Background
The incidence of emerging infectious diseases in humans has increased in the recent past and will continue to do so in the near future. The emergence of novel coronavirus (CoV) [severe acute respiratory syndrome-CoV-2 (SARS-CoV-2)] which causes CoV diseases or COVID-19 was first identified in Wuhan city of China in December 2019, when a cluster of unusual respiratory illnesses dominated by pneumonia was reported1,2. The initial cases were linked to a seafood wholesale market in Wuhan city; subsequently, many cases rapidly emerged with no linkage to the seafood market, indicating a person-to-person spread3. On January 30, 2020, the World Health Organization (WHO) declared the CoV epidemic or COVID-19 centred in Wuhan in Hubei province 'a public health emergency of international concern' (PHEIC)4. The WHO Director-General Dr Tedros Gabreseus said, “the decision to announce a PHEIC was made because of signs of human-to-human transmission outside China and WHO's concern regarding what might happen if the virus were to spread in a country with a weaker health system”4. On March 11, 2020, the WHO characterized COVID-19 as a pandemic5.
Genetic analysis early in the outbreak in China revealed that the virus was similar to, but distinct from, SARS-CoV-1, however, the closest genetic similarity was found in a CoV that had been isolated from bats6. CoVs are a family of large, enveloped, positive-strand RNA viruses that can be divided into four genera: alpha, beta, delta and gamma, of which alpha- and beta-CoVs are known to infect humans. Four HCoVs (HCoV 229E, NL63, OC43 and HKU1) are endemic globally and account for 10-30 per cent of upper respiratory tract infections in adults7.
In the 21st century, two highly pathogenic human CoVs - SARS-CoV-1 and Middle East respiratory syndrome (MERS)-CoV - emerged from animal reservoirs to cause outbreaks in many countries with alarming morbidity and mortality. The CoVs are ecologically diverse, with the greatest variety seen in bats, suggesting that they are the reservoirs for many of these viruses7,8. Peri-domestic mammals serve as intermediate hosts, facilitating recombination and mutation events, furthering the expansion of genetic diversity7.
Evolving global situation
The COVID-19 pandemic situation is at present rapidly evolving. The situation began in Wuhan in December 2019, an alert was issued by the Wuhan Municipal Health Commission on December 31, and the same day, a notification was made to the WHO3. On January 7, 2020, the causative pathogen was identified as a novel CoV9. Realizing the threat of rapid spread, China implemented a lockdown in Wuhan city, the epi-centre, to prevent further spread, even as cases started rising and more Chinese provinces were affected3, leading to declaration of a PHEIC on January 30, 20204.
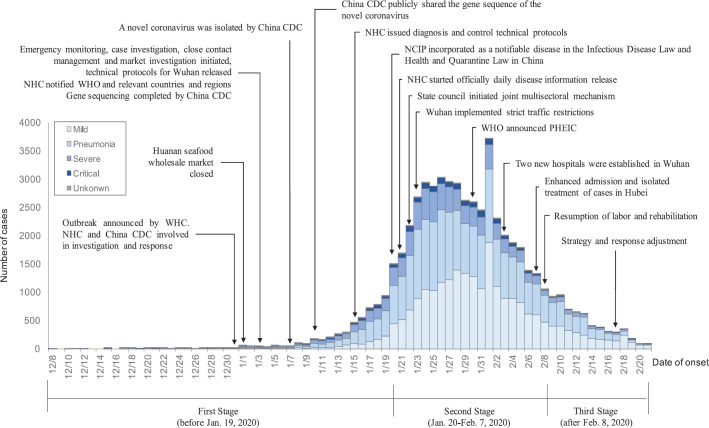
Till March 21, 2020, a total of 292,142 confirmed cases of COVID-19 had been reported to the WHO from 192 countries, with 12,784 deaths10. China reported a total of 113,702 confirmed cases and 4,012 deaths from 27 provinces. Of these, 83 per cent were reported from Hubei province alone. In provinces other than Hubei, the cases occurred either sporadically or human-to-human transmission was observed in clusters among families. Following the lockdown, the cases and deaths in China started to decline (Figure)3,11. The data also suggested that 80 per cent of cases in China were of mild nature and the severity increased with age, indicating that the elderly and those with underlying chronic conditions were at a higher risk of severe disease and dying11.
Figure.
Coronavirus disease-19 epidemic curve and major interventions implemented in China. CDC, Centers for Disease Control and Prevention; NHC, National Health Commission; WHO, World Health Organization; NCIP, novel coronavirus (2019-nCoV)-infected pneumonia; PHEIC, Public Health Emergency of International Concern. Source: Reproduced with permission from Ref. 11.
Over the recent weeks, a global spread of the infection at large, and at times a sharp increase in cases and deaths is occurring in countries outside China, namely South Korea, Iran, Italy and Spain. These include now cases with no clear link to China. A more focal community transmission may be presently underway in these countries, as well as in cruise ships. Therefore, the global outbreak is now undergoing a remarkable and ominous shift. While cases are declining in China, the pandemic caused by the novel virus is engulfing several countries of the world, both developed as well as developing ones12. COVID-19 is currently confirmed in nearly 192 countries around the world. The WHO revised the risk assessment on February 28, to very high, at regional as well as global level12.
The spread of COVID-19 to African region has been an issue of concern due to the relatively vulnerable health system13. Africa had remained unaffected till February 13, 2020, but now, it has 37 countries affected with more than 600 confirmed cases13. These recent developments have led to deep concerns that the pandemic will have grave health, social and economic consequences around the world.
India's response
In India, 283 confirmed cases and four deaths have been reported as of March 21, 2020, with many having had travelled to affected countries10. A few cases have occurred in a cluster, among family members. However, there are no reports of community transmission so far in the country.
While intensifying preparedness for the unprecedented threat posed by COVID-19, the Government of India (GOI) has constituted an inter-ministerial committee represented by the ministers of the Ministry of Health and Family Welfare, External Affairs, Home, Civil Aviation as well as the National Disaster Management Authority14. Several measures have been undertaken by the government for the early detection of cases including thermal screening at the international airports, major and minor seaports and land crossings. So far, more than half million incoming airline passengers and thousands coming through seaports have undergone the screening procedure. To engage the community, Gram Sabhas are organizing awareness drives regarding clinical presentation of the novel CoV diseases, preventive measures, and the need for reporting especially in the villages in border districts15.
The Integrated Disease Surveillance Programme (IDSP) based at the National Centre for Disease Control (NCDC), Delhi, has been conducting entry screening for all passengers arriving from other countries and has augmented community surveillance for severe acute respiratory illnesses. The national guidelines on surveillance, case investigation and laboratory detection of COVID-19 cases have been developed by the NCDC and made available to all States16.
The relevant laboratories across the country are working as a part of network of testing facilities for SARS-CoV-2 in accordance with the national testing guidelines developed by the Indian Council of Medical Research (ICMR)17. A 24×7 call centre has been operational at the NCDC from an early stage of COVID-19 outbreak which provides information and guidance about testing facilities and their location, sample collection facilities, as well as other aspects of the pandemic. The States/Union Territories (UTs) are on alert, and stock of personal protection equipment and face masks is progressively being augmented18.
The general public is advised to avoid travel to affected countries and visas of foreign nationals traveling from affected countries have been cancelled. The government has organized daily briefing for media with updates on the novel CoV situation as is evolving in the country.
The planning and preparedness for the next phase of the outbreak is indeed critical, currently seen in many countries reporting focal clusters of cases in the community and rapid escalation of the situation for the worst. Therefore, preparedness and readiness to have a public health surge capacities is urgently needed in the country. These would include active surveillance and expanded testing, contact tracing, isolation and management of cases after triage. In order to strengthen the national capacity for surveillance and outbreak investigation, we need to mobilize and effectively utilize the field epidemiology workforce, which is already trained and has skills in epidemiological analysis and disease control.
The India Epidemic Intelligence Service or India EIS programme run by the NCDC, in collaboration with the US Centers for Disease Control and Prevention (CDC), has been actively supporting the COVID-19 response. Established in 201219, this two-year, post-graduate, applied field epidemiology training programme is modelled after CDC's EIS programme and has now expanded to two additional hubs - the WHO India Country Office and ICMR's National Institute of Epidemiology, at Chennai. At present, 45 EIS officers (32 alumni and 13 currently in the programme) are supporting various States in this pandemic containment exercise, including Kerala, Maharashtra, Nagaland and Uttar Pradesh. The India EIS Programme has so far graduated 64 officers (across 21 States) through the end of 2019. During 2020, over 60 officers will be in training across the three hubs.
India EIS officers work in national or State government health programmes to evaluate disease surveillance systems; investigate outbreaks; respond to disasters, emergencies and mass gatherings and conduct epidemiological evaluations. The programme has great potential in strengthening epidemiological capacity in the country to respond effectively to public health emergencies such as COVID-19; strengthening core capacity in disease surveillance, early detection and rapid response and generating evidence that can be used for policymaking and implementation.
Challenges amidst uncertainties
Clearly, SARS-CoV-2 is not the first and would not be the last challenge to confront India. There is a need to report, promptly and openly, cases of any disease with the potential for international spread. In 2003, delay in reporting of early cases of SARS originating in China led to the virus spreading to 17 countries as far as North America and causing 774 deaths20. The outbreak was brought under control swiftly, within four months. The outbreak was, however, associated with considerable direct costs due to intensive medical care and control interventions, but the cost of social disruption and economic losses was clearly much higher than the medical cost.
To enable the world to deal with a situation such as this, the revised International Health Regulations (IHR) (2005) were adopted by the World Health Assembly in 2005, which called for developing core capacities in each member country to combat PHEIC21. The IHR (2005) core capacities are required to detect, assess, notify and report events and respond to public health risks and emergencies of national and international concern, as stipulated in Articles 5 and 13, and Annex 1, of the regulations22. The IHR (2005) requires all countries to be prepared at all times by strengthening their surveillance and response capacities to be able to deal with the new and emerging pathogens.
The COVID-19 pandemic is unfolding at a rapid pace. There are uncertainties how it will evolve in the coming days and what impact it will have. Almost on a day-to-day basis, new information is becoming available, helping us to better understand the new virus in terms of its natural history, incubation period, the period of communicability and case fatality rates. It has been clear from the beginning that the novel CoV is more infectious but less deadly compared to SARS23. New data are emerging which suggest that transmission can occur while the person is either at a pre-symptomatic phase or has only a mild disease24, which has major implications for disease transmission in communities, for identifying cases and contact tracing.
Investing in preparedness and health system strengthening
To respond to the ongoing pandemic and such events in the future, identification of critical public health measures and systemic investment in those is of utmost importance and includes the following:
First, we need to focus on preventing new infections and saving lives. A strong real-time national surveillance to detect COVID cases, respond rapidly by active case finding, prompt treatment and isolation of cases and contact tracing, thereby preventing an outbreak from happening or limiting its spread to the general population by immediate containment measures. Other than the ICMR-National Institute of Virology at Pune, the NCDC at New Delhi and other laboratories, it is necessary to expand network of virus diagnostic laboratories in private sector with adequate surge capacity to respond swiftly to the current and future events. Preparedness for ensuring skilled and trained human resources at all levels of health care by building their capacity is essential especially before the community transmission of the novel coronavirus occurs. The healthcare workers, who are at a high-risk of infection, need to strictly follow infection control procedures while managing critically ill patients. The WHO has recently issued guidelines on 'Infection Prevention and Control (IPC) for Novel Coronavirus (COVID-19)'25. Adequate amount of essential medical supplies such as personal protection equipment (PPEs), N95 face masks, hand sanitizers, test kits for diagnosis and ventilators should be made available.
Second, we need to empower individuals and community for efficient response through information, education and communication. At personal level, one needs to take precautions to avoid getting himself/herself infected with the virus. These precautions include 'staying at home' especially when sick, and thus not infecting others; covering your mouth or nose while coughing or sneezing; avoiding touching eyes, nose or mouth; regular and thorough hand washing with soap and water at least for 20 sec; and cleaning the frequently touched surfaces such as table, door handle etc., with a disinfectant, social or physical distancing at community level to protect those at high-risk of severe disease such as elderly and those with underlying chronic conditions and healthcare workers.
Finally and importantly, we need to ensure a resilient and responsive health system which can run itself in a sustainable manner. For this, adequate and sustained financing of health is required. The most important lesson we have learnt during the present pandemic as well as the past pandemics is that investing in preparedness can cost little and could save millions of lives.
The evolving situation calls for a stronger public health systems in the country. Message is loud and clear that a more resilient and responsive health system can help ensure early detection and prompt reporting of cases. A strong health system will be able to detect an unusual occurrence quickly.
In the final analysis, it is clear that investing in robust surveillance, laboratory testing, a comprehensive communication strategy in consonance with the IHR (2005), and a strong public health system could help save lives and avert grave socio-economic disruption that may likely be caused by this virus or those that may strike in the future. The threat is real and the time for action is now.
Footnotes
Conflicts of Interest: None.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–3. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China] Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145–51. [Google Scholar]
- 4.World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) WHO; 2020. [accessed on March 20, 2020]. Available from: https://wwwwhoint/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus- (2019-ncov) [Google Scholar]
- 5.World Health Organization. COVID-19 can be characterized as pandemic. WHO; 2020. [accessed on March 20, 2020]. Available from: https://wwwwhoint/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 . [Google Scholar]
- 6.Heymann DL, Shindo N WHO Scientific and Technical Advisory Group for Infectious Hazards. COVID-19: What is next for public health? Lancet. 2020;395:542–5. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paules CI, Marston HD, Fauci AS. Coronavirus infections - More than just the common cold. JAMA. 2020 doi: 10.1001/jama.2020.0757. doi:101001/jama20200757. [DOI] [PubMed] [Google Scholar]
- 8.de Wit E, van Doremalen N, Falzarano D, Munster VJ. MERS: Recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14:523–34. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;95:565–74. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report - 62. WHO; 2020. [accessed on March 22, 2020]. Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200322-sitrep-62-covid-19pdfsfvrsn=f7764c46_2 . [Google Scholar]
- 11.Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) [accessed on March 20, 2020]. Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200228-sitrep-39-covid-19pdfsfvrsn=aa1b80a7_4 .
- 12.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report - 42. WHO; 2020. [accessed on March 3, 2020]. Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200228-sitrep-39-covid-19pdfsfvrsn=aa1b80a7_4 . [Google Scholar]
- 13.World Health Organization - Regional Office for Africa. More than 600 Confirmed Cases of COVID-19 in Africa WHO Africa. 2020. [accessed on March 23, 2020]. Available from: https://wwwafrowhoint/news/more-600-confirmed-cases-covid-19-africa .
- 14.Press Information Bureau, Government of India, Ministry of Information & Broadcasting. Cabinet Secretary on “Novel Coronavirus” Outbreak. [accessed on March 3, 2020]. Available from: https://pib.gov.in/newsite/PrintRelease.aspx?relid=197678 .
- 15.Press Information Bureau, Government of India, Ministry of Health & Family Welfare. Health Secretary reviewed the Novel Coronavirus Disease Situation. [accessed on March 3, 2020]. Available from: https://pib.gov.in/newsite/PrintRelease.aspx?relid=199163 .
- 16.National Centre for Disease Control. COVID-19 New Delhi: Ministry of Health & Family Welfare, Government of India. 2020. [accessed on March 31, 2020]. Available from: https://ncdcgovin/index4phplang=1&level=0&linkid=127&lid=432 .
- 17.Indian Council of Medical Research. Note on COVID-19 Laboratory Preparedness in India. [accessed on March 24, 2020]. Available at: https://icmrnicin/sites/default/files/press_realease_files/ICMR_PressRelease_COVID_19pdf .
- 18.Press Information Bureau, Government of India, Ministry of Health & Family Welfare. Measures to Control Spread of Novel Coronavirus. [accessed on March 3, 2020]. Available from: https://pib.gov.in/newsite/PrintRelease.aspx?relid=199265 .
- 19.National Centre for Disease Control. Compendium of India Epidemic Intelligence Service (EIS) Programme. New Delhi: Ministry of Health & Family Welfare, Government of India; 2020. [accessed on March 3, 2020]. Available from: https://ncdcgovin/showfilephplid=406 . [Google Scholar]
- 20.Heymann DL, Rodier G. SARS: Lessons from a new disease. US: National Academies Press; 2004. [accessed on February 29, 2020]. Available from: https://wwwncbinlmnihgov/books/NBK92444/ [Google Scholar]
- 21.World Health Organization. International Health Regulations (2005) 2nd ed. WHO; 2008. [accessed on February 29, 2020]. Available from: http://wwwwhoint/ihr/publications/9789241596664/en/ [Google Scholar]
- 22.World Health Organization. International Health Regulations (2005) 3rd ed. WHO; 2016. [accessed on March 3, 2020]. Available from: https://wwwwhoint/ihr/publications/9789241580496/en/ [Google Scholar]
- 23.Narain JP. Infectious, but not so deadly. [accessed on March 4, 2020]. Available from: https://wwwtribuneindiacom/news/infectious-but-not-so-deadly-33563 .
- 24.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report - 46. WHO; 2020. [accessed on March 10, 2020]. Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200306-sitrep-46-covid-19pdfsfvrsn=96b04adf_2 . [Google Scholar]
- 25.World Health Organization. Infection Prevention and Control (IPC) for Novel Coronavirus (COVID-19) WHO; 2020. [accessed on March 3, 2020]. Available from: https://openwhoorg/courses/COVID-19-IPC-EN . [Google Scholar]