Abstract
Secondary syphilis can present with wide range of mucocutaneous lesions. Because of its varied morphology, it is considered a great mimicker. However, syphilitic lesions presenting as Sweet syndrome is uncommon. We report a case of a 28 year adult male presenting with erythematous edematous papules and plaques with pseudovesicular appearance, lichenoid annular plaques on skin, and painless indurated ulcer over the glans. The Venereal Disease Research Laboratory test was reactive (1:32 dilutions), and treponema pallidum hemagglutination test was positive. The histopathology from erythematous edematous lesion and genital ulcer revealed neutrophilic abscess and characteristic plasmacytic picture in biopsy, respectively. He was treated successfully with single dose intramuscular injection of benzathin penicillin 2.4 million units. This case is reported for its rarity.
Keywords: Immunocompetent individual, perifollicular pustules, secondary syphilis, sweet syndrome
Introduction
Syphilis is a great mimicker with wide range of clinical presentations. The varied morphology of skin and mucosal lesions can delay diagnosis and treatment. The most common clinical presentation is generalized non-pruritic symmetrically distributed papulo-squamous eruptions.[1] The less commonly described presentations of secondary syphilis may resemble pityriasis rosea, lichen planus, sarcoidosis, granuloma annulare, and subacute cutaneous lupus erythematous.[2] Lesions of secondary syphilis mimicking Sweet syndrome has been described rarely.[3,4] We report a case of secondary syphilis with Sweet syndrome like lesions in an immunocompetent individual.
Case Report/s
A 28 year unmarried male presented with reddish lesions over the body since 15 days. He complained of mild fever and pain in the ankle and knee joints. The skin lesions were of varied morphologies which included erythematous edematous papules and plaques with pseudovesicular look on the trunk [Figure 1 and 2], annular erythematous to violaceous plaques over face and hair margins [Figure 3a], non-tender pigmented annular plaques with collarette of scales over palm and soles [Figure 3b], and pale non-tender erythematous indurated plaques with surface erosion over glans and ill-defined scaly lesions on the shaft of penis [Figure 3c]. Other mucosa and mucocutaneous junctions showed no abnormality. There were no enlarged lymph nodes. He gave a history of unprotected penetrative sexual contact with commercial sex worker 1 month prior to the appearance of skin and genital lesions. There was no sensory or motor abnormality. On the basis of history and clinical features, clinical diagnosis of secondary syphilis and Sweet syndrome were made. Routine hematological and biochemical investigations were within normal limits. Venereal Disease Research Laboratory test was reactive with 1:32 titer, treponema pallidum hemagglutinition test was positive. HIV, HCV, and HBsAg screening tests were negative. Biopsy from the genital ulcer showed irregular papillomatosis and dense lymphoplasmocytic infiltration [Figure 4] and from the edematous skin lesions showed perifollicular neutrophilic abscess with neutrophilic exocytosis along with lymphoplasmocytic reaction [Figure 5]. Thus, a final diagnosis of secondary syphilis was made. Patient was treated with single intramuscular injection of benzathine penicillin 2.4 million units after negative skin sensitivity test and was counselled regarding possible hazards of sexual contact with unknown and un-reliable partner along with change of sexual behavior. All lesions healed leaving post-inflammatory pigmentation over 2 weeks. There is no recurrence during the last 9 months follow-up and the Venereal Disease Research Laboratory test became non-reactive at the end of 9 months.
Figure 1.

Erythematous edematous papules and plaques with pseudovesicular look on the trunk and chest
Figure 2.

Close-up view of skin lesions showing erythematous edematous papules and plaques
Figure 3.

(a) Annular erythematous to violaceous plaques over face and hair margins; (b) tender pigmented annular plaques with collarette of scales over palm and soles; (c) pale non-tender erythematous indurated ulcers over glans and ill-defined scaly lesions on the shaft of penis
Figure 4.
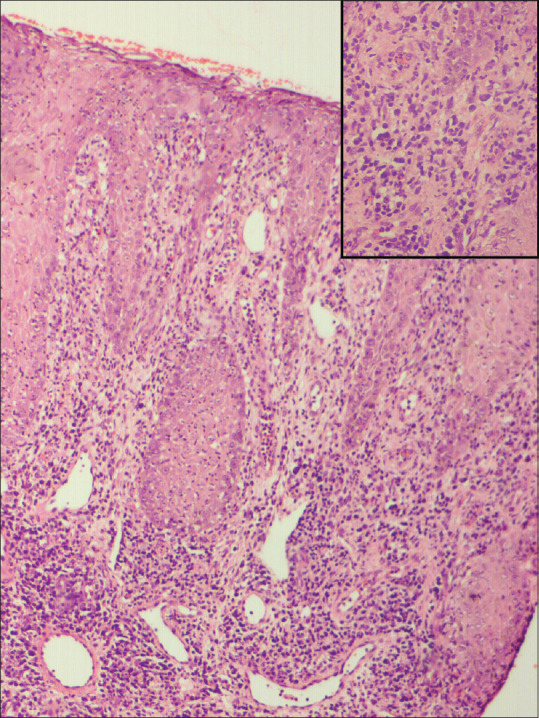
Biopsy from genital lesion showing irregular papillomatosis and dense lymphoplasmocytic infiltration [H and E; 100×], inset showing lymphoplasmacytic infiltration [H and E; 400×]
Figure 5.

Biopsy from edematous skin lesions showed perifollicular neutrophilic abscess with neutrophilic exocytosis along with lymphoplasmocytic reaction [H and E; 100×], inset showing neutrophilic infiltration [H and E; 400×]
Discussion
The incidence of secondary syphilis has drastically increased in the last decades because of emergence of HIV infection and change in life style. There are reports of atypical presentation of secondary syphilis, mostly in association with HIV co-infection. Atypical lesions mimicking other dermatoses can pose a diagnostic challenge for physicians, and there can be delay in diagnosis and treatment of secondary syphilis.
Secondary phase of syphilis is typically characterized by well to ill-defined erythematous non-pruritic papulosquamous eruptions of localized or generalized nature, with predilection for palms and soles. Other rarely described morphologies include nodular, lichenoid, annular, framboesa form, and nodulo-ulcerative lesions (lues maligna).[2,5] It may be associated with systemic features.
Secondary syphilis with pseudovesicular lesions and neutrophilic inflammation in histopathology has been described rarely, and only one of the previously reported cases was in an immunocompetent individual.[3,4]
Histology of syphilis lesion with subcorneal and intrafollicular collection of neutrophils is reported in pustular lesions of syphilis, known as syphiloderma pustulosum, characterized by follicular based pustules that heal with crusting and scar formation.[1,6] In the present case, the edematous papules and plaques mimicking Sweet syndrome also had histological features of irregular papillomatosis, dense lymphoplasmocytic infiltration, and perifollicular neutrophilic abscess with neutrophilic exocytosis along with lymphoplasmocytic reaction. This is interesting as the morphological appearance was different from the previously described lesions and the lesions healed without scarring.
Secondary syphilis is diagnosed on the basis of clinical suspicion because of the presence of characteristic skin and mucous lesions and confirmation by serologic tests that measure nontreponemal and treponemal antibodies. Treatment of choice remains benzathine penicillin G. Our case was also diagnosed from positive serology and was treated successfully with the standard dose of benzathine penicillin.[7,8]
Sweet syndrome requires to be differentiated from the secondary syphilis with Sweet syndrome like lesions. Diagnostic criteria for Sweet syndrome should fulfill one major and at least 2 minor criteria. Major criteria include abrupt onset of typical cutaneous lesions and consistent histopathology. Minor criteria include antecedent fever or infection; accompanying fever, arthralgias, conjunctivitis, or underlying malignancy; leukocytosis; and good response to systemic corticosteroids with no response to antibiotics.[9]
Our case had lesions with pseudovesicular look without any frank pustules mimicking Sweet syndrome clinically, but histopathology showed intrafollicular pustules (in addition to lymphoplasmacytic infiltration), and constitutional features fever, arthralgia, and antecedent infection; thus, fulfilling two of the major and two minor criteria for Sweet syndrome. Our case also had annular lichenoid plaques at hair margins and palms and soles, which were clues to the diagnosis of secondary syphilis. The non-tender pale indurated ulcers on the glans along with lesions of secondary syphilis suggest the transition between resolution of primary stage and initiation of secondary stage. Authors postulate the Sweet syndrome like morphology could be owing to endarteritis causing vascular damage and extravasation causing edema on the lesional site.
We report this case for its rare morphological presentation as pseudovesicular lesions mimicking Sweet syndrome clinically and unusual histopathological features of perifollicular neutrophilic abscess. This case is reported to bring awareness among the physicians to the fact that Sweet syndrome like lesions may be one of the varied morphological presentations of secondary syphilis which is aptly regarded as the great mimicker.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.De CarvalhoFagundes FN, Simoes JP, Pereira Magnago AG, De Sousa Brito Xavier MH. Annular and arcuate syphilis: An uncommon presentation of disseminated secondary syphilis. Dermatol Online J. 2018;24:5. [PubMed] [Google Scholar]
- 2.Balagula Y, Mattei PL, Wisco OJ, Erdag G, Chien AL. The great imitator revisited: The spectrum of atypical cutaneous manifestations of secondary syphilis. Int J Dermatol. 2014;53:1434–41. doi: 10.1111/ijd.12518. [DOI] [PubMed] [Google Scholar]
- 3.Jordaan HF, Cilliers J. Secondary syphilis mimicking Sweet's syndrome. Br J Dermatol. 1986;115:495–6. doi: 10.1111/j.1365-2133.1986.tb06244.x. [DOI] [PubMed] [Google Scholar]
- 4.Johnson LE, Armstrong AW, Dezube BJ, Tahan SR, Gold HS. Images in HIV/AIDS. Sweet syndrome and syphilis in an HIV-infected person. AIDS Read. 2008;18:134–5. [PubMed] [Google Scholar]
- 5.Pradhan S, Sirka CS, Panda M, Baisakh M. Lues maligna in an immunocompetent female. Indian Dermatol Online J. 2018;9:344–6. doi: 10.4103/idoj.IDOJ_277_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kazlouskaya V, Wittmann C, Tsikhanouskaya I. Pustular secondary syphilis: Report of three cases and review of the literature. Int J Dermatol. 2014;53:e428–31. doi: 10.1111/ijd.12337. [DOI] [PubMed] [Google Scholar]
- 7.Lautenschlager S. Cutaneous manifestations of syphilis: Recognition and management. Am J Clin Dermatol. 2006;7:291–304. doi: 10.2165/00128071-200607050-00003. [DOI] [PubMed] [Google Scholar]
- 8.Dupin N, Farhi D. Syphilis. Presse Med. 2013;42:446–53. doi: 10.1016/j.lpm.2012.09.024. [DOI] [PubMed] [Google Scholar]
- 9.Su WP, Liu HN. Diagnostic criteria for Sweet's syndrome. Cutis. 1986;37:167–74. [PubMed] [Google Scholar]


