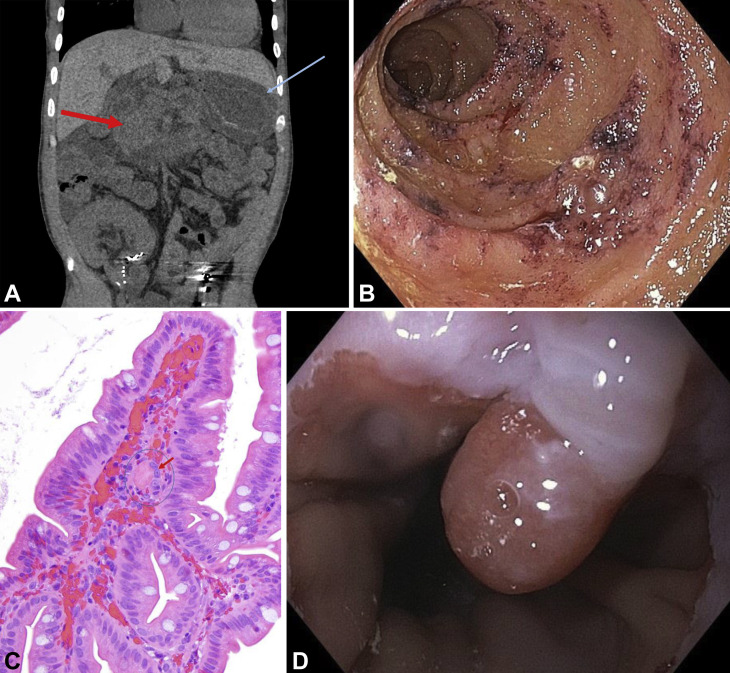
A 35-year-old man with sickle-cell trait and diabetes who had undergone renal transplantation presented with weeks of episodic severe cramping, abdominal pain, diarrhea, maroon stool, and anorexia despite using empiric antibiotics for gastroenteritis. At presentation, his laboratory results noted a mild leukocytosis and a hemoglobin of 6.4 g/dL. Real-time polymerase chain reaction of a nasopharyngeal sample gave a positive result for SARS-CoV-2 despite the lack of respiratory symptoms or fever. A CT scan demonstrated diffusely thickening of the stomach and small-bowel walls (A). Upper endoscopy revealed normal gastric mucosa but edematous, friable duodenal mucosa with contact bleeding (B). Examination of biopsy specimens from the duodenal mucosa demonstrated hemorrhage in the lamina propria with fibrin microthrombi (C, H&E, orig. mag. ×40). A biopsy specimen from a small gastroesophageal junction polyp incidentally showed dysplasia with a focus of adenocarcinoma (D). Magnetic resonance angiography failed to show any explanatory large-vessel disease. The patient’s melena resolved 4 weeks after symptom onset and 3 blood transfusions. Repeated endoscopy at 5 weeks showed normal mucosa; the polyp was successfully removed en bloc by submucosal dissection. No other thromboses were noted during his course; d-dimer peaked at 1633 mg/mL. GI involvement of SARS-CoV-2 is common; typical symptoms include diarrhea and nausea, although bleeding has been rarely described. To our knowledge, this is the first endoscopic description of biopsy-confirmed COVID-19–associated microthrombosis, reinforcing the importance of endoscopy with adequate biopsy.
Disclosure
All authors disclosed no financial relationships.
Commentary As our knowledge about COVID-19 evolves, we are starting to view the illness as a thrombotic microvascular injury of systemic nature in which the lung, skin, kidney, GI tract, and other organs are affected. Microthrombosis in COVID-19 is a complement-mediated disorder. It is unclear whether COVID-19–related coagulopathy is a byproduct of severe inflammatory response or a virus-specific–mediated coagulopathy.
As seen in this case, COVID-19–related microthrombotic disease of the small intestine presents endoscopically as edema, granularity, and patchy erythema, as seen in other ischemic disorders. Biopsy specimens showing hemorrhage in the lamina propria with fibrin microthrombi are diagnostic of the condition.
With the current rise of COVID-19 cases in hospitals worldwide, endoscopists should be aware of COVID-19–related microthrombosis syndrome as a cause of GI bleeding in this subset of patients. How prevalent this condition is among our hospitalized patients with COVID-19 and whether other comorbid conditions pose a synergetic effect on developing microthromboses are questions that remain to be answered.
Mohamed O. Othman, MD, Associate Editor for Focal Points
Mohamed O. Othman, MD, Associate Editor for Focal Points