Abstract
This study aims to develop and assess the psychometric properties of a measure of moral injury (MI) symptoms for identifying clinically significant MI in health professionals (HPs), one that might be useful in the current COVID-19 pandemic and beyond. A total of 181 HPs (71% physicians) were recruited from Duke University Health Systems in Durham, North Carolina. Internal reliability of the Moral Injury Symptom Scale-Healthcare Professionals version (MISS-HP) was examined, along with factor analytic, discriminant, and convergent validity. A cutoff score was identified from a receiver operator curve (ROC) that best identified individuals with significant impairment in social or occupational functioning. The 10-item MISS-HP measures 10 theoretically grounded dimensions of MI assessing betrayal, guilt, shame, moral concerns, religious struggle, loss of religious/spiritual faith, loss of meaning/purpose, difficulty forgiving, loss of trust, and self-condemnation (score range 10–100). Internal reliability of the MISS-HP was 0.75. PCA identified three factors, which was confirmed by CFA, explaining 56.8% of the variance. Discriminant validity was demonstrated by modest correlations (r’s = 0.25–0.37) with low religiosity, depression, and anxiety symptoms, whereas convergent validity was evident by strong correlations with clinician burnout (r = 0.57) and with another multi-item measure of MI symptoms (r = 0.65). ROC characteristics indicated that a score of 36 or higher was 84% sensitive and 93% specific for identifying MI symptoms causing moderate to extreme problems with family, social, and occupational functioning. The MISS-HP is a reliable and valid measure of moral injury symptoms in health professionals that can be used in clinical practice to screen for MI and monitor response to treatment, as well as when conducting research that evaluates interventions to treat MI in HPs.
Keywords: Moral injury, Internal conflict, Health professionals, Burnout, Depression, Religiosity
Background
Over the past 10 years, moral injury (MI) has been increasingly recognized as a common syndrome seen among veterans and active duty military experiencing trauma symptoms from war (Koenig et al. 2019a). MI has been described as “a deep sense of transgression including feelings of shame, grief, meaninglessness, and remorse from having violated core moral beliefs” (Brock and Lettini 2012) and also, as “a betrayal of what’s right, by someone who holds legitimate authority, in a ‘high-stakes situation’” (Shay 1994, 2014). In addition to the psychological symptoms above, MI includes symptoms of struggle with religious faith (and even loss of faith), given that moral values have their roots in religious teachings. The inner conflict that psychological and religious symptoms of MI create may have a significant effect on family, social, and occupational functioning.
Although much progress has been made in identifying and treating MI among current and former military personnel (Koenig et al. 2019b), there remains a large gap in what is known about the occurrence of MI among physicians, nurses, and other HCPs who must often work long hours in “high-stakes situations,” often experiencing exhaustion from the pressures that the healthcare systems place on them. This has become particularly evident during the recent COVID-19 pandemic when the influx of patients into hospitals has been so great that not all can be cared for, forcing HCPs to make decisions about allocation of ventilatory support and other critical resources (White and Lo 2020). Even before the COVID-19 pandemic, however, burnout among HCPs had already become epidemic (Reith 2018), driven in part by growing administrative responsibilities and limitations and increased pressure to see more patients (Sibeoni et al. 2019), often leaving little energy to care for the physical and often emotional needs of those for whom they were responsible (Gonçalves et al. 2019). The increasing suicide rate among physicians testifies to the seriousness of this situation (Duarte et al. 2020). As a result, experts in this field have begun to wonder whether undiagnosed moral injuries among HCPs may underlie burnout and other emotional conditions so often reported by those on the front lines of clinical care (Kopacz et al. 2019).
One factor that has slowed both the identification and treatment of MI among HCPs has been the lack of a reliable and valid measure of MI in this population. However, there already exists such a measure for identifying MI symptoms in veterans and active duty military, both a long version (45-item Moral Injury Symptom Scale-Military version [MISS-M-LF]; Koenig et al., 2018a) and a short version (10-item MISS-M-SF) for clinical and research purposes (Koenig et al. 2018b). The present study seeks to provide a reliable and valid measure for identifying MI among HCPs for use in healthcare settings. This has been done by modifying the language used in the 10-item MISS-M-SF so that it applies specifically to HCPs (Koenig et al. 2020a). Here, we report the psychometric properties of this new measure (the 10-item MISS-HP) for use by healthcare providers and clinical researchers to identify this syndrome and monitor response to treatment.
Objective
The goals of this study were to (1) determine the reliability and validity of the MISS-HP among physicians, nurses, and other health professionals and (2) determine a cutoff score on the MISS-HP for identifying symptoms that cause problems in family, social, and occupational functioning, one that can be used to identify HPs at high risk for clinically significant MI.
Methods
Sample recruitment, data collection, and measurement procedures have been described in detail elsewhere (Mantri et al. 2020). In brief, a cross-sectional study was conducted among health professionals at Duke University Health Systems in Durham, North Carolina. Participants were asked to complete an online survey using the Qualtrics software platform (https://www.qualtrics.com/lp/survey-platform-2/). Participants completed the survey between November 13, 2019, and March 12, 2020, just prior to the recent COVID-19 pandemic. An e-mail was sent out to Duke Health System departments requesting them to send a link to the survey to healthcare professionals in their department, particularly directed at physicians and nurses. Those who completed the anonymous survey were offered the opportunity to include their name (coded) in a raffle for a $1000 grand prize. Informed consent was provided at the beginning of the survey by a page that described the study, its purposes, and the confidential nature of responses. Participants were required to mark a box titled “I consent, begin the study” before they could start the survey. This study was approved by the institutional review boards (IRB) of Duke University Health Systems (Pro00104047).
Questionnaire
Sociodemographic
The survey began by asking participants their age, gender, race, and marital status.
Moral Injury
The original 10-item MISS-M-SF assesses 10 theoretically grounded dimensions of MI based on the writings and research of MI experts (Litz et al. 2009; Shay 1994; Shay 2014; Drescher et al. 2011; Brock and Lettini 2012; Nash et al. 2013; Currier et al. 2015). The 10 dimensions of MI assessed by this measure are betrayal, guilt, shame, moral concerns, loss of trust, loss of meaning, difficulty forgiving, self-condemnation, religious struggle and loss of religious faith. To our knowledge, this is the only measure of MI that assesses both psychological and religious symptoms (Koenig et al. 2019a). The MISS-M-SF has strong internal reliability, test–retest reliability, and criterion, discriminant, and convergent validity in military personnel suffering from PTSD symptoms (Koenig et al. 2018b). For the current study, we adapted the language of each item on the MISS-M-SF so that it would apply to health professionals caring for patients in medical settings, calling it the Moral Injury Symptom Scale-Health Professional version (MISS-HP) (Koenig et al. 2020). Each of the 10 items of the MISS-HP has response options on a visual analogue scale ranging from 1 (“strongly disagree”) to 10 (“strongly disagree). Four of the items are worded positively and six negatively in order to reduce response bias (Furnham 1986). After recoding the positively worded items (5, 6, 7, 10), item scores are summed to create a total score ranging from 10 to 100, with higher scores indicating greater MI.
In order to determine convergent validity for the MISS-HP, the 17-item Expressions of Moral Injury Scale (EMIS-M) was utilized (Currier et al. 2018). This scale was originally developed to assess symptoms of MI in former or current military personnel. For the purposes of this study, the wording of items on the EMIS-M was modified by Currier so that the statements would apply specifically to healthcare professionals (EMIS-HP). Each of the 17 items is rated on a Likert scale from 1 (strongly disagree) to 5 (strongly agree) with all items worded in the same direction. Higher total scores indicate the number and severity of MI symptoms, reflecting maladaptive behaviors and internal experiences associated with the moral challenges involved in delivering clinical care. The EMIS-HP includes only the psychological symptoms of MI. The internal reliability α of the EMIS-HP in the current sample was 0.93.
Clinical Characteristics
Participants were asked about their profession (physician, nurse, other), specialty (family medicine, internal medicine, pediatrics, surgery, psychiatry, neurology, other), work area (outpatient medicine, inpatient medicine, ICU/CCU, emergency room, other), and how long (years) they had been in practice.
Religion and Religiosity
Participants’ religious affiliation was assessed by asking if they were Christian, Jewish, Hindu, Muslim, Buddhist, had some other religious affiliation, no religious affiliation, or considered themselves atheist or agnostic. Level of religious commitment was measured by the 10-item Belief into Action (BIAC) scale (Koenig et al. 2014, 2015). Items on the scale are each rated from 1 to 10 on a visual analogue scale. When all 10 items are summed, this results in a score ranging from 10 to 100, with higher scores indicating greater religious involvement and commitment. The BIAC has solid psychometric characteristics (Koenig et al. 2014; Wang et al. 2016). The internal reliability alpha in the present sample was 0.93.
Depression
The Patient Health Questionnaire-9 (PHQ-9) was used to assess depressive symptoms (Kroenke et al. 2001; Spitzer et al. 1999). The PHQ-9 has been used widely in a range of populations, including HCPs (Verma 2019), and the measure has well-established psychometric properties (Beard et al. 2016; Manea et al. 2015). The internal reliability alpha of the PHQ-9 in the present study was 0.86.
Anxiety
The 7-item Generalized Anxiety Disorder (GAD-7) scale was used to assess anxiety symptoms (Spitzer et al. 2006; Swinson 2006). The GAD-7 is a sensitive and specific measure of anxiety symptoms (Kroenke et al. 2007). The internal reliability alpha of the GAD-7 in the present sample was 0.90.
Burnout
Symptoms of clinician burnout were assessed by the 22-item Maslach Burnout Inventory (MBI) (Maslach et al. 1996). Individual items on the MBI are rated on a 1–7 scale from “never” to “every day” with positively worded items reverse scored, resulting in a total score ranging from 22 to 154. For almost 40 years, the MBI has been the standard measure for assessing burnout symptoms in HPs around the world (Iwanicki and Schwab 1981; Maslach et al. 1986; Dewa et al. 2017). The internal reliability alpha of the MBI in the current study was 0.89.
Missing Values
When computing scale scores for the MISS-HP, PHQ-9, GAD-7, MBI, and EMIS-HP, missing values were handled as follows. The mean substitution method was used as described by Downey and King (1998). If respondents completed at least half of the items on a scale, the average of all items responded to was substituted for missing items on the scale. If fewer than half of the items on a scale were missing, the scale score was designated as missing.
Statistical Analyses
Sample characteristics are described in Table 1 with means (standard deviations) for continuous variables and % (n) for categorical variables.
Table 1.
Sample characteristics
| Characteristic | % (n) | Mean (SD) (n) | |
|---|---|---|---|
| Sociodemographic | |||
| Age, years | 45–65+ | 59.8 (107) | |
| 25–44 | 41.2 (72) | ||
| Gender (male) | 63.5 (113) | ||
| Race | Black/African-American | 5.0 (9) | |
| White Caucasian | 75.4 (135) | ||
| Other | 19.6 (35) | ||
| Marital status | Married | 79.3 (179) | |
| Clinical attributes | |||
| Profession | Physician | 70.7 (128) | |
| Nurse | 9.4 (17) | ||
| Other | 19.9 (36) | ||
| Specialty | Family medicine | 8.4 (15) | |
| Internal medicine | 20.1 (36) | ||
| Pediatric medicine | 22.9 (41) | ||
| Surgery (including Ob-Gyn) | 7.8 (14) | ||
| Psychiatry | 22.9 (41) | ||
| Neurology | 11.7 (21) | ||
| Other | 7.2 (13) | ||
| Work area | Outpatient medicine | 42.4 (75) | |
| Inpatient medicine | 45.2 (80) | ||
| ICU/CCU/CCU/other | 12.5 (22) | ||
| Length of practice (years) | 11.2 (11.0) | ||
| Religious | |||
| Denomination | Christian | 54.2 (97) | |
| Jewish | 6.7 (12) | ||
| Hindu | 5.0 (9) | ||
| Muslim | 3.9 (7) | ||
| Buddhist | 1.1 (2) | ||
| None/agnostic/atheist | 29.0 (45) | ||
| Other | 2.2 (4) | ||
| Religious commitment (BIAC) | 27.5 (18.8) | ||
| Depression and anxiety | |||
| Depression (PHQ-9) | 13.7 (4.5) | ||
| Anxiety (GAD-7) | 11.8 (4.6) | ||
| Burnout | |||
| Burnout (MBI) | 68.7 (19.8) | ||
| Moral injury | |||
| MISS-HP | 36.8 (13.3) | ||
| EMIS-HP | 34.2 (13.2) |
BIAC 10-item Belief into Action Scale; PHQ-9 9-item Patient Health Questionnaire; GAD-7 7-item Generalized Anxiety Disorder Scale; MBI 22-item Maslach Burnout Inventory; MISS-HP 10-item Moral Injury Symptom Scale-Healthcare Professional version; EMIS-HP 17-item Expressions of Moral Injury Scale Health Professional version
Reliability
Internal consistency of the MISS-HP was calculated using Cronbach’s alpha (α) for those without missing items and for those with missing items requiring item substitution. An α of 0.70 or higher is considered acceptable (Cronbach 1951).
Factor Analytic Validity
Exploratory factor analysis (EFA) using principle components factor analysis (PCA) with Promax rotation was conducted on the MISS-HF items using the Kaiser–Guttman rule that states the number of factors to be extracted should be equal to the number of factors having an eigenvalue of greater than 1.0 (Kaiser 1991). First, the overall sample (n = 181) was randomly split into two groups using PROC SURVEYSELECT in SAS. In the first group (n = 90), EFA was conducted to identify the number of factors (Table 2). Confirmatory factor analysis (CFA) was then performed in the second half of the sample (n = 91) to determine the extent to which results from the EFA could be confirmed in a different sample. Finally, the PCA with Promax rotation was conducted using the entire sample (n = 181) (Table 3).
Table 2.
Exploratory factor analysis with factor loadings for the MISS-HP (n = 90; first half of sample)
| MISS-HP items | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|
| MISS1 (betrayal) | .093 | .654 | .174 |
| MISS2 (guilt) | .742 | .499 | .461 |
| MISS3 (shame) | .628 | .722 | .408 |
| MISS4 (moral concerns) | .465 | .722 | .284 |
| MISS5 (loss of trust) (R) | .102 | .256 | .603 |
| MISS6 (loss of meaning) (R) | .427 | − .169 | .749 |
| MISS7 (unforgiveness) (R) | .406 | .399 | .487 |
| MISS8 (self-condemnation) | .708 | .309 | .281 |
| MISS9 (feeling punished by God) | .690 | .070 | .054 |
| MISS10 (loss of religious faith) (R) | .144 | .339 | .633 |
| Initial eigenvalues | 3.19 | 1.64 | 1.11 |
| Kaiser–Meyer–Olkin (KMO) = 0.771 | |||
| Bartlett’s Test of Sphericity = χ2 = 175.7, p < 0.001 |
MISS-HP = 10-item Moral Injury Symptom Scale-Healthcare Professional version
(R) = reverse scored due to positive wording
Bold factor loadings indicate factor assigned to
Table 3.
Final principle components analysis with factor loadings for the MISS-HP (n = 181)
| MISS-HP Items | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|
| MISS1 (betrayal) | .648 | .140 | .027 |
| MISS2 (guilt) | .708 | .342 | .384 |
| MISS3 (shame) | .779 | .331 | .454 |
| MISS4 (moral concerns) | .732 | .161 | .442 |
| MISS5 (loss of trust) (R) | 243 | .639 | − .029 |
| MISS6 (loss of meaning) (R) | .043 | .774 | .263 |
| MISS7 (unforgiveness) (R) | .377 | .681 | .411 |
| MISS8 (Self-condemnation) | .394 | .353 | .684 |
| MISS9 (Feeling punished by God) | .266 | .080 | .751 |
| MISS10 (loss of religious faith) (R) | .446 | .554 | − .290 |
| Initial eigenvalues | 3.24 | 1.39 | 1.05 |
| Kaiser–Meyer–Olkin (KMO) = 0.786 | |||
| Bartlett’s Test of Sphericity = χ2 = 369.3, df = 45, p < 0.001 |
MISS-HP = 10-item Moral Injury Symptom Scale-Healthcare Professional version
(R) = reverse scored due to positive wording
Bold factor loadings indicate factor assigned to
Discriminant Validity
In order to ensure that the MISS-HP is measuring a construct that is different from measures of existing constructs, associations between the MISS-HP total score and established measures of religiosity, depressive symptoms, and anxiety symptoms were examined using Pearson correlation.
Convergent Validity
In order to determine whether the MISS-HP is correlated with another measure of the construct of MI, the association between the MISS-HP and the EMIS-HP was examined using Pearson correlation. Given similarities between MI and burnout in HPs (Kopacz et al. 2019), the association between the MISS-HP and the MBI was also examined as an indicator of convergent validity.
Cutoff Determination
Immediately following completion of the MISS-HP, participants were asked: “Do the feelings you indicated above cause you significant distress or impair your ability to function in relationships, at work, or other areas of life important to you? In other words, if you indicated any problems above, how difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?” Response options included “not at all,” “mild,” “moderate,” “very much,” and “extremely.” Symptoms causing functional disability were categorized as either causing (1) none or only mild disability (not clinically significant) or (2) moderate, very much, or extreme disability (clinically significant). In DSM-5, impairment of social or occupational functioning is necessary in order to describe a condition as a “disorder” needing clinical attention (American Psychiatric Association 2013).
In order to determine the best cutoff on the MISS-HP that could be used to identify HPs with clinically significant MI symptoms, receiver operator curve (ROC) analysis was performed. The cutoff on the MISS-HP was determined based on the total score that was most sensitive and specific for identifying clinically significant functional disability (as above). The positive predictive value and negative predictive value for the cutoff score were also determined.
Level of statistical significance in all analyses was set at α = 0.05. SAS (version 9.3; SAS Institute Inc., Cary, North Carolina) was used for all analyses except for conducting the PCA and the ROC analysis, for which IBM SPSS Statistics, version 26, was used.
Results
A total of 272 healthcare professionals began the survey, although only 181 completed at least 50% of the items on the MISS-HP, which comprised the sample for this report. No significant difference on sociodemographic or clinical characteristics was present between the 181 participants who completed the MISS-HP and the 91 non-completers with regard to age, gender, race, marital status, profession, or work area; however, non-completers were more likely to indicate neurology as their specialty (37.0% vs. 11.7%, p < 0.001). In addition, those indicating “none” for religious affiliation were also more likely to not complete the MISS-HP (53.2% vs. 25.1%) (p < 0.01). Table 1 describes the characteristics of all 181 participants included in this analysis.
Reliability Internal consistency of the MISS-HP (Cronbach’s alpha) was 0.73 for those without missing items and 0.75 for those with missing items imputed, both above the minimal acceptable threshold of 0.70 for internal reliability (Cronbach 1951).
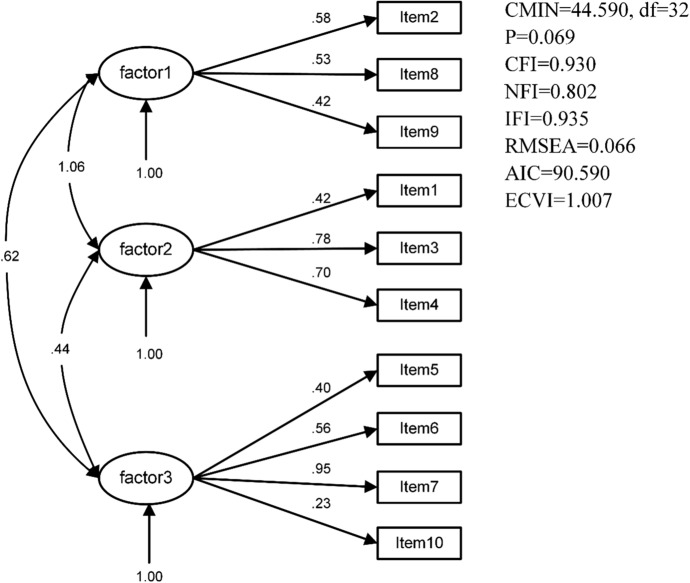
Factor Analytic Validity Exploratory factor analysis (EFA) with Promax rotation in the first half of the sample yielded three factors: Factor 1 (MISS2, MISS8, MISS9), Factor 2 (MISS1, MISS3, MISS4), and Factor 3 (MISS5, MISS6, MISS7, MISS10), which explained 54.7% of the variance (Table 2). Confirmatory factor analysis (CFA) verified the three-factor model for the MISS-HP in the second half of the sample (χ2 = 44.59, df = 32, p = 0.069, CFI = 0.93, NFI = 0.80, RMSEA = 0.07, IFI = 0.94, AIC = 90.59, ECVI = 1.01) (Fig. 1). The final PCA in the overall sample (n = 181) identified three factors: Factor 1 (MISS1, MISS2, MISS3, and MISS4, with the strongest loadings for guilt, shame, betrayal, and moral concerns, titled the Guilt/Shame factor), Factor 2 (MISS5, MISS6, MISS7, and MISS10, having to do with loss of trust, loss of meaning, being unable to forgive, and loss of faith, titled the Spiritual Troubles factor), and Factor 3 (MISS8 and MISS 9, with a focus on self-condemnation and punishment by God, titled the Condemnation factor), explaining 56.8% of the variance (Table 3). Note that all items composing the Spiritual factor involved positively worded items (signifying higher MI with lower scores) in contrast to items on the remaining factors that were negatively worded (signifying higher MI with higher scores).
Fig. 1.
Confirmatory factor analysis for MISS-HP in second half of sample (n = 91)
Discriminant Validity Discriminant validity was demonstrated by small to moderate correlations between the MISS-HP total score and religiosity (r = − 0.25), depressive symptoms (r = 0.35), and anxiety symptoms (r = 0.37). All associations, however, were in the expected direction.
Convergent Validity Convergent validity was demonstrated by strong correlations between the MISS-HP and both the EMIS-HP (r = 0.65) and the MBI (r = 0.57).
Cutoff Determination The ROC is displayed in Fig. 2. Area under the curve was 0.777 (asymptotic 95% CI = 0.701–0.852), standard error 0.38 (under the nonparametric assumption), and the asymptotic was significant at ≤ 0.001 (under the null hypothesis that true area = 0.5). Based on the Youden’s index from the ROC, the optimum cutoff score on the MISS-HP for identifying HPs with clinically significant MI symptoms was 36 or higher (indicating a positive test). With a 36 or higher cutoff score on the MISS-HP, the sensitivity for detecting MI symptoms associated with significant functional impairment was 84% (of the 43 impaired participants, 36 had a positive test). The specificity, in turn, was 93% (of the 94 with a negative test, 87 were not impaired). The positive predictive value (PPV) was 42% (of the 86 with a positive test, 36 were impaired), and negative predictive value was 64% (of the 137 without impairment, 87 had a negative test).
Fig. 2.
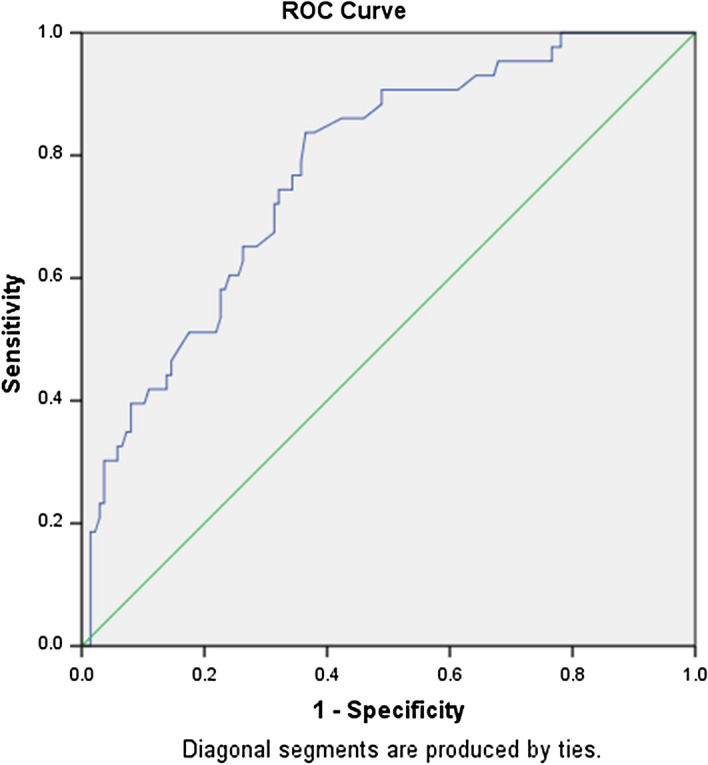
Receiver operator curve (ROC) for the MISS-HP
Discussion
The purpose of the present study was to identify the psychometric characteristics of the MISS-HP and identify the best cutoff score on the MISS-HP likely to identify those with significant functional impairment (defined as moderate, very or extreme impairment of family, social, or occupational functioning). The results from this study of 181 health professionals (more than 70% physicians) at an academic medical center in the southeastern US indicated that the MISS-HP is a reliable and valid measure for assessing moral injury in healthcare professionals. A cutoff score of 36 or higher (on a possible score range of 10 to 100) was the MISS-HP score that maximized sensitivity and specificity for identifying significant functional impairment warranting further clinical assessment and treatment of MI symptoms.
In another publication from this study, we found that MI symptoms assessed by the MISS-HP were positively associated with HPs making medical errors in the previous month, which suggests that MI may be the cause or the consequence of such clinical mishaps (Mantri et al. 2020). MI was also strongly associated with clinician burnout as assessed by the Maslach Burnout Inventory, independent of sociodemographic factors, clinical attributes, and religious characteristics (Mantri et al. 2020). MI has been shown to increase risk of suicide among military personnel (Bryan C. et al. 2013; Bryan A. et al. 2014; Ames et al. 2019). Suicidal thought are also higher among HPs with high MI, and the total MISS-HP score in the present study was positively correlated with suicidal thoughts (question 9 on the PHQ-9: “Thought that you would be better off dead or of hurting yourself in some way”) (r = 0.19, p = 0.01). Thus, MI is not a benign syndrome, even though it is commonly underrecognized given the absence of measures to identify it (up until now).
The MISS-HP was recently examined in over 3000 health professionals in mainland China during the COVID-19 pandemic between March 27 to April 26, 2020 (Wang et al. 2020). The prevalence of clinically significant MI (causing very much or extreme impairment of social and occupational functioning) at that time was 20.4% (compared to 7.8% in the current study; Mantri et al. 2020). The Cronbach’s alpha (α) of the MISS-HP in the Chinese study was 0.70 (compared to α = 0.75 in the present study) and intraclass correlation coefficient (ICC) for two-week test–retest reliability in 100 physicians was 0.77. A three-factor model was also identified in that study explaining 58.4% of the variance (compared to the final model in the present study explaining 56.8%). The MISS-HP items loaded slightly differently in the Chinese study with Factor 1 (MISS2, MISS3, and MISS4) similar to our Guilt/Shame factor, Factor 2 (MISS1, MISS7 MISS8, and MISS9) similar to our Condemnation factor, and Factor 3 (MISS5, MISS6, and MISS10) similar to our Spiritual factor. These small differences in item factor loading likely resulted from the translation of the measure into Chinese and/or cultural differences in the interpretation of these items.
Limitations
The findings from the present study are limited in several respects that may impact their generalizability and interpretation. First, this was a convenience sample of HPs from a single academic healthcare system in the southeastern USA, necessitating caution when generalizing results to HPs in other healthcare systems located in different locations. Second, most of the sample was physicians (over 70%), requiring some caution when generalizing the findings to nurses and other health professionals. Third, the sample size was relatively small for factor analysis, particularly after splitting the sample in half, increasing the likelihood of unstable estimates. Lastly, non-completers of our survey were more likely to be neurologists or to indicate no religious affiliation, raising the possibility of response bias in the present sample.
However, there were also a number of strengths to the study that need to be emphasized. First, to our knowledge, this is the first study to report on the psychometric properties of a measure to assess MI in health professionals in the USA, particularly one that assesses both the psychological and religious/spiritual symptoms of MI. Second, the psychometric properties of the MISS-HP were quite acceptable, including the internal reliability (α = 0.75), the discriminant validity (distinguishing it from psychometrically valid and widely used multi-item measures of religiosity, anxiety, and depression), and the convergent validity (strong correlations with another well-established measure of MI, the 17-item EMIS, as well as with clinician burnout assessed by the gold standard MBI, a concept quite similar to MI). Furthermore, the three factors identified in the overall sample were quite similar to those reported in the Chinese study cited above of over 3000 HPs (Wang et al. 2020). Finally, having a psychometrically valid measure for identifying MI during the current COVID-19 pandemic, future pandemics, and other war/disaster-related situations that place pressure on HPs working in stressed healthcare systems underscores the importance and timeliness of this report.
Conclusions
The MISS-HP is a reliable and valid scale for assessing symptoms of moral injury in healthcare professionals. This measure may be used in clinical settings to identify significant levels of MI causing impairment in social or occupational functioning that require clinical attention and can also be used to monitor response to treatment. Both psychological and spiritual interventions for MI in veterans and active duty military do exist (Harris et al. 2011; Paul et al. 2014; Litz et al. 2017; Harris et al. 2018; Pearce et al. 2018) and could easily be adapted for treating MI in healthcare professionals as well. In research settings, the MISS-HP may also be used when testing interventions for MI like those above, both for identifying potential participants and for determining response to treatment. Future studies are needed to examine the psychometric properties of the MISS-HP in different populations of health professionals working in different settings and under different conditions.
Appendix
Moral Injury Symptom Scale: Healthcare Professionals Version (MISS-HF)
The following questions may be difficult, but they are common experiences of busy healthcare professionals. They concern your experiences on your job as a health professional and how you are feeling now. Try to answer every question. Circle a single number between 1 (strongly disagree) and 10 (strongly agree) to indicate how much you personally agree or disagree with each statement.
- I feel betrayed by other health professionals whom I once trusted.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - I feel guilt over failing to save someone from being seriously injured or dying.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - I feel ashamed about what I’ve done or not done when providing care to my patients.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - I am troubled by having acted in ways that violated my own morals or values.
2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - Most people with whom I work as a health professional are trustworthy.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - I have a good sense of what makes my life meaningful as a health professional.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - I have forgiven myself for what’s happened to me or to others whom I have cared for.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - All in all, I am inclined to feel that I’m a failure in my work as a health professional.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - I sometimes feel God is punishing me for what I’ve done or not done while caring for patients.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - Compared to before I went through these experiences, my religious/spiritual faith has strengthened.
1 2 3 4 5 6 7 8 9 10 Strongly disagree Mildly disagree Neutral Mildly agree Strongly agree - Do the feelings you indicated above cause you significant distress or impair your ability to function in relationships, at work, or other areas of life important to you? In other words, if you indicated any problems above, how difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?
□ Not at all □ Mild □ Moderate □ Very much □ Extremely
Compliance with Ethical Standards
Conflict of interest
The author has no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sneha Mantri, Email: sneha.mantri@duke.edu.
Jennifer Mah Lawson, Email: jennifer.lawson@duke.edu.
ZhiZhong Wang, Email: wzhzh_lion@126.com.
Harold G. Koenig, Email: Harold.Koenig@duke.edu
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM-5®) Washington DC: American Psychiatric Publishing; 2013. [Google Scholar]
- Ames D, Erickson Z, Youssef NA, Arnold I, Adamson CS, Sones AC, et al. Moral injury, religiosity, and suicide risk in US veterans and active duty military with PTSD symptoms. Military Medicine. 2019;184(3–4):e271–e278. doi: 10.1093/milmed/usy148. [DOI] [PubMed] [Google Scholar]
- Beard C, Hsu KJ, Rifkin LS, Busch AB, Björgvinsson T. Validation of the PHQ-9 in a psychiatric sample. Journal of Affective Disorders. 2016;193:267–273. doi: 10.1016/j.jad.2015.12.075. [DOI] [PubMed] [Google Scholar]
- Brock RN, Lettini G. Soul repair: Recovering from moral injury after war. Boston, MA: Beacon Press; 2012. [Google Scholar]
- Bryan AO, Bryan CJ, Morrow CE, Etienne N, Ray-Sannerud B. Moral injury, suicidal ideation, and suicide attempts in a military sample. Traumatology. 2014;20(3):154. doi: 10.1037/h0099852. [DOI] [Google Scholar]
- Bryan CJ, Morrow CE, Etienne N, Ray-Sannerud B. Guilt, shame, and suicidal ideation in a military outpatient clinical sample. Depression and Anxiety. 2013;30(1):55–60. doi: 10.1002/da.22002. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. doi: 10.1007/BF02310555. [DOI] [Google Scholar]
- Currier JM, Farnsworth JK, Drescher KD, McDermott RC, Sims BM, Albright DL. Development and evaluation of the expressions of moral injury scale—Military version. Clinical Psychology & Psychotherapy. 2018;25(3):474–488. doi: 10.1002/cpp.2170. [DOI] [PubMed] [Google Scholar]
- Currier JM, Holland JM, Drescher K, Foy D. Initial psychometric evaluation of the moral injury questionnaire—Military Version. Clinical Psychology & Psychotherapy. 2015;22:54–63. doi: 10.1002/cpp.1866. [DOI] [PubMed] [Google Scholar]
- Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. British Medical Journal Open. 2017;7(6):e015141. doi: 10.1136/bmjopen-2016-015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey RG, King CV. Missing data in likert ratings: A comparison of replacement methods. Journal of General Psychology. 1998;125(2):175–191. doi: 10.1080/00221309809595542. [DOI] [PubMed] [Google Scholar]
- Drescher KD, Foy DW, Kelly C, Leshner A, Schutz K, Litz B. An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology. 2011;17:8–13. doi: 10.1177/1534765610395615. [DOI] [Google Scholar]
- Duarte D, El-Hagrassy MM, e Couto TC, Gurgel W, Fregni F, Correa H. Male and female physician suicidality: A systematic review and meta-analysis. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furnham A. Response bias, social desirability and dissimulation. Personality and Individual Differences. 1986;7(3):385–400. doi: 10.1016/0191-8869(86)90014-0. [DOI] [Google Scholar]
- Gonçalves A, Fontes L, Simães C, Gomes AR. Stress and burnout in health professionals. In: Arezes PM, editor. Occupational and Environmental Safety and Health. Cham: Springer; 2019. pp. 563–571. [Google Scholar]
- Harris JI, Erbes CR, Engdahl BE, Thuras P, Murray-Swank N, Grace D, Ogden H, Olson RH, Winskowski AM, Bacon R, Malec C, Campion K, Le T. The effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma. Journal of Clinical Psychology. 2011;67(4):425–438. doi: 10.1002/jclp.20777. [DOI] [PubMed] [Google Scholar]
- Harris I, Usset T, Voeck C, Thuras P, Currier J, Erbes C. Spiritually integrated care for PTSD: A randomized controlled trial of “Building Spiritual Strength”. Psychiatry Research. 2018;267:420–428. doi: 10.1016/j.psychres.2018.06.045. [DOI] [PubMed] [Google Scholar]
- Iwanicki EF, Schwab RL. A cross validation study of the Maslach Burnout Inventory. Educational and Psychological Measurement. 1981;41(4):1167–1174. doi: 10.1177/001316448104100425. [DOI] [Google Scholar]
- Kaiser HF. Coefficient alpha for a principal component and the Kaiser-Guttman rule. Psychological Reports. 1991;68:855–858. doi: 10.2466/pr0.1991.68.3.855. [DOI] [Google Scholar]
- Koenig HG, Ames D, Büssing A. Screening for and treatment of moral injury in veterans/active duty military with PTSD. Frontiers in Psychiatry. 2019;10:596. doi: 10.3389/fpsyt.2019.00596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG, Ames D, Youssef N, Oliver JP, Volk F, Teng EJ, et al. The moral injury symptom scale—Military version. Journal of Religion and Health. 2018;57:249–265. doi: 10.1007/s10943-017-0531-9. [DOI] [PubMed] [Google Scholar]
- Koenig HG, Ames D, Youssef N, Oliver JP, Volk F, Teng EJ, et al. Screening for moral injury—The moral injury symptom scale-military version short form. Military Medicine. 2018;183(11–12):e659–e665. doi: 10.1093/milmed/usy017. [DOI] [PubMed] [Google Scholar]
- Koenig HG, Mantri S, Lawson J. Moral injury symptoms scale—Health professionals version (MISS-HP) Durham, NC: Duke University Center for Spirituality, Theology and Health; 2020. [Google Scholar]
- Koenig HG, Nelson B, Shaw SF, Al Zaben F, Wang Z, Saxena S. Belief into Action scale: A brief but comprehensive measure of religious commitment. Open Journal of Psychiatry. 2014;5(01):66. doi: 10.4236/ojpsych.2015.51010. [DOI] [Google Scholar]
- Koenig HG, Wang Z, Al Zaben F, Adi A. Belief into Action Scale: A comprehensive and sensitive measure of religious involvement. Religions. 2015;6(3):1006–1016. doi: 10.3390/rel6031006. [DOI] [Google Scholar]
- Koenig HG, Youssef NA, Ames D. Assessment of moral injury in veterans and active duty military with PTSD: A review. Frontiers in Psychiatry. 2019;10(443):1–15. doi: 10.3389/fpsyt.2019.00443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopacz M, Ames D, Koenig HG. It’s time to talk about physician burnout…and moral injury. Lancet Psychiatry. 2019;6:e28. doi: 10.1016/S2215-0366(19)30385-2. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R, Williams W. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Litz BT, Lebowitz L, Nash WP, Gray MJ. Adaptive disclosure: A new treatment for military trauma, loss, and moral injury. NY, NY: Guilford Publications; 2017. [Google Scholar]
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, Maguen S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Reviews. 2009;29:695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Manea L, Gilbody S, McMillan D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. General Hospital Psychiatry. 2015;37(1):67–75. doi: 10.1016/j.genhosppsych.2014.09.009. [DOI] [PubMed] [Google Scholar]
- Mantri, S., Lawson, J.M., Wang, Z.Z., Koenig, H.G. (2020). Prevalence and predictors of moral injury in healthcare professionals. Journal of Nervous and Mental Disease (in submission) [DOI] [PubMed]
- Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- Maslach C, Jackson SE, Leiter MP, Schaufeli WB, Schwab RL. Maslach burnout inventory. Palo Alto, CA: Consulting Psychologists Press; 1986. pp. 3463–3464. [Google Scholar]
- Nash WP, Marino Carper TL, Mills MA, Au T, Goldsmith A, Litz BT. Psychometric evaluation of the Moral Injury Events Scale. Military Medicine. 2013;178:646–652. doi: 10.7205/MILMED-D-13-00017. [DOI] [PubMed] [Google Scholar]
- Paul LA, Gros DF, Strachan M, Worsham G, Foa EB, Acierno R. Prolonged exposure for guilt and shame in a veteran of Operation Iraqi Freedom. American Journal of Psychotherapy. 2014;68:277–286. doi: 10.1176/appi.psychotherapy.2014.68.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce M, Haynes K, Rivera NR, Koenig HG. Spiritually-integrated cognitive processing therapy: A new treatment for moral injury in the setting of PTSD. Global Advances in Health and Medicine. 2018;7:1–7. doi: 10.1177/2164956118759939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reith TP. Burnout in United States healthcare professionals: A narrative review. Cureus. 2018;10(12):e3681. doi: 10.7759/cureus.3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay J. Achilles in Vietnam: Combat trauma and the undoing of character. New York, NY: Scribner; 1994. [Google Scholar]
- Shay J. Moral injury. Psychoanalytic psychology. 2014;31:182–191. doi: 10.1037/a0036090. [DOI] [Google Scholar]
- Sibeoni J, Bellon-Champel L, Mousty A, Manolios E, Verneuil L, Revah-Levy A. Physicians’ perspectives about burnout: A systematic review and metasynthesis. Journal of General Internal Medicine. 2019;34(8):1578–1590. doi: 10.1007/s11606-019-05062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R, Kroenke K, Williams J. Validation and utility of a self-report Version of PRIME-MD: the PHQ Primary Care Study. Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Swinson RP. The GAD-7 scale was accurate for diagnosing generalized anxiety disorder. Evidence Based Medicine. 2006;11(6):184. doi: 10.1136/ebm.11.6.184. [DOI] [PubMed] [Google Scholar]
- Verma RP. Mental and physical health of physicians undergoing postgraduate training in the USA: A single center study. International Journal. 2019;2(4):10. [Google Scholar]
- Wang, ZZ, Koenig, HG, Tong, Y., Wen, J., Sui, M., Liu, H., Liu, G. (2020). Psychometric properties of the Moral Injury Symptoms Scale among Chinese health professionals during the COVID-19 pandemic. Epidemiology and Psychiatric Sciences (in submission)
- Wang ZZ, Ma H, Rong Y, Koenig HG. Psychometric properties of Belief into Action Scale among university students in China. International Journal of Social Science Studies. 2016;4:83. doi: 10.11114/ijsss.v4i3.1363. [DOI] [Google Scholar]
- White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. Journal of the American Medical Association. 2020;323(18):1773–1774. doi: 10.1001/jama.2020.5046. [DOI] [PubMed] [Google Scholar]