Abstract
Coronavirus disease 2019 (COVID-19) has resulted in public health measures and health care reconfigurations likely to have impact on chronic disease care. We aimed to assess the volume and characteristics of patients presenting to hospitals with acute decompensated heart failure (ADHF) during the 2020 COVID-19 pandemic compared with a time-matched 2019 cohort. Patients presenting to hospitals with ADHF from March 1, to April 19, 2020 and 2019 in an urban hospital were examined. Multivariable logistic-regression models were used to evaluate the difference in probability of ADHF-related hospitalization between the 2 years. During the COVID-19 pandemic, a total of 1106 emergency department (ED) visits for dyspnea or peripheral edema were recorded, compared with 800 ED visits in 2019. A decrease in ADHF-related ED visits of 43.5% (14.8%-79.4%, P = 0.002) and ADHF-related admissions of 39.3% (8.6%-78.5%, P = 0.009) was observed compared with 2019. Patients with ADHF presenting to hospitals (n = 128) were similar in age, sex, and comorbidities compared with the 2019 cohort (n = 186); however, a higher proportion had recent diagnoses of heart failure. Upon ED presentation, the relative probability of hospitalization or admission to intensive care was not statistically different. There was a trend toward higher in-hospital mortality in 2020. The decline in ADHF-related hospitalizations raises the timely question of how patients with heart failure are managing beyond the acute-care setting and reinforces the need for public education on the availability and safety of emergency services throughout the COVID-19 pandemic.
Résumé
La maladie à coronavirus 2019 (COVID-19) a transformé les stratégies de santé publique et les soins de santé, ce qui risque d’avoir des répercussions sur les soins aux patients atteints d’une maladie chronique. Nous avons comparé le nombre de patients qui se sont présentés à l’hôpital en insuffisance cardiaque aiguë décompensée (ICAD) durant la pandémie de COVID-19 et leurs caractéristiques avec le nombre et les caractéristiques des patients traités durant la même période en 2019. Les dossiers des patients qui se sont présentés en ICAD à un hôpital urbain entre le 1er mars et le 19 avril en 2020 et en 2019 ont donc été examinés. La différence entre les probabilités d’hospitalisation pour ICAD en 2020 et en 2019 a été évaluée au moyen de modèles de régression logistique multivariés. Durant la pandémie de COVID-19, on a dénombré en tout 1 106 consultations au service des urgences en raison d’une dyspnée ou d’un œdème périphérique, comparativement à 800 consultations en 2019. Le nombre de consultations au service des urgences en raison d’une ICAD a quant à lui diminué de 43,5 % (14,8 % à 79,4 %, p = 0,002) et le nombre d’admissions à l’hôpital pour ICAD, de 39,3 % (8,6 % à 78,5 %, p = 0,009) de 2019 à 2020. Les patients atteints d’ICAD qui se sont présentés à l’hôpital (n = 128) en 2020 avaient les mêmes caractéristiques que ceux de la cohorte de 2019 (n = 186) pour ce qui est de l’âge, du sexe et des affections concomitantes; toutefois, la proportion de patients ayant récemment reçu un diagnostic d’insuffisance cardiaque était plus élevée. Au moment de la consultation au service des urgences, les probabilités relatives d’hospitalisation ou d’admission aux soins intensifs ne différaient pas de manière significative sur le plan statistique. On observe toutefois une tendance à la hausse du taux de mortalité hospitalière en 2020. Le recul du nombre d’hospitalisations pour ICAD soulève une question pertinente quant au sort des patients atteints d’insuffisance cardiaque en dehors du contexte des soins actifs et renforce la nécessité d’informer le public que les services d’urgence demeurent accessibles et sûrs pendant la pandémie de COVID-19.
Since December 2019, the severe acute respiratory syndrome coronavirus 2 and resultant coronavirus disease 2019 (COVID-19) has evolved into an international public health crisis, designated a pandemic as of March 11, 2020, by the World Health Organization.1 Observational studies have identified that patients with cardiovascular disease, including heart failure (HF), have higher risks of COVID-19–related complications and overall mortality.2
The implementation of public health measures aimed at mitigating the spread of COVID-19 and accompanying reconfigurations in health care delivery has affected care for HF. Patients with HF rely on intense regimens of clinical follow-up that may be subject to delay, cancellation, or transition to different platforms, leading to destabilization and risk of hospitalizations. The public lockdown is likely to have exerted unknown sequelae on the psychological, behavioural, and physical states of these patients. The objective of this study was to evaluate the volume and characteristics of patients presenting to hospitals with acute decompensated HF (ADHF) during the 2020 COVID-19 pandemic compared with a time-matched 2019 cohort.
We compared consecutive patients presenting with ADHF to the University Health Network (Toronto General Hospital and Toronto Western Hospital), in Toronto, Canada, from March 1, to April 19, 2020, and from March 1, to April 19, 2019 (time-matched control cohort). This timeframe contains the sentinel public lockdown in Ontario, Canada, of March 12, 2020. This study was approved by the Research Ethics Board (#20-5326). Inclusion criteria consisted of adults patients (≥ 18 years) presenting either to the emergency department (ED) (with triage diagnoses of “shortness of breath” or “leg swelling/edema”) or as direct admission from ambulatory clinics (with an admitting diagnoses of “heart failure”) who had ADHF, defined by brain natriuretic peptide (BNP) of ≥ 100 pg/mL or left-ventricular ejection fraction (LVEF) by echocardiography within the last year or during the index hospitalization of ≤50%, along with clinical records recording a diagnosis of ADHF, based on compatible clinical symptoms. Patients were excluded if they had implantable ventricular assist devices or cardiac transplants, high BNP secondary to severe pulmonary disease, or ADHF secondary to acute coronary syndrome (ACS). Informed consent was obtained for patients whose data were collected prospectively from April 10, 2020, onward; consent was waived for patients included retrospectively.
We screened electronic medical records of all patients presenting to emergency departments and those directly admitted from ambulatory clinics with the prespecified triage or admitting diagnosis codes for study eligibility. We extracted clinical and laboratory data from electronic medical records, including demographics, comorbidities, HF characteristics, physical examination parameters, and laboratory data. COVID-19 status was determined in the 2020 patient cohort, according to institutional guidelines, using nasopharyngeal swab testing. We collected information on the number of ED visits for patients presenting with dyspnea or peripheral edema and with ADHF specifically. For patients hospitalized with ADHF, data on admission to intensive care units, and in-hospital mortality were abstracted.
For analysis, we compared characteristics of patients with ADHF seen during the 2020 pandemic with the 2019 time-matched cohort using Wilcoxon rank-sum tests and χ2 or Fisher’s exact tests for continuous and categorical variables, respectively. We used a generalized linear mixed model with random intercepts corrected for time as a weekly variable to estimate the percent change in ED visits of patients complaining with dyspnea or peripheral edema, ED visits for ADHF, and hospitalizations for ADHF during the pandemic and previous year. We used multiple logistic regression models to evaluate whether the odds of hospitalization after presenting to the emergency department with ADHF differed by timeframe after taking into account patient characteristics. All statistical analyses were performed using Stata 16 (StataCorp, College Station, TX).
Initial Clinical Experience
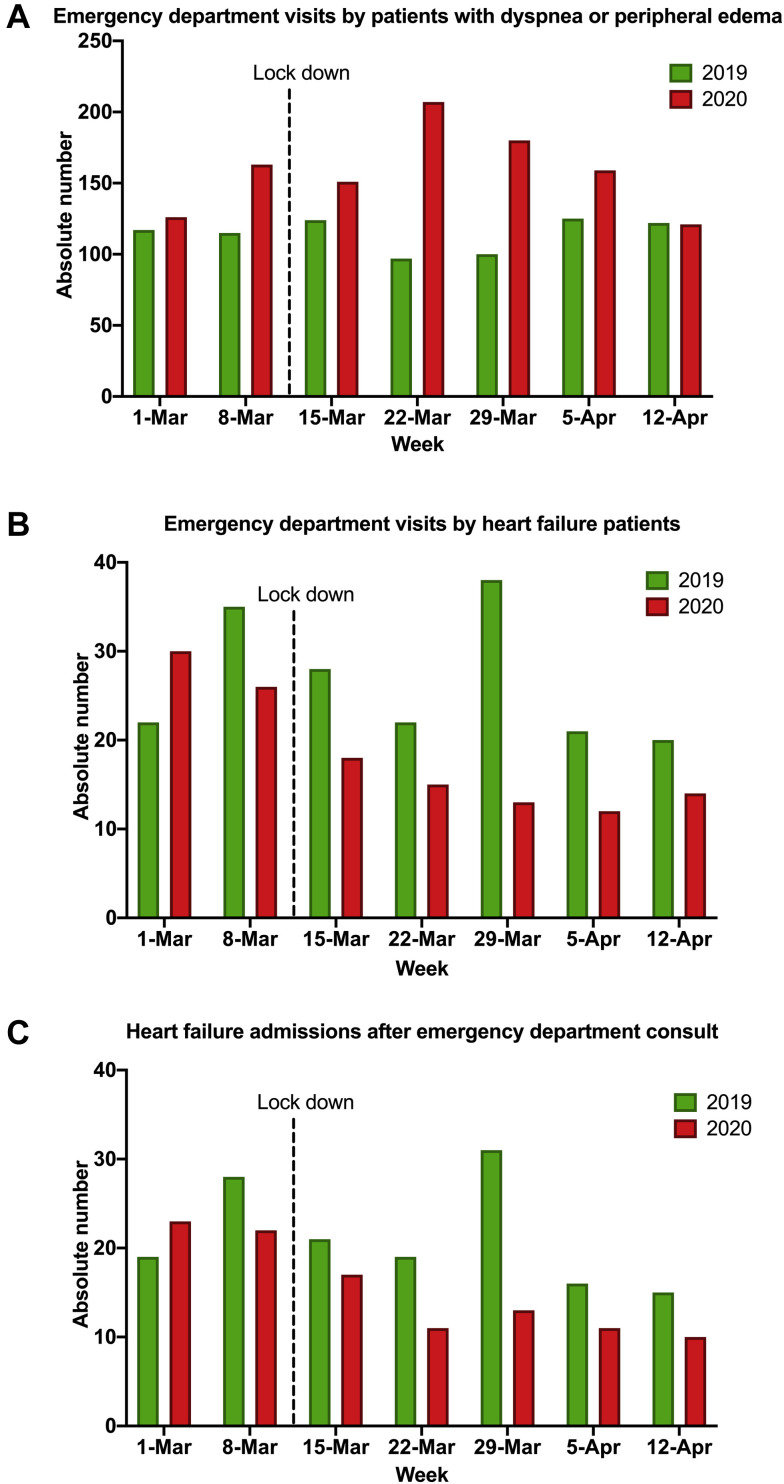
ED volume
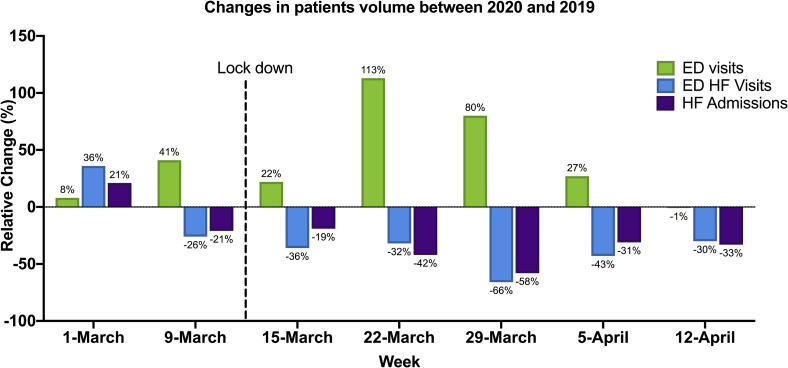
From March 1, to April 19, 2020, a total of 1106 ED visits for dyspnea or peripheral edema were recorded, compared with 800 ED visits during the same timeframe in 2019. Of the patients presenting to the emergency department, 128 had diagnoses of ADHF in 2020, with 107 hospitalized, compared with 186 in 2019, with 149 hospitalized (Fig. 1 ). Of patients hospitalized with ADHF, 16 (15.0%) and 28 (18.8%) were admitted directly from ambulatory clinics in 2020 and 2019, respectively. By mixed-method modelling, there was an average increase in total ED visits of 38.3% (26.3%-51.6%, P < 0.001), average decrease in ADHF-related ED visits of 43.5% (14.8%-79.4%, P = 0.002), and average decrease in ADHF-related hospitalizations of 39.3% (8.6%-78.5%, P = 0.009) between 2020 and 2019. These changes were more significant following the declaration of a public lockdown in Ontario, with an observed increase in total ED visits of 44.0% (29.4%-60.3%, P < 0.001), a decrease in ADHF-related ED visits of 79.2% (34.3%-139.0%, P < 0.001), and a decrease in ADHF-related hospitalizations of 64.5% (20.0%-225%, P = 0.002). Figure 2 exhibits the weekly changes in ED visits and hospitalization volumes over time.
Figure 1.
Patients presenting to the emergency department with dyspnea or peripheral edema (A), with acute decompensated heart failure (ADHF) (B), and with AHDF-related hospitalization (C). The differences in the volume of patients presenting to the emergency department and hospitalized with ADHF between March 1, and April 19 in 2019, and 2020 were more pronounced after the announcement of a provincial lockdown.
Figure 2.
Volume of patients presenting to hospital with dyspnea or peripheral edema and specifically with acute decompensated heart failure (ADHF) between March 1 and April 19 in 2019 and 2020. There was an average increase in total emergency deaprtment (ED) visits of 38.3% (26.3%-51.6%, P < 0.001), average decrease in ADHF-related ED visits of 43.5% (14.8%-79.4%, P = 0.002), and average decrease in ADHF-related hospitalizations of 39.3% (8.6%-78.5%, P = 0.009) between 2020 and 2019. These changes were more significant following the declaration of a public lockdown in Ontario, with an observed increase in total ED visits of 44.0% (29.4%-60.3%, P < 0.001), a decrease in ADHF-related ED visits of 79.2% (34.3%-139.0%, P < 0.001), and a decrease in ADHF-related hospitalizations of 64.5% (20.0%-225%, P = 0.002).
Patients presenting to hospitals with ADHF
The demographic characteristics of patients presenting to hospitals with ADHF were not significantly different between years. The median population age was 75 years; 161 (51%) patients were female, and 81 (26%) had underlying ischemic cardiomyopathies. A higher proportion of patients presenting in 2020 did, however, have more recent diagnoses of HF. A comparable proportion of patients were on guideline-directed medical therapy.
By multivariable analysis, odds of hospitalization following ED presentation for ADHF was not significantly increased (odds ratio [OR], 1.07; 95% confidence interval [CI], 0.52-2.27) in 2020 compared with 2019 after adjusting for age, sex, LVEF, body mass index (BMI), New York Heart Association (NYHA) functional class, recency of HF diagnosis, hypertension, systolic blood pressure, heart rate, and respiratory rate. Similarly, the odds of being hospitalized was not significantly different for patients presenting to emergency departments post-lockdown vs the 2019 time-matched cohort (adjusted OR, 0.66; 95% CI, 0.26-1.69); neither was the probability of being admitted to intensive care units. Among patients hospitalized with ADHF, there was a trend toward higher in-hospital mortality in 2020. The Supplementary Material features an extended version of the study findings.
Impact of COVID-19 pandemic on patients with HF
As a testament to the collateral damage of the COVID-19 pandemic, parallel trends in the volume of patients seeking medical care for non–COVID-19 medical concerns have been witnessed in jurisdictions around the world. In a retrospective analysis of 15 centres in the United States, a 43% reduction in hospitalization rates for acute cardiovascular conditions, including HF, ACS, and stroke from January to March 2020, was observed when compared with 2019, mirroring trends in the decline of ACS across the world.3 In Mississippi, a 50% decline in the number of hospitalizations for HF has been noted, mirrored by a likewise dramatic decline in HF hospitalizations in New York City.4 , 5
The observed phenomenon of reduced ADHF-related ED visit and hospitalization volumes is likely secondary to a complex interplay of public health and social factors. It is conceivable that fear of acquisition of COVID-19 associated with the medical environment, and strict social isolation imperatives, may have prejudiced patients with HF to either attempt to self-manage their conditions at home or defer pursuit of medical care. Conversely, public health measures resulting in limited access to the commercial food industry, increased medication adherence in the absence of otherwise habitual diversions (eg, work, travel), increased time for leg elevation, and lower total daily energy expenditure may be contributors to lower ADHF In addition, increased access to medical care via telecommunication may have resulted in more rapidly available follow-up and management, obviating the need for ADHF-related admission.
An important query raised by the decline in ADHF-related ED visits observed in this study pertains to the state of health and vital status of patients with HF who are no longer being seen in acute hospital settings, highlighting the critical and timely question of “where have all the patients gone?” An understanding of patients’ perspectives driving their behaviour is needed to target and mitigate deleterious health decisions. The reduced volume of patients presenting and hospitalized with ADHF may inevitably engender higher morbidity and mortality in the coming months. Ongoing surveillance of the cascade of the pandemic’s consequences on rates of adverse outcomes in patients presenting with ADHF is warranted to provide valuable lessons in cardiovascular patient care. Ongoing public education efforts on the continued availability of emergency care services and importance of seeking timely medical care, in addition to the close surveillance and management of patients with HF by clinicians throughout the COVID-19 pandemic, are likely needed.
Conclusions
Our description of the trends in ADHF-related ED volumes and hospitalization rates offers early insight into the indirect effects of the COVID-19 pandemic on patient care. Management of chronic HF is likely to be an integral component of the health system’s response to the COVID-19 pandemic, both in protecting this vulnerable population from acute and severe decompensations and in reducing the burden on hospital resources. The precipitous decline observed in ADHF-related ED visits and hospitalizations raises the timely question of how these patients are managing beyond the acute-care setting and reinforces the need for broad public education on the continued availability and safety of emergency services throughout the COVID-19 pandemic.
Funding Sources
The authors have reported that they have received no funding relevant to the contents of this paper.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 1684 for disclosure information
To access the supplementary material accompanying this article, visit the online version of the Canadian Journal of Cardiology at www.onlinecjc.ca and at https://doi.org/10.1016/j.cjca.2020.07.006.
Supplementary Material
References
- 1.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Madjid M., Safavi-Naeini P., Solomon S.D., Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020 Jul 1;5:831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 3.Bhatt A.S., Moscone A., McElrath E.E. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J AM Coll Cardiol. 2020;76:280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall M.E., Vaduganathan M., Khan M.S. Reductions in heart failure hospitalizations during the COVID-19 pandemic. J Card Fail. 2020;26:462–463. doi: 10.1016/j.cardfail.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barghash M.H., Pinney S.P. Heart failure in the COVID-19 pandemic: Where has all New York’s congestion gone? J Card Fail. 2020;26:477–478. doi: 10.1016/j.cardfail.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.