Abstract
Background
The severe acute respiratory syndrome coronavirus 2 pandemic has created challenges to neurosurgical patient care. Despite editorials evaluating neurosurgery responses to 2019 novel coronavirus disease (COVID-19), data reporting effects of COVID-19 on neurosurgical case volume, census, and resident illness are lacking. The aim of this study was to present a real-world analysis of neurosurgical volumes, resident deployment, and unique challenges encountered during the severe acute respiratory syndrome coronavirus 2 outbreak peak in New York City.
Methods
Daily census and case volume data were prospectively collected throughout the severe acute respiratory syndrome coronavirus 2 outbreak in spring 2020. Neurosurgical census was compared against COVID-19 system-wide data. Neurosurgical cases during the crisis were analyzed and compared with 7-week periods from 2019 and early 2020. Resident deployment and illness were reviewed.
Results
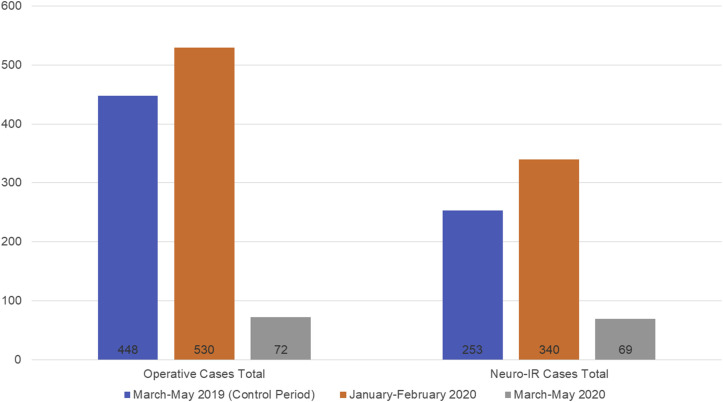
From March 16, 2020, to May 5, 2020, residents participated in 72 operations and 69 endovascular procedures compared with 448 operations and 253 endovascular procedures from January 2020 to February 2020 and 530 operations and 340 endovascular procedures from March 2019 to May 2019. There was a 59% reduction in neurosurgical census during the outbreak (median 24 patients, 2.75 average total cases daily). COVID-19 neurosurgical admissions peaked in concert with the system-wide pandemic. Three residents demonstrated COVID-19 symptoms (no hospitalizations occurred) for a total 24 workdays lost (median 7 workdays).
Conclusions
These data provide real-world guidance on neurosurgical infrastructure needs during a COVID-19 outbreak. While redeployment to support the COVID-19 response was required, a significant need remained to continue to provide critical neurosurgical service.
Key words: COVID-19, Neurosurgery residency, Pandemic, Residency training
Abbreviations and Acronyms: ACGME, Accreditation Counsel for Graduate Medical Education; ARDS, Acute respiratory distress syndrome; COVID-19, 2019 novel coronavirus disease; ICU, Intensive care unit; PCR, Polymerase chain reaction; PGY, Postgraduate year; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2
Introduction
The global pandemic associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus causing 2019 novel coronavirus disease (COVID-19), arrived in New York City on Sunday, March 1, 2020. To date at the time of this writing, there have been >340,000 cases confirmed in New York State, with 22,000 deaths.1 The Mount Sinai Health system has 3815 beds among 8 hospitals and is the largest health system within Manhattan caring for >150,000 inpatient admissions annually. At Mount Sinai, the neurosurgery department is one of several academic neurosurgery departments in the borough of Manhattan. The Mount Sinai Department of Neurosurgery has a 14-resident training program accredited by the Accreditation Counsel for Graduate Medical Education (ACGME), with residents participating in operative cases at 3 hospital locations and regularly fielding consultations from all 8 hospitals and affiliates within the health system.
On Saturday, March 7, 2020, the governor of New York declared a state of emergency, and on Sunday, March 15, the mayor of New York City announced that public schools would be closed and elective surgeries should be postponed. As of Monday, March 16, all surgeries within the Mount Sinai Health System were restricted to urgent or emergent cases. Focus was shifted toward preparing hospitals for maximal ventilatory capacity to address large amounts of intubated patients with severe COVID-19 pneumonia and acute respiratory distress syndrome. The majority of hospital and departmental resources were requested toward this effort. However, a significant burden of neurological disease was also encountered during this period.
We performed a numerical real-world analysis of our neurosurgical resident experience during the peak of the SARS-CoV-2 outbreak in New York City. Understanding volume and case mix of operative and neurointerventional procedures, daily patient census, intensive care unit (ICU) coverage needs, and rate of resident safety concerns and sick days during this period will aid in understanding resource allocation during future outbreaks. Our goal was to provide concrete real-world data that may help other departments prepare their response should they face subsequent second or third waves of the SARS-CoV-2 pandemic.
Resident Deployment
Mount Sinai Hospital
ICU Care
On Monday, March 23, 2020, the Neurosciences Intensive Care Unit at Mount Sinai Hospital became a primary COVID-19 unit with all Neurocritical Care faculty and fellows participating toward that effort. Another older ICU was converted to care for COVID-19–negative neurological patients. This functioning neurological ICU was staffed weekly with 1 cerebrovascular attending physician from the department. The neurocritical care fellows were replaced by 3 postgraduate year (PGY)–2 and PGY-3 neurosurgery residents, who alternated taking 24-hour in-house call every third night. This provided continuity of care while remaining compliant with work hour regulations. Additionally, a senior resident was assigned to the neurological ICU in a supervising fellow capacity and staffed emergent neurological transfers and remote neurological patient management.
As part of the larger COVID-19 effort, 1 senior resident and 1 PGY-2 or PGY-3 resident each contributed 4 12-hour shifts to the requisitioned COVID ICU on a weekly rotating basis, such that all residents had participated in caring for patients in the COVID-19 ICU. The overall resident deployment is depicted in Figure 1 .
Figure 1.
Neurosurgery residency clinical deployment. COVID-19, 2019 novel coronavirus disease; PGY, postgraduate year.
Service Line Care
The neurosurgical hospital service was staffed by 1 senior resident who rounded on all inpatients and consultations, with 3 interns, both categorical and noncategorical, alternating 24-hour in-house call every third night. This service chief resident supervised emergent non–operating room procedures and fielded all consultations before being staffed with a neurosurgical attending physician. One senior or chief resident was on call for all urgent or emergent neurosurgical operating room cases on a weekly rotating basis. One PGY-4 or PGY-5 resident with enfolded endovascular neurosurgical training was placed in the endovascular neurosurgical call pool and alternated call on a weekly basis.
Mount Sinai West Hospital
Mount Sinai West Hospital is a stand-alone hospital in the Mount Sinai Health System and is an intracerebral hematoma center of excellence. Before the COVID-19 pandemic, vascular, functional, spine, and brain tumor surgeries were regularly performed at this center. A chief resident and noncategorical intern staffed this rotation site and alternated weekend coverage to remain compliant with ACGME work hours. These residents were tasked with maintaining the neurosurgical service and were not primarily caring for intubated patients with COVID-19, although nonintubated patients with COVID-19 were boarded on the neurological floor and cared for by these residents.
Trauma Hospital
A senior resident and a categorical intern staffed our trauma hospital and alternated weekend coverage to remain compliant with ACGME work hours. These residents were tasked with maintaining the neurosurgical service and were not primarily caring for non-neurosurgical patients with COVID-19.
Materials and Methods
Daily neurosurgical census data were prospectively collected at the Mount Sinai Hospital during the peak of the New York City COVID-19 outbreak in spring 2020. All operative and interventional cases with direct neurosurgical resident coverage were collected at Mount Sinai Hospital and Mount Sinai West Hospital. All cases performed during the inclusion period were considered urgent and required approval by the system chair or vice-chair. Some diagnostic angiograms and kyphoplasties were performed only by an attending surgeon and nonphysician advanced practice providers without resident participation and were therefore excluded from this analysis. The study period was from the cessation of elective surgical procedures on March 16, 2020, until resumption of urgent nonemergent cases on May 5, 2020.
These case number data were compared with a 7-week period from January 6, 2020, to February 24, 2020 (before the SARS-CoV-2 outbreak) and a similar 7-week period from March 18, 2019, to May 6, 2019. Neurosurgical census data were analyzed and compared against system-wide COVID-19 hospitalization data. Neurosurgical and neurointerventional case data were analyzed with summary statistics. COVID-19 symptoms in residents and number of resident illnesses and lost workdays during quarantine periods were reported. For context, the resident deployment structure was reviewed.
Results
During the study period of 51 days, 72 operative neurosurgical cases and 69 neurointerventional procedures were performed at the 2 in-system hospital sites with direct resident participation and management. Mean (SD) patient age was 52 (20) years for operative interventions and 57 (20) years for neurointerventional procedures (Tables 1 and 2 ). Case volume decreased during the system-wide peak in COVID-19 hospitalizations and increased during the recovery. This case volume was decreased compared with 448 operations (decreased 83.9%) and 253 endovascular procedures (decreased 72.7%) from January 2020 to February 2020 and 530 operations (decreased 86.4%) and 340 endovascular procedures (decreased 79.7%) from March 2019 to May 2019 (Figure 2 ).
Table 1.
Characteristics of Open Neurosurgical Cases During the Peak Period of the COVID-19 Pandemic
| Characteristic | Surgeries (%) (n = 72) |
|---|---|
| Patient age, years, mean (SD) | 52 (±20) |
| Week | |
| 3/16–3/22 | 25 (34.7) |
| 3/23–3/29 | 12 (16.7) |
| 3/30–4/5 | 5 (6.9) |
| 4/6–4/12 | 4 (5.6) |
| 4/13–4/19 | 6 (8.3) |
| 4/20–4/26 | 3 (4.2) |
| 4/27–5/3 | 7 (9.7) |
| 5/4–5/5 | 10 (13.9) |
| Site | |
| Mount Sinai Hospital | 48 (66.7) |
| Mount Sinai West | 24 (33.3) |
| Type of operation | |
| CSF diversion | 8 (11.1) |
| Epilepsy | 2 (2.8) |
| Functional | 8 (11.1) |
| General neurosurgical | 4 (5.6) |
| Neuro-oncology | 12 (16.7) |
| Pediatric | 5 (6.9) |
| Skull base | 5 (6.9) |
| Spine | 13 (18.1) |
| Neurovascular | 10 (13.9) |
| Wound washout | 5 (6.9) |
| COVID-19 status | |
| Negative | 35 (48.6) |
| Positive | 10 (13.9) |
| Unknown | 27 (37.5) |
| Number of swabs, mean (SD) | 1.9 (±0.3) |
| Surgical emergency | 18 (25) |
| COVID-19 case volume | 72 |
| Case volume decrease, January–February 2020 | 83.9% |
| Case volume decrease, March–May 2019 | 86.4% |
COVID-19, 2019 novel coronavirus disease; CSF, cerebrospinal fluid.
Table 2.
Characteristics of Endovascular Neurosurgical Cases During the Peak Period of the COVID-19 Pandemic
| Characteristic | Procedures (%) (n = 69) |
|---|---|
| Patient age, years, mean (SD) | 57 (±20) |
| Week | |
| 3/16–3/22 | 8 (11.6) |
| 3/23–3/29 | 4 (5.8) |
| 3/30–4/5 | 10 (14.5) |
| 4/6–4/12 | 8 (11.6) |
| 4/13–4/19 | 5 (7.2) |
| 4/20–4/26 | 10 (14.5) |
| 4/27–5/3 | 21 (30.4) |
| 5/4–5/5 | 3 (4.3) |
| Site | |
| Mount Sinai Hospital | 64 (92.8) |
| Mount Sinai West | 5 (7.2) |
| Type of procedure | |
| Diagnostic | 19 (27.5) |
| Interventional | 50 (72.5) |
| Pathology | |
| Stroke | 20 (29) |
| Central retinal artery occlusion | 1 (1.4) |
| Subarachnoid hemorrhage | 10 (14.5) |
| Vasospasm | 10 (14.5) |
| Ruptured aneurysm | 2 (2.9) |
| Unruptured aneurysm | 3 (4.3) |
| Arteriovenous malformation | 5 (7.2) |
| Vein of Galen malformation | 1 (1.4) |
| Subdural hematoma | 6 (8.7) |
| Venous sinus thrombosis | 2 (2.9) |
| Moyamoya disease | 1 (1.4) |
| Vessel stenosis | 3 (4.3) |
| Tumor | 2 (2.9) |
| Compression fracture | 1 (1.4) |
| Epistaxis | 2 (2.9) |
| COVID-19 status | |
| Negative | 48 (69.6) |
| Positive | 15 (21.7) |
| Unknown | 6 (8.7) |
| Number of swabs, mean (SD) | 2 (±0) |
| Surgical emergency | 44 (63.8) |
| COVID-19 case volume | 69 |
| Case volume decrease, January–February 2020 | 72.7% |
| Case volume decrease, March–May 2019 | 79.7% |
COVID-19, 2019 novel coronavirus disease.
Figure 2.
Neurosurgical operations and endovascular procedures during March–May 2019, January–February 2020, and March–May 2020. Neuro-IR, neurointerventional radiology.
The most common categories of operative procedures were spine (18%), neuro-oncology (16.7%), neurovascular (13.9%), functional (11.1%), and cerebrospinal fluid diversion (11.1%). Most patients were COVID-19–negative (48.6%), confirmed with mean 1.9 swabs; 14% of patients were COVID-19–positive. The remainder were unknown (37.5%). Eighteen cases (25%) were treated as immediate surgical emergencies; all cases were considered urgent/nonelective.
Most endovascular procedures were interventions (72.5%), including thrombectomy for acute stroke (20.0%), lesional subarachnoid hemorrhage (14.5%), and arteriovenous malformation (7.2%). The majority of endovascular cases were considered immediate procedural emergencies (63.8%). Most patients were COVID-19–negative (69.6%), confirmed with mean 2.0 swabs.
Hospitalization patterns in the neurosurgical population correlated with system-wide COVID-19 admission status, with a corresponding peak in COVID-19–positive neurosurgical admissions. The overall neurosurgical census was initially decreased as COVID-19 admissions surged (Figure 3 ) but began steady growth as these patients recovered, and the overall COVID-19 admission rate decreased. The peak of neurosurgical COVID-19–positive ICU admissions coincided with the system-wide peak in admissions (Figure 3). COVID-19–negative ICU admissions decreased during the system-wide peak in COVID-19 admissions (Figure 3).
Figure 3.
Census of neurosurgical patients, COVID-19 intensive care unit neurosurgical patients, and total intensive care unit neurosurgical patients. COVID-19, 2019 novel coronavirus disease; ICU, intensive care unit.
Three residents became ill during the early period of the outbreak. One PGY-2 resident was quarantined for 6 days and returned to work with a negative COVID-19 polymerase chain reaction test, 1 PGY-6 resident quarantined for 11 days and returned to work after a negative polymerase chain reaction test, and 1 PGY-7 resident quarantined for 7 days and returned to work according to the system policy at the time (positive immunoglobulin G antibodies were later detected). A total of 24 days of work were missed (median 7 days). No residents required hospitalization.
Discussion
The SARS-CoV-2 pandemic has created unprecedented health care challenges. Despite COVID-19 pneumonia and associated syndromes accounting for the majority of hospital admissions during the period of evaluation, patients continued to present with acute ischemic stroke, aneurysmal subarachnoid hemorrhage, spinal cord compression/cauda equina syndrome, obstructive hydrocephalus, and other neurological emergencies.2 , 3 Balancing an appropriate commitment to the broader COVID-19 response effort, while preserving the ability to care for neurological patients, many of whom were also COVID-19–positive, is a challenge addressed by other authors in commentaries.4 , 5 We provide in this article the experience of 1 program in concrete numbers regarding redeployment needs, ongoing neurosurgical volume, and resident illness.
Case volume was substantially decreased compared with periods earlier in 2020 and during the 2019; however, a significant number of neurosurgical procedures were performed, with an average of 1.4 operative cases per day and 1.35 neuroendovascular cases per day. With a decrease in neurosurgery census to a median 24 patients during the COVID-19 outbreak, there was less of a workforce demand for residents, and during this time period the neurosurgery census was able to be maintained with 1 chief resident and 1 junior resident. This transition allowed for resident deployment to the COVID-19 ICU and the neurological ICU. Resident deployment allowed for around-the-clock available coverage of operative cases while adhering to work hour compliance and required guidelines. All graduating residents had satisfied case volume requirements well ahead of the COVID-19 pandemic. Three residents became ill. No residents required hospitalization. While a total of 24 days of work were missed, it is encouraging that no more severe illnesses occurred. System-wide data on hospital staff infection rates remain preliminary.
As has been described elsewhere, there was an increase in ischemic stroke volume commensurate with the COVID-19 outbreak, which affected both endovascular case volume and open operative intervention volume.3 In addition, our health system began to regularly perform systemic anticoagulation for patients with COVID-19 based on multiple published case series and recommendations from professional organizations.6, 7, 8 We saw multiple cases involving either primary intracerebral hemorrhage or hemorrhagic conversion of ischemic stroke, likely related to the use of systemic anticoagulation. The use of systemic anticoagulation in COVID-19 treatment has posed unique challenges for patients with neurological complications. It remains to be demonstrated whether the risk/benefit analysis clearly favors anticoagulation in COVID-19, but early data suggest it is reasonable.8
This study has several limitations. The analysis is descriptive and retrospective by nature. The experience at our large tertiary academic medical center is not necessarily generalizable to all centers.
Conclusions
During the height of the COVID-19 pandemic in New York City, we observed a 59.4% reduction in daily neurosurgical census over the study period and an 83.8% reduction in case volume compared with similar dates from March 2019 to May 2019. Despite this, our main hospital neurosurgical census was maintained at a median of 24 patients, and an average of 2.75 procedures (surgical and interventional) occurred per day. A total of 24 workdays were lost to illness among 3 of 14 residents. These data demonstrate the importance of maintaining a viable infrastructure to care for neurosurgical patients, even in the midst of one of the most intense COVID-19 epicenters. We hope this report will help other centers better estimate their needs and planned response should further infectious waves be encountered.
CRediT authorship contribution statement
Robert J. Rothrock: Conceptualization, Investigation, Writing - original draft, Formal analysis, Writing - review & editing. Georgios A. Maragkos: Investigation, Writing - original draft, Formal analysis, Writing - review & editing. Alexander J. Schupper: Investigation, Writing - original draft, Formal analysis, Writing - review & editing. Ian T. McNeill: Writing - original draft, Writing - review & editing. Eric K. Oermann: Writing - original draft, Writing - review & editing. Kurt A. Yaeger: Writing - original draft, Writing - review & editing. Jeffrey Gilligan: Writing - original draft, Writing - review & editing. Joshua B. Bederson: Supervision, Writing - review & editing. J.D. Mocco: Supervision, Writing - review & editing.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.New York State Department of Health Novel Coronavirus (COVID-19) https://coronavirus.health.ny.gov/home Available at:
- 2.Asadi-Pooya A.A., Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413:116832. doi: 10.1016/j.jns.2020.116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oxley T.J., Mocco J., Majidi S. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amin-Hanjani S., Bambakidis N.C., Barker F.G. Editorial. COVID-19 and neurosurgical practice: an interim report. https://doi.org/10.3171/2020.4.JNS201099 [e-pub ahead of print]. J Neurosurg. accessed May 29, 2020. [DOI] [PMC free article] [PubMed]
- 5.Carter B.S., Chiocca E.A. Editorial. COVID-19 and academic neurosurgery. https://doi.org/10.3171/2020.4.JNS201013 [e-pub ahead of print]. J Neurosurg. accessed May 29, 2020. [DOI] [PMC free article] [PubMed]
- 6.American College of Cardiology Thrombosis and COVID-19: FAQs for Current Practice. https://www.acc.org/latest-in-cardiology/articles/2020/04/17/14/42/thrombosis-and-coronavirus-disease-2019-covid-19-faqs-for-current-practice Available at:
- 7.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paranjpe I., Fuster V., Lala A. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76:122–124. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]