A 48-year-old-female was diagnosed with SARS-CoV-2 infection by reverse-transcriptase-polymerase-chain-reaction. One day later, she experienced an episode of acute typical chest pain and was transferred to our hospital due to elevated cardiac enzymes (high-sensitivity Troponin-T: 542,6 ng/l (reference upper level (RUL): 14 ng/l) and creatine kinase (CK): 226 U/l (RUL: 170 U/l). Electrocardiogram showed intermittent negative T-waves in inferior leads (II, III, aVF, V4 and V5) matching with inferior wall motion abnormalities in transthoracic echocardiography, leading to the diagnosis of non ST-elevation myocardial infarction (NSTEMI). C-reactive protein, interleukin-6, neopterin, procalcitonin and blood count were normal.
Coronary ECG-gated computed tomography angiography (CTA) ruled out coronary stenosis >50% but showed midventricular systolic constriction (Movie 1) without apical ballooning. Subendocardial myocardial perfusion defects were found in multiple myocardial segments (Fig. 1 ) representing typical imaging findings for myocardial infarction with non-obstructive coronary arteries (MINOCA). Cardiac magnetic resonance imaging (CMR) confirmed subendocardial inferior zonal late enhancement. Coronary CTA (Fig. 2 ) further showed diffuse irregular vessel walls thickening and perivascular edema, defined as a perivascular fat attenuation index (FAI) of > -70HU, suggestive for vasculitis. There was no typical COVID-19 pulmonary involvement. The patient was treated with acetylsalicylic acid and clopidogrel. Cardiac enzymes declined after 2 days and she was discharged asymptomatic after 6 days.
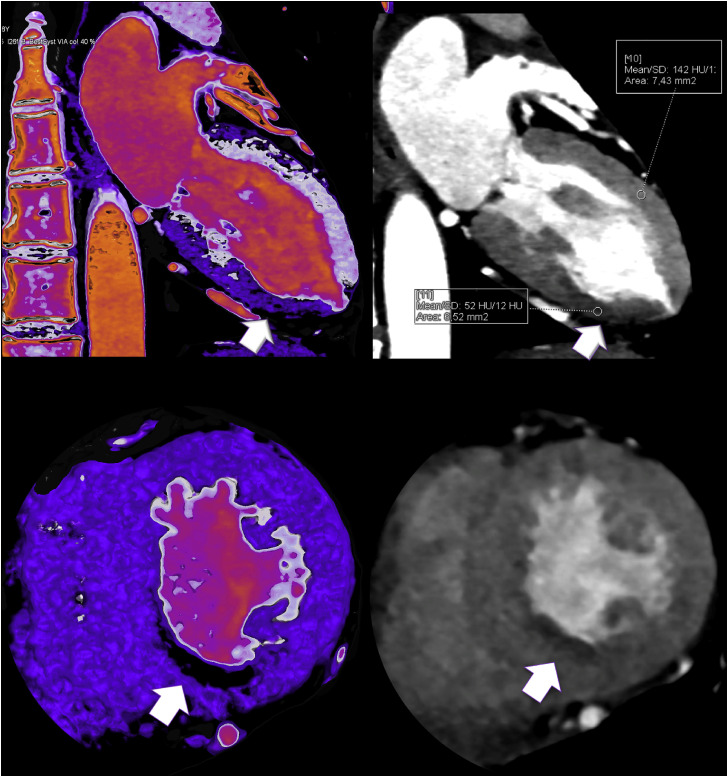
Fig. 1.
MINOCA by coronary CTA: Midsystolic phase (2-chamber view) shows territorial inferior myocardial hypoperfusion with lower attenuation (52 HU) as compared to the anterior myocardium (142 HU) during first pass arterial perfusion. Multiplanar reformation (MRP) (right) with narrow C/W settings and color-coded thin slice 3D VRT (left). 2-Chamber view (upper panel) and corresponding short axis (lower panel) view using a dedicated 3D postprocessing software (SyngoVIATM, Siemens). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
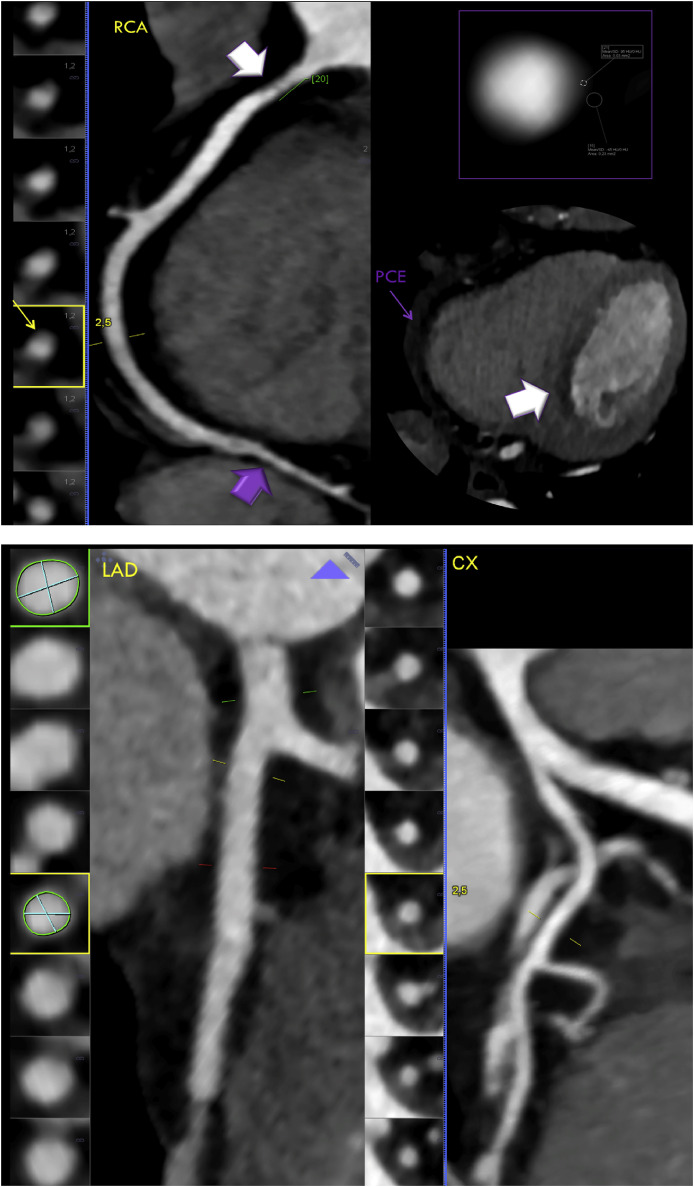
Fig. 2.
Coronary CTA findings suggestive for vasculitis: Right coronary artery (RCA) with diffuse irregular vessel walls, narrowing with less than 50% stenosis (white arrow, left) and isodense wall thickening (yellow arrow). Perivascular edema was diagnosed by quantifying a perivascular fat attenuation index (FAI) of −45HU on a cross sectional image (upper right). Diffuse narrowing of distal RCA (left,purple arrow) causing inferior and inferoseptal myocardial hypoperfusion (right, white arrow). Mild pericardial fluid collection suggesting mild pericardial effusion (PCE) (purple arrow). Left anterior descending (LAD) artery showed proximal ectasia, mild vessel wall irregularities and perivascular edema (FAI -55HU). CX = circumflex artery. RCA, LAD and CX are shown by curved multiplanar reformations (cMPR). (SyngoVIA™, Siemens). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
1. Discussion
Myocardial damage during SARS-CoV-2 infection occurs in 8–12%1 and more commonly, during severe clinical courses. In our patient, symptoms were mild and CTA-images showed midventricular systolic constriction but without apical ballooning. Multiple zonal subendocardial myocardial perfusion defects were present but no coronary stenosis >50%, suggesting MINOCA, which was confirmed by CMR late-enhancement. CMR ruled out myocarditis. Invasive coronary angiography was avoided. Further, CTA showed signs of vasculitis with diffuse wall irregularities and focal thickening, which may trigger endothelial dysfunction and vasospasm. Perivascular edema was quantified by coronary CTA using the fat-attenuation-index (FAI)3, which was >-70 HU and as well supports the presence of perivascular inflammation. SARS-CoV-2 may infect the endothelium over ACE-2 receptors. Viral elements within endothelial cells and inflammatory cell death were recently confirmed on pathohistology.2 In addition, SARS-CoV-2 has been linked with procoagulative states and hence may favor microvascular thrombosis, which represents a further possible cause of MINOCA.
In summary, coronary CTA was a useful imaging modality in our patient with NSTEMI and SARS-CoV-2 infection to avoid invasive angiography. CTA imaging findings should be regarded as “hypothesis-generating” for the initiation of further systematic research studies.
2. Summary - TOC
-
•In a 48 year-old-female with myocardial injury and SARS-CoV-2 infection, coronary CTA showed:
-
oMultiple subendocardial myocardial perfusion defects with less than 50% coronary stenosis (MINOCA)
-
oImaging features suggestive of vasculitis, with perivascular edema-defined as fat attenuation index (FAI)> - 70 HU and diffuse as well as focal vessel wall thickening, potential triggers of endothelial dysfunction, vasospasm and microvascular thrombosis.
-
oCTA ruled out coronary stenosis >50% and invasive coronary angiography was avoided.
-
o
Disclosures
No financial support was received. There is no conflict of interest.
There are no disclosures for all authors.
Declaration of competing interest
The authors declare no conflict of interest.
The manuscript has not been submitted elsewhere.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcct.2020.07.002.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Lippi G., Lavie C.J., Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020 Mar 10 doi: 10.1016/j.pcad.2020.03.001. pii: S0033-0620(20)30055-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Varga Z., Flammer A.J., Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oikonomou E.K., Marwan M., Desai M.Y. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet. 2018;392(10151):929–939. doi: 10.1016/S0140-6736(18)31114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.