them individually. In addition, a patient simulation of a difficult patient demanding CT imaging in a role play situation may be a tool that would aid in providers being able to manage patient expectations.” - ED Physician (Medium Volume, Urban ED) |
4. DISCUSSION
Despite the national attention generated by the Choosing Wisely campaign, imaging stewardship continues to be a controversial and challenging topic for the vast majority of EDs in the United States. The reduction of avoidable imaging is impeded by financial incentives that favor overutilization, requests from consulting and admitting physicians, overconfidence in imaging diagnostic capabilities, medicolegal risks, and the high capital cost of acquiring advanced imaging systems. These challenges are compounded by the lack of clear national performance benchmarks for specific conditions. Existing national benchmarks such as those published by the Emergency Department Benchmarking Alliance (EDBA) refer to overall CT utilization rates, but do not report rates by clinical target.15 To our knowledge, this is the first paper to report the implementation of a QI initiative for avoidable imaging that establishes benchmarking metrics and describes QI practices for specific clinical targets at the national level.
We found relatively high imaging utilization rates for each Choosing Wisely clinical target with broad variation in performance among all participating EDs, as evidenced by the large interquartile ranges for each measure. We also found large discrepancies in top versus bottom-performing scores for all clinical targets and imaging modalities. Our findings are consistent with earlier studies at the local and regional levels which report high but variable CT utilization among ED providers.16–18 For instance, a recent systematic review of 17 studies by Viau et al. found that 54.4% of ED patients presenting with syncope underwent Head CT.19 This is comparable with the rate of 56.4% reported in 2017 by our participating ED sites. Notably, this rate decreased significantly to 48.0% in 2018 for ED sites participating in both years, which may suggest that sustained dedication of resources to imaging stewardship is associated with tangible improvements in imaging utilization.
Our participating ED sites represent a sample of motivated volunteers who were highly engaged in QI efforts (96–99% reported that they completed all the recommended QI activities in our initiative). Our benchmarking data could therefore serve as performance improvement targets for EDs pursuing similar QI interventions to reduce avoidable imaging. We believe that these targets can be generalized as national benchmarks due to the large size and diversity of E-QUAL participants, which primarily includes smaller community and/or rural EDs that have been previously understudied for benchmarking purposes.20 We also describe the mean scores of top-performing ED sites, which can serve as “reach” performance targets for ED sites seeking specific targets for QI interventions or pay-for-performance programs.
Our data also suggests that CT imaging for Atraumatic Back Pain should be a focus area for future improvement. Amongst EDs participating in E-QUAL we found no significant change in CT imaging rates for this clinical target between 2017 and 2018. This could be due to more requirements from referring, consulting or admitting services to obtain ED imaging for this specific complaint. It could also be due to the lack of consensus on best practices for back pain imaging, including a lack of evidence-based risk scores or clinical-decision support tools to guide imaging decisions. The existence of such scores for Syncope (e.g., the Canadian Syncope Risk Score and San Francisco Syncope Rule) and Minor Head Injury (i.e., the NEXUS and Canadian Head CT Rules), as well as well-studied educational and shared-decision making frameworks, may have contributed to the success of QI interventions for these clinical targets. Encouragingly, and counter to conventional policy efforts however, the mean MRI utilization rate for Atraumatic Low Back Pain remained low at 0.9% for all ED sites (though this number may be constrained due to lack of MRI availability in some participating EDs).
Finally, our qualitative data confirms that there is broad support for national performance benchmarks to guide QI efforts at participating ED sites. Several participating sites explicitly prioritized the need for evidence-based targets to drive local improvement and communicate performance with clinicians and hospital leadership. One ED noted that having “baseline data” and “post-education data” would have smoothed the QI intervention process (see Table 3).
Our study has several limitations. First, the data in our study are self-reported by volunteer EDs without external audits, which may inflate engagement and performance rates. E-QUAL does provide standardized data submission instructions and support to all participating ED sites to encourage reliable data collection. Each ED site also attested to their results, such that false reporting is essentially fraud. Also, performance scores within E-QUAL are confidential to participating sites and no payment or policy incentives are tied to performance. Second, this is a descriptive study of imaging utilization trends among a non-random sample of motivated ED sites with high levels of QI engagement. The actual imaging performance of this sample is likely higher than that of the general ED population. While our findings are appropriate benchmarking targets for performance improvement, they are unlikely to be representative of the baseline performance of the general ED population. In addition, due to the absence of control data, we are unable to draw conclusions regarding the causality between specific QI interventions and performance improvements over time among our participating ED sites. Third, the E-QUAL quality measures are highly denominator dependent. For instance, the denominator for Syncope may include stroke workups at some ED sites. We attempted to minimize this denominator effect by including explicit ICD-10 Code lists under the benchmarking data submission instructions for each clinical target. Finally, we did not perform a formal qualitative analysis as part of this study. Qualitative results are reported only to support our discussion of the benchmarking data.
Now nearly seven years after its inception, the Choosing Wisely campaign remains relevant alongside broader national efforts directed at healthcare resource stewardship and cost reduction such as alternative payment models. Interestingly, what began as a moral call for physicians to take individual responsibility and accountability for resource stewardship is now accepted as a worthwhile topic for ED-wide improvement initiatives. EDs that joined the E-QUAL Avoidable Imaging Initiative did so without a clear external mandate from CMS to address imaging utilization and demonstrated the central role of emergency care in broader national value-based initiatives.
Future work should expand upon these findings and investigate how diagnostic yield is impacted by changes in imaging utilization. We can also further characterize which QI activities and best practices yielded the greatest improvements in imaging appropriateness and determine if implementing these practices at bottom-performing ED sites will result in appreciable performance improvements.
5. CONCLUSIONS
We found wide variation in imaging utilization performance among a large national sample of hospital-based EDs participating in the E-QUAL Avoidable Imaging Initiative. There was significant improvement among ED sites with sustained participation in the initiative from 2017–2018. Early evidence from this initiative supports the possibility of applying QI methods to improve imaging stewardship and reduce low-value care. Further efforts to translate recommendations of the Choosing Wisely campaign into practice should promote the use of data-driven benchmarking and learning collaboratives to achieve sustained practice improvement.
Supplementary Material
Highlights.
Benchmarking data from a large national sample of hospital-based EDs shows wide variation in imaging utilization among clinical targets of the Choosing Wisely ™ campaign including Atraumatic Low Back Pain, Syncope, and Minor Head Injury
ED sites with sustained participation in a national QI initiative showed significant reductions in imaging utilization
Imaging utilization rates from top-performing ED sites can serve as performance improvement targets for future QI efforts
Efforts to translate recommendations of the Choosing Wisely ™ campaign into practice should promote the use of data-driven benchmarking and learning collaboratives to achieve sustained practice improvement
Acknowledgments
SOURCES OF SUPPORT: The project described was supported by Funding Opportunity Number CMS-1L1CMS331479–02 from the US Department of Health and Human Services, Centers for Medicare and Medicaid Services. The contents provided are solely the responsibility of the authors and do not necessarily represent the official views of the US Department of Health and Human Services or any of its agencies. This award supports the American College of Emergency Physicians Support and Alignment Network (SAN) of the CMS Transforming Clinical Practice Initiative (TCPi). Dr. Venkatesh also reports career development support (grant KL2TR001862) from the National Center for Advancing Translational Science and Yale Center for Clinical Investigation.
DECLARATION OF INTEREST: Dr. Venkatesh reports support from the Centers for Medicare & Medicaid Services for the development of hospital outcome and efficiency quality measures.
ABBREVIATIONS:
- E-QUAL
The Emergency Quality Network
- QI
Quality Improvement
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Arjun K. Venkatesh, Department of Emergency Medicine, Yale University School of Medicine, New Haven, CT; Yale–New Haven Hospital Center for Outcomes Research and Evaluation, New Haven, CT.
Jean Sun Scofi, Department of Emergency Medicine, Yale University School of Medicine, New Haven, CT.
Craig Rothenberg, Department of Emergency Medicine, Yale University School of Medicine, New Haven, CT.
Carl T. Berdahl, Departments of Medicine and Emergency Medicine, Cedars-Sinai Medical Center, Los Angeles, CA.
Nalani Tarrant, American College of Emergency Physicians, Washington, DC.
Dhruv Sharma, American College of Emergency Physicians, Washington, DC.
Pawan Goyal, American College of Emergency Physicians, Washington, DC.
Randy Pilgrim, SCP Health, Lafayette LA.
Kevin Klauer, American College of Emergency Physicians, Washington, DC.
Jeremiah D. Schuur, Department of Emergency Medicine, Brown Alpert Medical School, Providence, RI.
REFERENCES
- 1.Choosing Wisely. An initiative of the ABIM Foundation. http://www.choosingwisely.org/clinician-lists/.
- 2.Cassel CK, Guest JA. Choosing Wisely: Helping Physicians and Patients Make Smart Decisions About Their Care. JAMA. 2012;307(17):1801–1802. doi: 10.1001/jama.2012.476 [DOI] [PubMed] [Google Scholar]
- 3.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007. JAMA. 2010;304(13):1465–1471. doi: 10.1001/jama.2010.1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306(16):1794–1795. doi: 10.1001/jama.2011.1561 [DOI] [PubMed] [Google Scholar]
- 5.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring Low-Value Care in Medicare. JAMA Intern Med. 2014;174(7):1067–1076. doi: 10.1001/jamainternmed.2014.1541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raja AS, Venkatesh AK, Mick N, et al. “Choosing Wisely” Imaging Recommendations: Initial Implementation in New England Emergency Departments. West J Emerg Med. 2017;18(3):454–458. doi: 10.5811/westjem.2017.1.32677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Le Grand Rogers R, Narvaez Y, Venkatesh AK, et al. Improving emergency physician performance using audit and feedback: a systematic review. Am J Emerg Med. 2015;33(10):1505–1514. doi: 10.1016/j.ajem.2015.07.039 [DOI] [PubMed] [Google Scholar]
- 8.Rosenberg A, Agiro A, Gottlieb M, et al. Early Trends Among Seven Recommendations From the Choosing Wisely Campaign. JAMA Intern Med. 2015;175(12):1913–1920. doi: 10.1001/jamainternmed.2015.5441 [DOI] [PubMed] [Google Scholar]
- 9.Griffey RT, Jeffe DB, Bailey T. Emergency physicians’ attitudes and preferences regarding computed tomography, radiation exposure, and imaging decision support. Acad Emerg Med. 2014;21(7):768–777. doi: 10.1111/acem.12410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin MP, Nguyen T, Probst MA, Richardson LD, Schuur JD. Emergency Physician Knowledge, Attitudes, and Behavior Regarding ACEP’s Choosing Wisely Recommendations: A Survey Study. Acad Emerg Med. 2017;24(6):668–675. doi: 10.1111/acem.13167 [DOI] [PubMed] [Google Scholar]
- 11.Kanzaria HK, Hoffman JR, Probst MA, Caloyeras JP, Berry SH, Brook RH. Emergency physician perceptions of medically unnecessary advanced diagnostic imaging. Acad Emerg Med. 2015;22(4):390–398. doi: 10.1111/acem.12625 [DOI] [PubMed] [Google Scholar]
- 12.Casarett D The Science of Choosing Wisely — Overcoming the Therapeutic Illusion. New England Journal of Medicine. 2016;374(13):1203–1205. doi: 10.1056/NEJMp1516803 [DOI] [PubMed] [Google Scholar]
- 13.American College of Emergency Physicians. Reduce Avoidable Imaging Initiative. https://www.acep.org/Advocacy/Reduce-Avoidable-Imaging-Initiative/.
- 14.Center for Medicare and Medicaid Services. Inpatient Hospital Compare Preview Help Guide. https://www.qualityreportingcenter.com/globalassets/iqr_resources/prhc/pr_apr-2019_iphc-preview-report_helpguide_vfinal508.pdf. Published April 2019.
- 15.Wiler JL, Welch S, Pines J, Schuur J, Jouriles N, Stone- Griffith S. Emergency Department Performance Measures Updates: Proceedings of the 2014 Emergency Department Benchmarking Alliance Consensus Summit. Academic Emergency Medicine. 2015;22(5):542–553. doi: 10.1111/acem.12654 [DOI] [PubMed] [Google Scholar]
- 16.Prevedello LM, Raja AS, Zane RD, et al. Variation in Use of Head Computed Tomography by Emergency Physicians. The American Journal of Medicine. 2012;125(4):356–364. doi: 10.1016/j.amjmed.2011.06.023 [DOI] [PubMed] [Google Scholar]
- 17.Prabhakar AM, Gottumukkala RV, Hemingway J, Hughes DR, Patel SS, Duszak R. Increasing utilization of emergency department neuroimaging in Medicare beneficiaries from 1994 to 2015. The American Journal of Emergency Medicine. 2018;36(4):680–683. doi: 10.1016/j.ajem.2017.12.057 [DOI] [PubMed] [Google Scholar]
- 18.Levin DC, Parker L, Rao VM. Recent Trends in Imaging Use in Hospital Settings: Implications for Future Planning. Journal of the American College of Radiology. 2017;14(3):331–336. doi: 10.1016/j.jacr.2016.08.025 [DOI] [PubMed] [Google Scholar]
- 19.Viau JA, Chaudry H, Hannigan A, Boutet M, Mukarram M, Thiruganasambandamoorthy V. The Yield of Computed Tomography of the Head Among Patients Presenting With Syncope: A Systematic Review. Academic Emergency Medicine. doi: 10.1111/acem.13568 [DOI] [PubMed] [Google Scholar]
- 20.Greenwood-Ericksen MB, Tipirneni R, Abir M. An Emergency Medicine–Primary Care Partnership to Improve Rural Population Health: Expanding the Role of Emergency Medicine. Annals of Emergency Medicine. 2017;70(5):640–647. doi: 10.1016/j.annemergmed.2017.06.025 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


