Abstract
Background
Globally, critical illness causes up to 45 million deaths every year. The burden is highest in low-income countries such as Malawi. Critically ill patients require good quality, essential care in emergency departments and in hospital wards to avoid negative outcomes such as death. Little is known about the quality of care or the availability of necessary resources for emergency and critical care in Malawi. The aim of this study was to assess the availability of resources for emergency and critical care in Malawi using data from the Service Provision Assessment (SPA).
Methods
We conducted a secondary data analysis of the SPA — a nationwide survey of all health facilities. We assessed the availability of resources for emergency and critical care using previously developed standards for hospitals in low-income countries. Each health facility received an availability score, calculated as the proportion of resources that were present. Resource availability was sub-divided into the seven a-priori defined categories of drugs, equipment, support services, emergency guidelines, infrastructure, training and routines.
Results
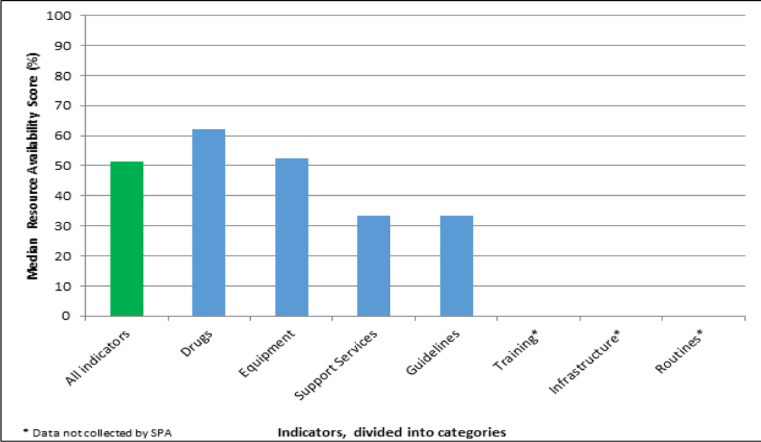
Of the 254 indicators in the standards necessary for assessing the quality of emergency and critical care, SPA collected data for 102 (40.6%). Hospitals had a median resource availability score of 51.6% IQR (42.2–67.2) and smaller health facilities had a median of 37.5% (IQR 28.1–45.3). For the category of drugs, the hospitals' median score was 62.0% IQR (52.4–81.0), for equipment 51.9% IQR (40.7–66.7), support services 33.3% IQR (22.2–77.8) and emergency guidelines 33.3% IQR (0–66.7). SPA did not collect any data for resources in the categories of infrastructure, training or routines.
Conclusion
Hospitals in Malawi lack resources for providing emergency and critical care. Increasing data about the availability of resources for emergency and critical care and improving the hospital systems for the care of critically ill patients in Malawi should be prioritized.
Keywords: Malawi, Health Services, Critical Illness, Emergency care
Introduction
Critical illness — any immediately life threatening condition1 — is common. Globally, it is estimated that critical illness causes 30–45 million deaths each year2. The burden is likely to be highest in low-income countries such as Malawi3,4. Critically ill patients require good quality, essential care to avoid negative outcomes such as death.5. Intensive Care Units are scarce in low-income countries6, and most critically ill patients are cared for in emergency departments and in general hospital wards.
For hospitals to provide emergency and critical care, certain resources are required7. Little is known about the availability of resources or the quality of care of emergency and critical care in Malawi. Lack of resources has been previously reported as a major contributing factor to poor quality of care in low-income countries8.
The Malawi Service Provision Assessment (SPA) was carried out in 2013–2014 as part of phase six of the Demographic and Health Survey (DHS) series9. SPA surveys are carried out regularly to collect data on resource availability from all health facilities in Malawi. The aim of this study was to use the SPA data to assess the availability of resources for emergency and critical care in health facilities in Malawi.
Methods
Design
We conducted a secondary data analysis of the Malawi Service Provision Assessment. The SPA, conducted in June 2013 – February 2014, included all public facilities, non-governmental-organisation facilities, private-for-profit, faith-based facilities, and facilities managed by corporate entities. The survey tools included inventories of clinical services and interviews with providers. Detailed methods are reported in the survey report9.
Data management
We used the only available standards for the resource requirements for emergency and critical care in hospitals in low-income countries7. The standards have been used in Tanzania7 and Sierra Leone10 and contain 254 indicators. We searched for and extracted data from the SPA database that contained information about these 254 variables.
We divided up the data according to the seven categories in the standards: drugs, equipment, support services, emergency guidelines, infrastructure, training and routines. When we found more than one variable that concerned the same resource, we used the variable that provided the most information on usability (for example we kept “functioning glucometer” and rejected “glucometer available”). For each health facility, each resource was classified as “available” or “not available”. Missing data were imputed as “not available”.
We classified health facilities into groups. Firstly, we classified them as hospitals or smaller health facilities: hospitals were facilities that had either been defined as hospitals by SPA or facilities that routinely provided in-patient care and smaller health facilities were the remaining facilities. Secondly we classified the health facilities into urban or rural, as defined by SPA. And thirdly we classified the health facilities according to their type of management — Government, Christian Health Association of Malawi, Private, Mission/Faith-based, NGO or Company — as described in the SPA database9.
Data analysis
Each hospital received an availability score, calculated as the proportion of resources that were present. The hospitals also received scores within each category — i.e. the proportion of resources that were present for drugs, equipment, support services, emergency guidelines, infrastructure, training and routines. The hospitals' overall availability scores, and scores for each category were summarized with medians and inter-quartile ranges (IQRs). Data analysis was conducted using Stata 15 (Release 15, Stata Corp, College Station, TX).
Ethical considerations
As a secondary analysis of anonymized and publicly available datasets, ethical considerations were minimal. Ethical approval for SPA was previously obtained by the DHS Program from the United States Department of Health and Human Services Institutional Review Board (IRB), and included authorization to distribute unrestricted survey files for secondary analysis purposes9.
Results
General characteristics of the health facilities
Of the 977 surveyed health facilities, 255 (26.1%) were classified as hospitals and 722 (73.9%) were smaller health facilities. Four hundred and seventy-eight of the facilities (49.0%), were managed by the government or public sector, and the remainder were managed by faith-based organisations, non-governmental organisations or private companies.
Of the 254 indicators in the standards necessary for assessing the quality of emergency and critical care (7), SPA collected data for 102 (40.6%). After combining indicators that were measuring the same resource, a total of 63 indicators were included in the analyses. (Table 1) No data were collected by SPA for the categories of infrastructure, (such as the presence of an intensive care unit), training or routines. Data were also not collected for some indicators within the other categories, such as, the presence of health workers in the emergency department or intravenous cannulas for adult patients (see the supplementary table 1).
Table 1.
Percentage availability of resources for emergency and critical care
| Hospitals n=255 | Smaller Health Facilities n=722 |
All Facilities n=977 | |
| Drugs | |||
| Adrenaline | 195 (76.5%) | 396 (54.9%) | 591 (60.5%) |
| Antibiotic for gram negative bacteria (Gentamycin or ceftriaxone) | 238 (93.3%) | 626 (86.7%) | 864 (88.4%) |
| Antibiotic for gram positive bacteria (Ceftriaxone, Penicillin or gentamycin) | 212 (83.1%) | 492 (68.1%) | 704 (72.1%) |
| Antimalarial (Artesunate or Quinine) | 198 (77.7%) | 487 (67.5%) | 685 (70.1%) |
| Dexamethasone injection | 81 (31.8%) | 94 (13.0%) | 175 (18.0%) |
| Dextrose (5% concentration) | 210 (82.4%) | 484 (67.0%) | 694 (71.0%) |
| Diazepam injection | 221 (86.7%) | 539 (74.7%) | 760 (77.8%) |
| Furosemide | 134 (52.6%) | 240 (33.2% | 374 (38.3%) |
| Glucose Injectable 50% (or other concentration > 10%) | 226 (88.6%) | 511 (70.8%) | 737 (75.4%) |
| Hydrocortisone | 74 (29.0%) | 105 (14.5%) | 179 (18.3%) |
| Insulin injection (Actrapid) | 64 (25.1%) | 12 (1.7%) | 76 (7.8%) |
| IV crystalloid (Ringers Lactate or Normal Saline) | 230 (90.2% | 540 (74.8%) | 770 (78.8%) |
| Ketamine | 50 (19.6%) | 20 (2.8%) | 70 (7.2%) |
| Lidocaine | 229 (89.8%) | 581 (80.5%) | 810 (83.0%) |
| Magnesium sulphate injection | 190 (74.5%) | 311 (43.1%) | 501 (51.3%) |
| Nifedipine | 96 (37.7%) | 113 (15.7%) | 209 (21.4%) |
| Oral rehydration salts | 233 (91.4%) | 589 (81.6%) | 822 (84.1%) |
| Oxytocin or other injectable uterotonic | 207 (81.2%) | 364 (50.4%) | 571 (58.4%) |
| Paracetamol | 228 (89.4%) | 608 (84.2%) | 836 (85.6%) |
| Parenteral opioid (Morphine or Pethidine) |
80 (31.4%) | 11 (1.5%) | 91 (9.3%) |
| Salbutamol inhaler | 118 (46.3%) | 197 (27.3%) | 315 (32.2%) |
| Equipment | |||
| Availability of Electricity always | 63 (24.7%) | 160 (22.2%) | 223 (22.8%) |
| Bag valve mask (Self inflating ambubag and mask-adult) | 108 (42.4 %) | 168 (23.3%) | 276 (28.6%) |
| Bag valve mask (Self inflating ambubag and mask-peads) | 141 (55.3%) | 216 (30.0%) | 35 (36.5%) |
| Blood pressure cuffs | 217 (85.1) | 592 (82.0%) | 809 (82.8%) |
| Disposable gloves | 223 (87.5%) | 649 (89.9%) | 872 (89.3%) |
| Endotracheal tubes | 53 (20.8%) | 0 | 53 (5.4%) |
| Fetal stethoscope | 212 (83.1%) | 299 (41.4%) | 511 (52.3%) |
| Gauze | 205 (80.4%) | 494 (68.4%) | 699 (71.6%) |
| Glucometer and test strips | 105 (41.2%) | 104 (14.4%) | 209 (21.4%) |
| Handwashing soap | 149 (58.4%) | 370 (51.3%) | 519 (53.1%) |
| Infusion sets | 208 (81.6%) | 458 (63.4%) | 666 (68.2%) |
| IV small cannula | 229 (89.8%) | 499 (69.1%) | 728 (74.5%) |
| Light source or flashlight | 128 (50.2 %) | 246 (34.1%) | 374 (38.2%) |
| Nasal gastric tube | 57 (22.4%) | 32 (4.4%) | 89 (9.1%) |
| Nebulization device (Nebuliser or spacers) | 80 (31.4%) | 70 (9.7%) | 150 (15.4%) |
| Oropharyngeal airway adult | 63 (24.7% | 0 | 63 (6.5%) |
| Oropharyngeal airway children | 57 (22.4%) | 0 | 57 (5.8%) |
| Oxygen | 100 (39.2%) | 65 (9.0%) | 165 (16.9%) |
| Peak flow meters | 22 (8.6%) | 15 (2.1%) | 3 (3.8%) |
| Pulse oximeter | 59 (23.1%) | 35 (4.9%) | 9 (9.6%) |
| Running water | 227 (89.0%) | 590 (81.7%) | 817 (83.6%) |
| Sharps container | 219 (85.9%) | 642 (88.9%) | 861 (88.1%) |
| Single use standard disposable syringes | 225 (88.2%) | 637 (88.2%) | 862 (88.2%) |
| Skin disinfectant | 222 (87.1%) | 222 (87.1%) | 770 (78.8%) |
| Stethoscope | 244 (95.7%) | 656 (90.9%) | 900 (92.1%) |
| Suction apparatus | 165 (64.7%) | 187 (26.0%) | 352 (36.0%) |
| Thermometer | 232 (91.0%) | 619 (85.7%) | 851 (87.1%) |
| Weigh scales (Adult and children) | 204 (80.0%) | 461 (63.9%) | 665 (68.1%) |
| Support Services | |||
| Blood chemistry analyser | 55 (21.6%) | 12 (1.7%) | 67 (6.9%) |
| Blood transfusion services | 89 (35.0%) | 0 | 89 (9.1%) |
| Blood typing services | 98 (38.4%) | 25 (3.5%) | 123 (12.6%) |
| Communication lines (Cell phone/Telephone/Radio) | 225 (88.2%) | 584 (80.9%) | 809 (82.8%) |
| Diagnostic radiology | 76 (29.8%) | 7 (1.0%) | 83 (8.5%) |
| Gram stain | 79 (31.0%) | 12 (1.7%) | 91 (9.3%) |
| Haemoglobin | 133 (52.2%) | 95 (13.2%) | 228 (23.3%) |
| Laboratory diagnostic services including rapid diagnostic tests | 236 (92.6%) | 569 (78.8%) | 805 (82.4%) |
| Refrigerator | 220 (86.3%) | 408 (56.5%) | 628 (64.3%) |
| Screening blood for HIV, Hepatitis B/C | 46 (18.0%) | 0 | 46 (4.7%) |
| Ultrasound machine in working order | 54 (13.1%) | 16 (2.8%) | 70 (7.2%) |
| Guidelines | |||
| Guidelines for Basic Obstetric Newborn Care | 112 (44.0%) | 154 (21.3%) | 266 (27.3%) |
| Guidelines for Comprehensive Emergency Obstetric Newborn Care | 67 (26.3%) | 81 (11.2%) | 148 (15.2%) |
| Guidelines on Integrated management of Emergency and essential surgical care. |
33 (13.0%) | 26 (3.6%) | 59 (6.0%) |
The hospitals had a median resource availability score of 51.6% IQR (42.2–67.2), the smaller health facilities had a median of 37.5% (IQR 28.1 45.3) and all health facilities combined ranged from 1.6% to 93.8% with a median of 40.6% (IQR 31.3–48.4). Urban hospitals had a greater availability of resources 66.4 (IQR 54.0–76.6) compared to rural hospitals (46.9 (IQR 40.6–59.4), p<0.001. (Supplementary table 2). Mission/Faith based organisation hospitals had the highest resource availability score 75.0 (IQR 73.4–79.7). Government hospitals had a resource availability score of 48.4 (IQR 40.6- 64.1). (Supplementary table 3).
Drugs
The hospitals had a median availability score for drugs of 62.0% IQR (52.4–81.0). Smaller health facilities had a median score of 52.4% IQR (38.1–62.0) and all health facilities combined had a median score of 57.1% IQR (42.9–62.0). One hospital (0.61%) had all of the drugs required to provide emergency and critical care. Two (0.8%) of hospitals did not have any drugs necessary for emergency and critical care. An antibiotic for treating gram negative bacteria was available in 238 (93.3%) and for gram positive bacteria in 212 (83.1%) hospitals.
Equipment
The hospitals had a median resource availability score for equipment of 51.9%, IQR (40.7–66.7). The smaller health facilities had a median score of 37.0% IQR (29.6–48.1%), and all health facilities combined had a median score of 40.7% (33.3–51.9%). Stethoscopes were the most available equipment, and were available in 244 hospitals (95.7%), followed by thermometers in 232 (91.0%). Peak flow meters were the least available resource — present in 22 hospitals (8.6%). Oxygen was available in 100 (39.2%) of the hospitals. Blood pressure cuffs were available in 217 (85.1%). Reliable electricity 24-hours-a-day was available in 63 (24.7%) of all hospitals.
Support services
The hospitals had a median availability score for support services of 33.3% IQR (22.2–77.8). Smaller health facilities had a median score of 22.2% IQR (11.1–22.2%) and all health facilities combined had a median score of 22.2% (11.1–22.2%). Twenty-two hospitals (8.6%) had all the support services necessary for emergency and critical care, 8 hospitals (3.1%) did not have any of the required support services. Laboratory diagnostics including rapid diagnostic tests were available in 236 (92.6%) of hospitals. Ninety-eight hospitals (38.4%) were able to provide blood typing services, 89 (35.0%) could provide blood transfusion services and 46 (18%) were able to screen donor blood for infectious diseases before transfusion. Seventy-six (29.8%) of the hospitals could perform diagnostic radiology.
Emergency Guidelines
The hospitals had a median availability score for emergency guidelines of 33.3% IQR (0–66.7%). Smaller health facilities had a median score of 0 (0%) IQR (0–33.3%). All health facilities combined had a median score of 0 (0%) IQR (0.33.3%). One hundred and twelve (44.0%) hospitals had guidelines for Basic Obstetric and Newborn care, 67 (26.3%) hospitals had guidelines for Comprehensive Emergency Obstetric and Newborn Care and 33 hospitals (13.0%) had guidelines for surgery. Data were lacking in SPA on guidelines on managing other common emergencies and critical conditions.
Infrastructure, Staff Training and Routines
The SPA did not collect any data for indicators in these categories.
Discussion
We have found that hospitals and health facilities in Malawi lack the necessary resources for the provision of emergency and critical care. The median availability score of necessary resources in the hospitals was 51.6%, and for smaller health facilities was 37.5%. The availability of resources in hospitals differed between the categories of resources: there were greater resources for drugs (62.0%) and equipment (51.9%) and fewer for support services (33.3%) and emergency guidelines (33.3%). Urban facilities had significantly higher resource availability scores than rural facilities.
Our findings are similar to studies from Tanzania and Sierra Leone that report a lack of resources for emergency and critical care7,10. These studies also found a greater availability of drugs than other resources — the availability of drugs was 100% in the Tanzanian hospitals and 82% in Sierra Leone. In the Solomon Islands, respondents reported that basic equipment such as pulse oximeters and oxygen concentrators were lacking11. This is also similar to our findings where 59 (23.1%) of Malawian hospitals had pulse oximeters and 100 (39.2%) could provide oxygen. In Tanzania, 90% of the hospitals could provide oxygen while in Sierra Leone oxygen was available in 57%. For equipment, our findings were lower than in the other studies - in Sierra Leone the score was 76%10 and in Tanzania was 90.0%7.
Further studies have reported the lack of necessary resources in low-income country hospitals for managing sepsis, critical illness and emergency care12–15. These are settings with a large burden of severe disease3,4, and yet resources are limited and intensive care units are scarce6,16, supporting the idea that a focus on essential services for all critically ill patients, (i.e the basic services that should be provided to all critically ill patients irrespective of physical location in hospitals), may be most appropriate for emergency and critical care5,17. It has been argued that emergency and critical care are services that should receive greater attention within health systems as mortality rates are high and quality improvement interventions could have a significant impact on reducing mortality at low cost14,18,19.
Our study highlights a lack of data collected about the availability of resources for emergency and critical care. SPA did not collect data about more than half (59.4%) of the resources necessary for emergency and critical care according to standards written for hospitals in low-income countries7. This may imply a lack of prioritisation or a lack of interest in emergency and critical care services in the health system20. Indeed, the Malawi Ministry of Health has since recognized this and as part of the drive to improve quality of care and has initiated plans to improve emergency and critical care services21. Collecting good quality data about resource availability would be an important part of such plans.
Our study's strength is the use of a comprehensive nationwide survey including health facilities throughout the country to investigate the neglected area of emergency and critical care in a low income country16. The study has some limitations. Firstly, the SPA data were collected in 2013–2014 and there may have been some changes to the availability of resources since then. Secondly, some data for emergency and critical care were not collected by SPA — a limitation that is also one of the key findings from the study that the collection of more of such data should be a priority20. Thirdly, data in SPA did not allow a breakdown of facilities by the presence of academic activity or expatriate staff.
Future research should further develop the requirements for essential emergency and critical care in low resource settings5. This could form the basis of minimum requirements for hospitals in Malawi, and should include clinical processes as well as the resources required for care. Implementation and intervention research could then aim to increase coverage of such essential care and evaluate the impact on patient outcomes. The World Health Assembly has recently emphasized the importance of emergency and critical care in health systems, and these efforts could be a crucial part of that challenge22.
Conclusion
Hospitals in Malawi lack resources for providing emergency and critical care. Increasing data about the availability of resources for emergency and critical care and improving the hospital systems for the care of critically ill patients in Malawi should be prioritized.
Figure 1.
Emergency and critical care resource availability scores, by category
Table 2.
Emergency and critical care median resource availability scores, by category
| Category | Hospitals | Smaller Health Facilities | All Health facilities | |||
| Median | IQR | Median | IQR | Median | IQR | |
| All Categories | 51.6% | 42.2–67.2 | 37.5 | 28.1–45.3 | 40.6 | 31.3–48.4 |
| Drugs | 62.0 | 52.4–81.0 | 52.4 | 38.1–62.0 | 57.1 | 42.9–62.0 |
| Equipment | 51.9 | 40.7–66.7 | 37.0 | 29.6–48.1 | 40.7 | 33.3–51.9 |
| Support services | 33.3 | 22.2–77.8 | 22.2 | 11.1–22.2 | 22.2 | 11.1–22.2 |
| Emergency Guidelines | 33.3 | 0–66.7 | 0 | 0–33.3 | 0 | 0–33.3 |
| Training* | - | - | - | - | - | - |
| Infrastructure* | - | - | - | - | - | - |
| Routines* | - | - | - | - | - | - |
Acknowledgements
RKK and TB conceptualised the idea, obtained the data and wrote the first draft of the manuscript and approved the final version. All authors revised the text, contributed scientifically to the manuscript and approved the final version.
Conflict of Interest
The corresponding author is a volunteer intern with the Malawi Meidical Journal.
References
- 1.Baker T. Critical care in low resource settings. Stockholm: Karolinska Institutet; 2015. [Google Scholar]
- 2.Adhikari NKJ, Fowler RA, Bhagwanjee S, et al. Critical care and the global burden of critical illness in adults. The Lancet. 2010;376(9749):1339–1346. doi: 10.1016/S0140-6736(10)60446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dunser MW, Baelani I, Ganbold L. A review and analysis of intensive care medicine in the least developed countries. Crit Care Med. 2006;34(4):1234–1242. doi: 10.1097/01.CCM.0000208360.70835.87. [DOI] [PubMed] [Google Scholar]
- 4.Baker T. Critical care in low-income countries. Trop Med Int Health. 2009;14(2):143–148. doi: 10.1111/j.1365-3156.2008.02202.x. [DOI] [PubMed] [Google Scholar]
- 5.Schell CO, Gerdin Wärnberg M, Hvarfner A, et al. The global need for essential emergency and critical care. Critical Care. 2018;22(1):284. doi: 10.1186/s13054-018-2219-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PLoS One. 2015;10(1):e0116949. doi: 10.1371/journal.pone.0116949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker T, Lugazia E, Eriksen J, et al. Emergency and critical care services in Tanzania: a survey of ten hospitals. BMC health services research. 2013;13:140–140. doi: 10.1186/1472-6963-13-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cerro G, Checkley W. Global analysis of critical care burden. The Lancet Respiratory Medicine. 2014;2(5):343–344. doi: 10.1016/S2213-2600(14)70042-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International. MoHMMaI, author. Malawi Service Provision Assessment(SPA) 2013–14. Maryland USA: Ministry of Health Lilongwe, Malawi and ICF International Rockville; 2014. p. 414. [Google Scholar]
- 10.Coyle RM, Harrison H-L. Emergency care capacity in Freetown, Sierra Leone: A service evaluation. BMC Emergency Medicine. 2015;15(1) doi: 10.1186/s12873-015-0027-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Westcott M, Martiniuk AL, Fowler RA, et al. Critical care resources in the Solomon Islands: a cross-sectional survey. BMC Int Health Hum Rights. 2012;12:1. doi: 10.1186/1472-698X-12-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baelani I, Jochberger S, Laimer T, et al. Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Crit Care. 2011;15(1):R10. doi: 10.1186/cc9410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoyler M, Finlayson SR, McClain CD, et al. Shortage of doctors, shortage of data: a review of the global surgery, obstetrics, and anesthesia workforce literature. World J Surg. 2014;38(2):269–280. doi: 10.1007/s00268-013-2324-y. [DOI] [PubMed] [Google Scholar]
- 14.Dondorp AM, Haniffa R. Critical care and severe sepsis in resource poor settings. Trans R Soc Trop Med Hyg. 2014;108(8):453–454. doi: 10.1093/trstmh/tru099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burke TF, Hines R, Ahn R, et al. Emergency and urgent care capacity in a resource-limited setting: an assessment of health facilities in western Kenya. BMJ Open. 2014;4(9):e006132. doi: 10.1136/bmjopen-2014-006132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vincent J-L, Marshall JC, Ñamendys-Silva SA, et al. Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. The Lancet Respiratory Medicine. 2014;2(5):380–386. doi: 10.1016/S2213-2600(14)70061-X. [DOI] [PubMed] [Google Scholar]
- 17.Manda-Taylor L, Mndolo S, Baker T. Critical care in Malawi: The ethics of beneficence and justice. Malawi medical journal : the journal of Medical Association of Malawi. 2017;29(3):268–271. doi: 10.4314/mmj.v29i3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murthy S, Adhikari NK. Global health care of the critically ill in low-resource settings. Ann Am Thorac Soc. 2013;10(5):509–513. doi: 10.1513/AnnalsATS.201307-246OT. [DOI] [PubMed] [Google Scholar]
- 19.Hirshon JM, Risko N, Calvello EJ, et al. Health systems and services: the role of acute care. Bull World Health Organ. 2013;91(5):386–388. doi: 10.2471/BLT.12.112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riviello ED, Letchford S, Achieng L, et al. Critical care in resource-poor settings: lessons learned and future directions. Crit Care Med. 2011;39(4):860–867. doi: 10.1097/CCM.0b013e318206d6d5. [DOI] [PubMed] [Google Scholar]
- 21.Malawi_Ministry_of_Health_and_Population. Quality Management Policy for the Health Sector. 2017. [Google Scholar]
- 22.WHO, author. Emergency care systems for universal health coverage: ensuring timely care for the acutely ill and injured. Report by the Director-General for the 72nd World Health Assembly 2019. [Google Scholar]