Abstract
Background
Hemodialysis (HD) patients have high unemployment rates associated with higher mortality and poor quality of life. Changes in employment status prior to dialysis initiation may predict subsequent patient outcomes. We sought to examine US national trends in employment status prior to and at HD initiation, risk factors for job loss and their association with transplantation and mortality.
Methods
Employment was defined as working full-time or part-time for 496 989 patients initiating maintenance HD from 2006 to 2015. Associations between patient and dialysis facility characteristics and employment change were analyzed using multivariable logistic regression. Cox regression was used to assess job loss with mortality and transplantation.
Results
About 26% (n = 129 622) of patients were employed 6 months prior compared with 15% (n = 75 719) at HD initiation. Employment rates 6 months prior to HD initiation decreased from 29% in 2006 to 23% in 2014. Employed patients who maintained employment increased from 57% in 2006 to 64% in 2015. Patients who were older, female, Hispanic, Black, with more comorbidities or living in low-income zip codes were less likely to maintain employment. Facility characteristics associated with employment maintenance included nonprofit status, more stations, dialysis availability after 5 p.m. and home dialysis training. Patients maintaining employment during the 6 months prior to HD had lower mortality and higher transplantation rates than patients who became unemployed.
Conclusions
Employment rates among HD patients are low and employment changes common during the 6 months prior to HD. Maintaining employment status was associated with key patient and facility characteristics, kidney transplantation and survival.
Keywords: employment, hemodialysis, mortality, transplantation
INTRODUCTION
Employment is a key determinant of quality of life for hemodialysis (HD) patients [1, 2], who typically have reduced work ability compared with the general population [3]. Employment offers social support and improves patients’ lifestyle, financial status, quality of life and self-esteem [4, 5], whereas unemployment in working-age adults is associated with physical and psychological difficulties [6] and loss of self-esteem [7]. Maintenance of employment prevents loss of productivity and, from a societal perspective, is advantageous because it reduces disability expenditures. In the USA, between 11% and 31% [2, 8–10] of working-age dialysis patients are employed compared with 30% in Europe and 55% in Japan [11]. In the general population, mortality is four times higher among unemployed Americans than those who are employed [12]. Among HD patients, those with poor social adaptability (including unemployment) and self-rated poor health also had higher mortality risks [13, 14].
Most prior studies of HD patients’ employment have focused on changes after dialysis initiation. Little research has explored employment changes before and at HD initiation or the impact of employment changes on mortality. Here, we describe trends in employment changes during the last 6 months prior to and at HD initiation, over a decade (2006–15). Analyses examine risk factors for unemployment and associations between change in employment status and the outcomes of transplant and mortality in a national population of patients starting maintenance HD.
MATERIALS AND METHODS
Study design, population and data sources
We examined all 496 989 noninstitutionalized US patients aged 21–65 years, who started thrice weekly HD for the first time from 1 January 2006 to 31 December 2015. Patients who were institutionalized were excluded as they would have very limited ability for employment. Data on patient characteristics and employment status were obtained from the Centers for Medicare and Medicaid Services’ (CMS) End-Stage Renal Disease (ESRD) Medical Evidence Form (Form CMS-2728) [15]. Facility characteristics were obtained from the Dialysis Facility Compare database [16], death status from the CMS ESRD Death Notification (Form CMS-2746) [17], and transplantation between 2006 and 2015 from the Scientific Registry of Transplant Recipients database [18]. This study was performed under the United States Renal Data System (USRDS) Coordinating Center contract with the NIH-NIDDK; research as part of the contract has been approved by the University of Michigan Institutional Review Board (HUM0086162).
Exposures and outcomes
For each patient who met the inclusion criteria, we examined demographic variables (age, sex, ethnicity, race, health insurance and employment history 6 months prior to first HD and at first HD), pre-ESRD care, fistula as the initial vascular access and relevant clinical data (comorbid conditions and laboratory values). Facility characteristics included the percentage of patients with a catheter >90 days, using a fistula, hemoglobin (Hgb) <10 mg/dL, phosphorus >7 mg/dL, calcium >10.2 mg/dL, number of dialysis stations, availability of home HD or peritoneal dialysis (PD), incenter shifts beginning after 5 p.m. and for- profit status of the facility. Adjusted gross income (AGI) data for 2005 were obtained from the Internal Revenue Service and merged to the patient-level data by zip code as a proxy for income [19].
We defined employment as a full- or part-time job at 6 months prior to HD initiation and at HD initiation. A negative change in employment status was from full-time or part-time work at any level to unemployed. Among individuals aged 21–65 years, <8% of all new patients’ Forms CMS-2728 submitted were missing data on employment status 6 months prior to HD initiation. All patients with data for employment 6 months prior had complete data for employment status at HD initiation. Therefore, we excluded patients with missing data on employment 6 months prior to HD initiation.
Analytic methods
Data were expressed as counts and percentages for discrete variables or means and SDs for continuous variables. Comparisons were made by a Chi-square test for categorical variables. For normally distributed continuous variables and non-normally distributed continuous variables, we chose a t-test or a Mann–Whitney test, respectively. Logistic regression was used to examine the odds of job loss at the patient and facility level; the latter were clustered to account for correlations within a facility. Cox proportional hazards regression was employed to examine associations between employment loss and successful transplant or mortality, adjusted for age, gender, race, ethnicity, starting estimated glomerular filtration rate (eGFR), Hgb, nephrologist care, insurance, comorbidities and AGI. Patients were followed through 8 January 2016.
All analyses were performed using SAS 9.3 software [SAS Institute, Cary, NC, USA]. To account for the increased power due to the large sample size, statistical significance level was defined as P = 0.005.
RESULTS
Of the 496 989 noninstitutionalized first-time HD patients between 2006 and 2015, 129 622 (26.1%) were employed at 6 months prior to initiating HD (Table 1). Compared with patients who were unemployed at 6 months prior to HD, employed patients were younger (49.2 years versus 53.4 years), more often male (66.5% versus 56.4%), had fewer comorbid conditions and had a much higher prevalence of employer group health plan (EGHP) coverage (61.4% versus 16.1%) rather than Medicare (8.0% versus 39.6%) or Medicaid (0.6% versus 4.1%). Employed patients also lived in zip codes with higher average AGI levels ($47 100 versus $42 700 per annum). Race distributions were similar between employed and unemployed patients.
Table 1.
Baseline characteristics of the study population initiating HD in the USA (2005–14; N = 448 641) by employment status 6 months prior, and at start of maintenance HD
| Measure | Mean (SD) or percent |
|||
|---|---|---|---|---|
| 6 months before HD |
HD initiation |
|||
| Not employed (n = 367 367) | Employed (n = 129 622) | Became unemployed (n = 53 903) | Still employed (n = 75 719) | |
| Age (years) | 53.4 (9.9) | 49.2 (10.5) | 49.1 (10.7) | 49.3 (10.4) |
| Male (%) | 56.4 | 66.5 | 64.4 | 68.0 |
| Race (%) | ||||
| White | 58.8 | 58.8 | 57.4 | 60.1 |
| Black | 36.1 | 34.3 | 36.5 | 32.8 |
| Asian | 2.7 | 4.4 | 3.9 | 4.7 |
| Other/missing | 2.4 | 2.3 | 2.2 | 2.4 |
| Hispanic (%) | 16.7 | 15.9 | 18.8 | 13.9 |
| Hgb <10 g/dL (%) | 61.8 | 60.1 | 61.8 | 58.9 |
| Pre-ESRD care (%) | 49.9 | 55.1 | 47.3 | 60.7 |
| Fistula (%) | 14.4 | 15.8 | 10.3 | 19.7 |
| Comorbidities (%) | ||||
| Alcohol abuse | 2.9 | 1.8 | 2.4 | 1.3 |
| Amputation | 5.0 | 1.8 | 2.1 | 1.6 |
| ASHD | 14.3 | 8.8 | 9.3 | 8.5 |
| Cancer | 4.6 | 4.5 | 5.0 | 4.1 |
| CHF | 28.9 | 16.5 | 19.3 | 14.6 |
| COPD | 8.3 | 3.1 | 3.8 | 2.6 |
| CVA/TIA | 9.2 | 3.6 | 4.7 | 2.8 |
| DM | 62.3 | 46.1 | 47.4 | 45.1 |
| Drug abuse | 3.1 | 1.1 | 1.7 | 0.7 |
| HTN | 85.9 | 86.0 | 85.1 | 86.7 |
| Unable to ambulate | 6.6 | 1.6 | 2.7 | 0.8 |
| Needs assistance | 11.5 | 3.1 | 5.3 | 1.5 |
| None | 1.9 | 4.1 | 3.8 | 4.2 |
| Other cardiac disease | 14.6 | 9.4 | 10.4 | 8.7 |
| PVD | 11.8 | 5.7 | 6.3 | 5.2 |
| Toxic nephropathy | 0.5 | 0.5 | 0.6 | 0.4 |
| Smoking | 9.8 | 7.0 | 8.2 | 6.2 |
| Insurance (%) | ||||
| EGHP | 16.1 | 61.4 | 47.0 | 71.6 |
| Medicare | 39.6 | 8.0 | 10.1 | 6.5 |
| Medicare Advantage | 4.1 | 0.6 | 0.7 | 0.5 |
| Medicaid | 41.6 | 11.6 | 18.1 | 7.1 |
| None | 12.1 | 13.7 | 21.2 | 8.5 |
| Other | 12.6 | 10.8 | 10.2 | 11.2 |
| Average AGIa ($) | 42.7 (22.8) | 47.1 (28.2) | 44.5 (27.6) | 48.9 (28.4) |
AGI for zip code of residence (in thousands of US dollars).
ASHD, atherosclerotic heart disease; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; CVA/TIA, cerebrovascular disease; HTN, hypertension; PVD, peripheral vascular disease.
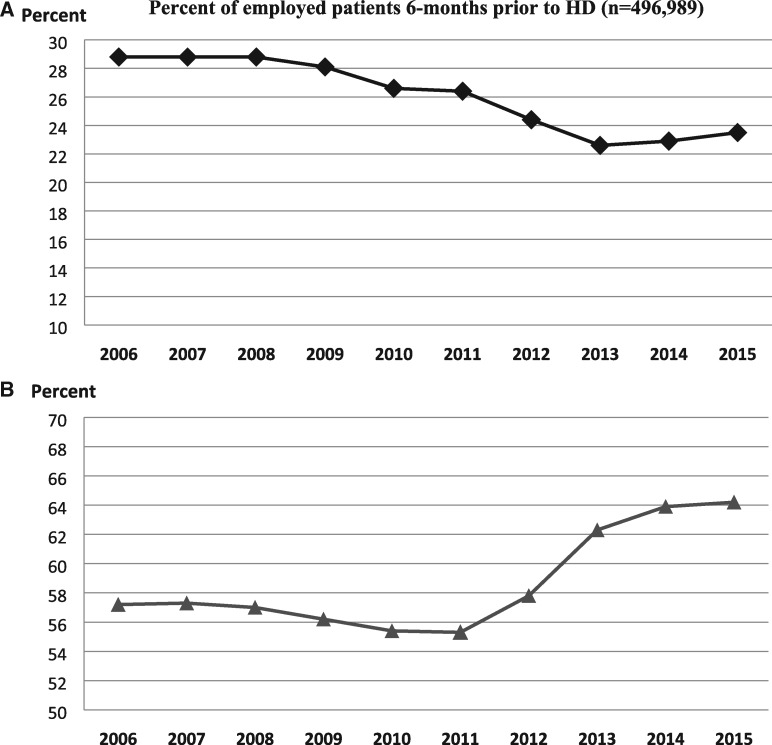
Over this 10-year period, employment at 6 months prior to HD declined significantly (Figure 1A). From 2006 to 2008, only 28.8% of new HD patients were employed 6 months prior to HD yet between 2008 and 2013, this figure was only 22.6%. From 2013 to 2015, employment 6 months prior to HD rebounded slightly, but at 23.5% was still nearly 5% lower than in 2006.
FIGURE 1.
Employment trends among patients initiating HD in the USA: 2006–15. (A) Percentage of employed patients 6 months prior to HD (n =496 989). (B) Percentage of patients who maintained employment at start of HD (among patients employed at 6 months prior to HD, n =129 622).
Among patients who remained employed from 6 months prior until HD initiation, we observed the opposite trend (Figure 1B). In 2006, 57.2% of new HD patients had maintained employment from 6 months prior to HD initiation; in 2011, this had declined to 55.3%. Starting in 2011, there was an increase to 64% of working patients who maintained employment during the last 6 months prior to first HD. The odds ratio (OR) of becoming unemployed was significantly higher from years 2006 to 2012 compared with 2015 (P < 0.0001), but then was not significantly different for 2013 (OR = 1.06) and 2014 (OR = 1.00) versus 2015 (Table 2).
Table 2.
Association between years of HD initiation with becoming unemployed at start of HD
| Measure | Unadjusted |
Adjusteda |
||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Year | ||||
| 2006 | 1.34 (1.28–1.41) | <0.0001 | 1.41 (1.33–1.48) | <0.0001 |
| 2007 | 1.34 (1.28–1.41) | <0.0001 | 1.37 (1.29–1.44) | <0.0001 |
| 2008 | 1.36 (1.29–1.43) | <0.0001 | 1.36 (1.29–1.43) | <0.0001 |
| 2009 | 1.40 (1.33–1.47) | <0.0001 | 1.39 (1.32–1.47) | <0.0001 |
| 2010 | 1.45 (1.38–1.52) | <0.0001 | 1.42 (1.35–1.50) | <0.0001 |
| 2011 | 1.45 (1.38–1.53) | <0.0001 | 1.44 (1.36–1.52) | <0.0001 |
| 2012 | 1.31 (1.25–1.38) | <0.0001 | 1.28 (1.21–1.35) | <0.0001 |
| 2013 | 1.09 (1.03–1.15) | 0.002 | 1.06 (1.00–1.12) | 0.06 |
| 2014 | 1.02 (0.96–1.07) | 0.59 | 1.01 (0.95–1.07) | 0.78 |
| 2015 | 1.00 | Reference | 1.00 | Reference |
Adjusted for variables in Table 1.
The OR of job loss during the last 6 months prior to HD initiation was higher for patients who were 44–65 years old, female, Hispanic, Black, those without EGHP insurance, and those with comorbidities of congestive heart failure, chronic obstructive pulmonary diseases, cerebrovascular disease, diabetes or other chronic illnesses (Table 3). The odds of job loss was lower for patients living in zip codes with higher AGI (OR = 0.96 for each higher $10 000 average AGI, P < 0.0001).
Table 3.
Association of patient characteristics with becoming unemployed at start of HD
| Measure | OR (95% CI) | P-value |
|---|---|---|
| Age at incidence (versus 44–65), years | ||
| <25 | 0.92 (0.84–1.00) | 0.68 |
| 25–44 | 0.88 (0.85–0.90) | 0.0004 |
| Male (versus female) | 0.85 (0.82–0.87) | <0.0001 |
| Race (versus White) | ||
| Black | 1.20 (1.17–1.23) | <0.0001 |
| Asian | 1.06 (0.99–1.12) | 0.08 |
| Other | 0.99 (0.92–1.07) | 0.80 |
| Hispanic (versus non-Hispanic) | 1.33 (1.28–1.38) | <0.0001 |
| Nephrologist care (yes versus no) | 0.76 (0.74–0.78) | <0.0001 |
| Fistula (yes versus no) | 0.62 (0.59–0.64) | <0.0001 |
| GFR (CKD-EPI, per 10 mL/min/1.73 m2 lower) | 1.21 (1.18–1.24) | <0.0001 |
| Hgb <10 (versus >10 g/dL) | 1.04 (1.01–1.06) | 0.01 |
| Insurance type (versus EGHP) | ||
| Medicare | 1.63 (1.56–1.71) | <0.0001 |
| Medicare Advantage | 1.44 (1.24–1.68) | <0.0001 |
| Medicaid | 3.29 (3.17–3.42) | <0.0001 |
| None | 3.32 (3.20–3.44) | <0.0001 |
| Other | 1.25 (1.20–1.30) | <0.0001 |
| Comorbidities (versus none) | ||
| Alcohol abuse | 1.35 (1.23–1.48) | <0.0001 |
| Cancer | 1.38 (1.30–1.46) | <0.0001 |
| CHF | 1.18 (1.14–1.22) | <0.0001 |
| ASHD | 1.02 (0.97–1.06) | 0.46 |
| COPD | 1.22 (1.13–1.30) | <0.0001 |
| CVA/TIA | 1.47 (1.38–1.57) | <0.0001 |
| DM | 1.09 (1.06–1.12) | <0.0001 |
| HTN | 0.91 (0.87–0.95) | <0.0001 |
| Drug abuse | 1.35 (1.20–1.51) | <0.0001 |
| Need assistance with daily activities | 2.34 (2.16–2.54) | <0.0001 |
| Unable to ambulate | 1.56 (1.39–1.74) | <0.0001 |
| PVD | 1.05 (0.99–1.11) | 0.08 |
| Smoking | 1.12 (1.06–1.17) | <0.0001 |
| Number of comorbidities (per 1) | 1.15 (1.14–1.16) | <0.0001 |
| Average AGI (per 10K)a | 0.96 (0.95–0.97) | <0.0001 |
CHF, congestive heart failure; ASHD, atherosclerotic heart disease; COPD, chronic obstructive pulmonary diseases; CVA/TIA, cerebrovascular disease; HTN, hypertension; PVD, peripheral vascular disease; eGFR, estimated glomerular filtration rate.
Average AGI for zip code of residence (in thousands of US dollars).
Patients were less likely to be become unemployed during the 6 months prior to HD initiation when their dialysis facilities offered a shift starting after 5 p.m. [OR = 0.76; 95% confidence interval (CI) 0.73–0.80], home HD training (OR = 0.92; 95% CI 0.88–0.97), PD training (OR = 0.94; 95% CI 0.90–0.98; all P < 0.0002) or had more dialysis stations (OR = 0.96; 95% CI 0.94–0.99; P = 0.002; Table 4). Conversely, patients who started HD in for-profit (FP) facilities had a higher odds of becoming unemployed before HD initiation (OR = 1.11; 95% CI 1.04–1.18; P = 0.002).
Table 4.
Association of facility characteristics with becoming unemployed a
| Measure | Prevalence or Mean (SD) (n = 6450) | OR (95% CI) | P-value |
|---|---|---|---|
| Late shift starting after 5 p.m. (yes versus no) | 17.7% | 0.76 (0.73–0.80) | <0.0001 |
| Offers home HD training (yes versus no) | 28.4% | 0.92 (0.88–0.97) | 0.0006 |
| Offers PD (yes versus no) | 51.3% | 0.94 (0.90–0.98) | 0.002 |
| Number of dialysis stations (per 10 stations) | 17.6 (8.5) | 0.96 (0.94–0.99) | 0.002 |
| FP (versus NFP) | 86.3% | 1.11 (1.04–1.18) | 0.002 |
Model is patient-level and adjusted for all variables in Table 1.
Compared with those who maintained employment from 6 months prior to dialysis initiation, patients who became unemployed during the 6 months prior to HD had a higher death rate [unadjusted hazard ratio (HR) = 1.19; 95% CI 1.16–1.21; P < 0.0001], which remained significant after adjustment for multiple co-variables (OR = 1.11; 95% CI 1.08–1.3; P < 0.0001; Figure 2). Conversely, those who continued to work were more likely to receive a transplant after adjustment (OR = 1.25; 95% CI 1.15–1.37; P < 0.0001; Figure 3).
FIGURE 2.
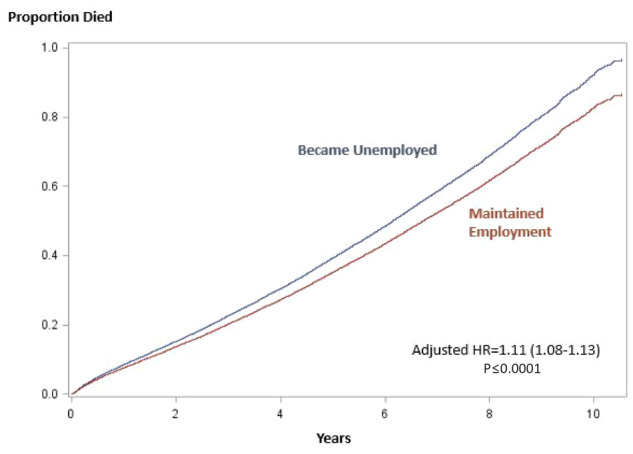
Adjusted cumulative incidence of mortality by loss of employment status. Adjusted for age, gender, race, ethnicity, starting eGFR, Hgb, nephrologist care, fistula as initial vascular access, insurance and comorbidities.
FIGURE 3.
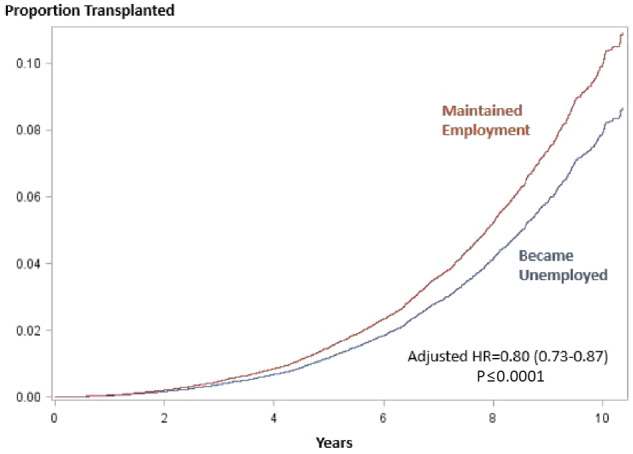
Adjusted cumulative incidence of transplantation by loss of employment status. Adjusted for age, gender, race, ethnicity, starting eGFR, Hgb, nephrologist care, fistula as initial vascular access, insurance and comorbidities.
DISCUSSION
This study had three main findings: first, the rate of employment 6 months prior to HD was stable at 29% from 2006 to 2008, then declined to 23% by 2014. Second, patients who were older, female, Hispanic, Black, with more comorbidities or living in a zip code with lower income were less likely to maintain employment, and facility characteristics that were associated with patient employment were availability of dialysis shifts after 5 p.m., home dialysis training and more stations. Third, maintained employment during the final 6 months prior to HD was a protective factor against mortality and showed higher rates of transplantation.
HD patients have impaired physical and mental functioning and tend to have low employment rates [20–22]. Employment loss affects social functioning, self-esteem [23], health-related quality of life [24] and financial status [25]. The cost to society is high as well.
Although employment loss often occurs after dialysis begins, many of those with chronic kidney disease (CKD) become unemployed earlier. In our study, no more than 29% of patients aged 21–65 years were working 6 months prior to HD, compared with 60.2% of those in the US general population in the same age group [26]. In this study, 35–43% of patients who were employed 6 months prior to HD had lost their jobs by HD initiation. This study shows that by 2011 more CKD patients had stopped working earlier than 6 months before HD—yet that same year, a growing number of CKD patients who had been employed 6 months prior to HD were still working at HD initiation.
In this study, patients who were female, Hispanic and Black were more likely to become unemployed before HD, characteristics that closely overlap with socioeconomic status [27]. Patients aged 25–44 years when starting HD were most likely to maintain employment; those who initiated HD at the age of ≥45 years more likely to have stopped working. Similar findings were reported among patients in the USRDS database from 1992 to 2003 [28]. Thus, nonmodifiable demographic or other unmeasured factors may be predictors of higher rates of unemployment.
We found that patients who had EGHP coverage were more likely to be employed during the 6 months prior to HD than those with Medicare, Medicare Advantage or Medicaid coverage, and others have reported similar findings [29, 30], likely because CKD patients aged <65 years and not otherwise disabled do not qualify for Medicare or Medicare Advantage; adults aged <65 years can only obtain Medicaid if they have very low income and/or are deemed to be too disabled to work [30]. Working-age patients with EGHP coverage may be motivated to maintain employment to keep their health insurance. Patients living in zip codes with higher average AGI were less likely to be unemployed, according to our results. It is possible that patients living in more affluent zip codes may be better educated, care more about their health conditions, and have higher self-esteem. On the contrary, working patients with higher incomes may be more motivated to keep working to maintain their standard of living.
New HD patients in our study who were employed were more likely to have been under a nephrologist’s care prior to HD (55.1%) than those who were unemployed (49.9%). Those who did not see a nephrologist prior to HD had a 1.5 times higher odds of job loss during the 6 months prior to first HD. The likelihood of seeing a nephrologist has been shown to depend on health insurance and socioeconomic characteristics (poverty rate, educate level, race, etc.) [31]. Receiving a nephrologist’s care may confer benefits such as better management of comorbidities (with counseling about lifestyle, blood pressure control, glycemic control, cardiovascular disease management—e.g. use of appropriate cardioprotective drugs), and complications such as anemia with appropriate use of erythropoietin or iron and better Hgb levels that make continued work more possible, superior management of volume status or heart failure, etc. Nephrologists are also likely to facilitate better vascular access planning before HD initiation. In this study, patients with Hgb <10 g/dL had significantly higher odds of job loss than patients with Hgb ≥10 g/dL (OR = 1.07; 95% CI 1.04–1.09; P < 0.0001). An A-V fistula is recommended by KDOQI as the first choice for vascular access when possible, when patients initiate HD. Vascular access type at initiation of HD is associated with patients’ mortality [32] and quality of life [33], so it is not unexpected that we find that individuals who begin dialysis with an A-V fistula were more likely to have maintained employment.
In this study, lifestyle behaviors such as abuse of alcohol or drugs and smoking were risk factors for job loss, as were certain comorbidities; patients with diabetes mellitus (DM) had higher odds of becoming unemployed whether treated with insulin, oral medicine or not treated at all. Not surprisingly, each additional comorbid condition was associated with a 15% higher likelihood of job loss during the final 6 months prior to first HD.
Several studies have found that ‘work-friendly’ treatments help patients maintain employment [34–36]. Patients who chose facilities where PD and/or home HD was offered were more likely to be still working at the same level when starting dialysis [3, 37]. Patients who want to work may be more likely to seek out and choose a dialysis facility that offers PD and/or home HD [2, 34] because these options are work-friendly. Although this study excluded PD patients, schedule flexibility and options for treatment did matter. For example, patients who started HD in facilities that offered shifts starting after 5 p.m. were more likely to be working at their first HD. New patients who were working were significantly more likely to dialyze in facilities that offered training for PD or home HD.
HD unit profit status was also associated with employment status. Patients in FP units had a higher odds of becoming unemployed than those in not-for-profit (NFP) units, an unexpected result, when FP units are well aware of their reliance on a favorable ‘payer mix’ of EGHP coverage versus Medicare or Medicaid to drive profits and stay in business. Multiple comparisons of mortality and hospitalizations between FP and NFP units have found that patients in NFP units have better health status and survival [38, 39], which may contribute to the likelihood of continued employment. However, our analysis at least partially accounted for differences in health status by adjusting for differences in age, race, gender, predialysis nephrology care and other patient and nonpatient factors between FP and NFP [40].
Successful kidney transplantation restores kidney function and improves quality of life [41–44]. We found that patients who maintained employment during the 6 months before HD were more likely to receive a kidney transplant, a difference that remained significant after adjusting for confounding factors. We hypothesize that patients who are working, have EGHP coverage and want to continue to work are more likely to become informed about transplant, to be motivated to complete the testing and to approach potential living donors or get on the transplant list to obtain a transplant, achieve better health and maintain their standard of living. Other studies have shown that patients’ pretransplant employment predicts posttransplant employment [37], and the latter is closely associated with graft and patient survival [38].
Patients who worked at the same level during the 6 months prior to HD had better survival than those who lost their jobs, a benefit that remained significant after adjustment for clinical risk factors. Due to limited data on the Form CMS-2728, some comorbidities at HD initiation, such as infection and inflammation—which may play important roles in outcomes—were unavailable. Some potentially confounding socioeconomic variables, such as education level and mental health conditions, were also unavailable.
Limitations of this study include its retrospective design, which allowed only examination of associations between known variables, not causal relationships, and the lack of data on some clinical and socioeconomic variables, such as residual renal function, depression and nutritional status, which are also key factors that impact patients’ outcomes. Future prospective studies that include these variables could help explain the relationship between decreasing kidney function and employment status.
Overall, we found that HD patients’ employment rates were much lower than in the general US working-age adult population and that changes from employed to unemployed were common during the 6 months prior to HD initiation. Patients’ ability to maintain employment during this period was associated with both patient and facility characteristics. Patients who remained employed during this period were more likely to receive a kidney transplant during the study period—and were more likely to survive.
ACKNOWLEDGEMENTS
The United States Renal Data System (USRDS) Coordinating Center is located at the Kidney Epidemiology and Cost Center, University of Michigan, in partnership with Arbor Research Collaborative for Health, Ann Arbor, MI. Director: R.S., MD, Professor of Medicine and Epidemiology, University of Michigan. Co-deputy Directors: Vahakn Shahinian, MD, University of Michigan, and Bruce Robinson, MD, Vice President, Arbor Research Collaborative for Health. NIDDK Project Officers: Kevin C. Abbott, MD, MPH; Lawrence Y.C. Agodoa, MD.
FUNDING
The USRDS is funded by NIDDK, through NIH contract HHSN276201400001C. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Curtin RB, Oberley ET, Sacksteder P. et al. Differences between employed and nonemployee dialysis patients. Am J Kidney Dis 1996; 27: 533–540 [DOI] [PubMed] [Google Scholar]
- 2. Kutner NG, Zhang R, Huang Y. et al. Depressed mood, usual activity level, and continued employment after starting dialysis. Clin J Am Soc Nephrol 2010; 5: 2040–2045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gutman RA, Stead WW, Robinson RR.. Physical activity and employment status of patients on maintenance dialysis. N Engl J Med 1981; 304: 309–313 [DOI] [PubMed] [Google Scholar]
- 4. Theorell T, Konarski-Svensson JK, Ahlmén J. et al. The role of paid work in Swedish chronic dialysis patients—a nation-wide survey: paid work and dialysis. J Intern Med 1991; 230: 501–509 [DOI] [PubMed] [Google Scholar]
- 5. Rasgon S, James–Rogers A, Chemleski B. et al. Maintenance of employment on dialysis. Adv Ren Replace Ther 1997; 4: 152–159 [DOI] [PubMed] [Google Scholar]
- 6. Linn MW, Sandifer R, Stein S.. Effects of unemployment on mental and physical health. Am J Public Health 1985; 75: 502–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sheeran P, Abraham C.. Unemployment and self-conception: a symbolic interactionist analysis. J Community Appl Soc Psychol 1994; 4: 115–129 [Google Scholar]
- 8. Holley JL, Nespor S.. An analysis of factors affecting employment of chronic dialysis patients. Am J Kidney Dis 1994; 23: 681–685 [DOI] [PubMed] [Google Scholar]
- 9. Ifudu O, Paul H, Mayers JD. et al. Pervasive failed rehabilitation in center-based maintenance hemodialysis patients. Am J Kidney Dis 1994; 23: 394–400 [DOI] [PubMed] [Google Scholar]
- 10. Kutner NG, Brogan D, Fielding B.. Employment status and ability to work among working-age chronic dialysis patients. Am J Nephrol 1991; 11: 334–340 [DOI] [PubMed] [Google Scholar]
- 11. van Manen JG, Korevaar JC, Dekker FW. et al. ; NECOSAD Study Group. Changes in employment status in end-stage renal disease patients during their first year of dialysis. Perit Dial Int 2001; 21: 595–601 [PubMed] [Google Scholar]
- 12. Kim JM, Son NH, Park EC. et al. The relationship between changes in employment status and mortality risk based on the Korea Labor and Income Panel Study (2003-2008). Asia Pac J Public Health 2015; 27: NP993–NP1001 [DOI] [PubMed] [Google Scholar]
- 13. Sandhu GS, Khattak M, Rout P. et al. Social Adaptability Index: application and outcomes in a dialysis population. Nephrol Dial Transplant 2011; 26: 2667–2674 [DOI] [PubMed] [Google Scholar]
- 14. Thong MS, Kaptein AA, Benyamini Y. et al. ; Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD) Study Group. Association between a self-rated health question and mortality in young and old dialysis patients: a cohort study. Am J Kidney Dis 2008; 52: 111–117 [DOI] [PubMed] [Google Scholar]
- 15.Centers for Medicare & Medicaid Services. https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/cms2728.pdf (4 May 2017, date last accessed)
- 16.Medicare Dialysis Facility Compare. https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/cms2728.pdf (4 May 2017, date last accessed)
- 17.Centers for Medicare & Medicaid Services. https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/cms2746.pdf (4 May 2017, date last accessed)
- 18.Scientific Registry of Transplant Recipients. https://www.srtr.org/
- 19.SOI Tax Stats Individual Income Tax Statistics ZIP Code Data. https://www.irs.gov/statistics/soi-tax-stats-individual-income-tax-statistics-zip-code-data-soi (27 September 2017, date last accessed)
- 20. Walters BA, Hays RD, Spritzer KL. et al. Health-related quality of life, depressive symptoms, anemia, and malnutrition at hemodialysis initiation. Am J Kidney Dis 2002; 40: 1185–1194 [DOI] [PubMed] [Google Scholar]
- 21. Nakayama M, Ishida M, Ogihara M. et al. Social functioning and socioeconomic changes after introduction of regular dialysis treatment and impact of dialysis modality: a multi-centre survey of Japanese patients. Nephrology (Carlton) 2015; 20: 523–530 [DOI] [PubMed] [Google Scholar]
- 22. Blake C, Codd MB, Cassidy A. et al. Physical function, employment and quality of life in end-stage renal disease. J Nephrol 2000; 13: 142–149 [PubMed] [Google Scholar]
- 23. Murray PD, Dobbels F, Lonsdale DC. et al. Impact of end-stage kidney disease on academic achievement and employment in young adults: a mixed methods study. J Adolesc Health 2014; 55: 505–512 [DOI] [PubMed] [Google Scholar]
- 24. Manavalan M, Majumdar A, Harichandra Kumar KT. et al. Assessment of health-related quality of life and its determinants in patients with chronic kidney disease. Indian J Nephrol 2017; 27: 37–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Al Eissa M, Al Sulaiman M, Jondeby M.. Factors affecting hemodialysis patients’ satisfaction with their dialysis therapy. Int J Nephrol 2010; 2010: 342901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.United States Department of Labor, Bureau of Labor Statistics. http://www.bls.gov/news.release/empsit.t01.htm (22 May 2017, date last accessed)
- 27. Assari S. Distal, intermediate, and proximal mediators of racial disparities in renal disease mortality in the United States. J Nephropathol 2016; 5: 51–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Muehrer RJ, Schatell D, Witten B. et al. Factors affecting employment at initiation of dialysis. Clin J Am Soc Nephrol 2011; 6: 489–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Waterschoot M. Evaluation of response to various erythropoiesis—stimulating proteins using anemia management software. J Ren Care 2007; 33: 78–82 [DOI] [PubMed] [Google Scholar]
- 30. Paradise J. 10 Things to Know about Medicaid: Setting the Facts Straight. Kaiser Family Foundation 9 May 2017. http://kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-setting-the-facts-straight (28 May 2017, date last accessed)
- 31. Yan G, Cheung AK, Greene T. et al. Interstate variation in receipt of nephrologist care in US patients approaching ESRD: race, age, and state characteristics. Clin J Am Soc Nephrol 2015; 10: 1979–1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Banerjee T, Kim SJ, Astor B. et al. Vascular access type, inflammatory markers, and mortality in incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study. Am J Kidney Dis 2014; 64: 954–956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Domenick Sridharan N, Fish L, Yu L. et al. The associations of hemodialysis access type and access satisfaction with health-related quality of life. J Vasc Surg 2018; 67: 229–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kutner N, Bowles T, Zhang R. et al. Dialysis facility characteristics and variation in employment rates: a national study. Clin J Am Soc Nephrol 2008; 3: 111–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hirth RA, Chernew ME, Turenne MN. et al. Chronic illness, treatment choice and workforce participation. Int J Health Care Finance Econ 2003; 3: 167–181 [DOI] [PubMed] [Google Scholar]
- 36. Molsted S, Prescott L, Heaf J. et al. Assessment and clinical aspects of health-related quality of life in dialysis patients and patients with chronic kidney disease. Nephron Clin Pract 2007; 106: c24–c33 [DOI] [PubMed] [Google Scholar]
- 37. Helanterä I, Haapio M, Koskinen P. et al. Employment of patients receiving maintenance dialysis and after kidney transplant: a cross-sectional study from Finland. Am J Kidney Dis 2012; 59: 700–706 [DOI] [PubMed] [Google Scholar]
- 38. Devereaux PJ, Schünemann HJ, Ravindran N. et al. Comparison of mortality between private for-profit and private not-for-profit hemodialysis centers: a systematic review and meta-analysis. JAMA 2002; 288: 2449–2457 [DOI] [PubMed] [Google Scholar]
- 39. Foley RN, Fan Q, Liu J. et al. Comparative mortality of hemodialysis patients at for-profit and not-for-profit dialysis facilities in the United States, 1998 to 2003: a retrospective analysis. BMC Nephrol 2008; 9: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Krishnan M, Christopher Bond T, Brunelli S.. Impact of potential confounders on comparisons between United Stated for-profit and nonprofit dialysis providers. Nephrol Dial Transplant 2013; 28 (Suppl 1): i258–i270 [Google Scholar]
- 41. von der Lippe N, Waldum B, Brekke FB. et al. From dialysis to transplantation: a 5-year longitudinal study on self-reported quality of life. BMC Nephrol 2014; 15: 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Czyżewski L, Sańko-Resmer J, Wyzgał J. et al. Assessment of health-related quality of life of patients after kidney transplantation in comparison with hemodialysis and peritoneal dialysis. Ann Transplant 2014; 19: 576–585 [DOI] [PubMed] [Google Scholar]
- 43. Danuser B, Simcox A, Studer R. et al. ; Psychosocial Interest Group, Swiss Transplant Cohort Study. Employment 12 months after kidney transplantation: An in-depth bio-psycho-social analysis of the Swiss Transplant Cohort. PLoS One 2017; 12: e0175161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Petersen E, Baird BC, Barenbaum LL. et al. The impact of employment status on recipient and renal allograft survival. Clin Transplant 2008; 22: 428–438 [DOI] [PubMed] [Google Scholar]