Abstract
COVID-19 is the disease caused by Novel Coronavirus (SARS-CoV-2) infection and world current main public health problem, due to its easy transmissibility and multiple clinical presentations. The main symptoms reported worldwide are dry cough, dyspnea, and fever, as well as anosmia and ageusia. COVID-19 diagnosis is made with RT-PCR, but many other complementary exams may be used to guide clinical practice, such as Chest Computerized Tomography (CT), showing ground glass opacities; increase in inflammatory markers, as C-Reactive Protein and Erythrocyte Sedimentation Rate; hemogram might show hypoalbuminemia, thrombocytopenia. Severe cases may evolve to thromboembolic and atheroembolic events, leading to stroke, myocardial infarction, pulmonary thromboembolism. Male, 28 years old, went for neurological appointment after presenting episode of intense headache, dysarthria, deviation of lip rhyme on appointment’s eve. Previously healthy, no comorbidities or risk factors. Underwent brain MRI and serum serological analysis. SARS-CoV-2 capacity of affecting brain homeostasis by breaking blood–brain barrier, makes it easier to develop ischemic or inflammatory damage, and invading central nervous system. Neurological symptoms and syndromes are the main consequences of COVID-19 pandemic and must be prevented through adequate clinical management.
Keywords: Stroke, Vasculitis, COVID-19, SARS-CoV-2
1. Introduction
COVID-19 is the disease caused by Novel Coronavirus (SARS-CoV-2) infection, which has quickly escalated to a pandemic scenario. Its transmission is mainly through respiratory droplets, allowing the virus to replicate in upper respiratory tract’s mucosal epithelium, where it may lead to anosmia and ageusia symptoms; and invade other tissues, as lower respiratory tract, and gastrointestinal system, allowing it to manifest as diarrhea and other gastrointestinal symptoms. However, it is inside lungs where the virus develops the main symptoms of COVID-19, such as dry cough, dyspnea and fever, due to intense inflammatory response, through T CD4 and T CD8 cytotoxic response, leading to lung’s epithelial and endothelial cells damage and death, causing intravascular content leakage and stimulating more intense inflammatory response [1], [2]. Other frequent features in complementary exams of COVID-19 are bilateral ground-glass opacities on chest CT; increase in inflammatory markers (C-Reactive Protein and Erythrocyte Sedimentation Rate), hypoalbuminemia, thrombocytopenia. More severe cases may develop Intravascular Disseminated Coagulation, leading to thromboembolic events, such as myocardial infarction, pulmonary embolism, stroke; and hemorrhagic events, such as necrotizing hemorrhagic encephalopathy [2].
2. Case report
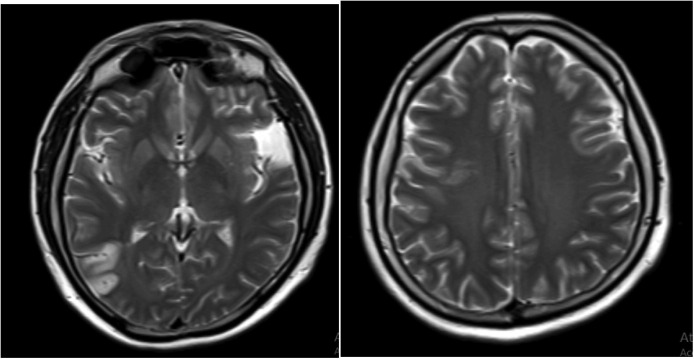
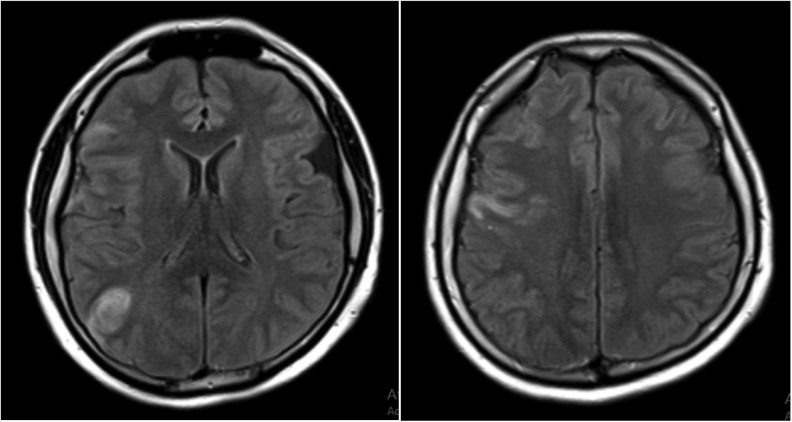
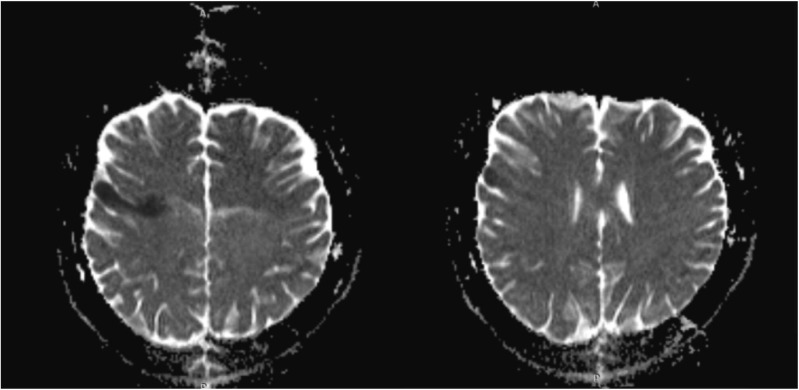
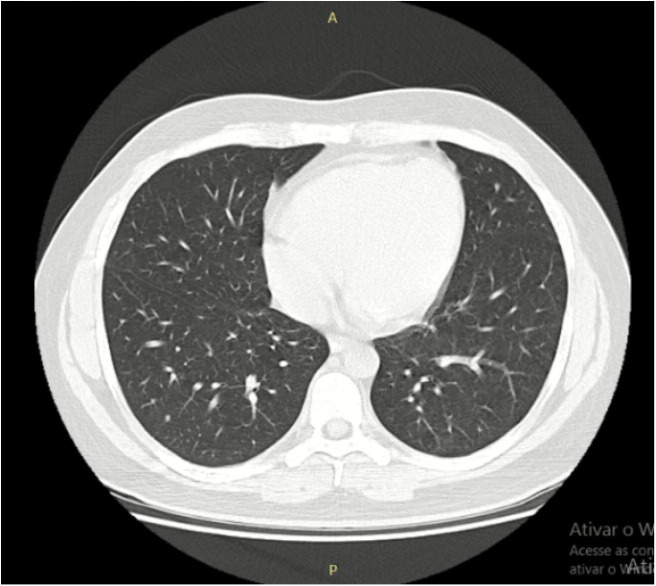
Male, 28 years old, went for neurological appointment after presenting episode of intense headache, dysarthria, deviation of lip rhyme to the left on appointment’s eve. Previously healthy, no comorbidities or risk factors. To the physical examination: motor aphasia, loss of strength in left hemi body, photophobia, and deviation of lip rhyme to the left, enhanced reflexes in right hemi body, incapable of walking. Underwent brain MRI and serum serological analysis (SARS-CoV-2 IgM positive) (Fig. 1, Fig. 2, Fig. 3, Fig. 4 ).
Fig. 1.
MRI image demonstrating T2 sequence showing hyperintensity in right temporal area measuring 3,1 × 1,9 cm.
Fig. 2.
MRI image demonstrates FLAIR sequence with two hyperintense lesions in right parietal and frontal areas at subcortical region, with diffusion restriction. Also, it is possible to note Arachnoid cyst in right temporal fossa. Conclusions: Two hyperintense lesions in cortical and subcortical regions, possibly due to vasculitis.
Fig. 3.
Diffusion restriction in right parietal and frontal areas at cortical and subcortical.
Fig. 4.
Thorax CT showing airways’ atelectasis in left lung’s lateral segment of mid lobe and posterior basal segment of inferior lobe.
3. Discussion
Ischemic stroke is a disease in which neurological deficit develop for a short period of time due to focal ischemia, due to temporary reduction or stop on brain’s blood flow, its main causes are thromboembolism, cardiac arrhythmias, and atheroembolism and its risk factors are high blood pressure, diabetes, high LDL cholesterol levels, age, Coronavirus’ infection leads to important inflammatory response and cytokine storm, which in more severe cases leads to IDC, causing thromboembolic phenomena and thrombocytopenia [2], [3], [4]. It is still uncertain SARS-CoV-2 capacity of invading certain tissues, but it is known its capacity of affecting brain homeostasis by breaking blood–brain barrier, making it easier to develop ischemic or inflammatory damage, and invading central nervous system. Neurological symptoms and syndromes have been related worldwide – agitation, enhanced tendon reflexes, ankle clonus and Guillain-Barré syndrome – strengthens the hypothesis of virus’ tropism for central nervous system [3], [4], [5].
4. Conclusion
SARS-CoV-2 has numerous still unknown clinical features and consequences to organism. It is important to relate all possible manifestations worldwide to control pandemic’s damages and prevent casualties by creating clinical management protocols of these patients.
Conflict of interest
None declared.
Funding
None.
References
- 1.Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin Immunol. 2020;215:1–23. doi: 10.1016/j.clim.2020.108427. Elsevier BV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance. World Health Organization, mar. 13, 2020. WHO/2019-nCoV/clinical/2020.4.
- 3.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E. Clinical laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:1–30. doi: 10.1016/j.tmaid.2020.101623. Elsevier BV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iroegbu J.D., Ifenatuoha C.W., Ijomone O.M. Potential neurological impact of coronaviruses: implications for the novel sars-cov-2: implications for the novel SARS-CoV-2. Neurol Sci. 2020:1–9. doi: 10.1007/s10072-020-04469-4. Springer Science and Business Media LLC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helms J., Kremer S., Merdji H. Neurologic features in severe SARS-CoV-2 infection. New Engl J Med. 2020:1–2. doi: 10.1056/nejmc2008597. Massachusetts Medical Society. [DOI] [PMC free article] [PubMed] [Google Scholar]