Abstract
A rather quick change in epidemiological shift from Trichophyton rubrum to Trichophyton mentagrophytes (ITS genotype VIII), several changes in clinical presentation of superficial dermatophytoses and the the response/ the lack of it, makes this current epidemic very interesting and novel. We present here some of the relatively less discussed variants that have been described under the broad terms of tinea corporis and tinea faceie. Many of them are found to occur uncharacteristically frequently and some in areas that were never described. We describe some representative cases of female genital dermatophytoses, periumblical and periocular dermatophytosis and discuss some unusual variants like those showing sole involvement of the ear (tinea auricularis), lip (tinea labialis) and superficial dermatophytosis of the scalp skin.
Keywords: Dermatophytosis, female genital dermatophytosis, periocular tinea, periumbilical tinea, superficial dermatophytosis of scalp skin, tinea auricularis, tinea labialis
The current epidemic like situation of dermatophytosis is known for two notable features, the rather quick epidemiological shift from Trichophyton rubrum to Trichophyton mentagrophytes and the raging abuse of super potent steroid containing fixed dose combinations (FDCs) that a majority of individuals apply at some point in time during the disease episode.[1,2,3,4,5,6,7,8] Some of the most common forms seen in the current scenario in India are tinea corporis et cruris, tinea corporis, tinea cruris individually, and tinea faciei, with many morphological patterns described.[9,10,11] Many of these are attributed to abuse of fixed dose combination (FDC) creams containing steroids.[6,12,14] Dermatophytosis is also known to mimic many other dermatoses.[15] This article is aimed at describing some seldom discussed individual anatomical locations where we see superficial dermatophytosis (SD) but which are perhaps not mentioned specifically because they get included in broader terms like tinea corporis, tinea faciei, and tinea cruris. It is our belief that documenting these hitherto undescribed anatomical sites would prompt us to scan them while examining patients of SD in addition to the areas pointed out by the patient. Relevant advice can then be given as part of the treatment.
Involvement of the Umbilicus
Tinea corporis presents in many morphological forms from single to multiple variably sized lesions, some individual lesions show coalescence. The umbilicus is seen to be affected quite frequently. The involvement is either strictly confined to the umbilicus, presenting as a well circumscribed lesion or a well-defined lesion surrounding the umbilicus with erythema, hyperpigmentation and scaling, itching, etc., [Figure 1a-d]. Widespread tinea corporis involving the umbilicus is common[16] [Figure 1e and f]. The localized involvement however, especially lesions confined to the umbilicus or spreading centrifugally, indicates a distinct predilection for the area to becoming infected with dermatophytes. The umbilicus is an anatomical structure that often depressed compared with the surrounding skin but shows variable concavity and convexity within the structure. It is prone to retaining moisture on account of perspiration and bathing. It also retains unwashed soap, fiber of clothes and often has an objectionable odor due to sebum. Individuals often do not consciously wipe or dry the umbilicus specifically. Retained moisture and in some cases friction, can lead to barrier dysfunction rendering the area more prone to seeding of the fungus and also provide an ideal milieu for its growth. However, this area does not show a similar predilection for viral or bacterial diseases. Paying special attention to the umbilicus while cleaning and drying the trunk with a towel is vital in our opinion. Failing to do so can lead to persistence of the dermatophyte in that area acting as a constant reservoir of infection.
Figure 1.
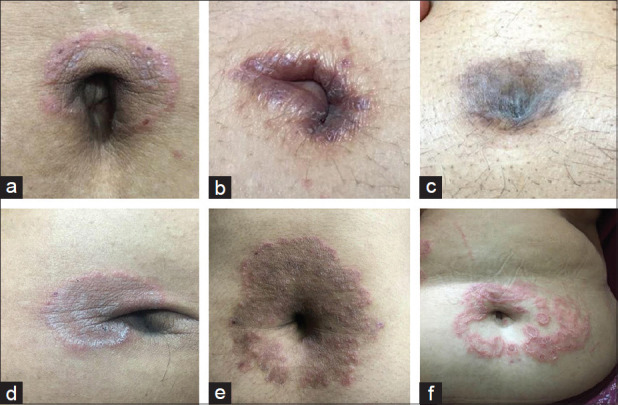
(a-d) SD of umbilicus with early centrifugal spread. (e and f) centrifugal spread of umbilical SD with involvement of abdominal skin
Genital involvement in women
Genital dermatophytic involvement in men is much more common as well as documented than in females.[12] The pubic region is seen to be predominantly involved with or without concomitant tinea cruris or tinea corporis [Figure 2a-d]. It is very common to elicit history of application of steroid containing fixed dose combination (FDC) creams in those areas.[13,14] Most women presenting with sole involvement of pubic region give history of shaving or waxing their pubic hair. Both these procedures can potentially damage the epidermis which becomes a locus minoris resistensae for introduction of the dermatophyte deeper in the skin. The possibility of a sexual transmission has also been alluded to in literature and the phenomenon needs to be studied in detail.[17]
Figure 2.

(a) Multiple erythematous annular and circular lesions restricted to the shaved pubic region. (b) Hyperpigmented patch covering the entire pubic area within which are small annular perifollicular plaques studded with peripheral pustules. (c) Double edged tinea involving the pubic region with early involvement ofsuprapubic, abdominal and groinareas. (d) Unusual case of tinea cruris with pronounced lesion on right side, scaly lesions on pubic region and early involvement of groin on the left side
Involvement of the External Ear (Tinea auricularis)
This is another common anatomical area that is increasingly observed to be affected by dermatophytosis. Although ears are protruding extensions of the face they are being discussed separately for the following reasons. The ear can get involved by direct extension of tinea faciei [Figure 3c]. However it can get involved in presence of distant lesions of tinea faciei too[18] [Figure 3d]. The uncommon but notable observation however, is the sole involvement of the ear with no sign of dermatophytosis on the face or elsewhere on the body [Figure 3a and b]. In such situations it is at times difficult to diagnose clinically, owing to the difficulty in discerning an active border on account of to the complex shape of the ear. While the 'ear sign' was used to differentiate tinea capitis from seborrhea capitis in the past, it is seen very often against the backdrop of tinea faciei in the current scenario.[18] The ipsilateral dermatophytic involvement of the ear in the presence of tinea faciei serves as an additional clinical confirmation of dermatophytic origin of both, especially in cases where steroid containing FDCs have been applied leading to masking or vitiation of clinical features. It is noteworthy to mention that in today's scenario it is very often the face on which true “tinea incognita” is observed. The term “tinea auricularis” seems appropriate to describe a dermatophytic involvement involving solely the ear [Figure 3a and b]. The ear too, like the umbilicus, is a structure full of convexities and concavities owing to its fibrocartilaginous structure. Water, sweat and moisture can easily get retained in this area and the condition may be perpetuated by wearing earrings in some cases. This as well as the retroauricular area is ignored while wiping the body. Therefore, like the umbilicus, this too becomes a potential site for growth and spread of dermatophytes. Meticulous cleaning, drying, and application of appropriate antifungals along with conventional oral antifungal agents are recommended in treating both the umbilicus as well as the ear.
Figure 3.
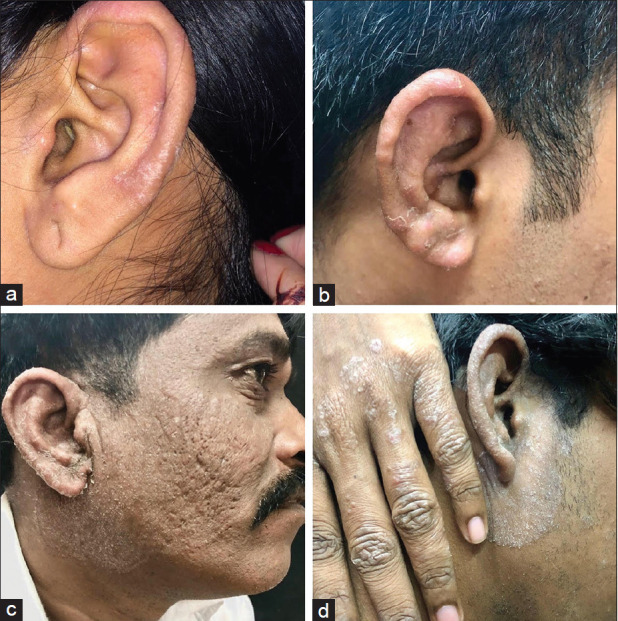
(a and b) Tinea auricularis-sole involvement of the ear. (c) Tinea faciei extending to the area of contiguous spread. (d) Tinea auricularis spreading to the surrounding skin of the face with involvement of the dorsum of the hand
Periocular involvement
Periocular involvement in tinea faciei is another less discussed clinical pattern in need of description. Tinea faciei, especially widespread infection, is much more frequently encountered in the current epidemic like scenario in India compared with the past. Almost all areas of the face are known to be affected, either as scaly, skin colored or erythematous lesions with distinct borders, and also as ill-defined areas of macular, papuler or plaque type of lesions with powdery scaling extending into the periocular region from the forehead, cheek area or nose [Figure 4b and d]. At times, as seen in the solitary lesions of tinea auricularis, the lesions are restricted only to the periocular area [Figures 4a, c and 5a, b]. Both lower and upper eyelids including the canthi can be involved and lesions are often difficult to discern due to the rugose skin of the eyelids especially in the elderly.[19] Close inspection reveals involvement of eyelashes at times. The periocular lesions, especially those which remain localized, are often treated with topical steroids with the mistaken working diagnosis of atopic dermatitis or seborrheic dermatitis[20] [Figure 5a]. Eventually a clearer picture of dermatophytosis emerges [Figure 5b]. A dermoscopic examination of eyelashes reveals a picture similar to tinea extending from neck or face to the scalp skin where scaling is visible, but there is no involvement of the eyelid hair [Figure 5c]. Patients very often complain of burning, exacerbation of erythema or worsening of itch in lesions upon exposure to kitchen heat, sunlight or sweating. The chronic rubbing and scratching of the periocular area may impart a rough, thickened, scaly appearance of eyelids which benefits from emollients as seen in patients with atopic dermatitis, in addition to topical and oral antifungal agents. Our routine advice to ensure avoidance of topical antifungal agents from coming into contact with eyes may result in “skipped areas” that may become a focus for chronicity, recurrence or reinfection.
Figure 4.

(a) Erythematous lesion of SD starting at the root of nose, involving both eyelids and ending at outer canthus. (b) “Double edged” lesion and powdery scales of tinea faciei visible on the right temple involving the entire upper eyelid and both canthi. (c) Erythematous scaly plaque with central clearing involving lower eyelid and inner canthus. (d) Fairly well defined powdery scaly lesion with mild erythema involving almost the entire left side of face including the eyelids
Figure 5.

(a) Ill-defined lesions of SD present along the eyelid margin diagnosed initially as atopic dermatitis and treated with topical steroid. (b) Steroid cream unmasking the lesions of underlying SD with appearance of erythematous papules and plaques in the periphery. (c) Inflammed scaly upper eyelid margin showing no obvious involvement of hair shaft
Dermatophytosis of the Scalp Skin (Extension of Tinea Corporis and Tinea Faciei onto the Skin of the Scalp)
While there is no corresponding increase in the incidence and prevalence of tinea capitis unlike in other variants already described above, a new observation awaiting documentation is extension of tinea corporis from the nape of the neck and tinea faciei from anterior and lateral aspects of the face into the scalp [Figure 6a-d]. Although we see only limited extension into the scalp some have observed it to begin and remain restricted to the scalp. The involved area, which in our experience is most often not too far into the scalp, shows no apparent alopecia, presence of black dots, grey, dull appearance of the hair or apparent pustulation/bogginess as one would expect in the noninflammatory and inflammatory variants of tinea capitis.[21,22,23] While some cases are very obvious, some require diligent examination involving parting and separating of the scalp hair to visualize the scaly lesions extending into the scalp. Trimming of the hair enables visualizing the active border in some cases. While it clinically seems to spare the hair shaft, it involves the skin of the scalp. The logic of sparing of the scalp in dermatophytosis in adults owing to its sebum rich milieu does not seem to apply here.[21] Dermoscopic examination performed in the cases that we have seen shows no obvious hair shaft involvement but the presence of scales in all and erythema in some cases. KOH examination from the scales on the scalp is positive in most of them. The culture positive cases of this variant of “dermatophytosis of the scalp skin” have all grown T. mentagrophytes. The entity responds to the conventional antifungal therapy. It is important to advise patients not to share combs in such patients. This phenomenon may be due to the increased virulence of T. mentagrophytes or an altered host response to this newly predominant species. A more in-depth study with a greater number of patients is in order.
Figure 6.

(a) Well-defined lesion on the nape of the neck with fine scaling merging into the scalp. (b) Ill-defined erythematous lesion with scattered papules and scales merging into the scalp. (c) Well defined erythematous scaly papular eruption with a well-defined margin on the nape of necktraversing the scalp margin. (d) Tinea faciei on the forehead extending to the scalp
Involvement of lip
Extensive dermatophytic involvement of the face is seen in the current scenario, but involvement of the lip is rare phenomenon. A female patient of tinea faciei presented with lesions on and around the philthrum that extended to the upper lip [Figure 7]. The active border of the lesion involved the alae and border of nostrils superiorly and involved the upper lip inferiorly presenting as a poorly defined scaly patch. She however did not complain of itching over the lip. Scraping of the upper lip was positive on a KOH mount for dermatophytes.
Figure 7.

Mildly erythematous Tinea faciei involving the alae, philthrum and the central upper lip showing an active edge and scaling
Involvement of areola
Similarly, one of us saw a patient with tinea corporis of the thighs who complained of severe itching over one areola. Mild erythema and scattered scaly papules were seen [Figure 8]. The surrounding skin of the breast was normal. KOH mount from the area was positive for dermatophytosis.
Figure 8.

Minimally erythematous itchy papular scaly lesions restricted to the right areola
Dermatophytosis on skin in contact with religious threads and bangles
Tinea corporis involving skin in contact with religious threads and bangles is increasingly being seen. Although dermatophytosis on areas in contact with bangles and watches is not uncommon, the disease does seems to favor skin in contact with woven threads of different colors like red, yellow, and black that are tied on the wrist and waist as part of Hindu ceremonies or certain religious beliefs [Figure 9a-f]. They remain in contact with the skin during bathing and washing, get soaked in water and perspiration and could have a significant role to play in the infection or its perpetuation. It is prudent to advise the patient to discontinue the practice.
Figure 9.

(a and b) Doubled edged tinea corporis of the wrists in the areas subjected to constant friction. (c and d) Tinea corporis of the abdomen and nape of neck where the black religious thread is tied. (e and f) Tinea corporis restricted to ceremonial threads tied on the wrist
In conclusion, it is becoming increasingly evident that dermatophytes seem to have a predilection for certain specific but under-discussed anatomical areas in the current scenario of superficial dermatophytosis in India. These often get lost in the wider terms like tinea corporis, tinea faciei, and tinea cruris. A diligent examination of all the areas under good lighting is recommended. Use of steroid containing FDCs have an indubitable role in the spread and changing morphology of various localized clinical variants of dermatophytosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nenoff P, Verma SB, Vasani R, Burmester A, Hipler UC, Wittig F, et al. The current Indian epidemic of superficial dermatophytosis due to Trichophyton mentagrophytes-A molecular study. Mycoses. 2019;62:336–56. doi: 10.1111/myc.12878. [DOI] [PubMed] [Google Scholar]
- 2.Dabas R, Janney M, Subramaniyan R, Arora S, Lal V, Donaparthi N. Use of over-the-counter topical medications in dermatophytosis: A cross-sectional, single-center, pilot study from a tertiary care hospital. J Drugs Dermatol. 2018;4:13–7. [Google Scholar]
- 3.Dogra S, Uprety S. The menace of chronic and recurrent dermatophytosis in India: Is the problem deeper than we perceive? Indian Dermatol Online J. 2016;7:73–6. doi: 10.4103/2229-5178.178100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rajagopalan M, Inamadar A, Mittal A, Miskeen AK, Srinivas CR, Sardana K, et al. Expert Consensus on The Management of Dermatophytosis in India (ECTODERM India) BMC Dermatol. 2018;18:6. doi: 10.1186/s12895-018-0073-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verma S. Emergence of recalcitrant dermatophytosis in India. Lancet Infect Dis. 2018;18:250–1. doi: 10.1016/S1473-3099(18)30079-3. [DOI] [PubMed] [Google Scholar]
- 6.Mahajan S, Tilak R, Kaushal S, Mishra R, Pandey S. Clinico-mycological study of dermatophytic infections and their sensitivity to antifungal drugs in a tertiary care center. Indian J Dermatol Venereol Leprol. 2017;83:436–40. doi: 10.4103/ijdvl.IJDVL_519_16. [DOI] [PubMed] [Google Scholar]
- 7.Sahai S, Mishra D. Change in spectrum of dermatophytes isolated from superficial mycoses cases: First report from Central India. Indian J Dermatol Venereol Leprol. 2011;77:335–6. doi: 10.4103/0378-6323.79718. [DOI] [PubMed] [Google Scholar]
- 8.Bhatia VK, Sharma PC. Epidemiological studies on Dermatophytosis in human patients in Himachal Pradesh, India. Springerplus. 2014;3:134. doi: 10.1186/2193-1801-3-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vineetha M, Sheeja S, Celine MI, Sadeep MS, Palackal S, Shanimole PE, et al. Profile of dermatophytosis in a tertiary care center. Indian Dermatol Online J. 2018;63:490–5. doi: 10.4103/ijd.IJD_177_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta AK, Chaudhry M, Elewski B. Tinea corporis, tinea cruris, tinea nigra, and piedra. Dermatol Clin. 2003;21:395–400. doi: 10.1016/s0733-8635(03)00031-7. [DOI] [PubMed] [Google Scholar]
- 11.Moriarty B, Hay R, Morris-Jones R. The diagnosis and management of tinea. Br Med J. 2012;345:e4380. doi: 10.1136/bmj.e4380. [DOI] [PubMed] [Google Scholar]
- 12.Verma S, Madhu R. The great Indian epidemic of superficial dermatophytosis: An appraisal. Indian Dermatol Online J. 2017;62:227–36. doi: 10.4103/ijd.IJD_206_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verma SB, Vasani R. Male genital dermatophytosis-clinical features and the effects of the misuse of topical steroids and steroid combinations-an alarming problem in India. Mycoses. 2016;59:606–14. doi: 10.1111/myc.12503. [DOI] [PubMed] [Google Scholar]
- 14.Bishnoi A, Vinay K, Dogra S. Emergence of recalcitrant dermatophytosis in India. Lancet Infect Dis. 2018;18:250–1. doi: 10.1016/S1473-3099(18)30079-3. [DOI] [PubMed] [Google Scholar]
- 15.15 Dogra S, Narang T. Emerging atypical and unusual presentations of dermatophytosis in India. Clin Dermatol Rev. 2017;1:12–8. [Google Scholar]
- 16.Chiriac A, Foia L, Coros MF, Podoleanu C, Stolnicu S. Umbilical psoriasis versus tinea corporis in infants: A simple clinical diagnosis/image view. Pediatrics Neonatol. 2017;58:291–2. doi: 10.1016/j.pedneo.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 17.Luchsinger I, Bosshard PP, Kasper RS, Reinhardt D, Lautenschlager S. Tinea genitalis: A new entity of sexually transmitted infection? Case series and review of the literature. Sex Transm Infect. 2015;91:493–6. doi: 10.1136/sextrans-2015-052036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agarwal U, Mathur D, Mathur D, Besarwal R, Agarwal P. Ear sign. Indian Dermatol Online J. 2014;5:105–6. doi: 10.4103/2229-5178.126064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calles Monar PS, Juarez Martin A. Eyelid tinea with blepharitis due to Microsporum canis. Arch Soc Esp Oftalmol. 2018;93:491–3. doi: 10.1016/j.oftal.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Machado AP, Hirata SH, Ogawa MM, Tomimori-Yamashita J, Fischman O. Dermatophytosis on the eyelid caused by Microsporum gypseum. Mycoses. 2005;48:73–5. doi: 10.1111/j.1439-0507.2004.01053.x. [DOI] [PubMed] [Google Scholar]
- 21.Auchus IC, Ward KM, Brodell RT, Brents MJ, Jackson JD. Tinea capitis in adults. Dermatol Online J. 2016;22 [PubMed] [Google Scholar]
- 22.Hay RJ. Tinea Capitis: Current Status. Mycopathologia. 2017;182:87–93. doi: 10.1007/s11046-016-0058-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta AK, Summerbell RC. Tinea capitis. Med Mycol. 2000;38:255–87. doi: 10.1080/mmy.38.4.255.287. [DOI] [PubMed] [Google Scholar]


