Abstract
COVID-19 is a global pandemic fuelled in some countries by government actions. The current issue of Clinical Kidney Journal presents 15 articles on COVID-19 and kidney disease from three continents, providing a global perspective of the impact of severe acute respiratory syndrome coronavirus 2 on electrolytes and different kidney compartments (glomeruli, tubules and vascular compartments) and presenting clinically as a syndrome of inappropriate antidiuretic hormone secretion, acute kidney injury, acute kidney disease, collapsing glomerulopathy and thrombotic microangiopathy, among others, in the context of a brand-new cardiorenal syndrome. Kidney injury may need acute dialysis that may overwhelm haemodialysis (HD) and haemofiltration capabilities. In this regard, acute peritoneal dialysis (PD) may be lifesaving. Additionally, pre-existent chronic kidney disease increases the risk of more severe COVID-19 complications. The impact of COVID-19 on PD and HD patients is also discussed, with emphasis on preventive measures. Finally, current therapeutic approaches and potential future therapeutic approaches undergoing clinical trials, such as complement targeting by eculizumab, are also presented.
Keywords: APOL1, acute kidney injury, cardiorenal, chronic kidney disease, COVID-19, Fanconi, haemodialysis, peritoneal dialysis, SIADH
We are in the midst of a global pandemic by the novel coronavirus evere acute respiratory syndrome coronavirus 2 (SARS-CoV-2). SARS-CoV-2 causes coronavirus 2019 (COVID-19), a disease first detected in Wuhan, China, at the end of 2019 [1]. On 30 January 2020, the Emergency Committee of the World Health Organization declared the outbreak a public health emergency of international concern [2]. Unfortunately, not all governments payed attention and the world is clearly divided between those countries whose governments took early appropriate measures to stop the expansion of SARS-CoV-2 and those who did not, and in some cases even contributed to expand the virus. The present issue of Clinical Kidney Journal (ckj) contains reports from the most affected countries (Figure 1) that illustrate the impact of SARS-CoV-2 on electrolytes and the kidneys, the different possibilities for acute renal replacement therapy (RRT) and the impact of COVID-19 in patients with pre-existing chronic kidney disease (CKD) and on chronic RRT, with emphasis on preventive measures and providing insights into therapy.
FIGURE 1.
Geographical origins of COVID-19 reports in the present issue of ckj.
ACTIVE CONTRIBUTION OF GOVERNMENTS TO EXPANSION OF THE PANDEMIC
The present issue would not exist if it not were for the actions and inactions of certain governments. This provides lessons for countries not yet affected and for future pandemics. Thus the distribution of the pandemic has not been even and government actions likely contributed to local extension. Italy was caught off-guard, but this cannot be said for other European governments. A case in point is Spain, currently the country with the most deaths per capita and whose capital city, Madrid, was recently surpassed by New York City as the city with the most deaths per capita (Figure 2). Despite further warnings on 2 March 2020 by the European Centres for Disease Prevention and Control on the moderate to high risk of transmission and impact of the disease [3], the Spanish government did not prepare for the epidemic, failed to limit public mass gatherings and astonishingly and actively promoted a large demonstration in Madrid on 8 March that was led by Deputy Prime Ministers Carmen Calvo and Nadia Calviño and by Ministers Irene Montero, Fernando Grande Marlaska, Isabel Celaá, Arancha González Laya and Carolina Darias. This attitude was associated with the insistence of the Public Health spokesman, Fernando Simon, on hand washing rather than masks to prevent disease transmission and his go-ahead for the large Madrid demonstration, reminiscent of the 1918 Philadelphia Liberty Loan demonstration experience, was enough to trigger the great Madrid tragedy. Hospitals were overwhelmed by COVID-19 patients and healthcare personnel were not provided with appropriate protective equipment, becoming one of the hardest hit communities (Figure 3). Spain was not alone in its disregard for basic public health principles. However, a different outcome was possible, as illustrated by Portugal, Germany, Poland and Greece, among others (Figure 2). One expected outcome of the current pandemic is the public discussion of government accountability, potentially extending to criminal charges, when they fail so blatantly to heed warnings by international public health officials, with such disastrous consequences.
FIGURE 2.
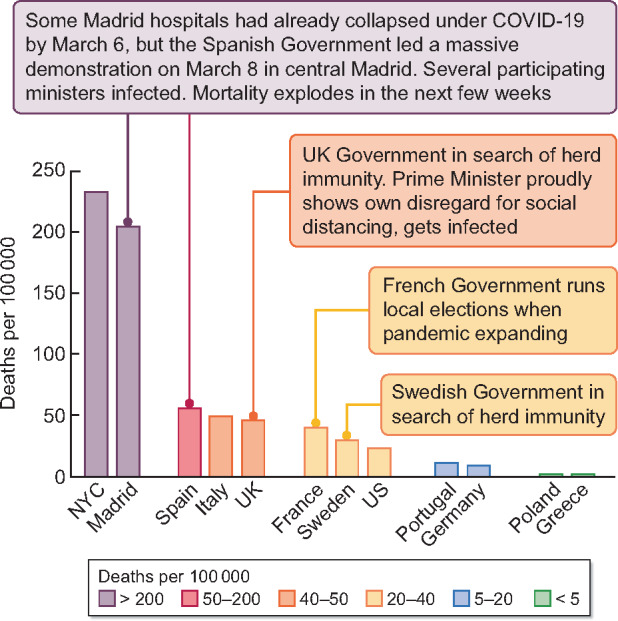
The contribution of governments to the expansion of the COVID-19 pandemic outside China. COVID-19 epidemiology cannot be understood without analysing government intervention. Contrary to citizens expectations, government intervention has sometimes contributed to expand the pandemic. Like China, Italy was caught off-guard. However, the Spanish government, after watching the Italian tragedy, not only failed to prepare the country for the pandemic but actively contributed to expand the disease. By 6 March 2020, Madrid hospitals were overwhelmed by COVID-19 and patients had to be moved to larger hospitals. What was the reaction of the government led by Pedro Sanchez? Promote a large demonstration on 8 March in Madrid. Government ministers spent days promoting the demonstration that they subsequently led. Several ministers became infected, one of them needing hospital admission. For weeks, the ministers had called for the 500 000 demonstrators of 2019 to show up again in 2020. Fortunately, a majority of Spanish citizens were actually paying attention to the news and ‘only’ 130 000 showed up. This was enough, on top of the usual weekend activity that the government did not prevent, to catapult Madrid to the worldwide top in terms of deaths per 100 000 persons, only recently surpassed by New York City (NYC). The government was fully aware of the danger and in the week preceeding 8 March, it had forbidden all meetings attended by medical doctors. Similar but milder patterns were repeated by other governments. France allowed local elections to proceed. Sweden and the UK were special cases, since health authorities purposely allowed the epidemic to expand to create ‘herd immunity’. In the UK this was done without making the necessary preparations for a large increase in the need for intensive care and healthcare personnel did not have access to appropriate protection in many instances. Prime Minister Johnson totally disregarded protective measures for himself and became infected. There is no need to comment on the unconventional US government intervention, as we have all seen it on the news. Despite last minute excuses by negligent governments, there was a different, successful approach around the pandemic, as illustrated by the low number of deaths in countries such as Germany, Portugal, Poland, Greece and others. Hopefully leaders of negligent governments will be prosecuted when the pandemic is over. For Madrid and NYC, all deaths included confirmed COVID-19 deaths at hospitals and suspected out-of-hospital deaths. Belgium is not shown, as they count all suspected COVID-19 deaths and those are not reported by other countries [45–48].
FIGURE 3.
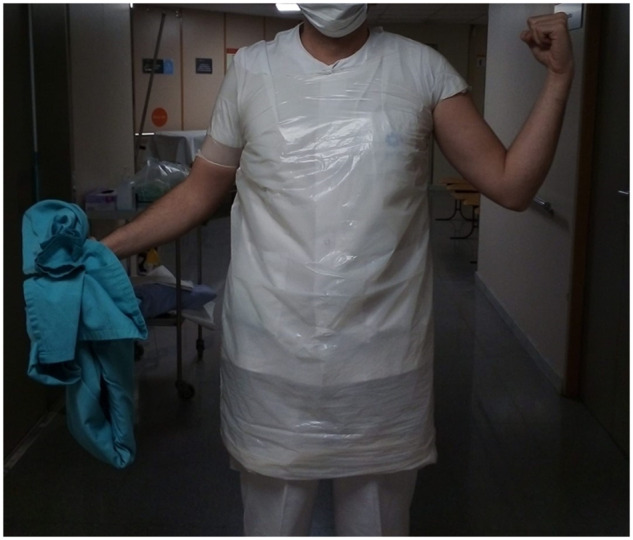
COVID-19 protection made from garbage bags in a Spanish hospital. In some hospitals, management provided garbage bags for staff, while in others, healthcare workers had to find their own garbage bags. As a consequence of the lack of enough and appropriate protective clothing or masks, Spain is among the countries with the most infected and dead healthcare personnel.
ELECTROLYTE ABNORMALITIES AND KIDNEY INJURY IN COVID-19
SARS-CoV-2 is best known for causing acute respiratory illness, with interstitial and alveolar pneumonia, but it can affect multiple organs and systems, including the cardiovascular system, gastrointestinal tract, blood, nervous system and kidneys [4]. Both viral infection and the ensuing inflammatory response contribute to the severity of disease and to mortality. Since kidney cells express receptors and enzymes required for viral entry, such as angiotensin-converting enzyme 2 (ACE2) and cellular transmembrane serine proteases [5, 6], direct renal cell infection is possible and is supported by some studies showing viral particles within proximal tubules and, less conclusively or reproducibly, in podocytes [7–9]. Additionally, in more severely affected patients, a hyperinflammation syndrome or cytokine storm contributes to tissue injury and is a therapeutic target independent from the virus [10, 11]. Inflammatory cytokines have long been known to induce acute kidney injury (AKI) and glomerulopathy [12, 13]. In severely affected COVID-19 patients, associated hypoxaemia, heart involvement (e.g. myocarditis, acute myocardial infarction, exacerbation of heart failure, shock and arrhythmia), cardiovascular instability and endothelial injury may also contribute to kidney injury in what is considered a brand new cardiorenal syndrome [14]. Thus, on top of direct virus infection, kidney injury may result from the systemic response to infection or from damage to other organs, and while it most commonly takes the form of AKI, other forms of kidney injury and electrolyte abnormalities have been described (Figure 4).
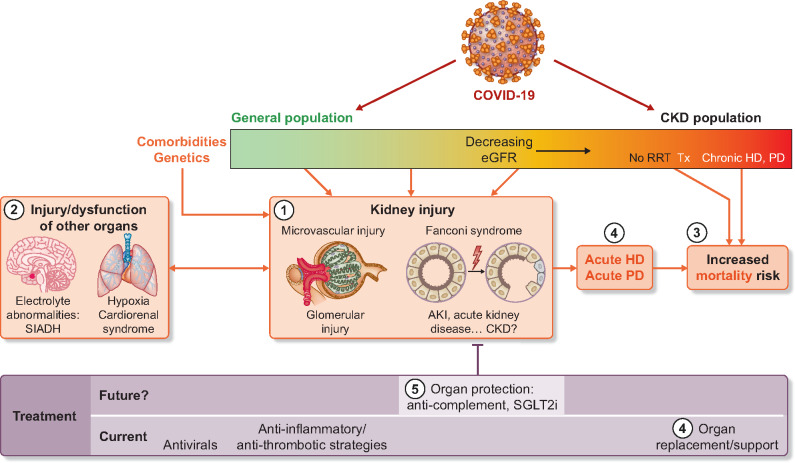
FIGURE 4.
COVID-19 and the nephrologist. The nephrologist is a key figure in COVID-19. (1) Both COVID-19 patients in the general population and those with prior CKD may develop COVID-19-associated kidney injury, which may adopt different forms. Thus tubular injury may initially only reflect proximal tubular injury (Fanconi syndrome) [17] but frequently evolves to AKI with a mainly tubulointerstitial pattern of injury [19, 20]. AKI may fail to resolve, leading to acute kidney disease and, potentially, to post-COVID-19 CKD, a possibility that requires prospective follow-up. However, thrombotic microangiopathy as well as glomerular injury have also been observed [30]. Both the genetic background and comorbidities may impact on the severity of COVID-19 and on the type and severity of COVID-19-associated kidney injury. As an example, persons of West African ancestry carrying APOL1 risk alleles may develop collapsing FSGS [8]. (2) Dysfunction or injury of other organs and systems may also cause complications that require nephrological consultation as well as negatively impact on kidney injury. Frequent examples are SIADH secretion causing hyponatraemia [15], lung disease–related hypoxaemia and inflammation aggravating AKI and heart disease causing a cardiorenal syndrome [14]. In fact, COVID-19-related kidney injury may also aggravate heart failure. (3) Both the development of kidney injury in the course of COVID-19 as well as pre-existent CKD not on dialysis or on RRT by kidney transplantation (Tx), HD or PD are associated with an increased risk of death [11, 43, 44]. Thus prevention strategies should be emphasized in HD patients and also in PD patients and kidney transplant programmes should be stopped at the peak of the pandemic [39–42, 49]. (4) Current therapy is multipronged, providing antiviral approaches together with anti-inflammatory and anti-thrombotic therapies to decrease the impact of overinflammation and prevent thrombotic complications. Finally, organ support or replacement (ventilator and dialysis) may be needed. RRT is most commonly offered by different HD or haemofiltration techniques, but in low-resource environments or when service providers are overwhelmed, acute PD is an alternative [38]. (5) However, the future lies in preventing lung, heart and kidney injury to avoid organ failure. Experimental tissue protective therapies undergoing clinical trials include anti-complement strategies (e.g. eculizumab) as well as the use of sodium–glucose cotransporter-2 inhibitors (SGLT2i), which are drugs that may protect the kidneys and heart in both diabetic and non-diabetic environments [30]. Some images are taken from https://commons.wikimedia.org/wiki/File: Kidney_Nephron_Cells.png; https://commons.wikimedia.org/wiki/File: Pituitary_gland_image.png and https://commons.wikimedia.org/wiki/File: Heart_%26_Lungs.png.
SYNDROME OF INAPPROPRIATE ANTIDIURETIC HORMONE
Hyponatraemia is common in COVID-19 patients and the cause appears to be outside the kidneys, as occurrence of the syndrome of inappropriate antidiuretic hormone (SIADH) has been well characterized by Ravioli et al. [15]. This observation is in line with previous experience with other forms of pneumonia, as hyponatraemia (serum sodium ≤130 mmol/L) was found in 8% of patients with community-acquired pneumonia, with nearly half of the cases having SIADH [16].
Fanconi syndrome
In accordance with ACE2 expression predominantly in proximal tubular cells and the finding of viral particles within these cells [5, 7], Kormann et al. [17] found that 75% (30/40) of hospitalized COVID-19 patients in France had at least two proximal tubule function abnormalities. Non-nephrotic proteinuria was found in 88% of patients and had a low urinary albumin content, as expected for tubular proteinuria, and renal phosphate wasting was found in 55%, hyperuricosuria in 43% and normoglycaemic glycosuria in 30%. Fanconi syndrome preceded severe AKI Kidney Disease: Improving Global Outcomes Stages 2 and 3 in 88% of AKI patients, but many patients did not developed AKI and improved over time.
AKI
The reported incidence of AKI has been very variable, likely depending on the severity of COVID-19 in the population studied. In any case, AKI is an independent predictor of COVID-19 in-hospital mortality [18].
Hong et al. [19] reported on 168 Chinese patients with a mean age of 47 years who had mainly mild to moderate COVID-19. On admission, proteinuria and haematuria were found in ~18% of patients and AKI was uncommon (<1%) and 1% of patients eventually required acute dialysis. However, proteinuria and haematuria were more common in and could predict severe or critical COVID-19. On the other side of the clinical spectrum, Rubin et al. [20] report on French intensive care units (ICUs), where the mean patient age was 61 years. Among ICU patients, 57/71 (80%) patients developed AKI during follow-up and 10/57 (18%) required RRT. Persistent AKI (for >72 h) was observed in 93% of patients and acute kidney disease (AKI persisting for >7 days) [21] was seen in 72% of patients. At Day 14, 48% still had acute kidney disease, raising the spectrum of potential post-COVID-19 CKD. Mean proteinuria and albuminuria:proteinuria ratios were consistent with tubulointerstitial injury. Haematuria and leucocyturia were present in 69 and 47%, respectively. These data expand on observations on albuminuria, haematuria and AKI and their association with in-hospital mortality [18].
It is striking the relatively high incidence of haematuria pro-tubular injury–associated AKI. In this regard, and as discussed above, several mechanisms may contribute to the development of AKI [22]. Initial histopathological data corresponding to post-mortem kidney biopsies disclosed mainly tubular injury [9].
Collapsing focal and segmental glomerulosclerosis
Collapsing focal segmental glomerulosclerosis (FSGS), similar to that found in human immunodeficiency virus (HIV)-infected patients, was also reported in patients with COVID-19 infection [8, 23]. Couturier et al. [8] describe two severe COVID-19 patients of African descent who developed AKI with proteinuria. Kidney biopsy showed collapsing FSGS and severe tubulo-interstitial lesions but no molecular expression of SARS-CoV-2. Both patients carried APOL1 risk alleles, similar to those associated with HIV-associated nephropathy [24], suggesting that as is the case for HIV, SARS-CoV-2 infection could act as a ‘second hit’ on a subclinical nephropathy.
A BRAND NEW CARDIORENAL SYNDROME
Both cardiovascular and renal involvement are prominent in severe COVID-19. The characteristics of this new cardiorenal syndrome are discussed by Apetrii et al. [14]. Myocardial injury, hypertension and therapy with renin–angiotensin system (RAS) blockers and the interaction with kidney disease are discussed. In this regard, high-sensitivity cardiac troponin I increases progressively in non-survivors [25]. Detailed management of the cardiorenal syndrome in COVID-19 patients emphasizes avoidance of volume overload, maintenance of blood pressure (mean arterial pressure >65 mmHg) and good oxygenation. The use of ACE inhibitors and angiotensin II receptor blockers was initially controversial, as they may increase ACE2 expression, the receptor for SARS-Cov-2 entry into cells. However, there is so far no evidence of deleterious effects of prior RAS blockade in COVID-19 patients and several societies have clearly recommended continuing RAS blockade in cardiovascular and kidney patients, including a position statement of the European Society of Cardiology Council on Hypertension and a joint statement from the American College of Cardiology, American Heart Association and Heart Failure Society of America [26, 27].
PROTHROMBOTIC STATE AND MICROVASCULAR INJURY
Closely linked to cardiovascular and kidney injury is evidence for endothelial injury and an associated prothrombotic state. Elevated d-dimer levels (>1 g/L) are strongly associated with in-hospital death in these patients [28]. In this regard, there is consensus that all hospitalized patients with COVID-19 should receive pharmacologic thromboprophylaxis with low molecular weight heparin [29].
Additionally, COVID-19 shares features with other microangiopathies such as thrombotic microangiopathy, disseminated intravascular coagulation and anti-phospholipid syndrome, as reviewed by Valga et al. [30]. In fact, some patients develop anti-phospholipid antibodies; there is evidence for endothelial cell injury, complement activation and deposition (of C5-b9, C4d and mannose-binding lectin-associated serin protease) and microthrombi, in addition to predisposition to arterial and venous thrombosis [4, 9, 31–36]. In addition to routine systemic anticoagulation, complement inhibition has been proposed as therapy and clinical trials are ongoing [30, 37].
RRT FOR COVID-19-ASSOCIATED AKI
AKI in the course of COVID-19 may require acute RRT. There is not yet evidence of the superiority of any specific form of RRT in COVID-19 patients. Continuous RRT techniques are most commonly used in the ICU setting. However, in many hospitals COVID-19 has overwhelmed facilities, far exceeding the capabilities to provide ICU care or certain acute RRT modalities. If no continuous therapy is available, intermittent haemodialysis (HD) is acceptable and peritoneal dialysis (PD) should be considered in selected patients. In this regard, Ponce et al. [38] provide an update on the potential use of acute PD in patients with COVID-19-related AKI without acute respiratory distress syndrome. They discuss detailed protocols and suggest initiating short and frequent cycles (high-volume PD or tidal PD) based on recent experiences from London, New Orleans and Perú.
COVID-19 AND CKD AND CHRONIC RRT
CKD patients are particularly susceptible to respiratory pathogens, probably related to the relatively suppressed immunity associated with uraemia and to frequent comorbidities such as hypertension, diabetes and even chronic obstructive pulmonary disease. Indeed, the risk for severe COVID-19 is 3-fold higher in CKD than in non-CKD patients; CKD is 12-fold more common in ICU patients than in non-hospitalized COVID-19 patients, and this ratio is higher than for diabetes or cardiovascular disease and is associated with COVID-19 mortality [11]. Within CKD, patients are at the highest risk because of more severe CKD-related immunosuppression, the use of immunosuppressants (e.g. transplantation) and the frequency of hospital visits. In this regard, the thrice-weekly visits of HD patients to dialysis centres or hospitals, which in some countries is by collective transport methods, enhance their risk of exposure to SARS-CoV-2. The ERA-EDTA Council published a key guidance document led by Mario Cozzolino on how to limit risk for both dialysis patients and healthcare personnel [39]. The present issue of ckj describes the clinical presentation of COVID-19 in Chinese and Italian dialysis patients and additionally describes in detail protective protocols to be applied to both HD units and PD facilities, including the creation of COVID-19 zones [40–42].
In Lazio (Italy), 16 COVID-19 patients were identified among 2245 HD patients from 32 centres and mortality was 50% [40]. In a further Italian single-centre study, Fontana et al. [43] described 15 patients (13 HD and 2 PD patients) positive for SARS-CoV-2 after testing patients who presented with symptoms or had contact with a confirmed case (37 of 306 HD patients). The mean age was 76 years and 13 required hospitalization. At presentation, most had interstitial infiltrates on chest X-ray, 75% had lymphocytopenia and none had respiratory insufficiency. However, during follow-up, 86% of patients received supplemental oxygen and the case fatality rate was 40% after a median of 5.5 days, mainly from respiratory failure related to COVID-19. This report emphasizes how apparently mild early disease may evolve to become life-threatening.
Wang et al. (Wuhan, China) [44] report on 7 of 202 HD patients diagnosed with COVID-19 at a mean age of 59 years, thus a different patient population from the Italian series. Computed tomography scan was used as a screening method for the whole HD population and bilateral ground-glass lung opacities and consolidation were the most common radiologic findings. Mortality was 43% and related to respiratory insufficiency and hyperkalaemia.
Overall, these reports highlight a high mortality from respiratory insufficiency in dialysis patients diagnosed with COVID-19 and partially contradict early reports of high mortality but not related to lung disease.
THE WAY FORWARD
Very active research is ongoing to better understand the pathogenesis and optimal therapeutic approach to COVID-19, including multiple clinical trials. These, together with the development of vaccines, will likely decrease the future impact of the disease. However, for the millions who have already been infected worldwide, including tens of thousands who survived ICU stays, a key future research item is whether acute COVID-19 leaves chronic sequalae to diverse organs, including the kidneys. The long-lasting episodes of AKI, fulfilling criteria for acute kidney disease, raise the spectrum of potential long-term impact on kidney function that will require protective studies. Regarding CKD patients and those on RRT, new guidelines to protect patients and healthcare personnel have been developed and should be frequently updated [50]. The occurrence of ‘silent’ COVID-19 infection in HD patients, estimated at 4.4% in a recent report [51], will make periodic screening of the full set of patients and healthcare personnel mandatory, as transmission from asymptomatic and pre-symptomatic individuals has contributed to expansion of the disease [52]. Additionally, any future drugs or vaccines will require additional studies in these populations regarding potential dose adjustments, drug interactions or response to vaccination and the eventual need for specific dosing recommendations for drugs and vaccines for patients with advanced CKD. Prevention and vaccines will be needed to safeguard the RRT population, which appears to be at exceptionally high risk of death once COVID-19 is diagnosed. Outcomes will likely be improved by massive screening of dialysis patients and early therapy approaches.
FUNDING
Sources of support include FIS/Fondos FEDER (PI18/01386, PI19/00588, PI19/00815), DTS18/00032, ERA-PerMed-JTC2018 (KIDNEY ATTACK AC18/00064 and PERSTIGAN AC18/00071, ISCIII-RETIC REDinREN RD016/0009), Sociedad Española de Nefrología, FRIAT, Comunidad de Madrid en Biomedicina B2017/BMD-3686 CIFRA2-CM.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Huang C, Wang Y, Li X. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO Timeline - COVID-19. https://www.who.int/news-room/detail/27-04-2020-who-timeline—-covid-19 (9 May 2020, date last accessed)
- 3.European Centres for Disease Prevention and Control. ECDC assessment of the COVID-19 situation in Europe as of 2 March 2020. https://www.ecdc.europa.eu/en/news-events/ecdc-assessment-covid-19-situation-europe-2-march-2020 (9 May 2020, date last accessed)
- 4. Wang D, Hu B, Hu C. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323: 1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Batlle D, Soler MJ, Sparks MA. et al. Acute kidney injury in COVID-19: emerging evidence of a distinct pathophysiology. J Am Soc Nephrol 2020; doi: 10.1681/ASN.2020040419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan XW, Xu D, Zhang H. et al. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: a study based on single-cell transcriptome analysis. I ntensive Care Med 2020. doi: 10.1007/s00134-020-06026-1. Online ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Farkash EA, Wilson AM, Jentzen JM.. Ultrastructural evidence for direct renal infection with SARS-CoV-2. J Am S oc Nephrol 2020; doi: 10.1681/ASN.2020040432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Couturier A, Ferlicot S, Chevalier K. et al. Indirect effects of SARS-CoV-2 on the kidney in COVID19 patients. Clin Kidney J 2020; 13: 347–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Su H, Yang M, Wan C, Yi LX. et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. K idney Int 2020; doi: 10.1016/j.kint.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shi Y, Wang Y, Shao C. et al. COVID-19 infection: the perspectives on immune responses. Cell Death Differ 2020; 27: 1451–1454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. D’Marco L, Puchades MJ, Romero-Parra M. et al. COVID-19 in chronic kidney disease. Clin Kidney J 2020; 13: 297–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. González-Cuadrado S, Lorz C, García del Moral R. et al. Agonistic anti-Fas antibodies induce glomerular cell apoptosis in mice in vivo. Kidney Int 1997; 51: 1739–1746 [DOI] [PubMed] [Google Scholar]
- 13. Sanz AB, Sanchez-Niño MD, Ortiz A.. TWEAK, a multifunctional cytokine in kidney injury. Kidney Int 2011; 80: 708–718 [DOI] [PubMed] [Google Scholar]
- 14. Apetrii M, Enache S, Siriopol D. et al. A brand-new cardiorenal syndrome in the COVID-19 setting. Clin Kidney J 2020; 13: 291–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ravioli S, Niebuhr N, Ruchti C. et al. The syndrome of inappropriate antidiuresis in COVID-19 pneumonia: report of two cases. Clin Kidney J 2020; 13: 461–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cuesta M, Slattery D, Goulden EL. et al. Hyponatraemia in patients with community-acquired pneumonia; prevalence and aetiology, and natural history of SIAD. Clin Endocrinol 2019; 90: 744–752 [DOI] [PubMed] [Google Scholar]
- 17.Kormann R, Jacquot A, Alla A et al Coronavirus disease 2019: acute Fanconi syndrome precedes acute kidney injury. Clin Kidney J 2020; 13: 362–370 [DOI] [PMC free article] [PubMed]
- 18. Cheng Y, Luo R, Wang K. et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int 2020; 97: 829–838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hong D, Long L, Wang AY. et al. Kidney manifestations of mild, moderate and severe coronavirus disease 2019: a retrospective cohort study. Clin Kidney J 2020; 13: 340–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rubin S, Orieux A, Prevel R. et al. Characterization of acute kidney injury in critically ill patients with severe coronavirus disease 2019. Clin Kidney J 2020; 13: 354–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chawla LS, Bellomo R, Bihorac A et al.. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 workgroup. Nat Rev Nephrol 2017; 13: 241–257 [DOI] [PubMed] [Google Scholar]
- 22. Naicker S, Yang CW, Hwang SJ. et al. The novel coronavirus 2019 epidemic and kidneys. Kidney Int 2020; 97: 824–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nasr SH, Kopp JB.. COVID-19-associated collapsing glomerulopathy: an emerging entity. Kidney Int Rep 2020; 5: 759–761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Campos P, Ortiz A, Soto K.. HIV and kidney diseases: 35 years of history and consequences. Clin Kidney J 2016; 9: 772–781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hu H, Ma F, Wei X. et al. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J 2020; doi: 10.1093/eurheartj/ehaa190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.European Society of Cardiology. Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang
- 27.American College of Cardiology. HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19 (6 May 2020, date last accessed)
- 28. Tang N, Li D, Wang X, Sun Z.. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020; 18: 844–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Society of Hematology. COVID-19 and VTE/Anticoagulation: Frequently Asked Questions. https://www.hematology.org/covid-19/covid-19-and-vte-anticoagulation (6 May 2020, date last accessed)
- 30. Valga F, Vega-Díaz N, Macia M. et al. Targeting complement in severe COVID-19 to address microthrombosis. Clin Kidney J 2020; 13: 477–479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhang Y, Xiao M, Zhang S. et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 2020; 382: e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Xu Z, Shi L, Wang Y. et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020; 8: 420–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tian S, Hu W, Niu L. et al. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol 2020; 15: 700–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Magro C, Mulvey JJ, Berlin D. et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res 2020; 220: 1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Campbell CM, Kahwash R.. Will complement inhibition be the new target in treating COVID-19 related systemic thrombosis? Cir culation 2020; 14: 1739–1741 [DOI] [PubMed] [Google Scholar]
- 36. Lippi G, Plebani M, Henry BM.. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta 2020; 506: 145–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Diurno F, Numis FG, Porta G. et al. Eculizumab treatment in patients with COVID-19: preliminary results from real life ASL Napoli 2 Nord experience. Eur Rev Med Pharmacol Sci 2020; 24: 4040–4047 [DOI] [PubMed] [Google Scholar]
- 38.Ponce D, Balbi A, Durand J et al. Is there room for peritoneal dialysis in the treatment of COVID-19-related AKI? Clin Kidney J 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cozzolino M. ERA-EDTA sharing Milan experience on coronavirus management in dialysis centres. Clin Kidney J 2020; doi: 10.1093/ckj/sfaa050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dominijanni S, Foniciello M, Tatangelo P. et al. Chronic kidney disease and SARS-CoV-2 outbreak: Lazio region organizational model. Clin Kidney J 2020; 13: 480–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Alfano G, Fontana F, Ferrari A. et al. Peritoneal dialysis in the time of COVID-19. Clin Kidney J 2020; 13: 265–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Yang Z, Dong J.. Operational considerations for peritoneal dialysis management during the COVID-19 pandemic. Clin Kidney J 2020; 13: 322–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fontana F, Giaroni F, Frisina M. et al. SARS-CoV-2 infection in dialysis patients in Northern Italy: a single-center experience. Clin Kidney J 2020; 13: 334–339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wang R, He H, Liao C. et al. Clinical outcomes of hemodialysis patients infected with severe acute respiratory syndrome coronavirus 2 and impact of proactive chest computed tomography scans. Clin Kidney J 2020; 13: 328–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.NYC Health. Coronavirus Disease 2019 (COVID-19) Daily Data Summary. https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-daily-data-summary-deaths-05062020-1.pdf (6 May 2020, date last accessed)
- 46.NYC Health. Confirmed and Probable COVID-19Deaths. Daily Report. https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-confirmed-probable-daily-05062020.pdf (6 May 2020, date last accessed)
- 47.Johns Hopkins University & Medicine Coronavirus Resource Center. COVID-19 Case Tracker. https://coronavirus.jhu.edu/ (6 May 2020, date last accessed)
- 48.Comunidad de Madrid. 2019-Nuevo Coronavirus. http://www.comunidad.madrid/servicios/salud/2019-nuevo-coronavirus#situacion-epidemiologica-actual (6 May 2020, date last accessed)
- 49. Akalin E, Azzi Y, Bartash R. et al. Covid-19 and kidney transplantation. N Engl J Med 2020; doi: 10.1056/NEJMc2011117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Basile C, Combe C, Pizzarelli F. et al. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres. Nephrol Dial Transplant 2020; 35: 737–741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rodrigo E, Piñera VC, Setién MA. et al. Silent COVID-19 in hemodialysis facilities in Cantabria, Spain: an ecological study. Clin Kidney J 2020; 13: 475–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gandhi M, Yokoe DS, Havlir DV.. Asymptomatic transmission, the Achilles’ Heel of current strategies to control Covid-19. N Engl J Med 2020; 382: 2158–2160 [DOI] [PMC free article] [PubMed] [Google Scholar]