Highlights
-
•
Complications after choledochal cyst resection are common, mainly anastomotic stricture, bowel obstruction, biliary fistula and pancreatic cyst remnant.
-
•
Reoperation is the optimal method for patients with pancreatic cyst remnant and hepaticojeju-nal anastomotic stricture.
-
•
ERCP, balloon dilation should be considered as a supporting tools to reduce the risk and mor-bidity of surgery.
Keywords: Choledochal cyst complications, Minimal invasive therapy, Remnant pancreatic duct cyst, Bilioenteric anastomotic stricture, Reoperation, Case report
Abstract
Introduction
Choledochal cyst is a rare benign congenital dilation of the bile duct, which causes recurring disturbing symptoms without totally resection. Nonetheless, postoperative complications are still a common issue. A step up management for patients with complex complications is required to address the problem.
Case presentation
We report a 10-year-old child who suffered complex postoperative complications after choledochal cyst resection at the age of 5, including cholangitis, bilioenteric stenosis and cystolithiasis in remnant intrapancreatic duct cyst. She occasionally endured episodes of epigastric pain, fever and jaundice afterwards. As the symptoms and recurrent rate were worsen over time, the patient was admitted multiple times and various approaches (balloon dilation, percutaneous transhepatic biliary drainage, endoscopic retrograde cholangiopancreatography and laparoscopic surgery) were applied. Afterwards, patient recovered and discharged without any complications.
Conclusion
Our case presented sophisticated complications relating to choledochal cyst that were successfully treated by a combination of modern minimal invasive techniques. Despite operated by experienced surgeons, the post-op complications are still a concerned problem due to difficult laparoscopic techniques, injuries of hepatic artery, infection and risk of malignancy. We suggested that minimal-invasive procedures should be considered first with the aim of relieving symptoms, biliary drainage and preparing for the reoperation.
1. Introduction
Choledochal cyst (CC) is defined as a congenital dilatation in extra or intra – hepatic part of biliary tree, mostly occurs in female and Asian population [1]. Patients will endure episodes of triad symptoms including abdominal pain, jaundice and abdominal mass. The risk of malignancy could reach over 10% at the age of 30 without proper treatment [2]. In most cases, the conditions could be treated by radical laparoscopic surgery [3]. However, patients could face various postoperative (post-op) complications (i.e. biliary fistula, bowel obstruction, intussusception, anastomotic stenosis and pancreatic cyst remnant) [1]. Stenosis of choledochal-jejunal anastomosis could occur as a consequence of small, tensive anastomosis, inflammation or infection. Besides, it was reported that a minority of patients may experience remnant intrapancreatic duct cyst, as it was not entirely resected during the first operation [4]. But rarely both happen in one patient and surgery is still a mainstay treatment for these complications. In this report, we introduce a 10-year-old girl case who suffered bilioenteric anastomotic stricture and remnant intrapancreatic duct cyst-originated stones that was successfully treated by multiple state-of-the-art tools. The work has been reported in line with SCARE criteria [5].
2. Case report
A 10-year old girl came to the hospital with the symptoms of fever, fatigue and abdominal pain. Her parents reported a history of laparoscopic operation at another center due to type I choledochal cyst at the age of 5, which had been identified after episodes of fever and jaundice since birth. The laparoscopic resection was conducted with cyst removal and hepatico-jejunal (HJ) anastomosis. Since then, abdominal pain and low-grade fever relapsed without signs of anastomotic stenosis and cystolithiasis three or five times each year. As the symptoms were worsen and the frequency increased, she was admitted and did a thorough examination. She had mild fever (around 38 °C), no sign of jaundice, intermittent pain in right upper quadrant 5–6 times per day. Her blood test showed the signs of infection, and amylase was higher than normal (twice-fold to upper limited normal value). The computed tomography (CT) scan (after 4 years since the first operation) showed a sign of common hepatic duct dilation and stones in the remnant pancreatic duct cyst (Fig. 1). Cholangiography and endoscopic retrograde cholangiopancreatography (ERCP) showed the stricture in bilioenteric anastomosis and pancreatic cyst remnant. We considered the minimal intervention since it was effective with the successful rate of more than 90% and without the risk of pancreatitis and severe infection when dissecting the pancreatic cyst. After excluding other causes of fever, the patient underwent balloon dilation (Fig. 2). The symptoms relieved and she was discharged 4 days afterwards.
Fig. 1.
CT-scan showed the stones in remnant pancreatic cyst duct (arrow) and HJ anastomosis (arrowhead).
Fig. 2.
Balloon dilation in hepaticojejunal anastomosis stenosis.
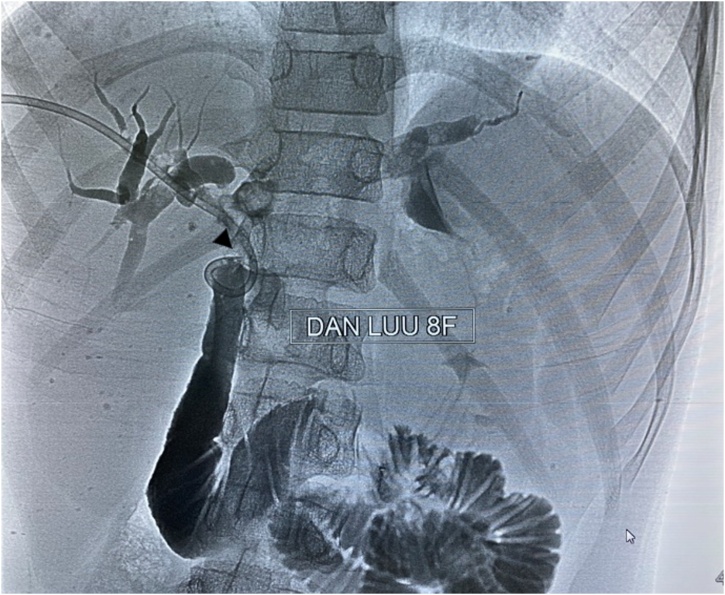
One month later, the symptoms reappeared and we spotted stones in proximally to the anastomosis as well as remnant duct. Liver function test deranged (AST/ALT was 64/95 U/L). The laboratory results did not show any sign of biliary obstruction (bilirubin was normal), ALP and GGT was not further examined. A biliary drainage was taken by radiologist to reduce the severity of infection and the risk of post-op fistula as the team planned for the second operation (Fig. 3).
Fig. 3.
Biliary drainage in the second hospitalization (arrowhead: proximal drainage end).
The operation was conducted after 14 days. Intraoperative findings revealed that the anastomosis was thickened and strictured due to inflammation. The HJ anastomosis was then opened and a stone was found in proximal margin of pancreatic cyst remnant. Thus, pancreatic cyst remnant with stone inside was also eliminated and clipped as well as new bilioenteric anastomosis was performed (Fig. 4). The biliary drainage was kept as a protective tool for avoiding bile leak and stenosis. Histopathology results showed the sign of inflammation in HJ anastomosis without any sign of malignancy. She was discharged 11 days after the operation without any complications. The follow‑up at 1 and 3 months showed remarkable improvement as physical conditions improved, laboratory results returned to normal value and MRI at 3 months illustrated a good anastamosis.
Fig. 4.
Minimal invasive surgery in stone removal (arrowhead) and redo HJ anastomosis.
3. Discussion
Choledochal cyst is classified into 5 types, with type I the most common form, in which the common bile duct but not intrahepatic duct is dilated. Our patient had type I cyst, hence it was removed during the first operation and a HJ anastomosis was performed.
Complications after laparoscopic choledochal cyst resection are common, including anastomotic stricture, pancreatic cyst remnant with lithogenesis. Anastomotic stricture is found in 2.5–17% of patients after biliary-enteric anastomosis [6]. The main causes include infection and inflammation, small diameter and tension. Yet an accepted definition for bilioenteric stricture has been published, some author defined as a radiologically demonstrated narrowing with relevant symptoms of obstructive (jaundice, cholangitis and deranged liver function) [6,7]. However, percutaneous transhepatic cholangiography has still been considered to achieve definitive diagnosis [8]. On the other hand, remnant choledochal cyst has been shown to increase the risk of malignancy. The mechanism of cancer development remains unclear, which may relate to inflammation, cell regeneration and DNA breaks caused by K-ras and p53 mutations [9]. Malignant cyst occurred mostly in type I and type IVa patients, followed by type V [9,10]. Both complications can affect patients’ quality of life as well as survival [11]. Thus, follow-up with awareness of likely complications is essential for early diagnosis and prompt treatment.
Complications usually occur separately in patients with choledochal cyst. To our best knowledge, there is still no literature case being reported a group of complications in one patient. Thus, a comprehensive and step up management is necessary to treat these conditions. Some authors pointed out that balloon dilation should be the first step as successful rate was 81%, whereas reoperation was considered as the final choice in all circumstances [12]. In addition, Sheng proposed that no delay in intervention should be showed in biliary obstruction [13]. Since the anastomosis’s quality depends on many factors as mentioned above and the risk of post-op pancreatitis is fairly high, balloon dilation should be performed first if possible. Balloon dilation was used for widening the anastomosis and reliving symptoms but was not the most effective method [14]. Although one-year success rate was reported as more than 90%, stenosis reoccurred after 1 month of intervention in our patient. Therefore, reoperation was inevitable and several approaches was considered including open/laparoscopic hepatico-jejunostomy, hepatico-duodenostomy (HD). Laparoscopic HJ anastomosis was then performed as the degree of adhesion was low, the blood loss as well as hospitalized days was demonstrated to be lowered and laparoscopic HD was associated with bile gastritis, duodenogastric reflux and harder to carry out [15,16]. Based on our personal experience, if patients have multiple lesions at once, preoperation intervention such as biliary drainage should be utilized to reduce post-op complications.
4. Conclusion
Choledochal cyst-related morbidities are still the concerned problem for doctors. The application of laparoscopic surgery has been showed to be effective. When re-operation is the optimal method, other tools should be used to prepare and reduce the risk and morbidity of surgery.
Conflicts of interest
None.
Funding
None.
Ethical approval
Informed consent was obtained from the parents for the report publication.
Consent
Informed consent was obtained from the parents for the report publication.
Author contribution
Hoa NT: Main surgeon
Phuong TH: Assistant surgeon
Ngoc NB: Assistant surgeon
Dung LT: Performed the percutaneous transhepatic cholangiography
Dang DH: Assistant surgeon, wrote manuscript
Hung NV: Wrote manuscript
Lan NT: Wrote manuscript
Tuan VH, Quan HQ, Chung VT, Trang DTH: Did the management strategy, the follow-up
Registration of research studies
No needed because it is not the first case conducted in human.
Guarantor
Hoa V. Nguyen, M.D, Ph.D.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Contributor Information
Hoa Viet Nguyen, Email: nvhoa96@yahoo.com.vn.
Dang Hai Do, Email: dangsp94@gmail.com.
Hung Van Nguyen, Email: dr.hungnguyen.hmu@gmail.com.
Tuan Hong Vu, Email: hongtuan@hmu.edu.vn.
Quan Quy Hong, Email: dr.hongquyquan@gmail.com.
Chung Ta Vo, Email: votachung214@gmail.com.
Trang Huyen Thi Dang, Email: trangtrocyhn@gmail.com.
Ngoc Bich Nguyen, Email: nguyenbichngocbeo@gmail.com.
Dung Thanh Le, Email: drdung74@gmail.com.
Phuong Ha Tran, Email: drphuongnt32@gmail.com.
Lan Thi Nguyen, Email: dr.nguyenlanvd@gmail.com.
References
- 1.Zhang B. Early complications after laparoscopic resection of choledochal cyst. Pediatr. Surg. Int. 2019;35(8):845–852. doi: 10.1007/s00383-019-04489-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin I.S. Biliary cystic disease: the risk of cancer. J. Hepatobiliary Pancreat. Surg. 2003;10(5):335–339. doi: 10.1007/s00534-002-0696-8. [DOI] [PubMed] [Google Scholar]
- 3.Soares K.C. Presentation and clinical outcomes of choledochal cysts in children and adults: a multi-institutional analysis. JAMA Surg. 2015;150(6):577–584. doi: 10.1001/jamasurg.2015.0226. [DOI] [PubMed] [Google Scholar]
- 4.Cheung T.T., Fan S.T. Technical note on complete excision of choledochal cysts. Hepatobiliary Pancreat. Dis. Int. 2013;12(2):218–221. doi: 10.1016/s1499-3872(13)60035-1. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 Statement: Updating Consensus Surgical CAse REport (SCARE) Guidelines. Int. J. Surg. 2018;60:132–1366. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 6.Kadaba R.S. Complications of biliary-enteric anastomoses. Ann. R. Coll. Surg. Engl. 2017;99(3):210–215. doi: 10.1308/rcsann.2016.0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.House M.G. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. Ann. Surg. 2006;243(5):571–578. doi: 10.1097/01.sla.0000216285.07069.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dimou F.M. Incidence of hepaticojejunostomy stricture after hepaticojejunostomy. Surgery. 2016;160(3):691–698. doi: 10.1016/j.surg.2016.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madadi-Sanjani O. Choledochal cyst and malignancy: a plea for lifelong follow-up. Eur. J. Pediatr. Surg. 2019;29(2):143–149. doi: 10.1055/s-0037-1615275. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe Y., Toki A., Todani T. Bile duct cancer developed after cyst excision for choledochal cyst. J. Hepatobiliary Pancreat. Surg. 1999;6(3):207–212. doi: 10.1007/s005340050108. [DOI] [PubMed] [Google Scholar]
- 11.Ronnekleiv-Kelly S.M. Management of choledochal cysts. Curr. Opin. Gastroenterol. 2016;32(3):225–231. doi: 10.1097/MOG.0000000000000256. [DOI] [PubMed] [Google Scholar]
- 12.Zhu J.Q. Bilioenteric anastomotic stricture in patients with benign and malignant tumors: prevalence, risk factors and treatment. Hepatobiliary Pancreat. Dis. Int. 2017;16(4):412–417. doi: 10.1016/S1499-3872(17)60033-X. [DOI] [PubMed] [Google Scholar]
- 13.Sheng Q. Reoperation after cyst excision with hepaticojejunostomy for choledochal cysts: our experience in 18 cases. Med. Sci. Monit. 2017;23:1371–1377. doi: 10.12659/MSM.900313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yamauchi H. Endoscopic balloon dilation for benign bilioenteric stricture: outcomes and factors affecting recurrence. Dig. Dis. Sci. 2019;64(12):3557–3567. doi: 10.1007/s10620-019-05811-3. [DOI] [PubMed] [Google Scholar]
- 15.Takada K. Duodenogastric reflux following biliary reconstruction after excision of choledochal cyst. Pediatr. Surg. Int. 2005;21(1):1–4. doi: 10.1007/s00383-004-1251-2. [DOI] [PubMed] [Google Scholar]
- 16.Javed A. Laparoscopic versus open surgery for the management of post-cholecystectomy benign biliary strictures. Surg. Endosc. 2020 doi: 10.1007/s00464-020-07496-6. [DOI] [PubMed] [Google Scholar]