Abstract
Aims
To create a low-cost ventilator that could be constructed with readily-available hospital equipment for use in emergency or low-resource settings.
Main methods
The novel ventilator consists of an inspiratory limb composed of an elastic flow-inflating bag encased within a non-compliant outer sheath and an expiratory limb composed of a series of two, one-way bidirectional splitter valves derived from a self-inflating bag system. An Arduino Uno microcontroller controls a solenoid valve that can be programmed to open and close to produce a set respiratory rate and inspiratory time. Using an ASL 5000 Lung Simulator, we obtained flow, pressure, and volume waveforms at different lung compliances.
Key findings
At a static lung compliance of 50 mL/cm H2O and an airway resistance of 6 cm H2O/L/s, ventilated at a PIP and PEEP of 16 and 5 cm H2O, respectively, tidal volumes of approximately 540 mL were achieved. At a static lung compliance of 20 mL/cm H2O and an airway resistance of 6 cm H2O/L/s, ventilated at a PIP and PEEP of 38 and 15 cm H2O, respectively, tidal volumes of approximately 495 mL were achieved.
Significance
This novel ventilator is able to safely and reliably ventilate patients with a range of pulmonary disease in a simulated setting. Opportunities exist to utilize our ventilator in emergency situations and low-resource settings.
Keywords: Low-resource ventilator, Respiratory, Lungs, COVID, SARS-CoV-2, Coronavirus
1. Introduction
The ongoing Covid-19 pandemic has placed marked strain on the global healthcare system. With a limited supply of mechanical ventilators to treat the severe acute respiratory distress syndrome (ARDS) associated with the disease, a shortage has ensued [1]. Few other healthcare decisions are as strikingly critical as the allocation of mechanical ventilation [2]. Faced with these unprecedented ethical conditions, physicians and engineers alike have launched widespread attempts to create low-cost and widely scalable ventilation alternatives [3]. Some efficacy has been demonstrated in using a single ventilator to support multiple patients [4,5]. Other designs have targeted volume-controlled ventilation via mechanical compression of a self-inflating bag-valve system attached to a patient's endotracheal tube [6]. Yet others have permitted tidal volume administration via regulated release of gas from a central pressure reservoir [7]. Nevertheless, an effective ventilator for emergency and low-resource settings must not only address the underlying pathophysiology of a variety disease processes, but must also be functionally designed to allow for large-scale construction and distribution.
Modern ventilators generate tidal volumes from a pressurized gas source via three different mechanisms. In a bellows ventilator, a compressible bellows is inflated with the inspiratory gas that is subsequently delivered to the patient by pneumatic forces from a surrounding compressive gas within a rigid chamber. Piston ventilators, in comparison, force tidal volume by mechanical compression of the inspiratory gas to generate a pressure gradient. Lastly, turbine ventilators use an electric motor to drive inspiratory flow and pressure [8,9].
In the present study, we aimed to design and prototype a mechanical ventilator that could be assembled of readily-available hospital equipment with minimal need for external hardware. The resulting design is sufficiently versatile to achieve a variety of ventilation strategies and adequately economical to make large-scale rapid production attainable. We developed a novel method and device for generating inspiratory pressure resulting in a customizable, efficacious, and cost-efficient mechanical ventilator. As such, this design is suitable for circumstances in which access to conventional ventilators is limited.
2. Materials and methods
Ventilator circuits require inspiratory and expiratory limbs. The inspiratory limb allows for the generation of a tidal volume by regulating peak inspiratory pressures (PIP), whereas the expiratory limb allows for exhalation while regulating and maintaining positive end-expiratory pressure (PEEP). The inspiratory and expiratory limbs must be temporally disconnected, allowing for uninhibited exhalation and differential regulation of PIP and PEEP.
The initial aim of this study was to assemble a functional ventilator from readily-available hospital equipment. The parts list utilized for the completion of that aim are represented in Table 1 with their associated costs and the total cost of the parts to build the ventilator were USD 98.58. The details of this dual-limb circuit are displayed in Fig. 1 .
Table 1.
Ventilator component costs and hospital availability.
| Item | Number | Hospital-available | Cost (USD) |
|---|---|---|---|
| Adjustable pressure relief valve | 1 | x | 10.00 [10] |
| Arduino microcontroller | 1 | 23.00 [11] | |
| Flow-inflating Mapleson bag | 2 | x | 23.99 [12] |
| One-way valves | 2 | x | 4.95 [13] |
| Oxygen tubing | 2 | x | 0.46 [14] |
| Adjustable PEEP valve | 1 | x | 9.29 [15] |
| Size 3 soccer ball | 1 | 7.90 [16] | |
| Solenoid valve | 1 | 18.99 [17] |
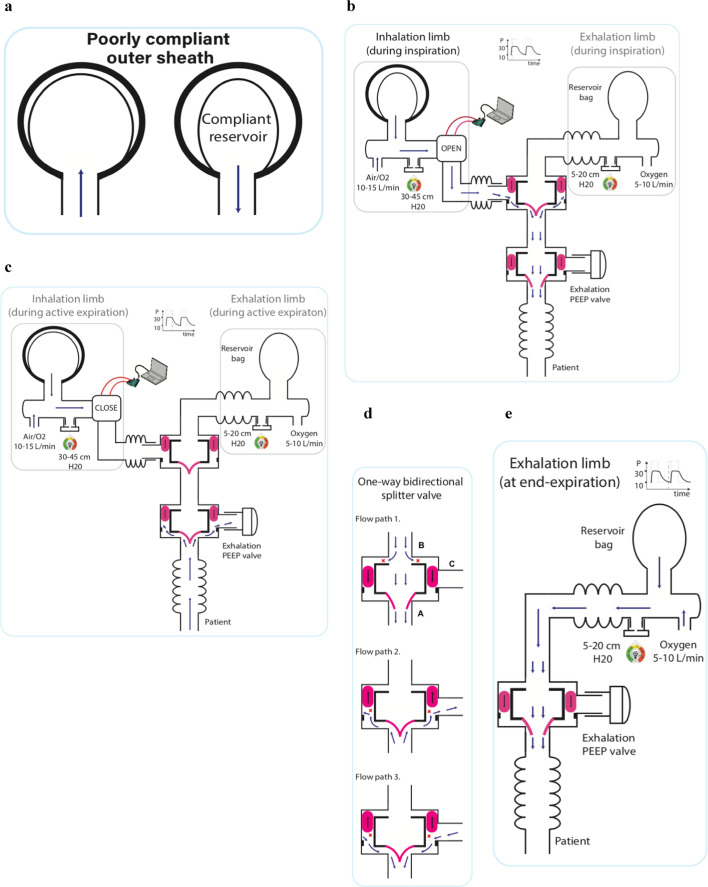
Fig. 1.
a: The noncompliant outer sheath encompassing the elastic flow-inflating bag on the inspiratory limb is depicted.
b: The inspiratory phase is depicted. With the solenoid valve open, tidal volume is delivered via flow paths 3 and 1 through the proximal and distal one-way valves, respectively.
c: The early expiratory phase is depicted. The predominance of the exhaled gas egresses via flow path 2 of the distal one-way valve through the PEEP valve.
d: The one-way bidirectional splitter valves are depicted with three possible flow paths. The common port labeled A can receive inflow from either of the inlet ports labeled B and C. With the valve leaflets open, gas can flow unidirectionally egressing out of the common port from the port labeled B. With the valve leaflets closed, gas can flow bidirectionally between the common port and the port labeled C.
e: At end-exhalation, the distal one-way bidirectional splitter valve permits flow through flow path 1 to maintain PEEP.
The inspiratory limb consists of an elastic flow-inflating bag encased within a noncompliant sheath, which is pressurized using flow from a compressed gas source. Medical gas at a flow rate of 10–20 L/min was used to pressurize the inspiratory limb of the system. The flow-inflating bag and the noncompliant sheath act as a series circuit of a capacitor and a resistor. The elasticity of the flow-inflating bag permits rapid release of stored energy to the patient, allowing for a physiologic rise of inspiratory pressures. The resistance of the noncompliant sheath permits for inspiratory pressures higher than that which could be achieved by the flow-inflating bag alone and serves as a protective barrier to prevent over-distension of the bag. The Arduino Uno microcontroller controls the programmable solenoid valve to open with a frequency and for a duration that is adjustable by the healthcare provider, resulting in a customizable respiratory rate, inspiratory time, and inspiratory-to-expiratory ratio. Upon opening of the valve, a large pressure gradient drives the delivery of the tidal volume to the patient. The working Arduino code is displayed as a supplemental table.
The expiratory limb consists of two one-way bidirectional splitter valves derived from a self-inflating bag system. As depicted in Fig. 1d, there are three permissible flow paths through these valves, which are uniquely connected to achieve a dual functionality of rapid exhalation and PEEP maintenance. The first of these functions is accomplished by the distal valve which interfaces with a spring-loaded PEEP valve through which the predominance of exhalation occurs as depicted in Fig. 1c. The large surface area of this PEEP valve can accommodate the high flow rates of early exhalation. The more proximal valve receives a second source of gas flow to refresh the dead-space of the circuit and to maintain PEEP between breaths as seen in Fig. 1e. The second flow-inflating bag on the expiratory limb also houses a reservoir volume to allow for patient-initiated breaths and for hand-ventilation during setting adjustments and in the event of device malfunction.
Specifically, the ALFA ventilator is assembled as follows. A 0.5 L flow-inflating bag is placed within a size 3 soccer ball via a 0.75 in. drill hole. This limb receives an inflow from a pressurized gas source, and has an adjustable pressure relief valve to limit the maximal pressure in this reservoir. Together, the flow-inflating bag, soccer ball, gas inflow, and pressure relief valve form the inspiratory reservoir. Tidal volume delivery from the inspiratory reservoir is controlled by a solenoid valve according to the Arduino code displayed in the supplemental table. The solenoid valve is then connected to the expiratory port of the proximal one-way bidirectional splitter valve. The inspiratory port of this valve is connected to a second flow-inflating bag with a secondary source of gas flow and a Mapleson relief valve. Notably, the pressure of this secondary reservoir must be less than or equal to the end-expiratory pressure set at the PEEP valve. The patient port of this proximal valve interfaces with the inspiratory port of a second one-way bidirectional splitter valve. The expiratory port of this valve connects to a spring-loaded PEEP valve, and the patient port of this valve connects to corrugated tubing leading to the patient's endotracheal tube. Fig. 2 displays a photograph of the fully assembled ALFA ventilator.
Fig. 2.
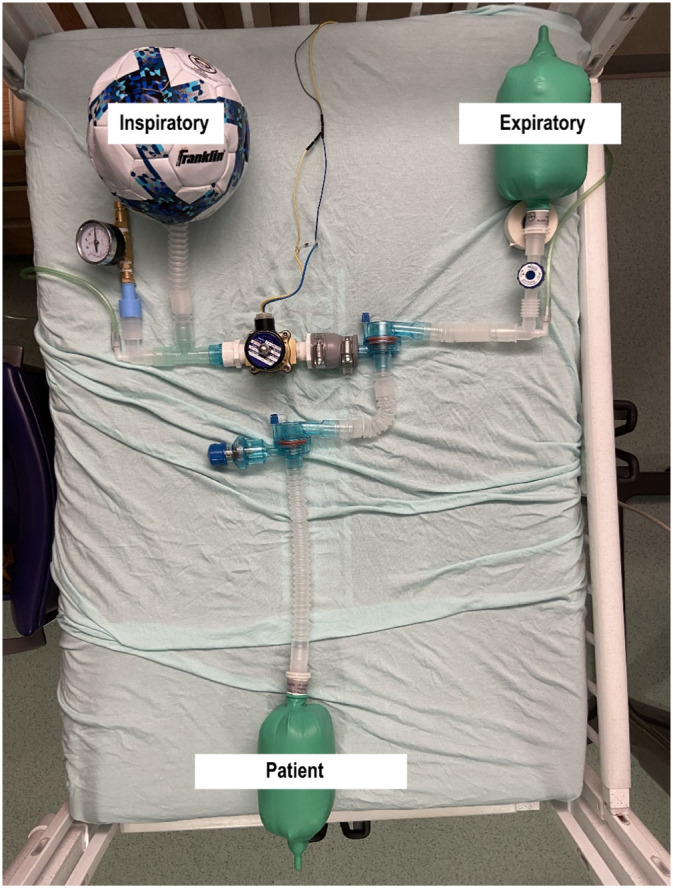
A photograph of the assembled ALFA ventilator.
3. Results
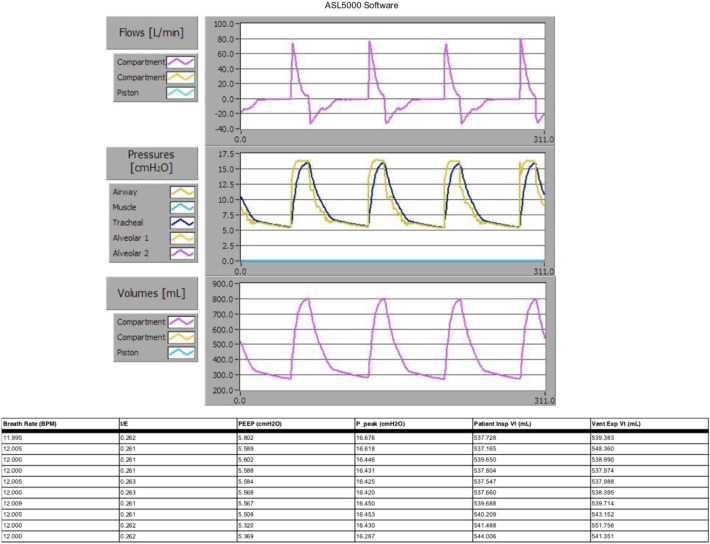
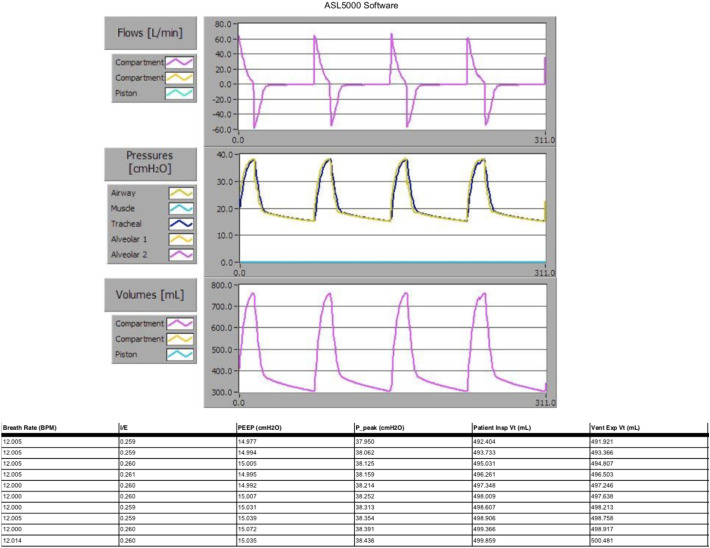
Simulated data was obtained using an ASL 5000 lung simulator (IngMar Medical, Pittsburgh, PA). Multiple simulation scenarios were included to mimic a range of pulmonary disease with varying airway resistance and compliance in populations from neonates to adults. Respiratory rate, inspiratory-to-expiratory time ratio, PEEP, PIP, and tidal volume were measured with each breath. Characteristic flow, pressure, and volume waveforms were obtained for graphical depiction. Fig. 3, Fig. 4 demonstrate a sample of such breath metrics and waveforms with a flow rate of medical gas of 10 L/min delivered to the inspiratory limb. In both simulations, the respiratory rate was set to 15 breaths per minute with an inspiratory time of 1 s and a resultant inspiratory to expiratory ratio of 1:3. Fig. 3 simulates a healthy adult patient with a static lung compliance of 50 mL/cm H2O and an airway resistance of 6 cm H2O/L/s, ventilated at a PIP and PEEP of 16 and 5 cm H2O, respectively, resulting in tidal volumes of approximately 540 mL. Fig. 4 simulates an adult with ARDS with a static lung compliance of 20 mL/cm H2O and an airway resistance of 6 cm H2O/L/s, ventilated at a PIP and PEEP of 38 and 15 cm H2O, respectively, resulting in tidal volumes of approximately 495 mL.
Fig. 3.
Flow, pressure, and volume waveforms of an adult lung with a compliance of 50 mL/cm H2O and an airway resistance of 6 cm H2O/L/s. The table below delineates the parameters of the final 10 breaths of the simulation.
Fig. 4.
Flow, pressure, and volume waveforms of an adult lung with a compliance of 20 mL/cm H2O and an airway resistance of 6 cm H2O/L/s. The table below delineates the parameters of the final 10 breaths of the simulation.
4. Discussion
Acute respiratory failure is the most common indication for tracheal intubation in the critical care unit [18]. As such, the ability to mechanically ventilate is tantamount critical care medicine. During the current Covid-19 pandemic, the frequency of acute respiratory failure requiring mechanical ventilation has precipitated a shortage of crucial supplies necessary for the delivery of critical care both in the developed and developing world, thereby limiting the provision of life-saving interventions to many [19,20]. In order to adequately address the needs of these emergency circumstances and, more broadly, other low-resource contexts, an innovative ventilator design must be not only fully customizable, but also economical to permit wide scalability. We propose a novel method and low-cost device for mechanical ventilation, assembled with readily-available components serving both to address a shortage in the setting of a pandemic and to expand access to ventilators in low-resource settings.
4.1. Simulation
As lung compliance varies with pulmonary disease, a ventilator must be able to deliver a wide range of pressure in inspiration and maintain high pressure at end-exhalation. With a lung compliance of 50 mL/cm H2O and an airway resistance of 6 cm H2O/L, our ventilator achieved tidal volumes in excess of 500 mL with a PIP of 16 cm H2O and a PEEP of 5 cm H2O. To simulate ARDS, we decreased lung compliance to 20 mL/cm H2O while maintaining airway resistance at 6 cm H2O/L/s. At these simulated values, we achieved tidal volumes of 495 mL with a PIP of 38 cm H2O and a PEEP of 15 cm H2O. Our ventilator prototype is able to safely and effectively overcome a variable spectrum of lung compliance in a simulated model. This suggests that it may be useful for a wide-array of disease processes, including ARDS.
4.2. Adaptability and customizability of design
Our design operates via a unique mechanism to produce inspiratory pressure. Whereas other conventional ventilators generate an inspiratory pressure reservoir via the use of either electrically mechanized motors or pneumatic forces in the cases of piston and bellows ventilators, respectively, our design harnesses the innate elastic forces inherent to a flow-inflating bag to rapidly administer tidal volume breaths. The flow-inflating bag, in series with a non-compliant sheath, permits for appropriate ventilation of a spectrum of lung compliances seen in various severities of respiratory disease. This ventilator is able to provide adjustable peak inspiratory pressures, inspiratory time, respiratory rate, and therefore inspiratory-to-expiratory ratios due to the contractile power of the pressurized system. Medical gas, be it ambient air or oxygen, at a flow rate of 10 L/min was used in the inspiratory limb. A blender can be easily attached to the inspiratory limb of the system to deliver the full spectrum of supplemental oxygen to the patient.
The aforementioned parameters can be easily modified in the present model similar to conventional ventilators. With these inspiratory characteristics, this prototype can generate tidal breaths sufficient for any ventilatory strategy to provide respiratory support at the volume and pressure goals that have been shown to decrease mortality from ARDS in adults [[21], [22], [23], [24]]. Similarly, expiratory metrics can be adjusted by modifying the spring-loaded PEEP valves. The ability to alter settings such as maximum inspiratory pressure, respiratory rate, inspiratory time, and positive end-expiratory pressure, all while providing reproducible breaths demonstrates clear advantages over alternative methods in times of supply shortages and in low-resource environments, such as manual bag ventilation, or other existing emergency ventilator designs [6,7].
4.3. Future directions and value
It is important to note that our current ventilator design was not intended to replace existing full-functioning conventional mechanical ventilations in settings in which resources permit their acquisition. Nevertheless, in comparison to commercially available products, our design has some notable weaknesses. The current model offers only intermittent mandatory pressure-controlled ventilation that can interface with a patient's spontaneous ventilation. While our ventilator design incorporates a reservoir on the expiratory limb to allow for patient-initiated breaths, we do not yet have mechanisms for synchronizing ventilator breaths with patient-initiated breaths. Future prototype models may incorporate flow sensors and electronic pressure valves, although these would add modestly to the cost and complexity of the design. Upon detection of a patient-initiated breath, the flow sensor may trigger the solenoid valve to provide a ventilator breath to provide support in a manner similar to assist control. The integration of flow sensors and electronic pressure regulators may permit for breath-to-breath alterations in the inspiratory reservoir to automatically adjust inspiratory pressures, perhaps making volume-controlled ventilation feasible. Moreover, incorporation of pneumatically controlled valves in subsequent models may create a self-regulated system and eliminate the need for electronic controls.
In consideration of value, one can assemble our proposed emergency ventilator quickly and at a low cost, which is necessary for broad scalability. As viewed in Table 1, the total cost of assembly of this device is less than $100 as compared with conventional ventilators that cost in excess of $20,000 [25]. Moreover, the components employed in this design are comparatively few and readily available in nearly all hospital settings, easing the burden of supply and quickening the process of assembly.
5. Conclusion
Our ventilator has demonstrated efficacy in high-fidelity simulations to ventilate adults and pediatric patients alike with a range of pulmonary disease. Though it was conceived in the setting of the Covid-19 pandemic, the applicability of this model may be far reaching, specifically for resource-limited communities. In conclusion, the proposed novel device for mechanical ventilation, economically constructed of readily-available hospital supplies, has robust ventilatory capability and customizability to address the spectrum of pulmonary disease in both the pediatric and adult populations adult and pediatric suitable for emergency and low-resource settings.
Financial support
This research did not receive any grant form funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that there are no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.lfs.2020.118113.
Appendix A. Supplementary data
Supplementary material
References
- 1.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. N. Engl. J. Med. 2020;(382):e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 2.Truog R.D., Mitchell C., Daley G.Q. The toughest triage—allocating ventilators in a pandemic. N. Engl. J. Med. 2020;(382):1973–1975. doi: 10.1056/NEJMp2005689. [DOI] [PubMed] [Google Scholar]
- 3.Pearce J.M. A review of open source ventilators for COVID-19 and future pandemics. F1000Research. 2020;9(218):218. doi: 10.12688/f1000research.22942.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neyman G., Irvin C.B. A single ventilator for multiple simulated patients to meet disaster surge. Acad. Emerg. Med. 2006;13(11):1246–1249. doi: 10.1197/j.aem.2006.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paladino L., Silverberg M., Charchaflieh J.G., Eason J.K., Wright B.J., Palamidessi N.…Manoach S. Increasing ventilator surge capacity in disasters: ventilation of four adult-human-sized sheep on a single ventilator with a modified circuit. Resuscitation. 2008;77(1):121–126. doi: 10.1016/j.resuscitation.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 6.MIT E-Vent: Emergency ventilator design toolbox. (n.d.). Retrieved April 4, 2020 from https://e-vent.mit.edu/.
- 7.Open source ventilator project. (n.d.). Retrieved April 6, 2020, from https://simulation.health.ufl.edu/technology-development/open-source-ventilator-project/.
- 8.Hess D., Kacmarek R.M., Kollef M.H. McGraw-Hill, Health Professions Division; New York: 1996. Essentials of Mechanical Ventilation. [Google Scholar]
- 9.Tobin M.J. McGraw Hill Professional; 2010. Principles and Practice of Mechanical Ventilation. [Google Scholar]
- 10.Control Devices CR series brass pressure relief valve. 2020. https://www.amazon.com Retrieved from.
- 11.Arduino Arduino Uno Rev3. 2020. https://store.arduino.cc/usa/arduino-uno-rev3 Retrieved from.
- 12.AirLife Flow-inflating Bag 0.5 L, Neoprene. https://www.boundtree.com/Oxygen-Equipment/Circuits-Accessories/AirLife-Flow-inflating-Bag-0-5L-Neoprene/p/2422-02510 Retrieved from.
- 13.Ambu one way valve with filter. https://www.cpr-savers.com/Ambu-One-Way-Valve-with-Filter-for-Res-Cue-CPR-Mask_p_7789.html Retrieved from.
- 14.Curaplex oxygen connecting tubing, 7 Ft L, 3/16 in ID. https://www.boundtree.com/Airway-Oxygen-Delivery/Oxygen-Tubing/Curaplex-Oxygen-Connecting-Tubing-7ft-L-3-16in-ID/p/87-3007EA Retrieved from.
- 15.Adjustable PEEP Valves, AMBU. https://www.boundtree.com/Oxygen-Equipment/Oxygen-Accessories/Adjustable-Peep-Valves/p/group000106 Retrieved from.
- 16.Franklin sports soccer ball, size 3. https://www.amazon.com/Franklin-Sports-Competition-Soccer-Assorted/dp/B000067R1I/ref=sr_1_2?dchild=1&qid=1587134637&refinements=p_n_feature_seventeen_browse-bin%3A5744251011&s=team-sports&sr=1-2 Retrieved from.
- 17.SNS DC 12V ½″ NPT Brass solenoid valve normally closed, water, air, diesel. https://www.amazon.com/SNS-2W025-08-Electric-Solenoid-Normally/dp/B0794X25XP Retrieved from.
- 18.Esteban A., Anzueto A., Alía I. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am. J. Respir. Crit. Care Med. 2000 doi: 10.1164/ajrccm.161.5.9902018. [DOI] [PubMed] [Google Scholar]
- 19.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages — the need for ventilators and personal protective equipment during the Covid-19 pandemic. N. Engl. J. Med. 2020 doi: 10.1056/nejmp2006141. [DOI] [PubMed] [Google Scholar]
- 20.Xie J., Tong Z., Guan X., Du B., Qiu H., Slutsky A.S. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tobin M.J. Advances in mechanical ventilation. N. Engl. J. Med. 2001 doi: 10.1056/NEJM200106283442606. [DOI] [PubMed] [Google Scholar]
- 22.Grasso S., Stripoli T., De Michele M. ARDSnet ventilatory protocol and alveolar hyperinflation: role of positive end-expiratory pressure. Am. J. Respir. Crit. Care Med. 2007 doi: 10.1164/rccm.200702-193OC. [DOI] [PubMed] [Google Scholar]
- 23.De Durante G., Del Turco M., Rustichini L. ARDSNet lower tidal volume ventilatory strategy may generate intrinsic positive end-expiratory pressure in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2002 doi: 10.1164/rccm.2105050. [DOI] [PubMed] [Google Scholar]
- 24.Slutsky A.S., Ranieri V.M. Mechanical ventilation: lessons from the ARDSNet trial. Respir. Res. 2000 doi: 10.1186/rr15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dräger Evita infinity V500 ventilator ICU ventilation and respiratory monitoring SKU: RS020004. https://diamedicalusa.com/medical-equipment/respiratory/ventilators/drager-evita-infinity-v500-ventilator-icu-ventilation-respiratory-monitoring/ Retrieved from.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material