Abstract
To control the novel coronavirus disease (COVID-19) outbreak, state and local governments in the United States have implemented several mitigation efforts that resulted in lower emissions of traffic-related air pollutants. This study examined the impacts of COVID-19 mitigation measures on air pollution levels and the subsequent reductions in mortality for urban areas in 10 US states and the District of Columbia. We calculated changes in levels of particulate matter with aerodynamic diameter no larger than 2.5 μm (PM2.5) during mitigation period versus the baseline period (pre-mitigation measure) using the difference-in-difference approach and the estimated avoided total and cause-specific mortality attributable to these changes in PM2.5 by state and district. We found that PM2.5 concentration during the mitigation period decreased for most states (except for 3 states) and the capital. Decreases of average PM2.5 concentration ranged from 0.25 μg/m3 (4.3%) in Maryland to 4.20 μg/m3 (45.1%) in California. On average, PM2.5 levels across 7 states and the capital reduced by 12.8%. We estimated that PM2.5 reduction during the mitigation period lowered air pollution-related total and cause-specific deaths. An estimated 483 (95% CI: 307, 665) PM2.5-related deaths was avoided in the urban areas of California. Our findings have implications for the effects of mitigation efforts and provide insight into the mortality reductions can be achieved from reduced air pollution levels.
Keywords: Air pollution, COVID-19, Mitigation, Mortality reduction
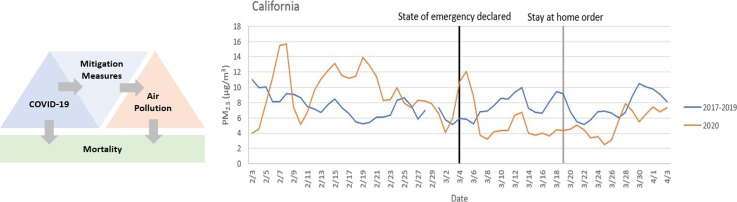
Graphical abstract
Highlights
-
•
PM2.5 levels during COVID-19 mitigation decreased across 7 states and the capital.
-
•
PM2.5 reduction during COVID-19 mitigation is estimated to lowered air pollution-related deaths.
-
•
Findings have implications for the indirect health effects of mitigation efforts.
-
•
Results have implications for potential health benefits from air pollution policy.
1. Introduction
A novel coronavirus disease (COVID-19) is causing a global pandemic with approximately 233,411 deaths worldwide as of April 30, 2020 (Worldmeter, 2020). State and local governments in the United States have implemented several mitigation efforts such as stay-at-home measures aimed at lowering the contact rate through social/physical distancing to reduce COVID-19 transmission. Although responses to COVID-19 are varied across states, these measures have generally reduced level of traffic-related air pollution. Similar phenomena were observed elsewhere, with recent studies finding dramatic decline in air pollution levels in China due to quarantine measures (Chen et al., 2020; Dutheil et al., 2020; Isaifan, 2020). Ambient air pollution is linked with a range of adverse health outcomes such as mortality, hospital admissions, emergency room visits, and respiratory symptoms through several pathways (e.g., oxidative lung damage and inflammation, hypoxemia, elevated plasma viscosity) (Pope 3rd, 2000; Samet and Krewski, 2007). Therefore, policies aimed at addressing the public health consequences of COVID-19 may have indirect health benefits through lower levels of air pollution. This is one of the many pathways through which the virus could indirectly impact health, such as through increases in domestic violence, psychiatric illness and emotional distress, harmful alcohol and drug use, and suicidal behavior, among many others (Graham-Harrison et al., 2020; Kumar and Nayar, 2020). This study investigated the impacts of COVID-19 mitigation measures on air pollution levels and the potential subsequence reductions in mortality for 8 US states and the District of Columbia.
2. Methods
To estimate the impacts of COVID-19 mitigation measures on air pollution levels and related reductions in mortality, we calculated changes in levels of particulate matter with aerodynamic diameter no larger than 2.5 μm (PM2.5) and the estimated avoided total and cause-specific mortality attributable to these changes in PM2.5 by state and district for 8 US states and the District of Columbia. Implementation of mitigation measures varied by US state and district as each area declared a state of emergency at different times (Table 1 ). We defined the baseline period (pre-mitigation measure) as the 30 days before the emergency declaration date and the mitigation period (during the mitigation measure) as the 30 days after the emergency declaration was enacted by each state or district. For this study, we selected 10 states (California, Connecticut, Florida, Maryland, Massachusetts, New Jersey, New York, Pennsylvania, Texas, and Washington) and the capital (Washington, D.C.) based on the high numbers of confirmed cases and deaths from COVID-19. We obtained monitor values of daily concentrations of PM2.5 for each state and the District from the U.S. Environmental Protection Agency (EPA) AirNow (U.S. EPA, n.d.). For states, we first calculated county-specific averages (i.e., average across all monitors within a county) and then state-specific averages (i.e., population-weighted average across counties within a state) for each period (baseline and mitigation period) using the Vintage 2018 postcensal estimates of the resident population released by National Center for Health Statistics (NCHS) to calculate death rates (NCHS, 2019). As monitors were not available for all locations throughout the states, we only included counties with monitors. As air pollution monitoring networks are more likely to be located in urban locations (Bravo et al., 2017), the states in this study represent the more urban areas within the states, not the entire states. We then quantified air pollution changes by calculating changes in PM2.5 concentration during the mitigation period compared to the baseline period for each of the 11 spatial units (10 states and the District). We compared average concentrations of PM2.5 during the mitigation measures (mitigation period) with those during the pre-emergency declaration measures (baseline period), by state/district. We compared these changes with those based on a difference-in-difference approach using the air pollution levels from 2017 to 2019 (Wing et al., 2018). In this approach, we compared two differences: (1) the difference in PM2.5 concentration during the mitigation measure (mitigation period) versus pre-mitigation measure (baseline period) in 2020 (EM-EB); and (2) the difference during the mitigation measure (mitigation period) versus pre-mitigation measure (baseline period) in 2017–2019 (CM-CB). The changes in PM2.5 concentration that are related to implementation of mitigation measure beyond background trends (e.g., seasonality) can be estimated as follows: (EM-EB)-(CM-CB). The difference-in difference analysis has a parallel trends assumption that the trends in outcomes (i.e., PM2.5 level) between the treated (i.e., year 2020) and control (i.e., 2017–2019) groups are the same prior to the intervention. If the assumption is satisfied, it is reasonable to assume that these parallel trends of PM2.5 concentration over time would be the same for both groups. We tested this assumption using a regression model by assessing the significance of the interaction term between time and pre-mitigation period. We found that coefficient for the interaction term is statistically insignificant, which suggests that the parallel trend assumption for difference-in-difference approach is plausible.
Table 1.
Date of some COVID-19 mitigation-related executive orders by state and the District.
Note: Each government involves a series of executive orders and policies, a subset of which are listed here. Other policies that affect air pollution such as guidance from local governments and corporations' work-from-home orders, etc. are not included but also likely impacted levels of air pollution.
| State | Date of executive orders |
|---|---|
| California | March 4, 2020: State of emergency declared March 12, 2020: Further respond to COVID-19 pandemic March 19, 2020: Stay at home order |
| Connecticut | March 10, 2020: State of emergency declared March 12, 2020: Prohibition of large gatherings, limits on nursing home visitors, waiver of 180-day school year etc. March 15, 2020: Canceled classes in public schools March 23, 2020: Restrictions on workplaces for non-essential business, stay at home |
| Florida | March 9, 2020: State of emergency declared April 3, 2020: Stay at home order |
| Maryland | March 5, 2020: State of emergency declared |
| March 12, 2020: Prohibiting large gatherings and events and closing senior centers | |
| March 30, 2020: Stay at home order | |
| Massachusetts | March 10, 2020: State of emergency declared |
| March 13, 2020: Prohibiting gatherings of more than 250 people | |
| March 15, 2020: Closure of all public and private schools | |
| March 24, 2020: Closing nonessential business and organizations, stay at home | |
| New Jersey | March 9, 2020: State of emergency declared March 16, 2020: Limits on gatherings of 50 or more; closure of all schools, closure of racetracks, casinos; restaurant restrictions March 21, 2020: Stay at home order |
| New York | March 7, 2020: State of emergency declared March 18, 2020: Closure of all schools March 22, 2020: Closure of nonessential business and bans of gatherings of any size, stay at home |
| Pennsylvania | March 6, 2020: State of emergency declared April 1, 2020: Statewide stay at home order |
| Texas | March 13, 2020: State of emergency declared April 2, 2020: Stay at home order |
| Washington state | February 29, 2020: State of emergency declared March 13, 2020: School closure March 23, 2020: Stay at home order |
| Washington D.C. | March 11, 2020: State of emergency declared March 24, 2020: Closure of non-essential businesses and prohibition on large gatherings April 1, 2020: Stay at home order |
Source: The Council of State Governments. State executive orders. https://web.csg.org/covid19/executive-orders/
We then estimated the avoided mortality attributable to PM2.5 changes based on the concentration-response function from a previous study and 2018 total and cause-specific mortality data from the Centers for Disease Control and Prevention (CDC) WONDER database (CDC and NCHS, n.d.; Krewski et al., 2009). To quantify PM2.5-related mortality, we chose Krewski et al. (2009) study used by the US EPA to quantify health risk assessment for PM2.5 (US EPA, 2010). US EPA chose Krewski et al. (2009) study for several reasons: (1) the cohort includes both men and women regardless of underlying health status; (2) the study includes data from cities from across the US; (3) the analysis has rigorous examination of model forms and effect estimates; and (4) the study includes coverage for extensive ecological variables (US EPA, 2010).
We used the following equation to estimate avoided total and cause-specific death associated with changes in PM2.5 exposure using the concentration-response function from Krewski et al. (2009) as applied by US EPA:
where ΔMi,j is the avoided death due to a particulate disease j (total or cause-specific mortality) for area i (specific US state or the District), Yi,j is the baseline mortality for disease j for area i, βj is the cause-specific effect estimates provided by Krewski et al. (Supplementary Table 1), ΔPM2.5i is the change in PM2.5 for area i, and Pi is the exposed adult population (above 30 years of age) for area i (i.e., population of included counties that have monitor(s) within state).
3. Results
3.1. Change in air pollution
The percentage of included counties of each state or district ranged from 11.4% in Texas to 100% in Washington D.C., with average of 55.5% across states/district. The population covered by the monitoring network for each area ranged from 59.3% in New Jersey to 100% in Washington D.C. Supplementary Fig. 1 shows PM2.5 levels before and throughout various COVID-19 measures for the 10 states and the District of Columbia, and comparable levels in previous years (2017–2019) for comparison. PM2.5 concentrations in Supplementary Fig. 1 represent the population-weighted average PM2.5 levels across counties with monitors within a state, not the whole state. The numbers of counties with monitors included in this study and total number of counties included for each state/district are provided in Table 2 . Results using the difference-in-difference approach generally indicated lower reductions in air pollution, but smaller reductions and not in all locations, with average reduction of 0.5 μg/m3 as opposed to 1.2 μg/m3, and the most consistent results for California (Table 2, Supplementary Fig. 1, Supplementary Table 2).We found that PM2.5 concentration during the mitigation period (after implementing the mitigation measures) decreased for most states (although not for Pennsylvania, Texas, and Washington state) and the capital. Except for 3 states, decreases of average PM2.5 concentration ranged from 0.25 μg/m3 (4.3%) in Maryland to 4.20 μg/m3 (45.1%) in California. On average, PM2.5 levels across 7 states and the capital reduced by 12.8%. The states/district with the highest baseline levels generally had larger percent reductions in air pollution (Table 2, Supplementary Fig. 1, Supplementary Table 2).
Table 2.
Average change in PM2.5 concentration during mitigation periods between 2020 and the comparable dates for 2017–2019, by state and the District, based on difference-in-difference approach.
| State/district⁎ | No. of counties included/total No. counties | Mitigation vs baseline period for 2020 | Mitigation vs baseline period for 2017–2019 | Difference in difference |
|---|---|---|---|---|
| California | 41/58 | −4.03 | 0.18 | −4.20 |
| Connecticut | 5/8 | −2.97 | −1.72 | −1.25 |
| Florida | 28/67 | 0.44 | 0.94 | −0.50 |
| Maryland | 11/24 | −1.26 | −1.01 | −0.25 |
| Massachusetts | 11/14 | −2.06 | −1.47 | −0.59 |
| New Jersey | 11/21 | −1.94 | −1.24 | −0.70 |
| New York | 18/62 | −2.27 | −1.70 | −0.57 |
| Pennsylvania | 28/67 | −1.48 | −1.49 | 0.01 |
| Texas | 29/254 | 2.91 | 0.78 | 2.13 |
| Washington state | 30/39 | −0.11 | −1.28 | 1.17 |
| Washington, D.C. | 1/1 | −0.84 | −0.45 | −0.39 |
States represent the portion of states with monitoring networks. PM2.5 levels are population weighted.
3.2. Changes in health estimates
We estimated that PM2.5 reduction during the mitigation period lowered PM2.5-related total and cause-specific deaths (Table 3 ). We estimated a total of 483 (95% CI: 307, 665) avoided PM2.5-related deaths in the urban areas of California, where the 95% confidence intervals are based on those from the concentration-response function in the epidemiological research. Avoided PM2.5-related deaths for cardiopulmonary, ischemic heart disease, and lung cancer were 207 (95% CI: 132, 286), 69 (95% CI: 44, 96), and 20 (95% CI: 13, 28) in California, respectively.
Table 3.
Estimated avoided adult (over 30 years) deaths due to air pollution reduction (PM2.5) during the COVID-19 measures for urban areas, by state and the District, for the first 30 days after the declared state of emergency.
| State/district⁎ | Covered population (%) of each state/district | Total | Cardiopulmonary | Ischemic heart disease | Lung cancer |
|---|---|---|---|---|---|
| California | 96.9 | 483 (307, 665) | 207 (132, 286) | 69 (44, 96) | 20 (13, 28) |
| Connecticut | 87.9 | 15 (10, 21) | 6 (4, 8) | 2 (1, 3) | 1 (0, 1) |
| Florida | 78.8 | 35 (22, 48) | 15 (9, 20) | 5 (3, 7) | 2 (1, 3) |
| Maryland | 71.1 | 4 (2, 5) | 2 (1, 2) | 1 (0, 1) | 0 (0, 0) |
| Massachusetts | 95.9 | 15 (9, 20) | 5 (3, 8) | 2 (1, 2) | 1 (0, 1) |
| New Jersey | 59.3 | 13 (8, 18) | 5 (3, 7) | 2 (1, 2) | 1 (0, 1) |
| New York | 80.6 | 30 (19, 42) | 14 (9, 19) | 6 (4, 9) | 1 (1, 2) |
| Washington, D.C. | 100.0 | 1 (1, 1) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
Note: In this Table, we excluded Pennsylvania, Texas, and Washington state to estimate avoided adult deaths due to air pollution reduction as those states did not show air pollution reduction during the first 30 days of mitigation period.
States represent the portion of states with monitoring networks.
4. Discussion
These estimates are based on lowered PM2.5 levels, the association between PM2.5 and mortality from previous epidemiological research, and county-level baseline adult mortality and population from CDC database. Results give insight into air pollution-related mortalities avoided by the COVID-19 mitigation measures, but should be interpreted with caution due to uncertainty in several areas. Importantly, the original concentration-response function is based on an association between outdoor air pollution levels and mortality based on activity patterns that have changed under current conditions (e.g., changes in activity patterns (indoor/outdoor) due to COVID-19 mitigation measures) and is based on long-term exposure. Ambient air quality may improve due to reduced outdoor activities due to COVID-19 mitigation measures, however indoor air pollution exposure during the mitigation period may increase due to increased time spent indoors leading to high exposure to household air pollution, such as from by cooking and use of consumer products (Anthes, 2020). Estimating the change in air pollution under the pandemic is challenging due to the decision needed about the baseline level for comparison, as demonstrated by different results for our two approaches. Results for two approaches are most consistent for California (PM2.5 reductions of 4.0 to 4.2 μg/m3).
Our study does not incorporate changes in chemical composition and sources of PM2.5, which may have changed due to COVID-19 mitigation policy. The chemical composition of PM2.5 varies with location, time, and season due to differences in pollutant sources including natural sources (e.g., wildfires), transportation, manufacturing or power plants (Adams et al., 2015; Bates et al., 2018). Mixtures of chemical constituents of PM2.5 from various emission sources show strong regional patterns across the US (Bell et al., 2007; Meng et al., 2018). Health impacts of PM2.5 appear to differ by its chemical composition (Adams et al., 2015; Bell, 2012). Presumably, changes in baseline activities, transportation, and major vehicle types (diesel-, leaded-gasoline-, and unleaded-gasoline-fueled vehicles) following the mitigation policies of COVID-19 could have altered the chemical composition of the particle mixture after the declared state of emergency, and these changes would further have different patterns in each state. Thus, the exposure-response functions of PM2.5 may have changed in our study period compared to the time period of the original epidemiological analysis. Further, studies indicate that short-term and long-term exposures to air pollution have different magnitude of mortality effects as findings vary among studies (Beverland et al., 2012; Cai et al., 2016; COMEAP, 2010). We note our limitation that adopting exposure-response functions from previous long-term exposure study for our 30-day exposure period may obscure more accurate quantification of mortality reduction due to air pollution level changes following the mitigation measures of COVID-19. Our exposure period is a month, whereas most studies examine exposure of a single day or few days or longer-term exposure of a year or several years, whereas our exposure period fits neither of these exposure metrics perfectly. Our results on the reduced PM2.5-related mortality does not represent potential mortality reduction of all populations in each state since counties without monitoring data were excluded in our analysis. We did not distinguish the mortality reductions for subgroups of sex or race/ethnicity.
Lower levels of air pollution have been documented during the COVID-19 pandemic. In Hubei province, where COVID-19 related mitigation measures were implemented on January 23, 2020, PM2.5 and nitrogen dioxide (NO2) levels were shown to have decreased in the weeks that followed (Chen et al., 2020). In the United States, estimates using satellite imagery indicate as much as a 30% reduction in air pollution levels compared to the same weeks of the previous year (NASA, 2020). Globally, reduction estimates range from 9% to 29%, depending on the air pollutant (Venter et al., 2020). Such a magnitude of reduction in air pollution during the COVID-19 pandemic is comparable to events such as the 2008 Beijing Olympics, during which air pollution levels were estimated to be approximately 10% lower (Wang et al., 2009). In the months during and immediately after the 2008 Beijing Olympics, the health status of the population in areas of reduced air pollution levels appeared to improve (Rich et al., 2012; Rich et al., 2015). Other researchers also hypothesized that reductions in air pollution during the COVID-19 pandemic could lead to avoided premature deaths due to reductions in air pollution exposure (Venter et al., 2020).
Air pollution and COVID-19 may be linked through pathways beyond reduced exposure resulting from mitigation measures. Ambient air pollution has been suspected to increase the risk of respiratory viruses (Contini and Costabile, 2020). Findings from recent studies suggest that areas with higher air pollution may have higher mortality risks associated with COVID-19. After adjusting for a range of potentially confounding factors (e.g. population density, socioeconomic status, weather), counties in the U.S. with higher long-term levels of PM2.5 had higher death rates attributable to COVID-19 (Wu et al., 2020). A similar analysis by Liang et al. (2020) found significant association between county-level long-term NO2 exposure and COVID-19 case-fatality and mortality rates, but not with PM2.5 or ozone (O3). A recent European study found that 78% of the COVID-19 deaths across 66 administrative regions in Italy, Spain, France and Germany occurred in the five regions with the highest NO2 levels (Ogen, 2020). Other studies also found positive associations between air pollution and the risk of COVID-19, after adjusting for potential confounders. Long-term average concentrations of NO2, O3, PM2.5, and particles with aerodynamic diameter ≤ 10 μm (PM10) were positively associated with confirmed cases in Italian provinces (Fattorini and Regoli, 2020). Findings of a Chinese study suggest that even shorter-term exposure (e.g., two weeks) to PM2.5, PM10, O3, and NO2 was associated with a higher number of daily confirmed cases (Zhu et al., 2020). Although these studies are rather preliminary, these findings suggest that long-term exposure to air pollutants increase vulnerability to severe COVID-19 outcomes. These findings of links between air pollution levels and COVID-19 warrant further research, but may relate to reduced host immune response, prolonged systemic inflammation, and chronic respiratory conditions due to air pollution exposures (Conticini et al., 2020; Rivellese and Prediletto, 2020). Air pollution is linked with several comorbidities that have been associated with poor diagnosis and higher mortality risk among COVID-19 patients. As more accurate data on the number of COVID-19 cases at a finer spatial scale and over a longer period of time become available, the complex relationship between air pollution, COVID-19, and health can be better disentangled with improved study designs.
Our results highlight one of the many complex pathways through which the economic, social, and cultural transitions of COVID-19 are impacting health. In the U.S., the public health burden of COVID-19 overwhelmingly outweighs these avoided mortalities from reduced air pollution. On the other hand, very stringent lockdowns were placed in China, leading to significant decrease in air pollution levels, and one study reported that the number of lives that were saved due to the decrease in air pollution potentially outnumbered the number of deaths directly due to COVID-19 in China (Chen et al., 2020). Findings linking the resulting decrease in air pollution with health benefits during this pandemic give insight into the extent to which aggressive air pollution mitigation policies can potentially reduce the public health burden of air pollution.
In this study, we observed that the mitigation measures to reduce the COVID-19 transmission led to improved air quality, which is estimated to result in lowered mortality due to the harmful mixture of particles from combustion such as through vehicle emissions. Clearly, the stark mitigation measures are not appropriate pathways to improve air quality, but our findings provide an insight for efforts to reduce ambient air pollution and show evidence of potential health benefits through the policy of air pollution control and restriction.
Funding sources
This publication was developed under Assistance Agreement No. RD835871 awarded by the U.S. Environmental Protection Agency to Yale University. It has not been formally reviewed by EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the Agency.
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R01MD012769. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CRediT authorship contribution statement
Ji-Young Son: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing. Kelvin C. Fong: Writing - review & editing. Seulkee Heo: Writing - review & editing. Honghyok Kim: Writing - review & editing. Chris C. Lim: Writing - review & editing. Michelle L. Bell: Writing - review & editing, Supervision.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Editor: Jay Gan
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2020.141012.
Appendix A. Supplementary data
Supplementary material
References
- Adams K., Greenbaum D.S., Shaikh R., van Erp A.M., Russell A.G. Particulate matter components, sources, and health: systematic approaches to testing effects. J. Air Waste Manage. Assoc. 2015;65(5):544–558. doi: 10.1080/10962247.2014.1001884. [DOI] [PubMed] [Google Scholar]
- Anthes E. Scientific American. Munn&Co; New York: 2020. Coronavirus lockdowns may raise exposure to indoor air pollution. (June 1) [Google Scholar]
- Bates J.T., Weber R.J., Verma V., Fang T., Ivey C., Liu C. Source impact modeling of spatiotemporal trends in PM2.5 oxidative potential across the eastern United States. Atmos. Environ. 2018;193:158–167. [Google Scholar]
- Bell M.L. Assessment of the health impacts of particulate matter characteristics. Res. Rep. Health Eff. Inst. 2012;161:5–38. [PubMed] [Google Scholar]
- Bell M.L., Dominici F., Ebisu K., Zeger S.L., Samet J.M. Spatial and temporal variation in PM2.5 chemical composition in the United States for health effects studies. Environ. Health Perspect. 2007;115(7):989–995. doi: 10.1289/ehp.9621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beverland I.J., Cohen G.R., Heal M.R. A comparison of short-term and long-term air pollution exposure associations with mortality in two cohorts in Scotland. Environ. Health Perspect. 2012;120(9):1280–1285. doi: 10.1289/ehp.1104509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo M.A., Ebisu K., Dominici F., Wang Y., Peng R.D., Bell M.L. Airborne fine particles and risk of hospital admissions for understudied populations: effects by urbanicity and short-term cumulative exposures in 708 U.S. counties. Environ. Health Perspect. 2017;125:594–601. doi: 10.1289/EHP257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Y., Zhang B., Ke W., Feng B. Associations of short-term and long-term exposure to ambient air pollutants with hypertension: a systematic review and meta-analysis. Hypertension. 2016;68(1):62–70. doi: 10.1161/HYPERTENSIONAHA.116.07218. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics. n.d. Underlying cause of death 1999–2018 on CDC WONDER online database, released in 2020. Data are from the multiple cause of death files, 1999–2018, as compiled from data provided by the 57 vital statistics jurisdictions through the vital statistics cooperative program. http://wonder.cdc.gov/ucd-icd10.html Accessed April 27, 2020.
- Chen K., Wang M., Huang C., Kinney P.L., Anastas P.T. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020 doi: 10.1016/S2542-5196(20)30107-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COMEAP . A Report by the Committee on the Medical Effects of Air Pollutants. Health Protection Agency; UK: 2010. The mortality effects of long-term exposure to particulate air pollution in the United Kingdom. [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in northern Italy? Environ. Pollut. 2020;261 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contini D., Costabile F. Does air pollution influence COVID-19 outbreaks? Atmosphere. 2020;11(4):377. [Google Scholar]
- Dutheil F. COVID-19 as a factor influencing air pollution? Environ. Pollut. 2020;263 doi: 10.1016/j.envpol.2020.114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;264 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham-Harrison E., Giuffrida A., Smith H., Ford L. The Guardian. 2020. Lockdowns around the world bring rise in domestic violence.https://www.theguardian.com/society/2020/mar/28/lockdowns-world-rise-domestic-violence [Google Scholar]
- Isaifan R.J. The dramatic impact of coronavirus outbreak on air quality: has it saved as much as it has killed so far? Global J Environ Sci Manage. 2020;6(3):275–288. [Google Scholar]
- Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y, Turner MC, Pope CA III, Thurston G, Calle EE, Thun MJ. 2009. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. HEI Research Report 140. Health Effects Institute, Boston, MA. [PubMed]
- Kumar A., Nayar K.R. COVID 19 and its mental health consequences. J. Ment. Health. 2020;27:1–2. doi: 10.1080/09638237.2020.1757052. [DOI] [PubMed] [Google Scholar]
- Liang D., Shi L., Zhao J., Liu P., Schwartz J., Gao S. Urban air pollution may enhance COVID-19 case-fatality and mortality rates in the United States. MedRxiv. 2020 doi: 10.1101/2020.05.04.20090746. Preprint. 2020 May 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng X., Hand J.L., Schichtel B.A., Liu Y. Space-time trends of PM2.5 constituents in the conterminous United States estimated by a machine learning approach, 2005–2015. Environ. Int. 2018;121:1137–1147. doi: 10.1016/j.envint.2018.10.029. [DOI] [PubMed] [Google Scholar]
- National Aeronautics and Space Administration (NASA) NASA satellite data shows 30 percent drop in air pollution over northeast U.S. 2020. https://www.nasa.gov/feature/goddard/2020/drop-in-air-pollution-over-northeast
- National Center for Health Statistics. 2019. Vintage 2018 postcensal estimates of the resident population of the United States. Prepared under a collaborative arrangement with the U.S. Census Bureau. Available from: /nchs/nvss/bridged_race.htm as of June 25, 2019, following release by the U.S. Census Bureau of the unbridged Vintage 2018 postcensal estimates by 5-year age group on June 20, 2019.
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to the coronavirus (COVID-19) fatality rate. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C.A., 3rd Epidemiology of fine particulate air pollution and human health: biologic mechanisms and who’s at risk? Environ. Health Perspect. 2000;108(Suppl. 4):713–723. doi: 10.1289/ehp.108-1637679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich D.Q., Kipen H.M., Huang W., Wang G., Wang Y., Zhu P. Association between changes in air pollution levels during the Beijing Olympics and biomarkers of inflammation and thrombosis in healthy young adults. JAMA. 2012;307(19):2068–2078. doi: 10.1001/jama.2012.3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich D.Q., Liu K., Zhang J., Thurston S.W., Stevens T.P., Pan Y. Differences in birth weight associated with the 2008 Beijing Olympics air pollution reduction: results from a natural experiment. Environ. Health Perspect. 2015;123(9):880–887. doi: 10.1289/ehp.1408795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivellese F., Prediletto E. ACE2 at the centre of COVID-19 from paucisymptomatic infections to severe pneumonia. Autoimmun. Rev. 2020;19(6) doi: 10.1016/j.autrev.2020.102536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet J., Krewski D. Health effects associated with exposure to ambient air pollution. J. Toxic. Environ. Health A. 2007;70:227–242. doi: 10.1080/15287390600884644. [DOI] [PubMed] [Google Scholar]
- U.S. EPA Quantitative health risk assessment for particulate matter – final report. 2010. https://www3.epa.gov/ttn/naaqs/standards/pm/data/PM_RA_FINAL_June_2010.pdf
- U.S. EPA Outdoor air quality data. https://www.epa.gov/outdoor-air-quality-data/download-daily-data
- Venter Z.S., Aunan K., Chowdhhury S., Lelieveld J. COVID-19 lockdowns cause global air pollution declines with implications for public health risk. MedRxiv. 2020 doi: 10.1101/2020.04.10.20060673. Preprint. 2020 April 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Primbs T., Tao S., Simonich S.L. Atmospheric particulate matter pollution during the 2008 Beijing Olympics. Environ. Sci. Technol. 2009;43(14):5314–5320. doi: 10.1021/es9007504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing C., Simon K., Bello-Gomez R.A. Designing difference in difference studies: best practices for public health policy research. Annu. Rev. Public Health. 2018;39:453–469. doi: 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- Worldmeter Coronavirus (COVID-19) mortality rate. 2020. https://www.worldometers.info/coronavirus/
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. Exposure to air pollution and COVID-19 mortality in the United States. MedRxiv. 2020 doi: 10.1101/2020.04.05.20054502. Preprint. 2020 April 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material