To the Editor
The outbreak of novel coronavirus disease in 2019 (COVID-19) has been very stressful worldwide. Fear, sleep disturbances, depression, and anxiety can be overwhelming, leading to strong emotions in those who have contracted COVID-19 [1]. As there is currently no consensus on the psychological/psychiatric treatment of COVID-19, physicians have taken into account current clinical and mental conditions, comorbidities, drug-drug interactions, and others [2] based on their knowledge and experience.
Transcranial direct current stimulation (tDCS) has been widely used for mood and anxiety conditions in clinical practice [[3], [4], [5]] with good outcomes. However, there are currently no reports on COVID-19 patients. Therefore, after obtaining informed consent, we used tDCS sessions for our hospitalized COVID-19 patient with a very severe level of anxiety.
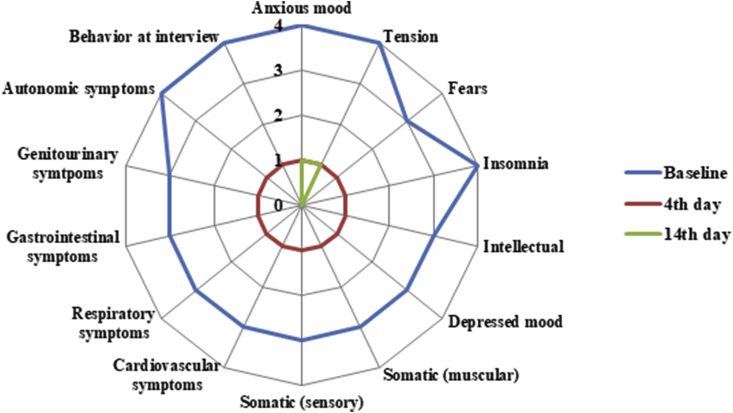
Here we report the case of a 32-year-old man with severe obesity (body mass index of 37.5 kg/m2) who developed fever, asthenia, cough, sore throat, and shortness of breath for five days. His chest computed tomography scan revealed multiple ground-glass opacities, mainly in the peripheral and lower areas of both lungs, compatible with COVID-19. In addition, his test (nasopharyngeal and oropharyngeal swabs) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was positive. Subsequently, the clinical condition deteriorated, requiring intubation and intensive care for nine days. When his conditions finally improved, he was transferred to the hospital ward. At that time, he presented significant emotional liability, tension, insomnia, episodes of panic attack, and widespread anxiety. He was on quetiapine on dose of 75 mg/day. In addition, the psychologist provided care for his emotional distress and, in the first interview, found a score of 47 out of 56 points (very severe anxiety levels, Fig. 1 ) on the Hamilton anxiety rating scale [6]. Several clinical and infectious events, such as pulmonary embolism, pneumonia, deep vein thrombosis, urinary tract infections, sepsis, and temporary dialytic renal insufficiency, occurred over approximately 60 days. During all period of hospital ward, the patient had been also followed daily by a physiotherapist to improve the muscle strength and respiratory function.
Fig. 1.
Hamilton anxiety rating scale applied in the present case report.
Due to the lack of improvement in pharmacotherapy and the impossibility of using transcranial magnetic stimulation (TMS) due to lack of availability in the ward, tDCS (Genius, NKL, Brazil) with 2 mA amplitude was submitted for 20 minutes in the morning for five consecutive days. The 5x7 sponge-electrodes were positioned with the anode over the left (F3) and cathode over the right (F4) dorsolateral prefrontal cortices, according to the 10–20 international systems for EEG electrodes placement.
During the tDCS period, the patient reported significant improvements of his previous psychological aspects and degree of anxiety. The patient used quetiapine on a stable dose (75 mg/day) throughout all sessions. He was at this dose for at least two weeks between tDCS onset, and remained using quetiapine until 10 days after tDCS treatment ended. The Hamilton anxiety rating scale questionnaire was administered four and 14 days later at the last tDCS session. He scored 14 (mild anxiety levels) and 2 (normal) out of 56 points, respectively (Fig. 1). Concerning physical aspects, we did not observe a significant improvement. He remained bedridden.
Therefore, to the best of our knowledge, the present case report shows that bifrontal tDCS can be a potential and (co)adjuvant therapy for physiological treatment of patients with COVID-19. More studies with significant samples and patients with different COVID-19 conditions are needed to corroborate our findings.
Financial support
This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) 303,379/2018–9, Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) 2019/11,776–6, the Program of Academic Productivity (PIPA) of Faculdade de Medicina da USP/SP to SKS; CNPq (PQ-1B), and the Program of Academic Productivity (PIPA) of Faculdade de Medicina da USP/SP to ARB.
Declaration of competing interest
All authors declare no conflict of interest.
References
- 1.Ornell F., Schuch J.B., Sordi A.O. Pandemic fear and COVID-19: mental health burden and strategies. Br J Psychiatry. 2020;42:232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khawam E., Khouli H., Pozuelo L. Treating acute anxiety in patients with COVID-19. Cleve Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc016. [DOI] [PubMed] [Google Scholar]
- 3.Sagliano L., Atripaldi D., De Vita D., D’Olimpio F., Trojano L. Non-invasive brain stimulation in generalized anxiety disorder: a systematic review. Prog Neuro-Psychopharmacol Biol Psychiatry. 2019;93:31–38. doi: 10.1016/j.pnpbp.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Vicario C.M., Salehinejad M.A., Felmingham K., Martino G., Nitsche M.A. A systemicatic review on the therapeutic effectiveness of non-invasive brain stimulation for the treatment of anxiety disorders. Nuerosci Biobehav Rev. 2019;96:219–231. doi: 10.1016/j.neubiorev.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Stein D.J., Fernandes Medeiros L., Caumo W., Torres I.L. Transcranial direct current stimulation in patients with anxiety: current perspectives. Neuropsychiatric Dis Treat. 2020;16:161–169. doi: 10.2147/NDT.S195840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]