Abstract
Background:
Acne scarring commonly seen in young adults causes marked psychological distress. Commonly used procedural treatments for post-acne scarring have limited efficacy. This prospective, randomized study was undertaken to evaluate the efficacy and adverse effects offractional CO2 laser, microneedling, and platelet-rich plasma (PRP) in post-acne scarring.
Materials and Methods:
Sixty clinically diagnosed cases of post-acne scarring of both sexes were enrolled and divided into three groups of 20 patients each. The severity of scarring was graded as per the qualitative and quantitative grading system proposed by Goodman and Baron. Group A, B, and C patients were treated with fractional CO2 laser, microneedling, and PRP,respectively, at monthly intervals for foursessions. Improve men tin quantitative and qualitative grades of scars and adverse effects were noted at each session and 1 month after the final sitting. Statistical analysis was done using Student 't' test for quantitative values and Chi square test for qualitative values.
Results:
At the end of foursessions, based on mean percentage of improvement in quantitative grade, the efficacy of fractional CO2 laser is significantly greater than that of PRP (P = 0.00), while CO2 laser and microneedling did not show significant difference (P = 0.106). Based on qualitative scores, fractional CO2 laser group showed statistically higher therapeutic efficacy compared to microneedling and PRP (P = 0.00).No significant adverse effects were encountered in any groups.
Conclusion:
Fractional CO2 laser resurfacing is more efficacious than microneedling and PRP. Unsatisfactory results were obtained with PRP as monotherapy in post-acne scarring.
Keywords: Fractional CO2 laser, microneedling, post acne scaring, platelet-rich plasma
Introduction
Post-acne scarring is one of the most common causes of disfiguring scars over the face.[1,2] Recent epidemiological studies have shown that nearly 80% of patients with acne have some scarring and 50% have clinically relevant scarring.[3] Acne scaring is commonly seen in adolescence and young adults causing marked psychological distress. Dermatology life quality index (DLQI) in these patients is significantly lower than in patients without scars.[4]
Acne scars respond poorly to medical treatment and achieving an acceptable level of patient satisfaction remains a challenge. The commonly used procedural treatments for post-acne scarring have limited efficacy and a single effective and definitive solution for acne scarring is still lacking.[5] Fractional CO2 laser, microneedling, and platelet-rich plasma (PRP) are newer promising modalities in the management of post-acne scarring.[6] This comparative study was undertaken to evaluate the efficacy and adverse effects of fractional CO2 laser resurfacing, microneedling, and PRP in post-acne scarring.
Material and Methods
This study was carried out in 60 patients who attended the outpatient department of dermatology at a suburban medical college hospital. It was a prospective, randomized, comparative interventional study carried out over a period of 18 months from January 2016 to June 2017 after being approved by Institutional Ethics Committee. The sample size was calculated by difference of means formula. To achieve a power of study of 80% and precision alpha of 0.05 with a 95% confidence interval (CI), the estimated sample size per group was determined to be 20.
Clinically diagnosed cases of post-acne scarring of both sexes in the age range of 16–45 years who had not used any treatment for scarring in the last 6 weeks were enrolled. Patients with active acne, active infections, keloida l tendency, pregnant and lactating females were excluded.
After taking informed consent, general demographic data regarding age, sex, and contact information were noted. Detailed history was taken regarding duration of disease and previous treatment modalities, odermatological examination was done in all patients taking note of the various clinical types of scar, extent of scaring, and pigmentary alterations. At the time of enrolment, patients were assessed clinically by a single trained dermatologist to grade the severity of scarring, as per qualitative and quantitative grading system proposed by Goodman and Baron.[7,8]
Complete hemogram, coagulation profile, and viral screening were performed in all patients. Patients were divided into three groups of 20 patients each: group A, B, and C. Randomized table provided by a statistician for the generation of the randomization sequence was used for group allocation. In patients of all groups, topical eutectic anesthetic cream was applied under occlusion for 60 min over the treated area to achieve adequate analgesia.
Group A patients were treated with fractional CO2 laser unit MORE-XEL SCANNING (Bison medicals). In the first session, fluence of 18 J/cm2 was used at a density of 100 MTZ/cm2, single pass providing energy of 18mJ with spot size 70μm 49 pixel. Parameters were increased in subsequent sittings based on treatment response and patient tolerability upto a maximum fluence of 22 J/cm2, density of 150 MTZ/cm2, double pass providing maximum energy of 44 mJ.
Group B patients were treated with microneedling device, dermaroller-T (Lazhoramedical cosmetics, Chennai). It had needles 1.5 mm long, 192 needles in 8 rows, needle diameter at penetration point: 0.25 mm, width and diameter of the roller head: 20 mm. The treatment area was rolled in four directions (vertical, horizontal, and in both diagonal directions) applying minimal pressure till uniform bleeding points appeared over the scarred area. The treated skin was stretched in a perpendicular direction to the dermaroller movement for achieving better penetration. Moist gauge was applied over the treated area to achieve hemostasis.
Group C patients were treated with PRP using meso therapy technique. Whole blood was withdrawn into acid citrate dextrose (ACD) tubes and centrifuged using a “soft” spin (160g for 10 min). The supernatant plasma containing platelets was transferred into another sterile tube (without anticoagulant) to a higher speed centrifugation (a hard spin, i.e., 400g for 20 min) for obtaining platelet concentrate. After discarding the upper 2/3rd platelet-poor plasma (PPP), lower 1/3rd PRP is mixed with 10% calcium chloride for activation. This activated fluid was then injected intradermally using insulin syringe using meso therapy technique, all over the scarred area.
Patients in all groups were subjected to the respective treatments at monthly intervals for four sessions. Photographic documentation was done before and after each treatment session. Improvement in quantitative and qualitative grading of scars, adverse effects, and recovery times after every session were noted. Final quantitative and qualitative grading was done 1 month after the final sitting in all the patients.
Quantitative data collected from all patients in each group were tabulated and analyzed using appropriate statistical methods with SPSS 16.0.2. Statistical analysis was done using Student “t” test for quantitative values and Chi square test for qualitative values. The significance of the outcome of the study was assessed by calculating the “P” value and a value less than 0.05 was taken as significant.
Results
In the present study, 42 (70%) patients were males and 18 (30%) patients were females with a male to female ratio of 2.3:1. Majority of the cases belonged to 18–24 years age group (n = 37, 61.6%) followed by 25–31 years age group (n = 19, 31.6%) with mean age of 25.4 years. Duration of acne scars was 3–4 year sin 28 patients (46.6%) and 5–6 years in 19 patients (31.6%) with a mean duration of 3.5 years.
Out of the 60 patients, involvement of cheeks was seen in 40 cases (66.6%), cheeks and forehead were involved in 17 cases (28.3%), whereas cheeks and chin were involved in three cases (5%). Combination of ice pick, rolling, and boxcar scars were seen in 16 (26.6%) patients, followed by combination of rolling, boxcar scars, and linear scars in 14 (23.3%) and predominantly boxcar scars in 12 (20%) patients. Combination of ice pick, rolling, boxcar, and linear scar were seen in 10 patients (16.6%), where a spredominant rolling and boxcar scars were seen in 8 (13.3%) patients.
Determination of pretreatment Goodman and Baron quantitative score showed a score between 49 and 60 in 19 patients followed by 14 patients (23.3%) each with a score of 37–48 and 61–72. Assessment of pretreatment Goodman and Baron qualitative grading of acne scars showed 37, 19, and 4 cases had grade 2, grade 3, and grade 4, respectively.
Of the 60 patients who were enrolled, a total of 51 completed the study. In CO2 laser group, no patients were lost to follow-up. Mean percentage of improvement in quantitative score for all 20 cases was 47.1% after 2nd sitting and 68.7% after 4th sitting [Figure 1]. In this group, pretreatment qualitative grade 2, 3, and 4 were seen in 5, 14, and 1 patient, respectively. After 4 sessions of CO2 laser treatment, grade 1 severity was seen in 19 patients and grade 2 in 1 patient only. Hence, at the end of four sessions, five patients had improvement of one grade whereas 15 patients showed 2 grades of improvement.
Figure 1.
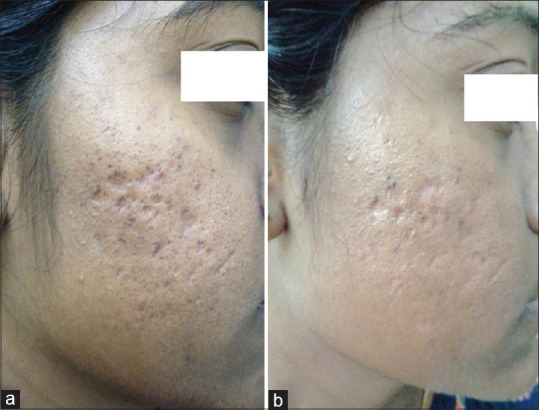
(a) Grade 3 acne scars (b) improvement in acne scars from grade 3 to grade 2 after four sessions of fractional CO2 laser treatment
In patients treated with microneedling, 17 patients completed the study and 3 cases were lost to follow-up. In this group, mean percentage of improvement in quantitative score was 41.9% after 2nd sitting and 60.3% after 4th sitting [Figure 2]. Pretreatment qualitative grade 2, 3, and 4 were seen in 7, 11, and 2 patients, respectively. After 4 sessions, grade 1 severity was seen 14 patients and grade 2 was seen in 3 patients. Hence, at the end of 4 sessions, 7 patients had improvement of one grade whereas 10 patients showed 2 grades of improvement.
Figure 2.
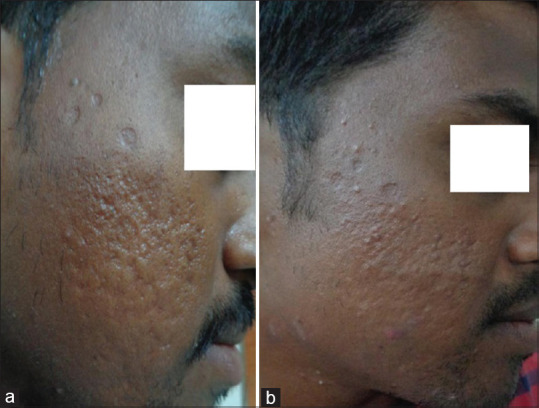
(a) Grade 3 acne scars (b) improvement in acne scars from grade 3 to grade 2 after four sessions of microneedling treatment
In the PRP group, six cases were lost to follow-up. The platelet concentration attained after double spin ranged from 800,000 to 10,00,000 platelets/ml of blood. In this group, mean percentage of improvement in quantitative score for 14 cases was 13.6% after 2nd sitting and 31.1% after 4th sitting [Figure 3]. Pretreatment qualitative grade 2, 3, and 4 were seen in 7, 12, and 1 patient, respectively. After four sessions of PRP treatment, number of patients with grade 1, 2, 3, and 4 severity were 2, 7, 4, and 1, respectively. Hence, at the end of four sessions, four patients had improvement of one grade, whereas 10 patients did not show any improvement in qualitative grade.
Figure 3.
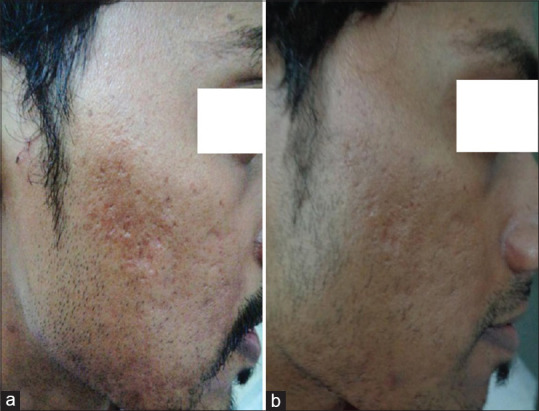
(a) Grade 3 acne scars (b) improvement in acne scars from grade 3 to grade 2 after four sessions of PRP treatment
On comparing the efficacy of all the three treatment modalities, based on mean percentage of improvement in Goodman and Baron quantitative grades, the efficacy offractional CO2 laser was significantly greater than that of PRP (P = 0.00), whereas statistically significant difference in efficacy was not observed between CO2 laser and microneedling (P = 0.106) [Table 1]. On comparing the efficacy of all the three treatment modalities based on Goodman and Baron qualitative grades, fractional CO2 laser showed significantly higher efficacy than microneedling and PRP (P = 0.00) [Table 2]. Based on the morphological types of scars, highest improvement in rolling scars was seen with microneedling (62%) followed by CO2 laser (57%) whereas highest improvement in boxcarscars was seen with CO2 laser (66%) followed by microneedling (54%). No significant improvement was noticed in ice pick scars in patients of all three groups.
Table 1.
Comparison of efficacy of all treatments based on Goodman & Baron quantitative grading
| Groups | Mean % of improvement in quantitative score (after 4 sessions) | t | P | Decision |
|---|---|---|---|---|
| CO2 laser | 68.7%±10.5 | |||
| Microneedling | 60.3%±14.5 | 1.662 | 0.106 | Not significant |
| PRP | 31.1%±6.7 | 5.809 | 0.000 | Significant |
Table 2.
Comparison of efficacy of all treatments based on Goodman & Baron qualitative grading
| Groups | Posttreatment | Chi-square | P | Decision | |
|---|---|---|---|---|---|
| Grade 1,2 | Grade 3,4 | ||||
| CO2 laser | 20 | 0 | 24.913 | 0.000 | Significant |
| Microneedling | 17 | 0 | |||
| PRP | 5 | 9 | |||
In CO2 laser group, posttreatment erythema and edema was seen in 10 patients which was transient and subsided in 3–4 days duration. The only significant adverse effect observed was persistent crusting and post-inflammatory hyperpigmentation (PIH) in four cases which resolved with topical therapy in 6 weeks [Figure 4]. Post-procedural pain and discomfort were the only transient adverse effects seen in microneedling group which lasted for few hours. Bruise and hematoma formation was seen in three patients treated with PRP which was self-limiting and resolved without any treatment [Table 3].
Figure 4.
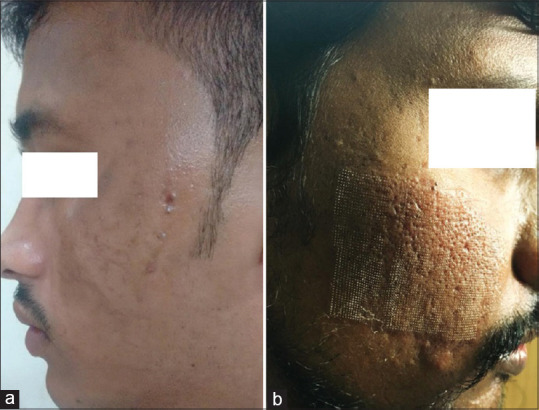
Adverse effects seen following fractional CO2 laser treatment (a) transient post-inflammatory hyperpigmentaion (b) transient erythema and edema
Table 3.
Adverse effects observed in the three treatment groups
| Adverse effect | CO2 laser | Microneedling | PRP |
|---|---|---|---|
| Erythema and edema | 10 | 5 | 0 |
| PIH | 4 | 1 | 0 |
| Pain | 7 | 10 | 10 |
| Bruises/hematoma | 0 | 0 | 3 |
| Persistent crusting | 4 | 0 | 0 |
Discussion
Post-acne scarring usually follows deep inflammatory lesions; but can also occur after superficial lesions in patients prone for scarring. The main cause of post-acne scarring is the formation of compromised collagen occurring during the natural wound healing process.[3] Acne scars are polymorphic and different type of scars can occur in the same patient. The different morphological types of acne scars respond variably to the available treatment modalities. The morphology of scars must be assessed and treatment should be planned based on the types of scars, overall appearance, and expectations of the patient. All these factors make the assessment of efficacy of any therapeutic option difficult to judge across all the patients.[1,3]
In present study, higher prevalence of acne scarring was seen in males (n = 42; 70%) compared to females (n = 18; 30%), which is in accordance with previous studies conducted by Chawla S et al. and Qian et al.[9,10] Male gender has been reported asan independent risk factors for acne scars previously.[3] Half of the patients (49.9%) had mixed type of scarring- combination of rolling, boxcar, linear, and ice pick scars. The morphological type of scars seen in each individual has therapeutic importance as fractional laser resurfacing, microneedling, and PRP have good efficacy in rolling scars and superficial boxcar scars, especially if combined with intermittent subcision treatments. In patients with predominant ice pick scars, the above treatments are unlikely to be very effective and supplementary treatment with trichloracetic acid CROSS (chemical reconstruction of scars) or punch excision or punch flotation are needed.[11]
In the present study, in the CO2 laser group, mean improvement in quantitative score after 4 sittings was 68.7%. Taking qualitative score into consideration, after 4 sitting of treatment, 15 patients and 5 patients achieved improvement by 2 grades and 1 grade, respectively. Similar observations of significant improvement in post-acne scarring after fractional CO2 resurfacing was reported by Imran Majid et al. and Omi T et al.[12,13] Fractional lasers treat only a “fraction” or a column of the affected skin leaving intervening areas of skin untreated. These untreated areas help in rapidre-epithelization of the skin, minimizing the chances of prolonged and serious adverse effects. In addition, the enormous heat generated during ablative fractional carbon dioxide laser treatment can remove dermal tissue and bring about tissue shrinkage in the adjacent dermal collagen accompanied by collagen remodeling and skin tightening.
The mean improvement in quantitative score was 60.3%after 4 sittings in microneedling group. Out of the 17 patients who completed the study, 7 patients had improvement of one grade and 10 patients showed 2 grades of improvement in qualitative grades. Intense procedural pain might be the reason for 3 patients being lost to follow-up. Significant improvement in post-acne scaring after microneedling was reported by Dogra Set al., Alster TS et al., and Ibrahim MK et al.[14,15,16] Microneedling is a technique that involves using a sterile dermaroller that punctures the skin with a series of fine sharp needles. The skin develops multiple microbruises in the dermis that initiate a complex cascade of wound healing and growth factors release, and finally results in collagen production.
In the patients who were subjected to PRP, at the end of 4 sittings, 31.1% improvement in quantitative score was seen; 4 patients had improvement of one grade whereas 10 patients did not show any improvement in qualitative grades. Higher number of dropouts (6 cases) in this group may be due to minimal reduction in scarring and invasive nature of treatment. Forpost-acnescarring, PRP as mono therapy has been employed in few studies and most of the previous studies have shown satisfactory results when PRP was used in combination with other modalities such as CO2 laser and microneedling.[17,18,19,20] Though relatively lower level of improvement in post-acne scarring was noticed in our study with PRP mono therapy, Nofal et al. and Asif M et al. have shown significant improvement in post-acne scarring when it was combined with other modalities.[17,18] PRP containing platelets in concentrated plasma release various cytokines and growth factors such as vascular endothelial growth factor, platelet-derived growth factor, epidermal growth factor, fibroblast growth factor, transforming growth factor-β, insulin-like growth factor, IL-8, etc., that promote angiogenesis, tissue remodeling, and wound healing.
In the present study, preparation of PRP was done using double spin method. The same method was used in studies by Nofal et al. and Chawla S et al.[9,17] Regardless of the rate of centrifugation or the time of centrifugation, a single spin cannot adequately concentrate platelets because the red blood cells will interfere with the fine separation of the platelets.[21]
Our study clearly demonstrates that fractional CO2 laser is a safe and effective treatment for post-acnescarring. It is significantly more effective than PRP, based on both quantitative and qualitative grades. Gratifying results canbe achieved with fractional CO2 laser when it is combined with intermittent sessions of subcision, especially for rolling and superficial boxcar scars. The difference in efficacy between fractional CO2 laser and micro needling was seen only with qualitative grades. In resource poor settings with no access to good quality fractional CO2 laser machine, micro needling is areas on able alternative which can also be combined with subcision. Long erintervalsin between sessions is advisable for microneedling as the process of neocollagenes is takes place over 6–8 weeks. Significant adverse effects warranting stopping the treatment were not encountered in all the three groups. Most adverse effects such as crusting, PIH in fractional CO2 laser group and bruising, pain in PRP group were transient and self-limiting.
Limitation
In the present study, PRP was administered by meso therapy and not with the use of a dermaroller. This couldbe one of the factors responsible for the lower efficacy of PRP.
Conclusion
Fractional CO2 laser resurfacing is more efficacious than microneedling and PRP but slightly longer down time is the only limiting factor. Microneedling has excellent safety profile but is relatively less effective than CO2 laser. PRP asmonotherapy in post-acne scarring is not advisable as results are unsatisfactory. Treatments that can completely resolve acne scars are not yet available. Institution of aggressive and effective therapy for inflammatory acne remains the key strategy to prevent post acne scarring.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Layton AM, Eady EA, Zouboulis CC. Acne. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, editors. Rook's Textbook of Dermatology. 9th ed. Oxford: Wiley Blackwell; 2016. pp. 901–65. [Google Scholar]
- 2.Vaishampayan S, Baveja S, Garg S. Acne, Rosacea and perioral dermatitis. In: Sacchidan S, Oberai C, Inamdar AC, editors. IADVL Text Book of Dermatology. 4rd ed. Mumbai: Bhalani Publishing House; 2015. pp. 1365–412. [Google Scholar]
- 3.Leyden JJ. Understanding and reducing the risk for acne scarring. Semin Cutan Med Surg. 2015;34:S89–91. doi: 10.12788/j.sder.2015.0164. [DOI] [PubMed] [Google Scholar]
- 4.Hayashi N, Miyachi Y, Kawashima M. Prevalence of scars and AND “mini-scars” AND, and their impact on quality of life in Japanese patients with acne. J Dermatol. 2015;42:690–6. doi: 10.1111/1346-8138.12885. [DOI] [PubMed] [Google Scholar]
- 5.Tan J, Kang S, Leyden J. Prevalence and risk factors of acne scarring among patients consulting dermatologists in the Unites States. J Drugs Dermatol. 2017;16:97–102. [PubMed] [Google Scholar]
- 6.Leo MS, Kumar AS, Kirit R, Konathan R, Sivamani RK. Systematic review of the use of platelet-rich plasma in aesthetic dermatology. J CosmetDermatol. 2015;14:315–23. doi: 10.1111/jocd.12167. [DOI] [PubMed] [Google Scholar]
- 7.Goodman GJ, Baron JA. Postacne scarring- a quantitative global scarring grading system. J Cosmet Dermatol. 2006;5:48–52. doi: 10.1111/j.1473-2165.2006.00222.x. [DOI] [PubMed] [Google Scholar]
- 8.Goodman GJ, Baron JA. Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458–66. doi: 10.1111/j.1524-4725.2006.32354.x. [DOI] [PubMed] [Google Scholar]
- 9.Chawla S. Split face comparative study of microneedling with PRP versus microneedling with vitamin C in treating atrophic post acne scars. J Cutan Aesthet Surg. 2014;7:209–12. doi: 10.4103/0974-2077.150742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qian H, Lu Z, Ding H, Yan S, Xiang L, Gold MH. Treatment of acne scarring with fractional CO2 laser. J Cosmet Laser Ther. 2012;14:162–5. doi: 10.3109/14764172.2012.699679. [DOI] [PubMed] [Google Scholar]
- 11.Lee J, Chung WG, Kwahck H, Lee KH. Focal treatment of acne scars with trichloracetic acid: Chemical reconstruction of skin scars method. Dermatol Surg. 2002;28:1017–21. doi: 10.1046/j.1524-4725.2002.02095.x. [DOI] [PubMed] [Google Scholar]
- 12.Majid I, Imran S. Fractional CO2 laser resurfacing as monotherapy in the treatment of atrophic facial acne scars. J Cutan Aesthet Surg. 2014;7:87–92. doi: 10.4103/0974-2077.138326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Omi T, Kawana S, Sato S, Bonan P, Naito Z. Fractional CO2 laser for the treatment of acne scars. J Cosmet Dermatol. 2011;10:294–300. doi: 10.1111/j.1473-2165.2011.00587.x. [DOI] [PubMed] [Google Scholar]
- 14.Dogra S, Yadav S, Sarangal R. Microneedling for acne scars in Asian skin type: An effective low cost treatment modality. J Cosmet Dermatol. 2014;13:180–7. doi: 10.1111/jocd.12095. [DOI] [PubMed] [Google Scholar]
- 15.Alster TS, Graham PM. Microneedling: A review and practical guide. Dermatol Surg. 2018;44:397–404. doi: 10.1097/DSS.0000000000001248. [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim MK, Ibrahim SM, Salem AM. Skin microneedling plus platelet-rich plasma versus skin microneedling alone in the treatment of atrophic post acne scars: A split face comparative study. J Dermatolog Treat. 2017;26:1–6. doi: 10.1080/09546634.2017.1365111. [DOI] [PubMed] [Google Scholar]
- 17.Nofal E, Helmy A, Nofal A, Alakad R, Nasr M. Platelet-rich plasma versus CROSS technique with 100% trichloroacetic acid versus combined skin needling and platelet rich plasma in the treatment of atrophic acne scars: A comparative study. Dermatol Surg. 2014;40:864–73. doi: 10.1111/dsu.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 18.Asif M, Kanodia S, Singh K. Combined autologous platelet-rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: A concurrent split-face study. J Cosmet Dermatol. 2016;15:434–43. doi: 10.1111/jocd.12207. [DOI] [PubMed] [Google Scholar]
- 19.Faghihi G, Keyvan S, Asilian A, Nouraei S, Behfar S, Nilforoushzadeh MA. Efficacy of autologous platelet-rich plasma combined with fractional ablative carbon dioxide resurfacing laser in treatment of facial atrophic acne scars: A split-face randomized clinical trial. Indian J Dermatol Venereol Leprol. 2016;82:162–8. doi: 10.4103/0378-6323.174378. [DOI] [PubMed] [Google Scholar]
- 20.Gawdat HI, Hegazy RA, Fawzy MM, Fathy M. Autologous platelet rich plasma: Topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg. 2014;40:152–61. doi: 10.1111/dsu.12392. [DOI] [PubMed] [Google Scholar]
- 21.Marx R. Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent. 2001;10:225–8. doi: 10.1097/00008505-200110000-00002. [DOI] [PubMed] [Google Scholar]


