The corona virus disease 2019 (COVID-19) pandemic has shaken the healthcare delivery system, all over the world.[1] Social distancing is the key to flatten the curve of disease spread and the same applies to healthcare and hospitals. For medical consultations, not involving serious or emergency situations, it would be important to ensure appropriate healthcare delivery, without compromising on social distancing protocols. This has opened up a whole world of opportunity for telemedicine, which was hitherto less used in India, where even a legal framework was lacking for this. The application of telemedicine in the context of dermatology is referred to as “teledermatology.” Because of the inherently visual nature of the specialty, dermatology can be considered to be especially suitable for telemedicine. There are some important aspects which need to be clarified and standardized for the optimum application of teledermatology in India.
Dermatologist and Telemedicine in India: Need for Improvement
In a country where the doctor-to-patient ratio is very small and speciality practice is predominantly urban centric, telemedicine is something that should have come into routine practice long ago.[2] Published information shows that, a doctor, approximately caters to 10,189 people and that there is a deficit of nearly 6,00,000 doctors in the country.[3,4] In India, we have less specialists (dermatologists) per population. Indian Association of Dermatologists Venereologists and Leprologists (IADVL) has a membership count of 12,740 as on 11th April, 2020 (Information sourced through personal communication from Honorary Secretary General of IADVL, Dr. Feroz. K) to cater to the 1341.0 million population with a ratio of approximately one dermatologist per 130,000 population. The COVID-19 pandemic and the resultant healthcare delivery issues could be a good time to plan and implement an effective and enduring teledermatology system for India.
Historic perspective. How it was done earlier?
World Health Organisation (WHO) has clearly defined telemedicine,[5] whereas in India, we never had a standard guideline for teleconsultation till the Medical Council of India (MCI) brought the directive to provide healthcare using telemedicine during the COVID-19 pandemic period.[6] This was to ease the burden and reduce the physical patient load and overcrowding in the outpatient departments across all hospitals in the country.
Advantages of teleconsultation over the routine ones
There have been a few interesting publications on this subject which did attempt to throw light on the subject earlier. In a nutshell, the consultant delivers the services from fixed point, without the need for direct contact with the patient or physical examination. This saves a lot of man hours and logistics and resources. Documentation can also be done quite easily using a paperless, electronic platform.[7,8,9,10,11,12]
Judicious application of teledermatology
Teledermatology has a definite role when people are restricted or discouraged from visiting hospitals unless there is a dire emergency, as in the COVID-19 crisis.[13]
Teledermatology, as in most forms of telemedicine, works best for periodic follow-up of patients unless it is very late review. They are most benefited from this as the doctor can easily decide things being aware of the case and with the data already from the previous personal visit and investigation reports available. Immunocompromised patients and organ recipients are best not exposed to crowds and hospitals unless in emergency to reduce chances of receiving cross-infections and hence can opt for teledermatology if the problem is trivial. Dermatology patients on prolonged medication and in remission can use teleconsult in between as they may need just a verification from the doctor to continue their medications. India has a lot of expatriates who come home during holidays and they visit Indian doctors during this time. They are usually unable to follow-up due to the short time spent here. Such people can also make use of the facility to update their progress. Drug prescription to people outside the purview of the medical council are not permitted in telemedicine guidelines. Bed ridden, pregnant, and debilitated patients who cannot be brought to doctor too often benefit well from the facility. Counselling and education sessions where medications do not have much role can be easily and efficiently carried out on teledermatology platforms.[14]
Critical care dermatology, like a severe cutaneous drug reaction [Eg. SJS/TEN], angioedema or acute urticaria, with anaphylaxis, severe vasculitic conditions, or exacerbation of bullous disorders, are best not taken up for teledermatology. Teledermatology can still be a tool for triage in such cases and the patient can be advised on the next action to be taken. Similarly, conditions involving multisystem complaints are also not suitable for conclusive teledermatology consults. First time consultation even if not an emergency is less amenable for teledermatology, as compared to follow-up consultations.
Those conditions that mandatorily need a physical examination involving palpation or special tests (e.g. Hansen's disease where the power of the limb or sensation over a patch needs to be ascertained, etc.) are best not taken up for teleconsultation to begin with.
Technicalities. Imaging and video streaming
With broadband services being available throughout the country, telemedicine can be easily practiced even using a patient-initiated model (through mobile applications like WhatsApp, Zoom, Google Duo. etc.) These media have the obvious advantage of the patient being familiar in using them. There is no need not wait for a dermatology referral from the health center or a general practitioner. However, patient-initiated consults using mobile apps are limited by lower validity and also the difficulty in linking to a formal electronic medical record and prescription.
An ideal system would need the consultation to be linked to a retrievable, secure, electronic medical record (EMR), where the patient can login with secure credentials, and after the consultations, the prescribed medications can be procured directly by the patient from linked pharmacists (or delivered at home to the patient). This would also need to be connected to a secure payment gateway.
The key technical requirement (other than the high-speed internet) for teledermatology is the quality of the images. Most smartphones these days have sufficient image resolution, in terms of megapixels, but it is important that the dermatologist not make conclusions if the images are not clear enough. Insist on alternate images in such cases.
The ideal format for teledermatology would be a hybrid of the store and forward (SAF) and real-time consults (RTC), where the images and basic patient data/history is sent to the dermatologists, who then gives an appointment for a real time consult.
Telemedicine service guidelines of the Medical Council of India
The Board of Governors (BoG) of MCI has issued telemedicine guidelines by amendment of MCI regulations 2002 by adding Regulation 3.8 titled as “Consultation by Telemedicine” in the said regulations and by adding Telemedicine Practice Guidelines (TPG) as appendix 5 to the said regulation. The directive gives an elaborate description of how to undertake telemedicine practice by the registered medical practitioners in India who is enrolled in the State Register or the National Register under the IMC Act 1956.[6] The council has left the doors for improvement open by stating that the TPG can be amended from time to time in larger public interest with the prior approval of Central Government (Ministry of Health and Family Welfare, Government of India). All registered medical professionals are supposed to enrol for an online course which is being formulated for this purpose. The Registered Medical Practitioner (RMP) has all rights to decide to go forward or defer a telemedicine consultation if he thinks it is not going to be of use for the patient. This is one of the most important points in the order.
MCI has made it mandatory that the following seven points need to be considered vital before any telemedicine consultation; (1) context, (2), identification of RMP and patient, (3) mode of communication consent, (4) type of consultation, (5) patient evaluation, (6). patient management. The Council has categorically mentioned that the medicines listed in Schedule X of Drug and Cosmetic Act and Rules or any Narcotic and Psychotropic substance listed in the Narcotic Drugs and Psychotropic substances, Act, 1985 CAN NOT be prescribed via teleconsultations. A sample prescription is also furnished in the directive issued by the MCI.
We tried to analyze the subsequent guidelines of various state medical councils (Karnataka, Tamil Nadu, Punjab, Gujarat, Kerala, and Madhya Pradesh) released in the months of March and April, 2020. All of them were in concurrence with the MCI guidelines. There is a lack of clarity on certain issues that needs to be sorted out. To cite two examples, there is a mention in some state orders that telemedicine is permitted till lockdown period only and in another order it is mentioned that that telemedicine facility shouldn't cover beyond the purview of that state medical council without a mention if the doctor can cater to patients from other states within the country.[15,16,17,18,19,20]
Professional organisations and their directives
IADVL also has come forward with a directive of teledermatology services that can be offered in view of the COVID-19 pandemic.[21] They have also adopted the guidelines furnished by the MCI and stresses the importance of adhering to the norms laid in the said primary order of the MCI. The British Association of Dermatologists (BAD) and the American Academy of Dermatology (AAD) also came out with their guidelines on managing teledermatology services during this pandemic time.[22,23] Taking into account the MCI order which instructs doctors to undergo training in telemedicine prior to undertaking telemedicine facility, Telemedicine Society of India has come out with an online training module which is offered free for a certain period.[24]
How to run the show?
There can be mainly three ways of delivering the services on teledermatology.
Patient operated system connecting to the healthcare provider in real time using available modes of texting, imaging, audio, and video facility on smartphone, personal computer, and such devices [Figures 1a, b, 2a, b, 3a, b]
Trained assistant (located in the remote location) operated system which also works in the same lines but the infrastructure is better and there is likely to be a more standardized approach to the procedure. This is also in real time [Figure 4]
Create, Store, and forward system where the images, videos, and information are entered by the patient or the trained assistant in the remote locations and sent to the healthcare system via cloud storage and retrieved and processed at a later time. This is more useful for mass screening and camps, etc., The advantage being, a larger number of patients can be recruited to avail the facility and the quality is also likely to be better than real time as there are scopes for retakes.
Figure 1.

(a) Teledermatology consultation using Google Duo application-based video calls being carried out with projection on a large screen. (b) Teledermatology consultation using Zoom Application projected on a computer screen
Figure 2.
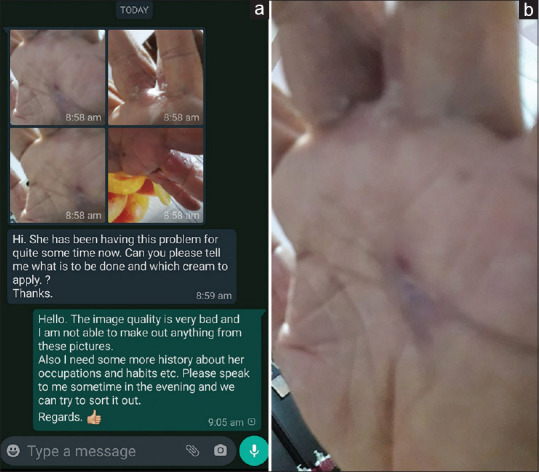
(a) Screenshot of a WhatsApp communication for online consultations with poor quality images (b) The image is out of focus and one cannot make out the morphology of the lesion
Figure 3.
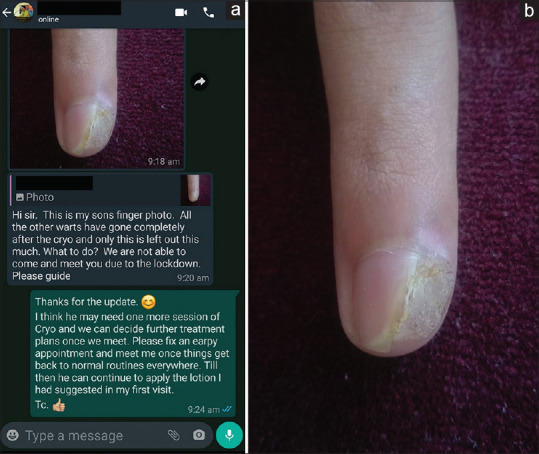
(a) Screenshot of a WhatsApp communication for online consultations with good quality image (b) The image is clear and the residual wart is well made out and the clinician is able to make a decision seeing the image
Figure 4.

Teledermatology set up at a tertiary care referral hospital
Testing the waters: Patient and the doctor
Though legally valid, we are of the opinion that teledermatology in India is still in a test mode and the number of people used to this system are very less be it the patient or the doctor. Obviously, hiccups are likely till a flawless system evolves in the coming times. Patients who have been used to a traditional face to face consultation may feel less satisfied after an online consultation. The same goes for doctors who have been used to examining patients in person. It would also be frustrating for dermatologists as many a time they may find it difficult to come to a definitive clinical conclusion looking at an image and a brief history. This calls for a statutory disclaimer which is read and understood by the patient or the person handling the teleconsultation, which says that the accuracy may be lesser than a real time personal consultation and teleconsultation cannot be equated to the same. The clinician should make it very clear that he is giving probable differentials and suggesting best treatments with the information available at his disposal. The patient should be advised to come for a face-to-face consultation if the desired response is not seen with the advices given. The need for repeat sessions also has to be kept in mind by both parties in view of the compromised working environment. Prescribing procedures or injections via teleconsultation is not recommended in any situations as of now.[6]
Major hurdles in the Indian context
One of the major issues in India is the technology illiteracy of the masses and appropriate devices in spite of having access to high speed internet. This calls for adequate training, dedicated telemedicine units in peripheral hospitals or even a telemedicine van (Mobile Telemedicine Unit) with necessary infrastructure and technical manpower that can go to various remote places from where they can coordinate the consultations with the specialist in the parent center.
There are several commercially available teleconsultation portals and in the midst of COVID-19, there is an all the more aggressive marketing in vogue. One of the concerns raised by those who are using such options is that the patient details are retained by the third party and they may even manipulate to divert or decide reviews of the patients. This is at the cost of compromising the rights of the patients which is uncalled for. Additionally, patient images and data being left with them is risky and may breach privacy. Such matters need to be addressed to. It is always desirable to get a review of such teleconsultation platforms from familiar people and friends before committing to any of them. And the best one would be where data is retained at the clinician's end. People who take consults on WhatsApp tend to repeatedly communicate later for even unrelated matters which is intruding into the privacy of the clinicians.
Economics of teleconsultations
A doctor doing a teleconsultation will definitely be expected to get a professional fee for the service rendered. MCI had made it very clear in their directive that no additional fee should be charged for a teleconsultation. A receipt if the situation demands has to be handed over to the patient who may be able to present it for reimbursements like the routine consultations.[6] Still, the unaccustomed patient who feels he is getting less than what he is paying for may end up as unhappy after the teleconsultation. This is going to be a mismatch that needs to be addressed and correction will happen only over time once the service becomes widely used and people get used to it. The services are best retained as prepaid and not postpaid to avoid misuse. If it is a unified system in place there can be various ways this can be tackled like a part payment to initiate a consultation and prescription can be generated from the system only upon completion of payment after the consultation
Need for a centralised system
Standard prescription pattern is the most important requirement for online consultations. This is going to be a tough ask initially as there are multiple software companies coming up with their own approaches. There are plenty of them already available in the market as well. This is the time where the government has to interfere and regularize proceedings or it may go haywire like the EMR. Although centralizing and streamlining may seem difficult, it is worth the effort. Otherwise it may be a bit chaotic as in each hospital or clinic having their own EMR software in place which don't sync well.
Medicolegal implications
Now that it is a legal process, all the laws pertaining to regular consultation are likely to be applied for teleconsultations also. Hence all routine steps like consent, identity protection, human rights, professional ethics, etc., should be taken into consideration before venturing into teledermatology services too. All said and done, patients undergoing teledermatology care should be advised to present themselves for a personal consultation when an earliest favorable situation comes up at their disposal to ensure correctness and completeness of healthcare delivery. As mentioned earlier, it would be ideal to incorporate a disclaimer at the beginning of the consult, which would serve as both consent and an understanding of the limitation of teleconsultations.
Plus and minus of teledermatology services in published literature
Teledermatology has its own limitations. In a study conducted at Denmark by Vestergaard et al. found that teledermatology has the potential to diagnose suspicious skin lesions faster, limit the number of direct consultations, triage patients directly for surgical procedures, and provide meaningful feedback to the general practitioners but they also observed that the diagnostic accuracy of teledermatology was significantly lower than that of a face-to-face consultations in identifying benign and malignant conditions.[25]
There is always a risk of missing malignant skin conditions and hence this calls for extra caution and suggest that the doctor doing a teledermatology service has to keep this important point in mind.[26,27,28,29]
Tips, tricks and techniques
When telephonic dermatology consultations are done, the patient should be asked to send clear images on phone and after the discussion, they can be advised to go to the nearest pharmacy and revert once more. This helps increase correctness as the instructions can be verbally conveyed at ease to the pharmacy and even alternative medications can be suggested at ease
WhatsApp business account is one app that can be exploited for teledermatology consultations.[30,31] The advantage is that it can be installed on to the regular phone of the doctor without cluttering the personal WhatsApp account. The business account also has the advantage of setting automated replies to messages which can be used to convey information, instructions, and disclaimers about teledermatology consultations to anyone who connects. A tip for doctor using WhatsApp is to try the web version (WhatsApp web), which allows better visualization of the images, typing and easier attachment of documents, images
While prescribing via WhatsApp, the doctor can send across a regular prescription as an image (with official seal and signature), but clearly writing “Prescription sent on WhatsApp” somewhere on the top so that this is not confused with a regular consultation if something does not work out well later
Teleconsultation be it patient delivered, or assistant delivered should be scheduled for a particular day of the week or limited hours in a day only. This should not be at the cost of making oneself less available for face-to-face consults. In organizations with more manpower there can be a teledermatology OPD which is managed by consultants on rotation so that there is a system in place.
What is the way forward?
Now that the spark has come, telemedicine and teledermatology in India is here to stay and we hope it evolves for better. The COVID-19 pandemic might end up changing our way of life significantly. As in other aspects of life, this will lead to some unexpected positive offshoots in the practice of medicine too, like the increased use of telemedicine, artificial intelligence, and robotics. Dermatologists should use the opportunity to adopt the practice of teledermatology and harness its advantages. India is probably a bit late in using the full potential of teledermatology but as the saying goes “better late, than never.” This facility if used with caution, within its limitations and exploited to the fullest can definitely help to improve the reach and quality of dermatology care in India. Understandably, the present policies made in the context of the pandemic are likely to have loopholes and concerns. It would be important that once the pandemic settles down, the policies are reviewed and revised, Special interest groups for teledermatology, under the aegis of organizations like IADVL would need to be instituted. National professional societies like IADVL could itself take the lead in designing and implementing a teledermatology practice platform, with integration of electronic medical records and secure payment gateways. It would also be important to build consensus and bring the whole dermatology community on board. Official medical/dermatology associations would need to take inputs and suggestions from practicing dermatologists and devise a detailed, long term, standard operating procedures for teledermatology practice in future.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Acknowledgements
Figure 1a. Image courtesy of Dr. Sribiju. M.K. Consultant in Dermatology. Government Hospital of Dermatology. Chevayur, Calicut. Kerala.
Figure 1b and Figure 4. Images Courtesy of Dr. Soumya Jagadeesan. Consultant Dermatologist and Associate Professor. Department of Dermatology. Amrita Institute of Medical Sciences. Kochi. Kerala.
References
- 1.Coronavirus disease (COVID-19) Pandemic. [Last accessed on 2020 Apr 16]. Available from: https://wwwwhoint/emergencies/diseases/novel- coronavirus-2019 .
- 2.Verma S. Nonclinical challenges of Indian dermatology-cities vs. villages, poverty, and lack of awareness. Int J Dermatol. 2007;46(Suppl 2):42–5. doi: 10.1111/j.1365-4632.2007.03565.x. [DOI] [PubMed] [Google Scholar]
- 3.India has a doctor for every 10,189 people, finds WHO survey. [Last accessed on 2020 Apr 10]. Available from: https://indianexpress.com/article/india/who-health-index-doctor-patient-ratio-5842648/
- 4.India Population. [Last accessed on 2020 Apr 10]. Available from: https://wwwceicdatacom/en/indicator/india/population .
- 5.WHO. A health telematics policy in support of WHO's Health-For-All strategy for global health development: Report of the WHO group consultation on health telematics, 11–16 December, Geneva, 1997. Geneva: World Health Organization; 1998. [Google Scholar]
- 6.Telemedicine Practice Guidelines Enabling Registered Medical Practitioners to Provide Healthcare Using Telemedicine (25th March 2020) [Last accessed on 2020 Apr 09]. Available from: https://wwwmohfwgovin/pdf/Telemedicinepdf .
- 7.Kanthraj GR. Newer insights in teledermatology practice. Indian J Dermatol Venereol Leprol. 2011;77:276–87. doi: 10.4103/0378-6323.79696. [DOI] [PubMed] [Google Scholar]
- 8.Thomas J, Kumar P. The scope of teledermatology in India. Indian Dermatol Online J. 2013;4:82–9. doi: 10.4103/2229-5178.110579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dasgupta A, Deb S. Telemedicine: A new horizon in public health in India. Indian J Community Med. 2008;33:3–8. doi: 10.4103/0970-0218.39234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pasquali P, Sonthalia S, Moreno-Ramirez D, Sharma P, Agrawal M, Gupta S, et al. Teledermatology and its current perspective. Indian Dermatol Online J. 2020;11:12–20. doi: 10.4103/idoj.IDOJ_241_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feroze K. Teledermatology in India: Practical implications. Indian J Med Sci. 2008;62:208–14. [PubMed] [Google Scholar]
- 12.Kanthraj GR. Teledermatology: Its role in dermatosurgery. J Cutan Aesthet Surg. 2008;1:68–74. doi: 10.4103/0974-2077.44162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee I, Kovarik C, Tejasvi T, Pizarro M, Lipoff JB. Telehealth: Helping your patients and practice survive and thrive during the COVID-19 crisis with rapid quality implementation [published online ahead of print, 2020 Mar 27] J Am Acad Dermatol. 2020;S0190-9622(20):30472–2. doi: 10.1016/j.jaad.2020.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oldenburg R, Marsch A. Optimizing teledermatology visits for dermatologyresident education during the COVID-19 pandemic. J Am Acad Dermatol. 2020;S0190-9622(20):30520-X. doi: 10.1016/j.jaad.2020.03.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Advisory on online consultations in view of COVID-19. Available from: Circular No KMC/COVID/19/PR/03/2020 . Dated: 27032020.
- 16.Advisory on online consultations in view of COVID-19. Available from: TNMC Advisory on Telemedicine Dated: 26032020.
- 17.Advisory on online consultations in view of COVID-19. Available from: Circular No PMC/2020/2382 Dated: 23032020.
- 18.Advisory on regarding online consultations in view of COVID-19. Available from: Circular No GMC/7/3048/20 Dated: 24032020.
- 19.Advisory on online consultations in view of COVID-19. Available from: Order No: A1 6898/2020/TCMC Dated: 31032020.
- 20.Advisory on online consultations in view of COVID-19. Available from: Order No MPMC/Vividh/2020/2115 Dated: 23032020.
- 21.Online Consultation Guidelines (6th Apr 2020) [Last accessed on 2020 Apr 09]. Available from: https://iadvlorg/announcementsphpAnnouncementId=5e8ad48a9f2d29172f76952 .
- 22.COVID-19: TELEDERMATOLOGY. [Last accessed on 2020 Apr 11]. Available from: https://www.aad.org/member/practice/coronavirus/teledermatology .
- 23.COVID-19: Clinical guidelines for the management of dermatology patients remotely. [Last accessed on 2020 Apr 11]. Available from: https://wwwbadorguk/healthcare-professionals/covid-19/remote-dermatology-guidance .
- 24.Telemedicine Practice Guideline. [Last accessed on 2020 Apr 11]. Available from: https://tsiorgin/indexhtml .
- 25.Vestergaard T, Prasad SC, Schuster A, Laurinaviciene R, Andersen MK, Bygum A. Diagnostic accuracy and interobserver concordance: Teledermoscopy of 600 suspicious skin lesions in Southern Denmark [published online ahead of print, 2020 Feb 07] J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16275. [DOI] [PubMed] [Google Scholar]
- 26.Warshaw EM, Lederle FA, Grill JP, Gravely AA, Bangerter AK, Fortier LA, et al. Accuracy of teledermatology for pigmented neoplasms. J Am Acad Dermatol. 2009;61:753–65. doi: 10.1016/j.jaad.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 27.Borve A, Terstappen K, Sandberg C, Paoli J. Mobile teledermoscopy-there's an app for that! Dermatol Pract Concept. 2013;3:41–8. doi: 10.5826/dpc.0302a05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dahlen Gyllencreutz J, Paoli J, Bjellerup M, Bucharbajeva Z, Gonzalez H, Nielsen K, et al. Diagnostic agreement and interobserver concordance with teledermoscopy referrals. J Eur Acad Dermatol Venereol. 2017;31:898–903. doi: 10.1111/jdv.14147. [DOI] [PubMed] [Google Scholar]
- 29.Warshaw EM, Lederle FA, Grill JP, Gravely AA, Bangerter AK, Fortier LA, et al. Accuracy of teledermatology for nonpigmented neoplasms. J Am Acad Dermatol. 2009;60:579–88. doi: 10.1016/j.jaad.2008.11.892. [DOI] [PubMed] [Google Scholar]
- 30.WhatsApp business. [Last accessed on 2020 Apr 10]. Available from: https://wwwwhatsappcom/business .
- 31.Kaliyadan F, Ashique KT, Jagadeesan S, Krishna B What's up dermatology. A pilot survey of the use of WhatsApp in dermatology practice and case discussion among members of WhatsApp dermatology groups. Indian J Dermatol Venereol Leprol. 2016;82:67–9. doi: 10.4103/0378-6323.171638. [DOI] [PubMed] [Google Scholar]


