Abstract
Purpose
In the current COVID pandemic, hermetically sealed eyewear is recommended for safe surgical practices to prevent eye contact with contaminated airborne particles or aerosols. These sealed eyewears definitely reduce the risk of contamination of eyes. However, there is a constant issue of fogging up of the inner surface that prevents good surgical visibility which can impair surgeons’ performance and their ability to perform fine tasks, especially in operating rooms with temperature and humidity controlled as per the COVID guidelines. We investigated the effectiveness of surface-modified anti-fog polyethylene terephthalate(PET) films and the application of a detergent-based surfactant liquid, applied to the inner aspect of viewing frame, and addition of filtered vents in the prevention of fogging up of the protective eyewears in a simulated operating room environment.
Methods
Ten volunteer orthopedic surgeons tested three modifications of a poly-hydrocarbon based hermetically sealed eyewear as a) application of a surface-modified anti-fog PET film on the inner aspect of eyewear, b) application of a detergent-based surfactant coating on the inner aspect of the protective eyewear, and c) addition of two filtered vents/holes on each side of the protective eyewear, covered with an N95 mask cutting. The testing was performed while completing a synthetic bone-based surgical task in a simulated operating room environment of 24–26° temperature and humidity between 40 and 70%, for a maximum of 2 h. The duration to the loss of clear visibility (ability to read a newspaper) and workable visibility (ability to perform the surgical task) was recorded for each volunteer.
Results
The detergent-based surfactant provided the longest duration of clear visibility (69.3 ± 8.16 min) and the workable visibility was maintained for more than 2 h. The second best durations of clear visibility (31.9 ± 3.75 min) and workable visibility (41.6 ± 5.39 min) were provided by the surface-modified anti-fog PET film. The addition of the filtered vents provided only a marginal improvement in the visibility.
Conclusion
A detergent-based surfactant coating of the viewing surface provides a simple, inexpensive and effective solution to the problem of fogging of the protective eyewears. Besides this, the workable vision is maintained for a prolonged duration.
Keywords: Eyewear, Fogging, Misting, Protection, COVID pandemic, Safety
1. Introduction
The current COVID scenario has brought a challenging situation for all healthcare workers. While all efforts should be made to provide quality medical/surgical care to the patients, self-protection is equally important in the current scenario. High transmissibility and fatality rates have been associated with the SARS-CoV-2 virus.1 Orthopedic surgical procedures in the current times carry a high risk of disease exposure because of the generation of aerosol particles.2 Additionally, considering the high incidence of asymptomatic patients, and a major proportion of patients with false-negative reports with the conventionally used RT-PCR (Reverse transcription-polymerase chain reaction) test, every operative patient should be treated as a potential COVID infected patient for the purpose of self-protection.3 The standard surgical outfits used to be light and comfortable; however, the personal protective equipment that covers the surgeon from head to toe using an impermeable layer is cumbersome; and with prolonged surgeries, there is increased sweating and perspiration that can result in discomfort and can potentially impair the surgeon’s performance as well. Secondly, eye protection needs to be different from that used in pre-COVID times. Previously, with limited risk of infection from aerosol and airborne particles, eye protection was mainly used to prevent direct contact with blood or fluid spill droplets. A simple eye shield or goggles used to be sufficient to prevent such a contact. A common issue with the use of protective eyewear is the fogging up of the viewing surface which often results in a lack of compliance with the eyewear among surgeons.4 However, in the pre-COVID era, with the exception of high-risk infected patients, the risk of any serious infection with non-compliance to the eyewears had not been reported or was not significant.5 A few techniques to prevent fogging of eyewears had been suggested in the past by tightening the seal on top of the mask and by the use of surfactant liquid on the inner aspect of eyewear.6,7 These techniques looked attractive and were useful as well. However, the big difference of the protective eyewears in the COVID era compared to the earlier used ones is the sealed protection to the eyes. The currently recommended protective eyewears to prevent the exposure of the eye to aerosol or airborne particles are hermetically sealed eyewears.8,9 With no space for outer air circulation and increased perspiration of skin in a closed cavity, the risk of fogging increases. Additionally, with the recommended operating room conditions in COVID times, i.e, temperature between 24 and 30 °C and humidity between 30 and 70%, and also with the orthopedic procedures requiring exertion, the perspiration increases, resulting in excessive fogging.10 Fogging impairs the clarity of vision and the surgeon’s ability to locate and operate fine instruments. This results in extra efforts to perform common tasks, early exhaustion, increased sweating, and perspiration. The cost-effectiveness of protective eyewears that claim to prevent fogging has not been established which limits their practical applicability. The claims of anti-fog glasses have been shown to fail and there is a general lack of regulations to establish the superiority and effectiveness of the antifog designs.11 Therefore, a low-cost modification of the hermetically sealed protective eyewear that can prevent fogging is desirable in the current times. Plastic films such as polyethylene terephthalate (PET) with surface modifications,12 surfactant sprays,6,13 and addition of N95 mask cutting to the air vents of the sealed eyewear9 are some attractive low-cost modifications to prevent fogging of the viewing frames. However, their effectiveness in a real surgical scenario or a simulated operating room environment with the aforestated modified parameters has not been tested. This comparative observational study investigates the effectiveness of these three modifications on a common hermetically sealed protective eyewear in controlling fogging up of the viewing frames in a simulated operating room environment.
2. Materials and methods
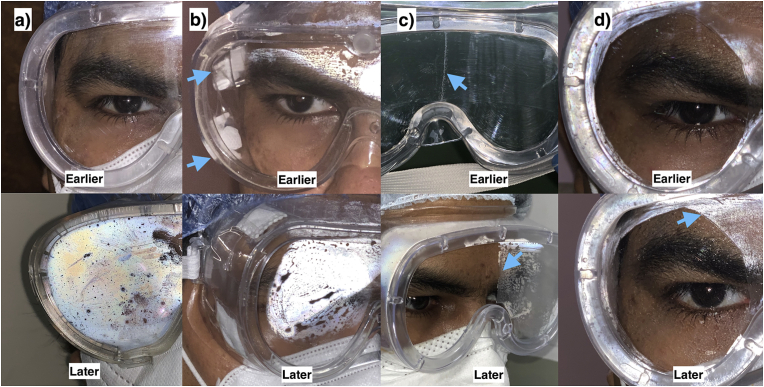
We created four testing groups based on the modifications of a poly-hydrocarbon based hermetically sealed protective eyewear that was common to all the testing groups. Group A consisted of protective eyewear without any modification(Fig. 1a). In group B, four holes with a centimeter diameter were created, with two holes on each side of the eyewear (Fig. 1b). The holes were covered with N95 mask cuttings that were sealed to the hole margins circumferentially, using an adhesive tape. In group C, the inner surface of the eyewear was coated with a detergent-based surfactant liquid that was allowed to dry for a few minutes prior to the testing (Fig. 1c). In group D, the inner surface of the viewing frame of the eyewear was covered with a commercially available anti-fog nano-coated PET film (Fig. 1d). Ten volunteer orthopedic surgeons with unaided normal vision participated in the study to test each of the eyewear modifications in the aforestated groups. The testing was performed in an operating room with a temperature set between 24 and 26 °C and humidity set between 40 and 70%. Each volunteer was provided with a newspaper, a synthetic model of the femur, a 4.5 mm LCP (locking compression plate) instrumentation, and a large bone external fixator instrumentation. Each volunteer was asked to perform the following tasks in a repeat mode in the following sequence: a) create a simple fracture of the synthetic bone model using multiple drill holes, b) fixation of the fracture using a 4.5 mm LCP with four screws on each side of the fracture, c) removal of the plate, d) stabilization of the fracture with an external fixator with two pins each in the proximal and distal fragments, e) removal of the external fixator, for a maximum of 2 h duration or to the point when fogging limits visibility completely, whichever is earlier. The time point when the volunteer felt a change in visibility due to fogging, the viewing ability was checked by the ability to read the newspaper comfortably. The time duration up to the failure to read the newspaper was recorded for each volunteer as the loss of clear visibility. The volunteers continued to perform the given task until the fogging distorted the vision to such an extent that the task couldn’t be performed. This was regarded as the loss of workable visibility. The total duration up to the loss of workable visibility was recorded. The mean duration and standard deviation (SD) of the time taken to the loss of clear visibility and workable visibility was calculated for each of the volunteers and testing groups. The time duration to the loss of clear visibility and workable visibility among the modified testing groups (group B-D) were compared to the unmodified group (group A) using paired samples t-test.
Fig. 1.
a) In group A, the eyewear was used without any modification resulting in an early and extensive fogging. b) In group B, the filtered vents on the sides of the eyewear provided only a marginal improvement in delaying the fogging. c) In group C, the detergent-based surfactant was applied and dried on the inner surface of the viewing frame. A representational picture shows the surfactant being applied on the right half of the viewing frame (upper arrow) resulting in extensive fogging of the left half (lower arrow), while clear visibility is maintained on the right side. d) In group D, a round segment of the surface-modified anti-fog PET film was applied on the inner surface. The film prevented the fogging for a prolonged duration while the remaining peripheral part displayed fogging (arrow).
3. Results
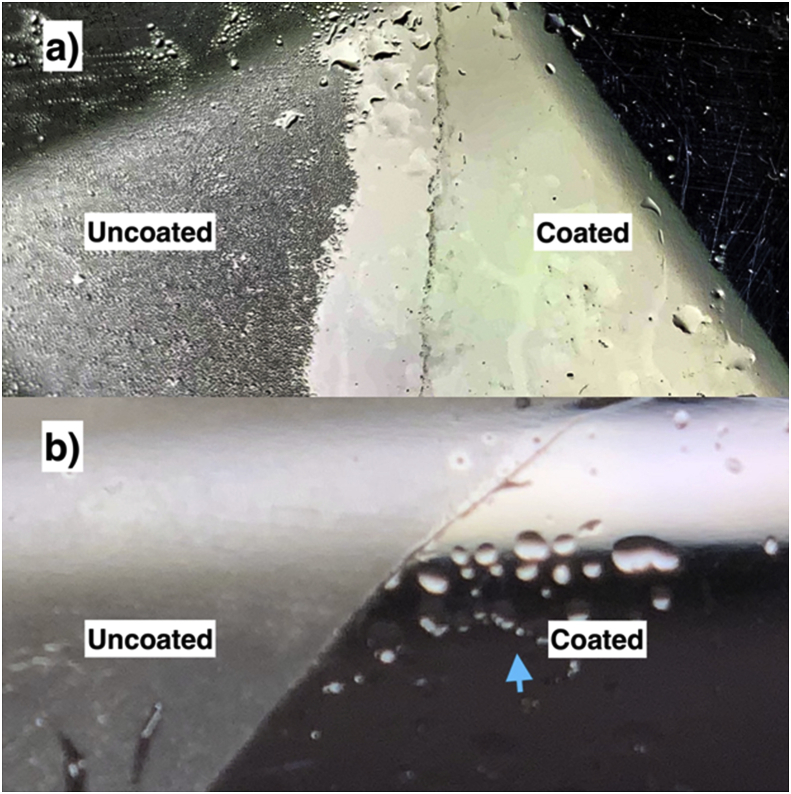
The longest duration of clear visibility (69.3 ± 8.16 min) was observed in group C with detergent-based surfactant coating of the inner surface of the viewing frame and its workable visibility was maintained for more than 2 h for all the volunteers. All the modified groups tested significantly better than group A (group without any modification). The group D with surface modified PET film had provided workable visibility for a prolonged duration (41.6 ± 5.39 min), however, the workable visibility was lost not because of fogging but because of the formation of large droplets on the inner surface (Fig. 2a). The moisture did collect on the detergent-based surfactant coating also, but that formed more of a uniform layer unlike the PET film(Fig. 2b). The detailed results are presented in Table 1.
Fig. 2.
A closeup view of the surfactant based coating (a) shows a little distortion of the vision on the coated side due to more uniform spread of the moisture, compared to the surface-modified anti-fog PET film (b) where moisture coalesced to form larger droplets (arrow) that hindered clear vision.
Table 1.
Time taken to the loss of clear visibility and workable visibility through protective eyewear among different testing groups.
| Time to loss of clear visibility (mean ± SD) (In minutes) | Time to loss of workable visibility (mean ± SD) (In minutes) | Comparison using the paired t-test | |
|---|---|---|---|
| Group A (protective eyewear without modification) | 17.7 ± 2.31 | 23 ± 3.80 | NA |
| Group B (protective eyewear with N95 mask cuttings based filter vents) | 23 ± 2.94 | 27.3 ± 1.70 | Significant improvement in clear and workable visibility compared to group A (p < 0.05) |
| Group C (Detergent based surfactant coating on the inner surface) | 69.3 ± 8.16 | Workable vision was maintained at 2 h duration for all volunteers | Significant improvement in clear and workable visibility compared to group A (p < 0.05) |
| Group D (surface modified PET film on the inner surface) | 31.9 ± 3.75 | 41.6 ± 5.39 | Significant improvement in clear and workable visibility compared to group A (p < 0.05) |
4. Discussion
The protection of healthcare workers is of paramount importance in the current COVID pandemic. Orthopedic surgical procedures have been shown to have a high risk of aerosol generation and contamination of eye fields.14 Protective eyewear helps in preventing the conjunctival or corneal contamination by the surgical splash particles. Even ordinary eyewear has been shown to be effective in preventing contact with splash particles.15 However, in the current COVID scenario, sealed protection from all sides of the eye is recommended. The disposable single-use plastic eyewear with contoured margins to create a seal with the skin in contact has been shown to have a very low risk of contamination and therefore should be preferred.16 A common problem with the eyewear and more with the sealed eyewear is the issue of fogging that limits the clear visibility which contributes to intraoperative stress and impairs the surgeon’s performance. Hermetically sealed eyewears have a higher risk of fogging considering the entrapment of moisture in a closed cavity. Moreover, it is difficult to change the eyewear intraoperatively as that would add the risk of contamination of eyes by the airborne particles in the surrounding field.
The ongoing research in development of antifog surfaces focuses on the use of eco friendly materials, especially the plant based products like starch, cellulose and fibres; application of nano surface modifications in preventing collection of moisture on surface; and inducing self healing properties in surface coating under degradation. However, their application in the medical field is prominent and will need further investigations to establish the same. For example, Titanium dioxide has been widely used as an anti fogging coat for the eyewears because of its hydrophilic nature and self-cleaning ability due to photocatalysis.17
Among the simple methods to prevent fogging of the eyewear, a variety of methods including the application of surfactant liquid, converting the eyewear to a filtered eye mask by creating vents sealed with N95 mask cutting and use of anti-fog glasses or anti-fog coating have been described.6,9,12,13 However, the actual effectiveness of these methods which perform the operative procedures remains unknown. We tested three inexpensive modifications on a disposable sealed poly-hydrocarbon based protective eyewear and found that the detergent-based liquid surfactant was effective in maintaining the workable vision for as long as 2 h. The PET material based anti-fog film although prevented fogging for long but failed to provide the workable vision required for a simulated surgical task. The perspiration or the fog droplets appeared to be coalesced to form larger droplets on the surface of the PET films forming a nonuniform layer that hindered a clear vision. On the contrary, the surfactant formed a uniform layer of moisture on the applied surface, and therefore vision was not distorted. It is therefore important to spread the surfactant uniformly over the viewing surface to prevent the non-uniform deposition of moisture. The addition of the filtered vents sealed with N95 mask cutting had only marginal improvement compared to the unmodified version of the eyewear and thus may not be helpful. The effectiveness of the anti-fog glasses has previously been questioned and it is difficult to establish or control the same considering the lack of regulatory mechanisms. Also, with preference to single-use goggles, the expenses on the anti-fog glasses may not be a cost-effective measure.
As we move ahead in this pandemic, more effective solutions may emerge with more research and development concerning the protective eyewear. In the current scenario, judicious use of the limited resources is required, and therefore, low-cost modification of the eyewear for effectively clear intraoperative visibility is required. Our results suggest that the same can be very well achieved. The ministry of health and family welfare (MOHFW) of India recommends the sealed goggles with viewing-surface modifications and addition of indirect vents to reduce fogging.18 However, the effectiveness of vents and the fog resistant coatings has not been tested previously and currently there are no regulations for the same. The information provided in this preliminary study can be helpful in further exploring the use of dried surfactant coatings for preventing fogging in practical scenarios with a judicious approach.
There are some limitations of this study considering the small number of testing volunteers and lack of the data from the actual surgical scenarios. However, it would be difficult to conduct such a trial on a real surgical situation as that can compromise the safety of the surgeon as well as the patient. In the situation of conducting this exercise in a real surgical scenario, the backup options in the form of additional glasses and personal protective equipment (PPEs) should always be available. Lastly, the results are based on an ordinary poly-hydrocarbon made single-use protective eyewear. The results with other eyewears may or may not differ. Thus, it would be desirable to test these methods on the eyewears prior to surgery through a simulated exercise.
To conclude, a detergent-based surfactant coating of the viewing surface provides an effective and inexpensive solution to the problem of fogging of the protective eyewears. Besides this, the workable vision is maintained for a prolonged duration. The surface-modified PET film does prevent fogging but that may not be helpful in a surgical scenario.
Source of funding
None.
Declaration of competing interest
None.
Contributor Information
Arvind Kumar, Email: arvindmamc@gmail.com.
Owais Ahmed Qureshi, Email: drowaisqureshi@gmail.com.
Rajesh Arora, Email: rajeshmamc@gmail.com.
Sandeep Kumar, Email: drsandeepkumar20@gmail.com.
Javed Jameel, Email: drjavedjameel@gmail.com.
Rizwan Khan, Email: drrizwan85@gmail.com.
References
- 1.Cheng H.Y., Jian S.W., Liu D.P. Contact tracing assessment of COVID-19 transmission dynamics in taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yeh H.C., Turner R.S., Jones R.K., Muggenburg B.A., Lundgren D.L., Smith J.P. Characterization of aerosols produced during surgical procedures in hospitals. Aerosol Sci Tech. 1995 Jan 1;22(2):151–161. [Google Scholar]
- 3.WHO Q&A: infection prevention and control for health care workers caring for patients with suspected or confirmed 2019-nCoV. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-on-infection-prevention-and-control-for-health-care-workers-caring-for-patients-with-suspected-or-confirmed-2019-ncov Cited.
- 4.Crebolder J.M., Sloan R.B. Determining the effects of eyewear fogging on visual task performance. Appl Ergon. 2004;35(4):371-381. doi: 10.1016/j.apergo.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PloS One. 2012;7(4) doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malik S.S., Malik S.S. A simple method to prevent spectacle lenses misting up on wearing a face mask. Ann R Coll Surg Engl. 2011;93(2):168. doi: 10.1308/003588411x12851639107313b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jordan D.J., Pritchard-Jones R. Tying a surgical mask to prevent fogging. Ann R Coll Surg Engl. 2014;96(2):165. doi: 10.1308/rcsann.2014.96.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J.O., Lam D.S.C., Chen Y., Ting D.S.W. Novel Coronavirus disease 2019 (COVID-19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020 Mar;104(3):297–298. doi: 10.1136/bjophthalmol-2020-315994. [DOI] [PubMed] [Google Scholar]
- 9.Douglas D., Douglas R. Addressing the corona virus pandemic: will a novel filtered eye mask help? Int J Infect Dis. 2020;95:340-344. doi: 10.1016/j.ijid.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malhotra N., Bajwa S.J., Joshi M., Mehdiratta L., Trikha A. COVID operation theatre- Advisory and position statement of Indian society of anaesthesiologists (ISA national) Indian J Anaesth. 2020;64:355–362. doi: 10.4103/ija.IJA_454_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dain S.J., Hoskin A.K., Winder C., Dingsdag D.P. Assessment of fogging resistance of anti-fog personal eye protection. Ophthalmic Physiol Optic. 1999;19(4):357-361. doi: 10.1046/j.1475-1313.1999.00418.x. [DOI] [PubMed] [Google Scholar]
- 12.Sason E., Kolitz-Domb M., Chill J.H., Margel S. Engineering of durable antifog thin coatings on plastic films by UV-curing of proteinoid prepolymers with PEG-diacrylate monomers. ACS Omega. 2019;4(5):9352–9360. doi: 10.1021/acsomega.9b00336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nezhat C., Morozov V. A simple solution to lens fogging during robotic and laparoscopic surgery. J Soc Laparoendosc Surg. 2008;12(4):431. [PMC free article] [PubMed] [Google Scholar]
- 14.Hirschmann M.T., Hart A., Henckel J., Sadoghi P., Seil R., Mouton C. COVID-19 coronavirus: recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1690. doi: 10.1007/s00167-020-06093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bell K.M., Clement D.A. Eye protection for the surgeon. J R Coll Surg Edinb. 1991 Jun;36(3):178–179. [PubMed] [Google Scholar]
- 16.Mansour A.A., 3rd, Even J.L., Phillips S., Halpern J.L. Eye protection in orthopaedic surgery. An in vitro study of various forms of eye protection and their effectiveness. J Bone Joint Surg Am. 2009;91(5):1050–1054. doi: 10.2106/JBJS.H.00460. [DOI] [PubMed] [Google Scholar]
- 17.Durán I.R., Laroche G. Current trends, challenges, and perspectives of anti-fogging technology: surface and material design, fabrication strategies, and beyond. Prog Mater Sci. 2019;99:106–186. [Google Scholar]
- 18.Ministry of Health and Family Welfare Directorate General of Health Services [Emergency Medical Relief] Novel coronavirus disease 2019 (COVID-19): guidelines on rational use of personal protective equipment. https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf Cited July 9,2020.