Abstract
To conduct a systematic review and develop a conceptual framework on the mechanisms linking loneliness, social isolation, health outcomes and mortality. Electronic databases were systematically searched (PubMed, MEDLINE, Scopus and EMBASE) from inception to October 2018 followed by manual searching to identify research on loneliness, social isolation and mortality in adults published in the English language. Articles were assessed for quality and synthesised into a conceptual framework using meta-ethnographical approaches. A total of 122 articles were included. These collated observational designs examining mediators and moderations of the association in addition to qualitative studies exploring potential mechanisms were included. A framework incorporating 18 discrete factors implicated in the association between loneliness, social isolation and mortality was developed. Factors were categorised into societal or individual, and sub-categorised into biological, behavioural and psychological. These findings emphasise the complex multidirectional relationship between loneliness, social isolation and mortality. Our conceptual framework may allow development of more holistic interventions, targeting many of the interdependent factors that contribute to poor outcomes for lonely and socially isolated people.
Keywords: Social conditions and disease, health policy, qualitative research, health promotion
Introduction
Loneliness and social isolation are increasingly recognised epidemics within our societies.1 Although frequently used interchangeably, these are distinct conditions.2 Loneliness is defined as the subjective experience of feeling alone3 and is commonly assessed using self-report scales. It reflects an individual’s dissatisfaction with the frequency and closeness of their social contacts. Social isolation, in contrast, is defined as an objective measure quantifying social contacts assessed by metrics such as network size.4 A recent survey carried out by the British Office for National Statistics suggests that loneliness is experienced by 5% of all UK adults.5 Nearly one million people in the survey said that they always or often felt lonely, and 3.6 million aged over 65 years reported their televisions as a main source of company. Loneliness and social isolation are more common with increasing age due to factors including reduced mobility, impaired speech or hearing, cognitive decline, loss of social networks, fragmentation of families, greater ill health and limited financial resources.6
Individuals who experience loneliness or social isolation have an increased risk of cardiovascular disease (social isolation relative risk [RR] = 1.29, 95% confidence interval [CI] 1.04–1.59, p = 0.02), stroke (social isolation RR = 1.32, 95% CI 1.04–1.68, p = 0.02) and all-cause mortality (loneliness hazard ratio [HR] = 1.22, 95% CI 1.10–1.35, p < 0.001).2,7,8 They are more likely to be diagnosed with depression9 and dementia,10 and suffer from multimorbidity.11
Efforts to reduce loneliness and social isolation are therefore a high priority to the UK government as reflected by the appointment of the first minister for loneliness in 2018.12 To date, evidence of successful interventions to combat loneliness and social isolation in the community are lacking.13 In part, research has been hampered by the fact that these are often examined together rather than as two independent processes.1 There is also a paucity of conceptual understanding on the pathways and mechanisms that might explain the link between loneliness, social isolation, health outcomes and mortality.14 Understanding of these pathways could inform future intervention development. Accordingly, we systematically identified and synthesised evidence into a single conceptual model to explain the pathways between loneliness, social isolation, health outcomes and mortality.
Methods
Systematic review
Data sources and searches
We followed the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidance15 and searched the following databases from inception to January 2019: MEDLINE, PubMed, Scopus and EMBASE. We initially included the terms loneliness, social isolation and mortality as shown in Table 1. The term ‘health outcomes’ was too broad on our initial searches, so we modified our search strategy and restricted this to ‘cardiovascular disease’ in response to a recent meta-analyses on this subject.7 Manual searching of references from previous reviews was also conducted and we additionally looked through conference abstracts.
Table 1.
Search criteria used across scientific databases from inception until October 2018.
| Boolean logic terms used in our search |
| ((Loneliness) or (social isolation)) and Mortality |
| ((Loneliness) or (social isolation)) and Cardiovascular disease |
| ((Loneliness) or (social isolation)) and Mortality and Mechanism |
| ((Loneliness) or (social isolation)) and Mortality and Cause |
| ((Loneliness) or (social isolation)) and Mechanism and Mortality |
| ((Loneliness) or (social isolation)) and Cause and Mortality |
Study selection
Studies assessing relationships between loneliness, social isolation and health outcomes were included in analysis. We included studies of any design in adults over 18 years within middle- and high-income countries. Low-income countries, as defined by World Bank criteria, were excluded due to the differing social and healthcare context that would limit application to UK populations. We did not have the resources to include translation services and so restricted studies to those published in the English language. Other exclusion criteria were animal studies or non-scientific articles.
Data extraction and risk of bias assessment
All titles and abstracts were initially screened by one researcher and then a subset (50%) were independently screened by a second researcher (HD-M). Full-text articles were reviewed by two researchers, and disagreements between researchers resolved by discussion. We extracted data on study design, participants, setting, country, lists of exposure and outcomes variables (in cohort study), and intervention description if any. We also looked at the completeness of outcome data. If these were not reported, we contacted study authors. We then used the Critical Appraisal Skills Programme (CASP) checklist to assess methodological rigour of included papers and we examined relevance through pre-determined research criteria as set out by Dixon-Woods et al.16 Included articles were independently scored as either ‘key’ (providing rich data for synthesis) or ‘satisfactory’ (providing some valuable data) by two researchers, and agreement reached through discussion.
Meta-ethnography
Synthesis of included studies were undertaken using validated meta-ethnographical techniques and definitions.17 In brief, data were extracted from each study using a standardised form to summarise main themes alongside critical appraisal as described above. One researcher extracted data from all studies, and then data were additionally extracted from a sample of studies by two researchers. Schutz’s model of first-, second- and third-order constructs was used to synthesise data from initially extracted themes into one conceptual framework. The significant heterogeneity in methodologies, exposures and outcomes limited direct comparison between studies, so data and subsequent constructs were not weighted in the meta-ethnographical process.
First-order constructs
Included papers were read in full to extract first-order constructs. First-order constructs were data relating to loneliness, social isolation, cardiovascular disease and mortality. Themes emerging from first-order constructs were recorded alongside extracted data, for example the theme of increased inflammation arising from studies assessing isolated biomarkers such as C-reactive protein and erythrocyte sedimentation rate.
Second-order constructs
Author interpretations of first-order constructs were further developed into second-order constructs through discussions and several iterations. Second-order constructs were organised in reverse chronological order, i.e. with data from the oldest publications integrated last, and then grouped into broader themes. These were based solely upon primary data captured within first-order constructs. Themes were discussed between authors and the process was repeated several times until agreement was reached.
Third-order constructs
This final step involved both first- and second-order constructs being synthesised into a conceptual framework. Two authors listed first and second author constructs in an electronic table, and then independently developed an overarching framework to link the constructs and author interpretations. These frameworks were merged and presented for discussion. We went through several iterations of the framework and through further refinement and discussion, agreement was reached. The validity of our approach to developing this has been described previously.17
Results
Systematic review
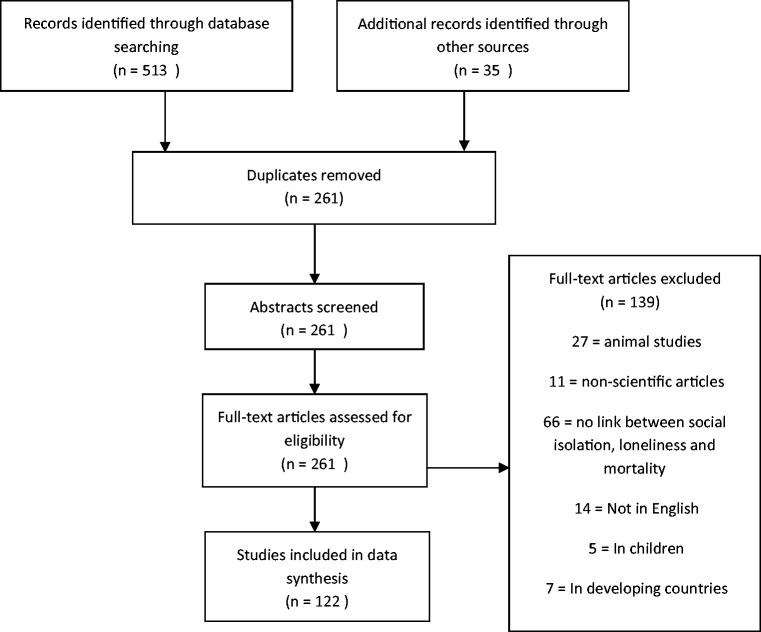
A total of 513 papers were identified through search criteria and a further 35 through reference screening (Figure 1). After duplicates were removed, 261 abstracts were screened for relevance and 122 were included. A full reference list of included papers is available in online Appendix 1. A summary of included papers’ characteristics is included in online Appendix 2. Reasons for study exclusion are listed in the PRISMA flow chart (Figure 1). Using the CASP checklist, nine articles were excluded mainly due to unclear methods of data collection (online Appendix 1). A broad range of tools to describe loneliness and social isolation were observed across studies which to some extent limited our ability to synthesise evidence. There was also variation in how loneliness and social isolation were measured. Loneliness was most commonly assessed by multiple-item scales such as the UCLA Loneliness Scale.18 In several studies, loneliness was assessed by only a single question. Social isolation was commonly measured using more validated tools such as the Social Isolation Scale, Friendship Scale and Social Network Index.6
Figure 1.
Flow diagram demonstrating number of research articles identified in searches, screened, assessed for eligibility, included in data synthesis, and excluded, in line with PRISMA guidelines.
Loneliness and social isolation
While loneliness and social isolation are independent conditions, the two also frequently coexist1 individuals who are lonely are more likely to be socially isolated, and individuals who are socially isolated are more likely to be lonely.6,8 This interdependence was rarely unpicked in the existing literature. Often, studies assumed that they were same thing or reported on one of these. For example, a scoping review reported on loneliness and social isolation in studies examining existing health condition.1 It suggests that 75% of studies into depression include a measure of loneliness without considering social isolation, while 72% of studies on cardiovascular disease assessed social isolation without loneliness. Direct comparisons between individual and collective effects of loneliness and social isolation were limited by the paucity of published data.
First-, second- and third-order constructs
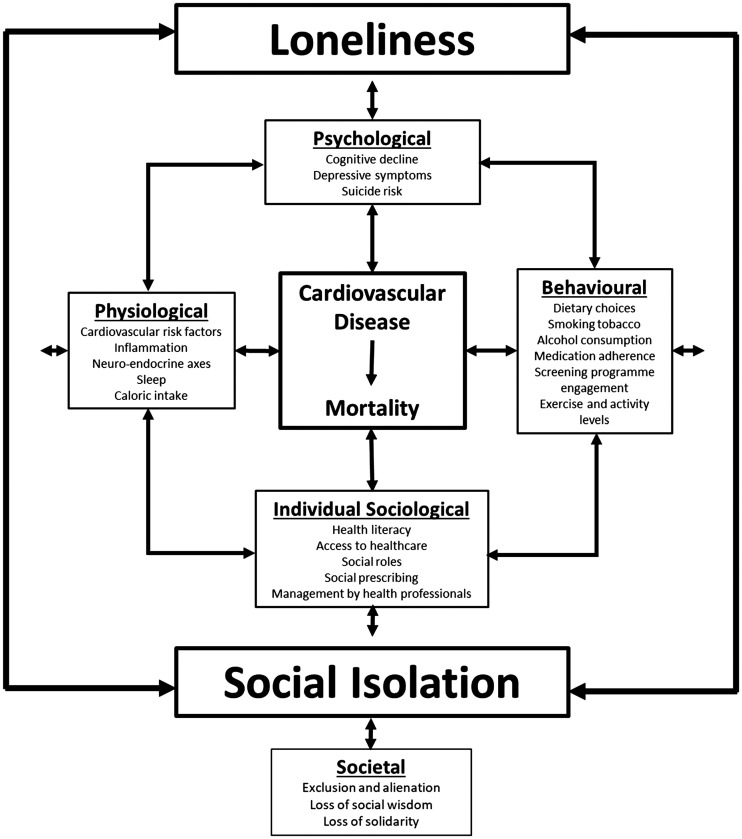
First-order constructs extracted from each of the 122 included papers are shown in online Appendix 1. Second-order constructs are summarised in Table 2. A single conceptual framework integrating first- and second-order constructs is depicted in Figure 2. The conceptual framework we developed could not acknowledge the significant interdependence between constructs and themes. For example, harmful behaviours such as smoking can have a significant addictive effect on psychological and physiological elements which in turn impacts cardiovascular disease risk factors. Moreover, smoking is more prevalent within certain socioeconomic groups. The frequency and complexity of such relationships between constructs preclude their inclusion in our framework but we integrated as much as we could from first- and second-order construct into third-order construct.
Table 2.
Second-order constructs implicated in the association between social isolation, loneliness, cardiovascular disease and mortality, grouped according to theme.
| Physiological |
| Cardiovascular risk factors (including cholesterol, HbA1c, blood pressure) |
| Inflammation |
| Quality and duration of sleep |
| Caloric intake |
| Neuro-endocrine axes |
| Psychological |
| Cognitive decline |
| Depressive symptoms |
| Suicide risk |
| Behavioural |
| Dietary choices |
| Smoking tobacco |
| Alcohol consumption |
| Medication adherence |
| Screening programme engagement |
| Exercise and activity levels |
| Sociological |
| Health literacy |
| Access to healthcare |
| Social roles |
| Social prescribing |
| Quality of management by healthcare professionals |
| Exclusion and alienation |
| Loss of social wisdom |
| Loss of solidarity |
Figure 2.
Conceptual framework demonstrating mechanisms underlying associations between loneliness, social isolation, cardiovascular disease and mortality. The outer coloured layer represents loneliness and social isolation; their interaction and interdependence is demonstrated with bi-directional arrows. Factors implicated in the association between loneliness, social isolation, cardiovascular disease and mortality were grouped into ‘psychological,’ ‘behavioural,’ ‘sociological’ and ‘physiological’. The associations between these categories, cardiovascular disease, mortality, loneliness and social isolation are demonstrated through bi-directional arrows. Outside the coloured layer, the broader impact of loneliness and social isolation on wider society and its reciprocal relationship is demonstrated under the ‘societal’ category.
Developing a conceptual framework
Multiple pathways underlying the associations between loneliness, social isolation, cardiovascular disease and mortality were identified. During framework development, constructs were divided into societal and individual mechanisms. After further discussion, individual constructs were grouped into four broader themes: physiological, psychological, behavioural and sociological. This grouping simplified our framework and understanding of the pathways involved. Themes arose from first-order constructs and were not a priori selections by researchers. The conceptual model is shown in Figure 2 and each of themes included is discussed in more detail below.
This conceptual model is best understood from the starting point of loneliness and social isolation, depicted as a layer within our model, with their interaction depicted with bi-directional arrows. We conceptualise factors implicated in the pathways between loneliness, social isolation, cardiovascular disease and mortality within four categories, demonstrated on pathways to cardiovascular disease and mortality highlighted by arrows. In turn, there is significant interaction between these categories; and further interaction between factors within these categories and cardiovascular disease, loneliness and social isolation, as depicted by further bi-directional arrows. Finally, the broader impact of loneliness and social isolation on societal factors, and vice versa, is captured outside the pathways implicated in associations with cardiovascular disease and mortality.
Physiological factors
We found that the risk of mortality remains elevated in loneliness even after controlling for social and behavioural factors, suggesting involvement of biological mechanisms19 which we incorporated into our conceptual framework (Figure 2). It is hypothesised that loneliness triggers a significant neuroendocrine response. Those who feel lonely or are judged to be socially isolated can show elevated activation of the hypothalamic-pituitary-adrenal (HPA) axis, an increased chronic stress response, elevated blood pressure and serum cortisol.20 These are then independently associated with an increased risk of cardiovascular disease and death.20 Both loneliness and social isolation have additionally been associated with reduced quality and duration of sleep,21 although it is unclear if this occurs as a result of, or independent of, HPA axis dysfunction. Higher levels of inflammatory markers may be an additional contributor. We found evidence that both loneliness and social isolation correlate with C-reactive protein and fibrinogen which have previously been associated with cardiovascular disease and mortality.22 Loneliness also correlates with an increased rate of cognitive decline.23 In addition to predisposing to conditions with known increased mortality risk, such as dementia, reduced cognition may influence social and behavioural risk factors, for example impacting on medication adherence, physical activity and the ability to seek help.
Psychological and behavioural factors
Psychological and behavioural mechanisms underlying the association between social isolation, mortality, cardiovascular disease and death are demonstrated in Figure 2. Loneliness is associated with increased rates of both depression and suicide.9 These relationships demonstrate significant interdependence. Harmful behaviours associated with increased mortality are more common in those who are lonely or isolated. Both lonely and socially isolated individuals are more likely to smoke, drink alcohol and make poor dietary choices.24 They are less likely to leave their homes regularly to participate in exercise and have poor adherence to prescribed medication.25
Sociological factors
Figure 2 depicts sociological factors implicated in the associations between loneliness, social isolation, cardiovascular disease and mortality. These are divided into individual sociological factors and broader societal factors. Social roles are protective against mortality in lonely individuals, with the feeling of ‘being needed’ the most protective factor for reduced mortality.3 Those who are isolated are also less likely to be able to access emergency and routine healthcare due to a smaller network from which to seek help and a lack of access to transport.25 We also found evidence of poor care delivery from healthcare professionals who perceive this group as hard to treat and time-consuming.6 This may exacerbate poor health outcomes. Loneliness is additionally associated with harm to the broader society, through loss of solidarity, the alienation of exclusion and the loss of social wisdom. There are also increased costs to individuals and their society through increased healthcare utilisation and longer hospitalisations amongst those who are lonely.26 Our review identified a few papers examining mortality outcomes after social prescribing interventions, defined as non-medical interventions aimed at addressing wider determinants of health.13 In the short term, elderly populations report satisfaction from psychosocial platforms such as art, therapeutic writing and group exercise.13 However, we found no evidence of studies reporting on long-term endpoints such as mortality or cardiovascular disease, although surrogate predicted long-term outcomes look promising.13
Discussion
Key findings
In this study, we carried out a systematic review and meta-ethnography to develop a conceptual framework explaining the pathways that link loneliness, social isolation, cardiovascular disease and mortality. We identified multiple factors that might contribute to this pathway which were then grouped from over 20 uncategorised constructs into four simple concepts of physiological, psychological, behavioural and sociological factors. We then connected concepts and individual variables taking into account direction and interactions in a single conceptual framework.
Comparison to existing literature
To the best of our knowledge, this is the first study to provide a comprehensive overview and synthesis of the literature to explore the pathways underlying the association between loneliness, social isolation, cardiovascular disease and mortality.1 By integrating findings from the existing literature, we present a framework which attempts to unify the numerous interdependent associations underpinning these pathways with the purpose of informing future intervention development. Cotterell et al. present an ecological framework to identify risk factors for social isolation at individual, relationship, community and societal levels, and review interventions to prevent social isolation.14 Their approach does not incorporate understanding of how social isolation may lead to poor health outcomes or mortality, nor does it integrate loneliness. Doane et al. present a model associating loneliness with cortisol activity, describing several dynamic pathways underlying this mechanism over timescales from immediate to chronic.27 While this model describes a meaningful mechanism by which loneliness may cause cardiovascular disease and increased mortality, it does not integrate alternate pathways, nor does it incorporate social isolation. Other authors have presented models defining the interaction between social isolation, inflammation, gender and mortality, but have not integrated loneliness or alternate mechanisms.28
Strengths and limitations
We conducted a comprehensive literature review across several databases and included manual searching to capture as many relevant studies as possible. We did not limit study design and carried out rigorous abstract checking with appraisal using the CASP tools to ensure high-quality inclusions. However, our searches were restricted to studies published in the English language and to high-income countries. This may limit generalisability of our findings. The inconsistency with which the terms loneliness and social isolation are used within the literature additionally limits generalisability of findings. We were unable to provide weighting evidence of each included paper due to the inclusion of both qualitative and quantitative data, although this approach contributed to a more holistic and comprehensive framework. The interdependence between factors in our framework was not fully considered and we did not attempt to qualitatively analyse the relative effect sizes of different factors within our framework. These challenges were partially overcome through construct iteration and discussion between researchers.
Future research and conclusions
In this study, we highlight the complex multidirectional relationship between loneliness, social isolation, cardiovascular disease and mortality. The evidence for effectiveness and cost benefit of interventions to address loneliness and social isolation remains weak.13 Ongoing trials describe constructs included within our framework as endpoints – such as blood pressure and cholesterol status – while omitting others such as alcohol usage, smoking and depressive symptoms. We suggest that the use of our framework during the planning stage of interventions may allow development of more holistic interventions, targeting many of the interdependent factors that contributing to poor outcomes for lonely and socially isolated people. For example, initiation of a social prescription could trigger a broader health screen for associated co-morbidities including hypertension, hypercholesterolaemia, alcohol dependence, depression and cognitive decline; early identification and treatment of these on a population level might confer an overall morbidity and mortality reduction.
Application of our framework to individual patients may permit greater appreciation of the multiple interdependent and contributing factors to that individual’s loneliness. This will allow practitioners to develop personalised management strategies that acknowledge the interdependence of those factors. For example, one might consider an elderly widowed patient with hypertension, alcohol dependence, depression, insomnia and malnutrition who has stopped attending his bridge club. Signposting this individual towards a local alcohol dependency service might provide initial social connection, followed by education on the harms of alcohol consumption and targeted dietary advice. Reduction in alcohol consumption may in turn improve depressive symptoms, alleviating insomnia and anhedonia and promoting resumption of previous social activities and connections.
On a policy level, the large cost on adult social and healthcare services of social isolation and loneliness is a clear incentive to improve outcomes.29 Both social isolation and loneliness are associated with increased levels of deprivation, and considerations of addressing these inequalities should be incorporated into any large-scale intervention.29 The need for a joined-up approach between healthcare and social care agencies in tackling the issue is clear.30
Supplemental Material
Supplemental material, JRS918236 Supplemental Material for Loneliness, social isolation, cardiovascular disease and mortality: a synthesis of the literature and conceptual framework by Sam Hodgson, Isabella Watts, Simon Fraser, Paul Roderick and Hajira Dambha-Miller in Journal of the Royal Society of Medicine
Acknowledgements
None.
Declarations
Competing interests
None declared.
Funding
None declared.
Ethics approval
NA.
Guarantor
HDM.
Contributorship
HDM, SF, PR & IW conceived the study. Data were extracted and analysed by SH, IW, HDM. SH & IW were responsible for data anlysis and writeup. SF & PR interpreted and contextualised results.
Provenance
Not commissioned; peer-reviewed by Johanna Lynch.
ORCID iD
Sam Hodgson https://orcid.org/0000-0002-5610-850X Isabella Watts https://orcid.org/0000-0003-1974-2365 Hajira Dambha-Miller https://orcid.org/0000-0003-0175-443X
Supplemental material
Supplemental material for this article is available online.
References
- 1.Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Community 2017; 25: 799–812. [DOI] [PubMed] [Google Scholar]
- 2.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci 2015; 10: 227–237. [DOI] [PubMed] [Google Scholar]
- 3.Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med 2010; 40: 218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: changes in core discussion networks over two decades. Am Sociol Rev 2006; 71: 353–375. [Google Scholar]
- 5.Office for National Statistics. Loneliness – what characteristics and circumstances are associated with feeling lonely? See https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/lonelinesswhatcharacteristicsandcircumstancesareassociatedwithfeelinglonely/2018-04-10 (last checked 18 December 2019).
- 6.Cacioppo JT, Hawkley LC, Berntson GG. The anatomy of loneliness. Curr Dir Psychol Sci 2003; 12: 71–74. [Google Scholar]
- 7.Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 2016; 102: 1009–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rico-Uribe LA, Caballero FF, Martín-María N, Cabello M, Ayuso-Mateos JL, Miret M. Association of loneliness with all-cause mortality: a meta-analysis. PLoS One 2018; 13: e0190033–e0190033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang EC, Chang OD, Lucas AG, Li M, Beavan CB, Eisner RS. Depression, loneliness, and suicide risk among latino college students: a test of a psychosocial interaction model. Soc Work 2019; 64: 51–60. [DOI] [PubMed] [Google Scholar]
- 10.Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry 2007; 64: 234–240. [DOI] [PubMed] [Google Scholar]
- 11.Jessen MAB, Pallesen AVJ, Kriegbaum M, Kristiansen M. The association between loneliness and health – a survey-based study among middle-aged and older adults in Denmark. Aging Ment Heal 2018; 22: 1338–1343. [DOI] [PubMed] [Google Scholar]
- 12.Pimlott N. The ministry of loneliness. Canadian Family Physician 2018; 64: 166–167. [PMC free article] [PubMed] [Google Scholar]
- 13.Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017; 7: e013384–e013384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cotterell N, Buffel T, Phillipson C. Preventing social isolation in older people. Maturitas 2018; 113: 80–84. [DOI] [PubMed] [Google Scholar]
- 15.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339: b2700–b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006; 6: 35–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008; 8: 21–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol 1980; 39: 472–480. [DOI] [PubMed] [Google Scholar]
- 19.Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging 2010; 25: 132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eisenberger NI, Taylor SE, Gable SL, Hilmert CJ, Lieberman MD. Neural pathways link social support to attenuated neuroendocrine stress responses. Neuroimage 2007; 35: 1601–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smagula SF, Stone KL, Fabio A, Cauley JA. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Med Rev 2016; 25: 21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hänsel A, Hong S, Cámara RJA, von Könel R. Inflammation as a psychophysiological biomarker in chronic psychosocial stress. Neurosci Biobehav Rev 2010; 35: 115–121. [DOI] [PubMed] [Google Scholar]
- 23.Lara E, Martín-María N, De la Torre-Luque A, Koyanagi A, Vancampfort D, Izquierdo A, et al. Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res Rev 2019; 52: 7–16. [DOI] [PubMed] [Google Scholar]
- 24.Malcolm M, Frost H, Cowie J. Loneliness and social isolation causal association with health-related lifestyle risk in older adults: a systematic review and meta-analysis protocol. Syst Rev 2019; 8: 48–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A 2013; 110: 5797–5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health 2015; 105: 1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doane LD, Adam EK. Loneliness and cortisol: momentary, day-to-day, and trait associations. Psychoneuroendocrinology 2010; 35: 430–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang YC, McClintock MK, Kozloski M, Li T. Social isolation and adult mortality: the role of chronic inflammation and sex differences. J Health Soc Behav 2013; 54: 183–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clake M, Bowers J and Harris F. Social Isolation and Loneliness in Hampshire A Health Needs Assessment, 2016. See https://documents.hants.gov.uk/corprhantsweb/2017-07-04SocialIsolationandLonelinessinHampshireHF000014384094.pdf (last checked 6 Jan 2020).
- 30.Public Health Matters. Loneliness and Isolation: Social Relationships Are Key to Good Health. See https://publichealthmatters.blog.gov.uk/2015/12/08/loneliness-and-isolation-social-relationships-are-key-to-good-health/ (last checked 6 January 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, JRS918236 Supplemental Material for Loneliness, social isolation, cardiovascular disease and mortality: a synthesis of the literature and conceptual framework by Sam Hodgson, Isabella Watts, Simon Fraser, Paul Roderick and Hajira Dambha-Miller in Journal of the Royal Society of Medicine