Abstract
The present study evaluated secondary emotional and behavioral outcomes among adolescents who received Prolonged Exposure (PE-A) or Client Centered Therapy (CCT) for posttraumatic stress disorder (PTSD) in a randomized controlled trial. Participants were 61 adolescent girls (age: M = 15.33; SD = 1.50) with sexual-abuse related PTSD seeking treatment at a community mental health clinic. Multilevel modeling was employed to evaluate group differences on the Youth Self-Report (YSR) over acute treatment and 12-month follow-up. Both treatment groups showed significant improvements on all YSR scales from baseline to 12-month follow-up. Adolescents who received PE-A showed significantly greater reductions than those receiving CCT on the Externalizing subscale (d = 0.70), rule breaking behavior (d = 0.63), aggressive behavior (d = 0.62), and conduct problems (d = 0.78). No treatment differences were found on the Internalizing subscale or among other YSR problem areas. Both PE-A and CCT effectively reduced many co-occurring problems among adolescents with PTSD. Although PE-A focuses on PTSD and not on disruptive behaviors, PE-A was associated with greater sustained changes in externalizing symptoms, supporting broad effects of trauma-focused treatment on associated problem areas.
Adolescent survivors of sexual abuse are at elevated risk for posttraumatic stress disorder (PTSD; Hanson et al., 2008), a chronic and disabling disorder characterized by intrusive reexperiencing symptoms, avoidance behaviors, elevated arousal, and changes in cognition and mood (American Psychiatric Association, 2013). In adults, PTSD is associated with a number of comorbid disorders and related difficulties, including depression, general anxiety, anger, and interpersonal problems (e.g., Brown et al., 2001; Kessler et al., 2005). Studies of PTSD comorbidity in adolescents generally replicate these findings. For example, in addition to depression and anxiety (e.g., Giaconia et al., 1995), adolescents with PTSD show higher rates of social difficulties, academic dysfunction, and conduct problems compared to age-matched controls (Bolten et al., 2004; Lipschitz, Rasmusson, Anyan, Cromwell, & Southwick, 2000; Mclean, Rosenbach, Capaldi, & Foa, 2013). Not only do these associated problems affect the clinical presentation of PTSD in adolescents, they may have a long-term negative impact on the adolescent’s developmental trajectory. Therefore, it is important that treatments aimed at reducing PTSD in adolescents also have an impact on co-occurring problems.
Randomized clinical trials (RCTs) support the efficacy of several cognitive behavioral therapies (e.g., trauma-focused cognitive behavioral therapy; group cognitive behavioral intervention for trauma in schools) in the reduction of PTSD symptoms for youth (See Silverman et al., 2008 for a review). When these studies have included measures of secondary problems, such as general anxiety, sexual concerns, externalizing symptoms, and functional impairment, they have generally shown significant reductions on these associated symptoms (e.g., Deblinger, Steer, & Lippmann, 1999; Jensen et al., 2014; Smith et al., 2007) and superior effects compared to non-directive supportive counseling (Cohen et al., 2004). The samples in these studies, however, are typically comprised of children exclusively, or a mixed child-adolescent sample, making it difficult to isolate the response of adolescents specifically. Adolescents and children are likely to have unique treatment needs based on their developmental stage, and are also likely to struggle with different associated problems. To our knowledge, there are only three studies that have examined the impact of PTSD treatment on associated problems specifically among adolescents. Of these, one was a pilot study evaluating the feasibility of an adapted version of cognitive processing therapy (Matulis et al., 2014), and another was a study of a cognitive behavioral group treatment (Sinclair et al., 1995). Both of these studies were uncontrolled, precluding strong conclusions about intervention effects. The third study compared Seeking Safety (Najavits, Gallop, & Weiss, 2006), a program for substance use and PTSD, to treatment–as-usual, finding that those who received Seeking Safety were less likely to meet criteria for a substance use disorder and reported fewer sexual concerns than those who received treatment-as-usual.
To date, only one RCT has examined the treatment of adolescents with sexual abuse-related PTSD. This study (Foa, McLean, Capaldi, & Rosenfield, 2013) evaluated the effects of prolonged exposure for adolescents (PE-A; Foa, Chrestman, & Gilboa-Schechtman, 2008) compared to client-centered therapy (CCT; Cohen & Mannarino, 1996) among adolescents with PTSD secondary to sexual abuse. PE-A is a form of cognitive behavioral therapy and was adapted from the widely studied and empirically supported adult treatment protocol (PE; Foa, Hembree, & Rothbaum, 2007). PE-A provides psychoeducation about the effects of trauma and then focuses on helping youth to systematically and repeatedly confront trauma-related memories (imaginal exposure) and reminders (in vivo exposure). The results of this trial showed that although both treatments were associated with significant reductions in symptoms, PE-A was superior to CCT in improving PTSD severity, depression, and clinician-rated overall functioning. The outcomes, however, of other problems co-occurring with PTSD were not examined. In particular, no outcomes were reported that focused on disruptive behaviors or conduct problems that may significantly impact academic and social functioning. The current study utilizes data from the Foa et al. (2013) study to address this gap by reporting the effects of the PE-A versus CCT on associated problems as measured by Youth Self-Report (YSR; Achenbach & Rescorla, 2001). The YSR assesses a range of behavioral and emotional problems in adolescents ages 11–18 years, and is a widely used and psychometrically validated measure that has been normed in a large nationally representative sample.
In adults, PE has been found effective in reducing many problems that co-occur with PTSD, including depression, anxiety, anger, interpersonal functioning, and physical health complaints (see McLean & Foa, 2014 for a review). As noted previously, studies with combined child-adolescent samples have demonstrated greater improvement in secondary internalizing and externalizing problems following trauma-focused cognitive behavioral therapy compared to non-directive supportive counseling or treatment as usual (Cohen et al., 2004; Deblinger et al., 1999; Jensen et al., 2014). Based on these findings, we hypothesized that patients receiving PE-A would show greater improvements in emotional and behavioral problems as measured by the YSR as compared to patients receiving CCT.
Method
Participants and Procedure
Participants were 61 adolescent girls aged 13–18 who participated in a RCT comparing PE and CCT (Foa et al., 2013). All participants sought treatment for PTSD at Women Organized Against Rape (WOAR), a community mental health clinic in Philadelphia that provides counseling to survivors of sexual abuse. Inclusion criteria were a primary diagnosis of PTSD based on the criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth edition, text revision (DSM-IV-TR; American Psychiatric Association, 2000) or subthreshold PTSD (≥1 reexperiencing symptom, ≥ 2 avoidance symptoms, and ≥ 2 hyperarousal symptoms) resulting from rape or attempted rape by same-age peers, or sexual abuse (by a perpetrator 5 or more years older) that occurred 3 months or more prior to intake. Approximately half of the sample (52.3%) reported repeated (2 or more) sexual assaults; 29.5% reported being sexually assaulted by a blood relative; and 19.6% percent endorsed chronic victimization defined as reporting sexual abuse occurring “more than 99” times. Adolescents who had initiated psychotropic medication within the previous 12 weeks and those with pervasive developmental disorder, unmanaged bipolar disorder, schizophrenia, conduct disorder, alcohol or substance dependence, or suicidal ideation with intent were excluded.
Mean patient age was 15.33 years. 55.7% of the sample identified as African American, 27.9% White, and 11.5% Hispanic. Fifty seven percent had at least one co-morbid Axis I diagnosis. The most common disorders were major depression disorder (MDD; 47.5%), obsessive compulsive disorder (16.4%), generalized anxiety disorder (14.8%), attention deficit hyperactivity disorder (8.2%), and specific phobia (8.2%). 11.5% were taking psychotropic medications.
The study was approved by the University of Pennsylvania institutional review board and the executive board of WOAR. Full details on patient flow through the study can be found in Foa et al. (2013) and Figure S1. Potential participants called WOAR’s 24-hour hotline and completed an initial screening with a WOAR counselor who assessed for sexual abuse and length of time since trauma (≥ 3 months). Adolescents who met these initial screening criteria and their non-offending primary guardian were invited to participate in a pretreatment assessment with a doctoral level clinical psychologist, who served as an independent evaluator (IE) blind to treatment condition. Participants and their primary guardian signed informed assent/consent forms and completed a 2–3 hour baseline evaluation comprised of a clinical interview to assess eligibility and self-report measures.
Eligible participants completed 1–3 pretreatment preparation sessions prior to randomization to address case management issues (e.g., confidentiality, risk assessment, legal issues, level of parental involvement, and motivation for treatment). After the pretreatment session(s), participants were randomized to PE-A (n = 31) or CCT (n = 30). The PE-A and CCT groups did not significantly differ in the number of pretreatment sessions received (p = .509). Participants in both conditions then received between eight and fourteen 60–90 minute sessions of PE-A or CCT (M = 12.0 for PE-A; M = 11.0 for CCT, p > 0.05). Treatment non-completion was defined as receiving less than eight sessions. In the PE-A condition, three participants (9.7%) were non-completers; In the CCT condition, five participants (16.6%) were non-completers.
Therapists
Both treatments in this study were provided by master’s level counselors (n = 4) employed at the rape crisis center trained to deliver PE-A and CCT. All therapists were female with a mean age of 29.4 years (range = 26–34). Three therapists reported a client- or person-centered orientation; one therapist reported an eclectic orientation. Mean years of therapy experience was 3.13 (range = 2.5 to 4.0).
Prior to the start of the study, counselors attended a 4-day training in PE-A conducted by Edna Foa and colleagues, as well as 4 days of training in CCT, conducted by Esther Deblinger and Judy Cohen. Therapists were required to successfully complete two cases of PE-A and two cases of CCT under intensive supervision before treating study participants. Therapists also received at least biweekly supervision throughout the trial. Adherence to prescribed components of the treatments was determined by randomly selecting 20.0% of the treatment sessions to be viewed by trained adherence raters. Adherence was 90.8% for PE-A and 90.5% for CCT.
Assessment
Blinded independent evaluations and completion of self-report measures took place at baseline, mid-treatment (following Session 7), posttreatment, and at 3-, 6-, and 12-months after completing treatment.
Measures
The Youth Self-Report (YSR; Achenbach & Rescorla, 2001), which is a companion form to the parent-report Child Behavior Checklist, has 105 problem items and 14 positive qualities items that are rated 0 = not true, 1 = somewhat or sometimes true, or 2 = very true or often true based on the preceding 6 months. Achenbach and Rescorla’s factor analyses yielded eight syndromes: Withdrawn/Depressed, Anxious/Depressed, and Somatic Complaints (all loading on a broad-band, second-order factor designated as Internalizing); Rule-Breaking Behavior and Aggressive Behavior (both loading on a broad-band, second-order factor designated as Externalizing); and Social Problems, Thought Problems, and Attention Problems (not loading differentially on either broad-band, second-order factor). Six DSM-oriented scales (Anxiety Problems, Affective Problems, Somatic Problems, Attention Deficit Hyperactivity Problems, Oppositional Defiant Problems, and Conduct Problems) comprise items identified by experts from 16 societies as consistent with diagnostic constructs from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013). The YSR also contains Obsessive-Compulsive and Posttraumatic Stress Problems scales (Achenbach & Rescorla, 2007). Achenbach and Rescorla (2001) reported excellent internal consistency (alphas of .90 to .97) for the Internalizing and Externalizing scales and adequate internal consistency (alphas of .72 to .97) for the syndrome and DSM-oriented scales. The measure also shows good test-retest reliability with test-retest coefficients ranging from .78 to .88 (Achenbach et al., 2003) and shows significant discrimination between children referred for mental health problems and demographically matched, non-referred children (Achenbach & Rescorla, 2001). The internal consistency of the scales in this measure in the current sample ranged from .48 to .90 (see supplementary Table S1). The DSM Anxiety Problems subscale had a low internal consistency (alpha of .48) and was subsequently removed from analyses.
Data Analysis
Multilevel modeling was used to investigate group differences in the YSR scales over time. The YSR was collected at five time points (baseline, posttreatment, 3-month follow-up, 6-month follow-up, and 12-month follow-up). First, we determined the best fitting shape of the growth trajectory over time (linear, quadratic, log, or hyperbolic) using maximum likelihood estimation and comparing different transformations of time using relative Akaike’s Information Criterion (AIC) and Schwarz’s Bayesian Criterion (BIC) indices, where smaller values indicate a better model fit (Heck, Thomas, & Tabata, 2014). Based on these models, all YSR scales were best fit with a hyperbolic transformation of time, which was thus used for subsequent analyses. Hyperbolic transformations of time are similar in shape to quadratic and log transformations and are, therefore, useful for modeling the steep declines in symptoms seen in many treatment studies.
Next, we determined the best fitting repeated measures error-covariance structure for each scale by testing model fit with −2 Log Likelihood (−2LL) fit values obtained using restricted maximum likelihood estimation and comparing them using a chi-square test. All error-covariance structures were compared to the unstructured model. For an in-depth description of the various error-covariance structures, see Garson (2013). The best fitting repeated measures error-covariance structures for each YSR scale were as follows: unstructured (Withdrawn Depressed, Aggressive Behavior, Internalizing, DSM Affective Problems, DSM Somatic Problems), Toeplitz heterogeneous (Attention Problems, Total Problems, DSM ADHD, Obsessive Compulsive Problems, Posttraumatic Stress Problems), Toeplitz homogeneous (Anxious Depressed, Social Problems, Thought Problems, Rule Breaking, Positive Qualities), autoregressive heterogeneous (Somatic Complaints), and autoregressive homogeneous (Externalizing, DSM ODD, DSM Conduct Problems).
Finally, we determined whether the model should include random effects for the intercept and time using restricted maximum likelihood estimation and −2LL. For the Anxious-Depressed, Somatic Complaints, Thought Problems, Attention Problems, Rule Breaking, Total Problems, DSM ADHD, Posttraumatic Stress Problems, and Positive Qualities scales, the model did not converge when random effects for the intercept and Time were included; therefore, only the random intercept for Time was included in these models. For the Externalizing scale, the model did not converge when random effects for the intercept and Time were included so only the random effect for the intercept was included in this model. For the Withdrawn-Depressed, Social Problems, Aggressive Behaviors, Internalizing, DSM Affective Problems, DSM Somatic Problems, and DSM Conduct Problems scales, the model did not converge when random effects for the intercept and Time were included, either together or separately; therefore, no random effects were included in these models. The DSM ODD, and Obsessive-Compulsive Problems scales included random effects for both the intercept and Time. Following model fitting, linear mixed models were used to fit a multilevel model with a treatment condition by time interaction used to investigate whether change over time in each YSR scale differed due to treatment condition (PE-A vs. CCT). False discovery rate (FDR) correction was used to correct for the possibility of inflated Type 1 errors; all p-values reported are FDR corrected for multiple comparisons.
The intent-to-treat sample was used for all analyses. Multilevel modeling is robust to missing data due to dropout and does not exclude cases with missing data at some time points; therefore, we did not conduct replacement or imputation of missing values. Data analyses were conducted using IBM SPSS Statistics program (version 22) using the linear mixed model procedures outlined in Heck, Thomas, and Tabata (2014) and Shek and Ma (2011).
Results
Baseline Differences Between Treatment Groups
To evaluate whether participants in the PE-A and CCT conditions showed differences in any the YSR scales prior to the initiation of treatment, we analyzed the main effect of treatment group with time centered at the baseline assessment. There were no treatment group differences on any YSR scales at baseline (all p-values ≥ .119). It should be noted, however, that pretreatment means were in the non-clinical range for all scales. For means and standard deviations at baseline, see supplemental Table S2.
Change in YSR Scales Over Time
Next, we examined whether there was a significant change in the YSR scales over time. In general, there was a significant decrease in all YSR scales from baseline to 12-month follow-up (all p-values ≤ .001), except for Positive Qualities, which significantly increased over the course of treatment (p = .007). See Table 1 for p-values for each scale. This suggests that, across treatment groups, there was a significant improvement in these symptoms during both the treatment and follow-up phases.
Table 1.
Change in YSR Scales Over Time (N=61)
| Variable | β | SE | t-value | df | p-value† |
|---|---|---|---|---|---|
| Anxious/depressed | −11.19 | 1.34 | −8.37 | 73.30 | < .001 |
| Withdrawn/depressed | −10.08 | 1.32 | −7.63 | 65.33 | < .001 |
| Somatic complaints | −9.49 | 1.63 | −5.83 | 51.80 | < .001 |
| Social problems | −6.92 | 1.20 | −5.75 | 155.86 | < .001 |
| Thought problems | −10.75 | 1.28 | −8.38 | 83.36 | < .001 |
| Attention problems | −7.52 | 1.16 | −6.49 | 51.59 | < .001 |
| Rule breaking | −4.25 | 1.25 | −3.40 | 78.27 | .001 |
| Aggressive behavior | −7.91 | 1.18 | −6.70 | 55.45 | < .001 |
| Internalizing | −11.42 | 1.38 | −8.30 | 57.60 | < .001 |
| Externalizing | −6.98 | 1.12 | −6.24 | 148.15 | < .001 |
| Total problems | −10.85 | 1.35 | −8.04 | 132.50 | < .001 |
| DSM affective problems | −12.47 | 1.32 | −9.43 | 54.85 | < .001 |
| DSM somatic problems | −6.08 | 1.45 | −4.19 | 57.83 | < .001 |
| DSM ADHD | −6.99 | 1.17 | −5.96 | 52.90 | < .001 |
| DSM ODD | −6.49 | 1.30 | −5.00 | 65.03 | < .001 |
| DSM conduct problems | −7.82 | 1.22 | −6.41 | 127.94 | < .001 |
| Obsessive-compulsive problems | −10.88 | 1.24 | −8.79 | 60.34 | < .001 |
| Posttraumatic stress problems | −12.81 | 1.28 | −10.04 | 48.75 | < .001 |
| Positive qualities | 3.58 | 1.29 | 2.78 | 77.83 | .007 |
Note.
p-values are corrected using the false discovery rate (FDR) correction; YSR = Youth Self Report; DSM = Diagnostic and Statistical Manual of Mental Disorders; ADHD = Attention deficit-hyperactivity disorder; ODD = Oppositional defiant disorder; SE = standard error; df = degrees of freedom.
Treatment Group Differences in Internalizing Problems
To evaluate group differences on reduction of internalizing problems, we analyzed time by treatment group interactions for the Internalizing broad-band scale, which consists of the Anxious/ Depressed, Withdrawn/Depressed, and Somatic Complaints scales. We also looked at group differences in the DSM Affective Problems, DSM Somatic Problems, Obsessive-Compulsive Problems, and Posttraumatic Stress Problems scales. No significant treatment group differences were found for any of the internalizing scales (p-values ≥ .067; see Table 2).
Table 2.
Treatment Group Differences in Change in YSR Scales Over Time (N=61)
| Variable | β | SE | t-value | df | p-value† |
|---|---|---|---|---|---|
| Anxious/depressed | 5.48 | 2.80 | 1.96 | 70.74 | .084 |
| Withdrawn/depressed | 3.38 | 2.83 | 1.19 | 54.19 | .264 |
| Somatic complaints | 7.06 | 3.20 | 2.21 | 42.93 | .070 |
| Social problems | 6.56 | 2.47 | 2.65 () | 137.21 | .030* |
| Thought problems | 5.10 | 2.72 | 1.88 | 81.83 | .092 |
| Attention problems | 5.03 | 2.35 | 2.14 | 45.66 | .070 |
| Rule breaking | 7.05 | 2.48 | 2.85 | 82.52 | .028* |
| Aggressive behavior | 6.22 | 2.25 | 2.77 | 51.17 | .030* |
| Internalizing | 6.37 | 2.72 | 2.34 | 51.94 | .066 |
| Externalizing | 6.41 | 2.24 | 2.87 | 142.11 | .028* |
| Total problems | 7.10 | 2.20 | 3.23 | 43.44 | .024* |
| DSM affective problems | 6.05 | 2.65 | 2.28 | 50.93 | .067 |
| DSM somatic problems | 6.10 | 2.89 | 2.11 | 52.83 | .070 |
| DSM ADHD | 4.90 | 2.34 | 2.09 | 46.92 | .070 |
| DSM ODD | 1.21 | 2.69 | 0.45 | 56.50 | .654 |
| DSM conduct problems | 10.26 | 2.24 | 4.58 | 85.82 | < .001* |
| Obsessive-compulsive problems | 3.90 | 2.48 | 1.57 | 54.74 | .154 |
| Posttraumatic stress problems | 3.88 | 2.52 | 1.54 | 45.82 | .154 |
| Positive qualities | −4.20 | 2.69 | −1.56 | 72.23 | .154 |
Note.
p-values are corrected using the false discovery rate (FDR) correction; YSR = Youth Self-Report; DSM = Diagnostic and Statistical Manual of Mental Disorders; ADHD = Attention deficit-hyperactivity disorder; ODD = Oppositional defiant disorder; SE = standard error; df = degrees of freedom.
Treatment Group Differences in Externalizing Problems
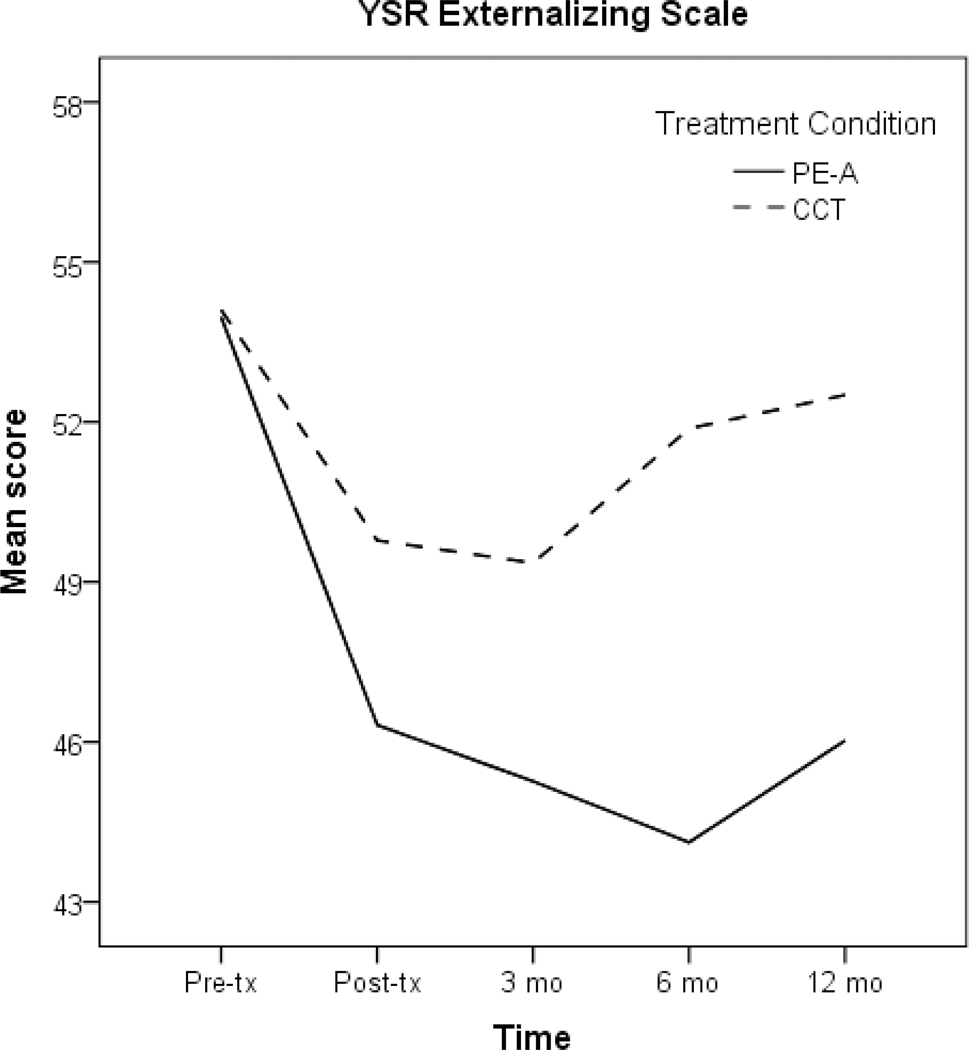
To evaluate group differences on reduction of externalizing problems, we analyzed time by treatment group interactions for the Externalizing broad-band scale, which consists of the Rule-Breaking Behavior and Aggressive Behavior scales. We also looked at group differences in the DSM Conduct Problems, Attention Problems, DSM ADHD, and DSM ODD scales. A significant group difference was found for the Externalizing scale (p = .028; see Table 2 for estimates and Table 3 for effect sizes), with greater reductions found in the PE-A group compared to CCT group. As seen in Figure 1, PE-A resulted in greater reductions in externalizing symptoms at posttreatment and at 3-, 6-, and 12-months follow-up (p-values ≤ .028). This group difference was significant for both the Rule-Breaking Behavior (p = .028) and Aggressive Behavior scales (p = .030) when analyzed separately.
Table 3.
Effect Sizes for the Difference between Groups at 12 Month Follow-Up
| PE-A (N = 28) | CCT (N = 27) | ||||
|---|---|---|---|---|---|
| Variable | M | SE | M | SE | d |
| Somatic complaints | 43.97 | 1.61 | 49.63 | 1.60 | 0.64 |
| Attention problems | 45.74 | 1.66 | 50.40 | 1.64 | 0.51 |
| Rule breaking | 47.13 | 1.75 | 53.21 | 1.73 | 0.63 |
| Aggressive behavior | 45.50 | 1.85 | 51.88 | 1.86 | 0.62 |
| Internalizing | 44.73 | 1.75 | 49.29 | 1.74 | 0.47 |
| Externalizing | 45.88 | 1.69 | 52.38 | 1.68 | 0.70 |
| Total problems | 44.58 | 1.68 | 50.47 | 1.66 | 0.64 |
| DSM affective problems | 43.61 | 1.80 | 48.41 | 1.78 | 0.49 |
| DSM conduct problems | 45.54 | 1.70 | 52.78 | 1.68 | 0.78 |
Note. PE-A = prolonged exposure therapy for adolescents; CCT = client centered therapy; DSM = Diagnostic and Statistical Manual of Mental Disorders; M = mean; SE = standard error; d = Cohen’s d calculated using the pooled standard deviation.
Figure 1.
Change over time in the Externalizing scale by treatment condition. PE-A = prolonged exposure therapy for adolescents; CCT = client centered therapy; Pre-tx = pretreatment; Post-tx = posttreatment; mo = months; N = 61.
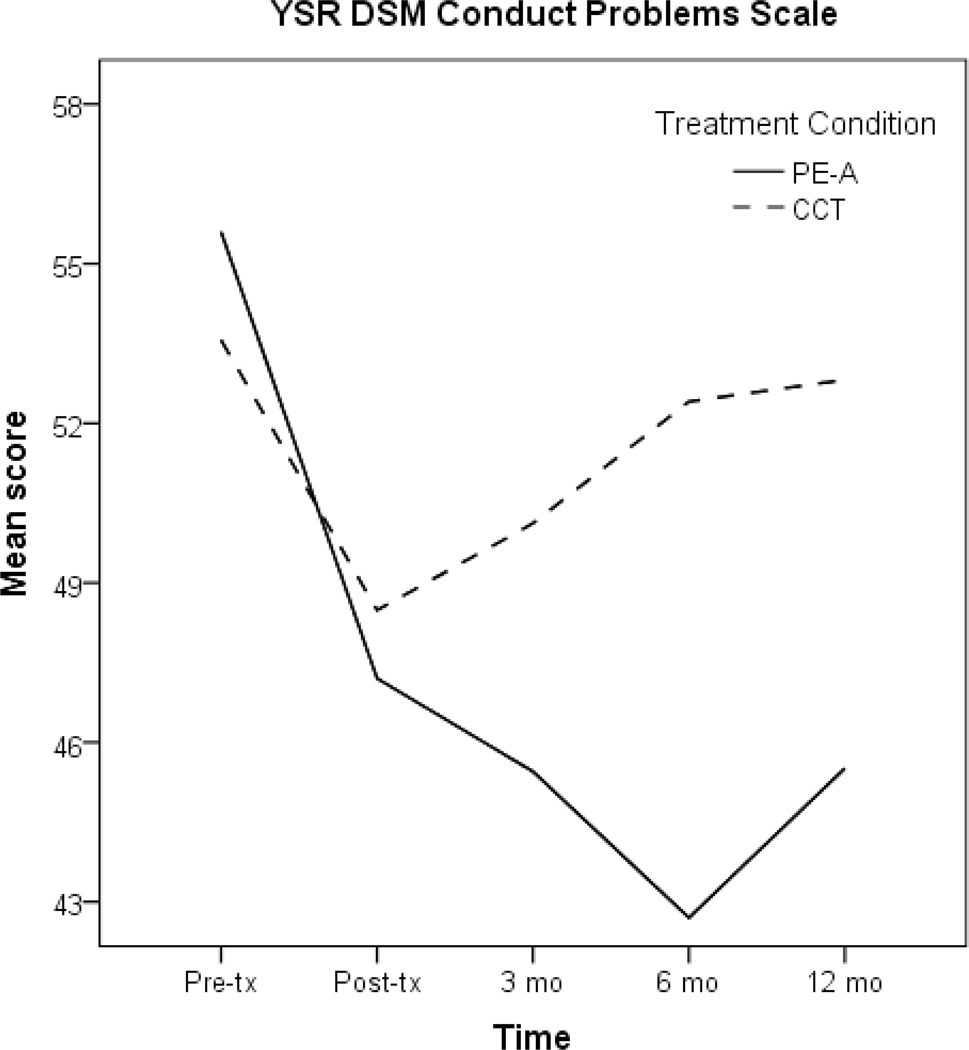
In addition, a significant group difference was found for DSM Conduct Problems (p < .001). PE-A resulted in greater reductions in Conduct Problems at posttreatment and 3-, 6-, and 12-month follow-up compared to CCT (p-values ≤ .028). Conversely, the CCT group showed an increase in DSM Conduct Problems over the follow-up period (see Figure 2). No significant group differences were found for the other externalizing scales (p ≥ .070).
Figure 2.
Change over time in the DSM Conduct Problems scale by treatment condition. PE-A = prolonged exposure therapy for adolescents; CCT = client centered therapy; Pre-tx = pretreatment; Post-tx = posttreatment; mo = months; N = 61.
Other YSR Scales
Finally, although the Social Problems scale showed a significant time by group interaction suggesting dissimilar growth curves between the groups (p = .030), examination of the group differences at each time point revealed only marginally significant differences (p-values ≥ .054). There were no significant group differences for the Thought Problems scale (p = .092) or the Positive Qualities scale (p = .154).
Discussion
The current study examined changes in co-occurring emotional and behavioral problems among adolescents with sexual abuse-related PTSD who received either PE-A or CCT. Both treatment groups showed significant improvements on all YSR scales from baseline to 12-month follow-up. As hypothesized, PE-A was associated with significantly greater reductions on the Externalizing scales of the YSR. Adolescents who received PE-A showed greater reductions in Rule Breaking Behavior, Aggressive Behavior, and Conduct Problems compared to those who received CCT, and these differences were associated with medium to large effect sizes. The superiority of PE-A over CCT was evident between pre- and posttreatment for some subscales (i.e., Rule Breaking and Conduct Problems), and during the follow-up phase for other subscales (i.e., Aggressive Behavior), where participants in CCT were more likely to demonstrate posttreatment increases in these problems. This latter finding highlights the importance of evaluating the durability of treatment effects among adolescents with PTSD after contact with the therapist has been discontinued.
While PE-A outperformed CCT in reducing several externalizing problems over time, contrary to hypotheses, both treatments showed similar impact on the Internalizing scales (Anxious/ Depressed, Withdrawn/Depressed, and Somatic Complaints), Thought Problems, Attention Problems, DSM Affective Problems, DSM Somatic Problems, DSM ADHD, DSM ODD, Obsessive Compulsive Problems, and Posttraumatic Stress Problems scales. These results are encouraging and suggest that, based on patient self-report, PE and CCT are both effective in reducing many problems that co-occur with PTSD.
The current finding that Posttraumatic Stress Problems and Withdrawn/Depressed scale scores did not significantly differ in PE-A versus CCT appears to conflict with the main outcome results (Foa et al., 2013), which demonstrated superiority of PE-A on the Child PTSD Symptom Scale–Interview (CPSS-I; Foa, Johnson, Feeny, & Treadwell, 2001; Gillihan, Aderka, Conklin, Capaldi, & Foa, 2013) and the Child Depression Inventory (Kovacs, 1985) relative to CCT. With respect to PTSD symptoms, there are meaningful differences between these assessment tools that likely account for discrepant results: First, the CPSS-I is a clinician-administered structured interview that was administered by evaluators blind to the patient’s treatment condition, while the YSR is a patient self-report measure. Second, the CPSS-I is a more comprehensive measure of PTS symptoms based on DSM-IV criteria. In contrast, the YSR PTSD problem scale is comprised of 14 pre-existing YSR items that other investigators had found associated with the experience of abuse among children and adolescents (e.g., trouble concentrating or paying attention, feeling nervous or tense, suddenly changing moods/feelings, etc.), and key symptoms related to PTSD (e.g., avoidance of memories and trauma-reminders) are not included in the subscale. Indeed, the Posttraumatic Stress Problems scale was recently renamed Stress Problems to reflect the fact that it is not strictly a PTSD measure (Achenbach, Rescorla, & Ivanova, 2015). For all the aforementioned reasons, the CPSS-I would generally be considered the more valid and reliable measure of PTSD. In contrast, with respect to depressive symptoms, the CDI and YSR scales are both patient self-report measures, both demonstrated adequate psychometrics, yet the two measures yielded a different pattern of findings.
Taken together, the main outcome paper and the current study suggest that PE-A and CCT are effective treatments that are both associated with significant reduction of co-occurring problems on the internalizing spectrum. The main outcome study shows superiority of PE-A in reducing PTSD symptoms using a gold-standard assessment method, and the current study suggests that PE-A was more effective than CCT in reducing secondary externalizing problems. Given the elevated rates of social and academic dysfunction common to adolescents with PTSD (Bolton et al., 2004; Lipschitz et al., 2000), the superior sustained effects of PE-A in several domains of externalizing problems (Rule Breaking Behavior, Aggressive Behavior, and Conduct Problems) is noteworthy, and may be particularly important in protecting youth from long-term negative effects of PTSD on academic and social functioning. Thus, overall, the evidence to date suggests that when possible, using a trauma-focused approach such at PE-A will maximize treatment benefits. Additional RCTs are needed to replicate these findings, and should include well-validated measures that assess both PTS symptoms and associated internalizing and externalizing problems.
Strengths of the current study include the randomized controlled design of the parent study and the provision of treatment in a community clinic, which enhances the external validity of the findings. Secondary problems were evaluated using a normed and widely used measure assessing a range of behavioral and emotional problems. In addition, the present study employed a sophisticated statistical approach that is robust to missing data and allowed for evaluation of treatment effects both during and up to 12 months following treatment.
Several limitations should be noted. First, pretreatment means of the YSR scales were in the nonclinical range, and as such, for many participants change on these scales reflected reductions further into the nonclinical or minimal range. Since the current sample was selected on the basis of elevated PTSD symptoms (and not based on presence of co-occurring emotional or behavioral problems), there was variability in the level of co-occurring symptoms at baseline. Given that more than half of the sample were diagnosed with co-morbid disorders based on clinical interview, it is possible that lower pretreatment means on the YSR reflect adolescent under-reporting on self-report measures. Pretreatment YSR scores on some scales (e.g., conduct problems) might have been restricted due to study exclusion criteria. Replications using larger and more varied adolescent samples (e.g., different trauma types and co-morbidities) are needed. Second, the current study is limited by reliance on youth self-report without corroborating assessments. Reliance of youth report in this investigation was based on the design of the study (which did not include parent-report on youth symptoms), and the predominance of adolescents at WOAR who presented for therapy and assessment appointments without a caregiver. When possible, future studies would benefit from examining parent or teacher perspectives on key aspects of patient mood and behavior, particularly externalizing symptoms.
Supplementary Material
Acknowledgments
This study was supported by the National Institute of Mental Health (R01 MH074505) PI: Edna Foa.
References
- Achenbach TM, Dumenci L, & Rescorla LA (2003). DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of Clinical Child and Adolescent Psychology, 32, 328–340. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Achenbach TM, Rescorla LA & Ivanova MY (2015). Guide to family assessment using the ASEBA Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Bolton D, Hill J, O’Ryan D, Udwin O, Boyle S, & Yule W (2004). Long-term effects of psychological trauma on psychosocial functioning. Journal Of Child Psychology, 45, 1007–1014. [DOI] [PubMed] [Google Scholar]
- Brown T, Campbell L, Lehman C, Grisham J, & Mancill R (2001). Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal Of Abnormal Psychology, 110, 585–599. 10.1037//0021-843X.110.4.585 [DOI] [PubMed] [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, & Steer R (2004). A multisite randomized controlled trial for multiply traumatized children with sexual abuse-related PTSD. Journal of the American Academy of Child and Adolescent Psychiatry, 29, 747–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, & Mannarino A (1996). Client-Centered Therapy Treatment Manual. Pittsburgh, PA: Hahnemann University School of Medicine. [Google Scholar]
- Deblinger E, Steer R, & Lippmann J (1999). Two-year follow-up study of cognitive behavioral therapy for sexually abused children suffering post-traumatic stress symptoms. Child Abuse & Neglect, 23, 1371–1378. 10.1016/s0145-2134(99)00091-5 [DOI] [PubMed] [Google Scholar]
- Foa E, Chrestman K, & Gilboa-Schechtman E (2009). Prolonged exposure therapy for adolescents with PTSD. Oxford: Oxford University Press. [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, & Treadwell KRH (2001). The child PTSD symptom scale (CPSS): A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology, 30, 376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Foa E, McLean C, Capaldi S, & Rosenfield D (2013). Prolonged exposure vs supportive counseling for sexual abuse related PTSD in adolescent girls. JAMA, 310(24), 2650 10.1001/jama.2013.282829 [DOI] [PubMed] [Google Scholar]
- Garson DG (2013). Hierarchical Linear Modeling: Guide and Applications. Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Gianconia R, Reinherz H, Silverman A, Pakiz B, Frost A, & Cohen E (1995). Traumas and posttraumatic stress disorder in a community population of older adolescents. Journal Of The American Academy Of Child & Adolescent Psychiatry, 34, 1369–1380. 10.1097/00004583-199510000-00023 [DOI] [PubMed] [Google Scholar]
- Gillihan SJ, Aderka IM, Conklin PH, Capaldi S, & Foa EB (2013). The child PTSD symptom scale: psychometric properties in female adolescent sexual assault survivors. Psychological Assessment, 25, 23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson R, Barntrager C, Self-Brown S, Kilpatrick D, Saunders B, Resnick H, & Amstadter A (2008). Relations among gender, violence exposure, and mental health: the national survey of adolescents. American Journal Of Orthopsychiatry, 78, 313–321. 10.1037/a0014056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck R, Thomas S, & Tabata L (2012). Multilevel modeling of categorical outcomes using IBM SPSS. New York: Routledge. [Google Scholar]
- Jensen T, Holt T, Ormhaug S, Egeland K, Granly L, & Hoaas L et al. (2014). A randomized effectiveness study comparing trauma-focused cognitive behavioral therapy with therapy as usual for youth. Journal Of Clinical Child & Adolescent Psychology, 43, 356–369. 10.1080/15374416.2013.822307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Chiu W, Demler O, & Waters E (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives Of General Psychiatry, 62, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M (1985). The Children’s Depression Inventory (CDI). Psychopharmacological Bulletin, 21, 995–998. [PubMed] [Google Scholar]
- Lipschitz D, Rasmusson A, Anyan W, Cromwell P, & Southwick S (2000). Clinical and functional correlates of posttraumatic stress disorder in urban adolescent girls at a primary care clinic. Journal Of The American Academy Of Child & Adolescent Psychiatry, 39, 1104–1111. 10.1097/00004583-200009000-00009 [DOI] [PubMed] [Google Scholar]
- Matulis S, Resick P, Rosner R, & Steil R (2013). Developmentally adapted cognitive processing therapy for adolescents suffering from posttraumatic stress disorder after childhood sexual or physical abuse: a pilot study. Clinical Child And Family Psychology Review, 17, 173–190. 10.1007/s10567-013-0156-9 [DOI] [PubMed] [Google Scholar]
- McLean CP, & Foa EB (2014). The use of prolonged exposure therapy to help patients with PTSD. Clinical Practice, 11, 233–241. doi: 10.2217/cpr.13.96 [DOI] [Google Scholar]
- McLean C, Rosenbach S, Capaldi S, & Foa E (2013). Social and academic functioning in adolescents with child sexual abuse-related PTSD. Child Abuse And Neglect, 37, 675–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits L, Gallop R, & Weiss R (2006). Seeking safety therapy for adolescent girls with PTSD and substance use disorder: a randomized controlled trial. The Journal Of Behavioral Health Services & Research, 33, 453–463. 10.1007/s11414-006-9034-2 [DOI] [PubMed] [Google Scholar]
- Rauch S, Grunfeld T, Yadin E, Cahill S, Hembree E, & Foa E (2009). Changes in reported physical health symptoms and social function with prolonged exposure therapy for chronic posttraumatic stress disorder. Depression And Anxiety, 26, 732–738. 10.1002/da.20518 [DOI] [PubMed] [Google Scholar]
- Shek D, & Ma C (2011). Longitudinal data analysis using linear mixed models in SPSS: Concepts procedures and illustrations. Scientific World Journal, 11, 42–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman W, Ortiz C, Viswesvaran C, Burns B, Kolko D, Putnam F, & Amaya-Jackson L (2008). Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal Of Clinical Child & Adolescent Psychology, 37, 156–183. 10.1080/15374410701818293 [DOI] [PubMed] [Google Scholar]
- Sinclair J, Larzelere R, Paine M, Jones P, Graham K, & Jones M (1995). Outcome of group treatment for sexually abused adolescent females living in a group home setting: preliminary findings. Journal Of Interpersonal Violence, 10, 533–542. 10.1177/088626095010004011 [DOI] [Google Scholar]
- Smith P, Yule W, Perrin S, Tranah T, Dalgleish T, & Clark D (2007). Cognitive-behavioral therapy for PTSD in children and adolescents: a preliminary randomized controlled trial. Journal Of The American Academy Of Child & Adolescent Psychiatry, 46, 1051–1061. 10.1097/chi.0b013e318067e288 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.