Abstract
Hydroxychloroquine is one of the most frequently used drugs in dermatology with a wide variety of uses due to its immunomodulatory, anti-inflammatory, photoprotective, and metabolic actions and low side effect profile. Demonstration of its antiviral action in vitro has led to renewed interest by physicians worldwide during the ongoing coronavirus disease of 2019 (COVID-19) pandemic. Like its immunomodulatory action, its antiviral activity is also due to its ability to alkalinize the intracytoplasmic milieu, leading to disordered viral entry/fusion and deranged viral protein synthesis. However, randomized controlled trials are the need of the hour to conclusively determine its clinical efficacy in such infections. A review of the multitude of mechanisms of action, updated screening and monitoring guidelines, drug interactions, side effects, and its use in special populations is described.
Keywords: arrhythmias, cardiotoxicity, COVID-19, dermatology, hydroxychloroquine, lupus, mechanism, retinopathy, side effects, uses
Introduction
Although Payne is credited with the first use of quinine for the treatment of discoid lupus erythematosus (DLE), the formal efficacy of the drug has been ascribed to Page who used quinacrine (mepacrine) in DLE, systemic lupus erythematosus (SLE), and rheumatoid arthritis (RA).[1] We will focus on hydroxychloroquine (HCQ) in this article.
HCQ has been used successfully to treat a number of dermatological disorders, and new uses continue to be found even today, most notably, its antiviral effect has been rediscovered, making it a much sought after drug by governments worldwide. We seek to review its effects and safety profile while detailing its relevance in the current coronavirus disease of 2019 (COVID-19) pandemic.
History of Antimalarials in Dermatology
All the antimalarials used in LE and RA are quinine derivatives and have a common 4-aminoquinoline radical.
Some of the quinine derivatives used in Dermatology are listed in Table 1.
Table 1.
List of common quinine derivatives
| Class of drug | Examples |
|---|---|
| 4-aminoquinalines* | Chloroquine, hydroxychloroquine, amodiaquine, and pyronaridine |
| Acridine compounds (4-aminoquinolines with benzene ring)* | Quinacrine (mepacrine) |
| Cinchona alkaloids* | Quinine, quinidine |
| 8-aminoquinolines | Primaquine, tafenoquine, and bulaquine |
| Quinolone methanol | Mefloquine |
*Quinine derivatives that have been or are used in Dermatology
Cinchona bark was serendipitously discovered to be effective in treatment of malaria in 1634. It took almost 200 years for quinine to be identified as the main antimalarial component in cinchona bark in 1820 by Pelletier and Caventou.
The history of the use of antimalarials in LE and RA is deeply intertwined with world history. Chloroquine (CQ) was synthesized in 1930s by German Hans Andersag (Resochin in 1934 and Sontochin in 1936).[2] But after Germany's defeat in World War II, this compound was taken to and “re-introduced” in the United States as CQ, and was seen to be substantially more potent than quinine due to the chlorine atom at C7 position, following which it became famous worldwide owing to its potency, stability, low toxicity, and low cost.
Also, during the war, antimalarials had been administered to the soldiers as malaria prophylaxis. However, at the end of the war, British physicians realized that they had led to improvement of the soldiers' skin rashes and inflammatory arthritis as well![3] This led to quinacrine, and later CQ, being tried in LE and RA. Payne, a physician in London, had described the successful use of quinine to treat DLE[4] much earlier in 1894. However, it was Page who, apparently unaware of the Payne's publication, published a series of 20 patients with LE and RA treated successfully with quinacrine in 1951 in Lancet, which led to extensive use of quinacrine and later other antimalarials in LE and RA worldwide.[5]
In 1946, HCQ was introduced as the hydroxylated analog of CQ. It was shown to be approximately 40% less toxic than CQ in animal studies.[6] It was first used for SLE and RA in 1955 and received U.S. Food and Drug Administration (U.S. FDA) approval soon afterward in 1956 especially for skin and joint symptoms of SLE and RA.
Pharmacokinetics
Between 75% and 100% of oral HCQ is absorbed, and 50% is eventually bound to serum proteins. The drug is excreted in a rapid phase followed by a slower phase. The half-life of the drug in rapid phase is 3 days and 40–50 days in the slower phase.[7] Forty-five percent of HCQ is excreted through the kidney, 20% via the gastrointestinal tract, 5% via the skin. And around 25–45 % is stored in lean body tissues. Acidification of the urine increases the renal excretion of HCQ. Steady-state plasma levels are reached after 6 months of therapy.[8]
It is preferentially stored in the adrenal and pituitary glands, melanin-rich tissues, liver, spleen, and leukocytes. The epidermal levels are 100–200 times the plasma concentrations, but the main dermatological effect seems to be via its effect on the immune system and its anti-inflammatory action.
Mechanisms of Action[9]
Apart from its antimalarial activity, HCQ has antiproliferative, anti-inflammatory, photoprotective, and immunomodulatory effects. Among its varied actions [Table 2], there is a renewed interest in its antiviral action against HIV, influenza, and coronavirus.
Table 2.
Overview of Mode of action[9]
| Effect | Mechanism of action |
|---|---|
| Anti-infectious | Antimicrobial effects on HIV, coronavirus, influenza viruses. |
| Anti-inflammatory effects | Inhibition of phospholipase A2 and C. Inhibition of formation of IL1β, TNF-α. Inhibition of mast cells. Inhibition of Toll-like receptor 9 signal pathway. |
| Antiproliferative | Inhibits protein synthesis Promote chemo sensitization. Inhibit cell growth or cell death or both. Prevent mutations in cells with high mitotic rates. |
| Effect on coagulation | Inhibit platelet aggregation and adhesion. Inhibit formation of antiphospholipid antibody-β2-glycoprotein 1 complexes. Prevent antiphospholipid antibody binding of annexin-5 |
| Immunological | Inhibits autoantigen processing (MHCII). |
| Response | Reduced stimulation of autoreactive CD4+ T cells Reduced cytokine production: Reduces serum interleukin (IL)-1β, IL-6, IL-18, and tumor necrosis factor-alpha (TNF-α)(takes 3 months)[10] IL-18, is the interferon gamma (IFN-γ)-inducing factor, thus its reduction affects the adaptive immunity.[11] CQ inhibits macrophage TNF- α mRNA transcription and endotoxin induced secretion of TNF- α, IL-1, and IL-6. Binding to DNA and thus competitive inhibition of anti-DNA antibodies. Block of activation of innate and adaptive immunity process mediated by Toll-like receptors.[12] |
| Metabolic | Decreased hydroxylation of Vitamin D Lowered levels of LDL, Triglycerides and cholesterol. Increased excretion of porphyrin due to complex formation of HCQ with porphyrin |
| Photoprotective | Increased UV filtration? (Questionable relevance). It can cause spectral shift due to accumulation in melanin and increase in epidermal concentrations Inhibition of UV-induced inflammatory reactions |
Immunomodulatory effects (Inhibition of antigen presentation and apoptosis)
HCQ is an amphiphilic molecule (lipophilic ring structure and hydrophilic side chain) and preferential localizes to interphases such as phospholipid membranes. Being a weakly basic molecule, it can pass through the cell membranes and is protonated in the acidic milieu of the cytoplasm. It then loses its ability to pass through the membrane, and thus accumulates in the cell primarily in macrophages and lysosomes (100–1000 times higher). This leads to an increase in the vesicle pH from approximately 4.0 to 6.0, which interferes with the acid-dependent subcellular functions.[7]
The acidic cytoplasmic compartments are required for the antigen peptide processing and presentation. An essential initial step is the uptake and processing of antigen by the antigen-presenting cells (APCs) followed by expression of antigen-major histocompatibility complex (MHC) protein to the helper T lymphocytes (CD4+). The process of association of antigen peptide with MHC is pH sensitive. The antigen is digested by proteases and the peptides need to assemble with the α and β chains of MHC class II proteins. In the normal acidic environment, the digested peptides compete with the invariant (Ii) chains to form the complex of peptide-MCH that will be transported to the surface of the cell membrane to interact with CD+ T cells.[7] The intracellular raised pH secondary to HCQ decreases the affinity of the peptides and prevents the displacement of the α-Ii and β-Ii, and thus decreases the antigen presentation [Figure 1].
Figure 1.
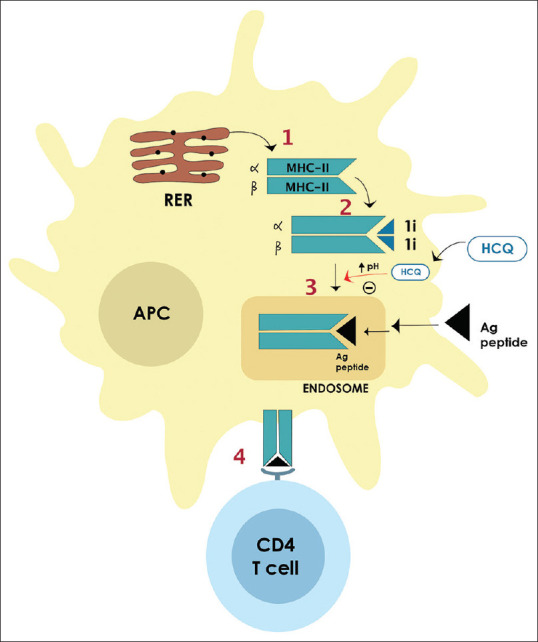
1. α&β chains of the MHC-II proteins are synthesized on the RER. 2. They bind to 1i (invariant) chain, forming α-1i and β-1i complexes. 3. After entering acidic endosomes→ acid hydrolases lead to dissociation of 1i chains from α&β chains→ bind to peptide antigens (Ags) → MHC-Ag peptide complex expresses at the cell membrane. 4. The antigen presenting cell interacts with the T cell via the T-cell receptor (TCR) that binds to the MHC-Ag. HCQ increases the pH of endosomes→ inhibits the dissociation of the α-1i and β-1i→ leads to decreased binding of the MHC-II to Ags→ ineffective presentation of antigens to T cells
The increased pH leads to immunoregulatory effects, including stabilization of lysosomal membranes, attenuation of antigen processing and presentation, and inhibition of cell-mediated cytotoxicity.[13] Furthermore, it inhibits the intracellular Toll-like receptors (TLRs), particularly TLR9.TLR3, TLR7, TLR8, and TLR9 specifically recognize nucleic acid motifs and are also distinct from other TLRs in that they are expressed not on the plasma membrane but intracellularly.[14]
HCQ does not consistently inhibit tumor necrosis factor (TNF-α), but blocks interleukin 1 (IL-1), IL-6, and IFN-α production.[15] HCQ-related clinical improvement has been correlated with reduction in IFN-α levels, which corroborate its clinical effects in SLE.[16]
The effect of HCQ is delayed due to its slow process of altering the pH of the antigen processing cells. Also, cryptic autoantigens are characterized by their low affinity for self-MHC. The selective uptake of exogenous peptides and selective sparing of self-peptides is facilitated by an increased pH in the endoplasmic reticulum loading compartment which explains why no increase in infections would occur with HCQ.
Anti-inflammatory properties
The anti-inflammatory effects of HCQ result from downregulation of the components of the arachidonic acid pathway, namely phospholipase A2 and C, which contribute to the production of pro-inflammatory prostaglandins and lipid peroxidation.[17] Lipid peroxidation is thought to play a role in apoptosis, particularly in response to ultraviolet A and ultraviolet B irradiation.[18] HCQ also has antioxidant properties and may protect against tissue damage from free radicals.[19]
Photoprotective action
In the skin, HCQ absorbs ultraviolet (UV) light in a concentration-dependent manner. It has been proposed that the beneficial effect of the HCQ in various photodermatoses may result from its ability to enhance the protective early limb of the UV response. It also binds to cellular deoxyribonucleic acid (DNA) by intercalation between base pairs, thus stabilizing the DNA and regulates ribonucleic acid (RNA) transcription; thus, subsequent RNA translation is inhibited.[9]
A more relevant mode of action is described by Wozniacka et al.,[20] who showed that HCQ reduces the expression of pro-inflammatory cytokines in the irradiated skin of patients with SLE, and also causes a reduction of human leukocyte antigen (HLA)–DR+ and CD1a+ cell numbers in both unirradiated and UV-irradiated skin. This is the plausible explanation of its use in skin lupus.
Anti-infective action
HCQ increases the pH of intracellular organelles leading to reduced survival of intracellular bacteria and fungi and viruses in lysosomes and endosomes, and a disordered posttranslational modification of synthesized proteins (such as viral envelope glycoproteins) in infected cells.[21] In rheumatological literature, multiple studies have shown a reduction in the risk of major infections which account for its real-life proof of this action[22,23] and a renewed interest has been generated in the COVID-19 epidemic.
Anti-bacterial
In Q fever (Coxiella burnetii) and Whipple's disease (Tropheryma whipplei), its action is via alkalinization of intracellular phagosomes (where the bacteria live), thus inhibiting their growth and multiplication and restoring the intracellular activity of antibiotics. This is the basis of successfully combining doxycycline and HCQ.[24]
Antiviral
There are many probable mechanisms for its antiviral activity:[21]
-
Increase in pH
- Inhibition of low-pH-dependent changes responsible for fusion, penetration, or uncoating of viruses within endosomes (influenza virus, hepatitis A virus [HAV], and hepatitis C virus [HCV])
- Inhibition of posttranslational modification of viral proteins (such as gp120 in HIV) and inhibition of sialic acid production[25] (present in HIV-1 glycoproteins and severe acute respiratory syndrome coronavirus 2 [SARS-Cov-2] receptor angiotensin-converting enzyme 2 [ACE2])
Immunomodulatory and anti-inflammatory: HIV and SARC-CoV-2
Decreased cellular iron: HIV
CQ and HCQ have been reported to interfere with flavivirus infections in vitro, Japanese encephalitis virus internalization, Yellow fever virus replication, and Dengue virus penetration and maturation. However, in a randomized controlled trial (RCT), CQ failed to significantly reduce viremia in dengue patients.[26] Thus, in vitro activity of HCQ does not always translate to clinical efficacy.
COVID-19
Though studies are still on, HCQ probably interferes with the glycosylation of ACE2 (the cellular receptor of SARS-CoV-2) and blocks viral fusion with the host cell.[27] Due to diminished glycosylation of ACE2, there occurs inefficient binding between SARS-CoV spike (S) viral protein and ACE2 on host cells[28] Also, the S-protein uses sialic acid linked to host cell surface ganglioside for entry. HCQ binds to sialic acid and gangliosides and the viral S-protein is unable to bind the ganglioside further interfering with viral entry[29]
In addition, HCQ has been shown to block the transport of SARS-CoV-2 from early endosomes to endolysosomes, which is needed to release the viral genome[25,30,31]
The anti-inflammatory effects of HCQ [Table 2] may probably partially combat the cytokine storm seen in critically ill COVID-19 patients as high concentration of cytokines have been seen in their plasma.[32] However, it remains to be seen whether this effect is clinically relevant or not.
Other actions
HCQ inhibits platelet adhesion and aggregation leading to an antithrombotic effect and has a favorable effect on lipid profile (reduced cholesterol, triglycerides [TG], very-low-density lipoprotein [VLDL], low-density lipoprotein [LDL])[33] particularly in patients on concomitant corticosteroid therapy. Thus, HCQ may be a useful drug in patients with comorbid cardiovascular disease, diabetes, and dyslipidemia due to its metabolic benefits.[34,35]
Indications
HCQ is often used as adjunctive therapy in combination regimens for RA and LE and is the most common disease-modifying agent used in rheumatology [Table 3].
Table 3.
Approved and unapproved uses of HCQ[9]
| FDA approved | Lupus erythematosus Rheumatoid arthritis Malaria |
|---|---|
| Off label | |
| Photosensitivity disorders | PCT, PMLE, solar urticaria, chronic actinic dermatitis, and hydroa vacciniforme |
| Granulomatous disorders | Sarcoidosis, granuloma annulare, LMDF, and granulomatous cheilitis |
| CT disorders | Dermatomyositis, scleredema, and LE |
| Disorders with Lymphocytic Infiltrate | Jessner’s infiltrate and lymphocytoma cutis |
| Panniculitis | Lupus panniculitis and erythema nodosum |
| Miscellaneous | Alopecia areata |
| Atopic dermatitis | |
| Eosinophilic fasciitis | |
| Follicular mucinosis | |
| Lichen nitidus | |
| Lichen planus | |
| Morphea | |
| Psoriatic arthritis | |
| Ulcerative stomatitis | |
| Urticarial vasculitis | |
| Infections | HIV, influenza, SARS-CoV, and SARS-CoV2 (COVID-19) |
LE
Chronic Cutaneous Lupus Erythematosus
When antimalarial therapy is initiated, 85% of lesions show resolution but the onset of action varies from 1 to 3 months.[36] Significant scalp involvement with alopecia in addition to disseminated discoid, annular, or papulosquamous subacute cutaneous LE skin lesions also respond to antimalarials. Verrucous and hypertrophic plaques do not respond well to antimalarial therapy. Due to the delay in achieving consistent plasma concentrations, it is recommended that therapy be administered for at least 2 months before switching to another drug. Smokers have been shown to have a poorer response to treatment.
SLE
HCQ is useful for arthritis, pleuritis, pericarditis, and lethargy.[37] In case the patient is not responsive, HCQ may be switched to CQ, but the two should not be used together because of the greater risk of ophthalmologic toxicity.[38] HCQ can inhibit exacerbations in longstanding SLE and prolong patient survival.[39] In addition, the drug has a protective effect against irreversible organ damage, thrombosis, and loss of bone mass. It is also known to cause reduction in blood lipids, protection against osteonecrosis, remission of lupus-related nephritis, delayed development of systemic lupus, and protective effects against developing cancer. Additional symptoms such as fatigue, weakness, arthralgia, myalgia, serositis, and mucous membrane ulcers improve in patients with SLE.[40] Also early HCQ use is associated with delayed onset of SLE.[41]
An overview of its use in LE in given in Box 1.
Box 1.
Overview of antimalarials in LE[9]
| Dose: Hydroxychloroquine initially at 200 mg twice daily, reducing to 200 mg/day, once a response is achieved |
| Onset of action: 6 weeks (4-8 weeks) |
| Duration: 6 months |
| Tapering: Reduce by 25% every 3-6 months, maintain with 1-2 tablets/week |
| Efficacy: 60%-75% of patients respond; subacute LE (60%-75%): tumid LE (90%) |
| Relapse: 50% relapse within 6 months |
PMLE
Its efficacy is based on its inhibitory effect on IL-1, IL-6, and IL-8, which play a role in the inflammatory process.[42] HCQ in a dose of 400 mg daily for 1 month, and 200 mg daily for 2 months, was superior to placebo in preventing development of the rash.[43]
Porphyria Cutanea Tarda
In this disorder, either twice weekly 125 mg CQ or 100 mg HCQ is given. In patients with elevated plasma iron levels, combination therapy, that is, beginning with bloodletting—500 mL every 4 weeks—plus CQ 250 mg/weekly (HCQ 200 mg/weekly) is recommended.[44,45]
Pseudolymphoma
A dose of HCQ of 200 mg/day initially, increased to 400 mg/day, has been noted to be effective.[46]
Jessner's Lymphocytic Infiltrate
Both CQ sulfate and HCQ sulfate have been found to be useful but in different dosages as compared to DLE. HCQ 200 mg once or twice a day, or CQ 200 mg daily can be used.[47]
Sarcoidosis
HCQ, similar to corticosteroids, tends to suppress the disease rather than cure it. Indications for administering CQ or HCQ in patients with sarcoidosis include chronic disfiguring skin lesions, progressive extracutaneous lesions in patients in whom steroid therapy is contraindicated, adjuvant therapy with steroid treatment, and neurosarcoidosis with steroid failure.[48] Hypercalcemia in sarcoidosis, but not in B-cell lymphoma, has shown improvement after HCQ therapy.
Granuloma Annulare
HCQ has been used in generalized granuloma annulare with a dose of 9 mg/kg/day for 2 months, tapered down to 6 mg/day for 1 month and 2 mg/kg/day for another 1 month.[49]
Lichen planus
COVID-19
The Centers for Disease Control and Prevention (CDC) stated that in the absence of any approved drug for COVID-19, the U.S. FDA has granted “emergency authorization” in March 2020 for the use of CQ and HCQ in hospitalized COVID-19 patients. The U.S. FDA has also given its nod to Phase III clinical trials with approximately 440 patients in the USA to evaluate the use of HCQ in a randomized, double-blind, placebo-controlled manner.
In India, the Indian Council of Medical Research National Taskforce for COVID-19 has advocated extended HCQ prophylaxis for healthcare workers and household contacts as follows:
Eligible individuals and dose (for prophylaxis):[53]
Asymptomatic healthcare workers involved in the care of suspected or confirmed cases of COVID-19: 400 mg twice a day on Day 1, followed by 400 mg once weekly for next 7 weeks
Asymptomatic household contacts of laboratory confirmed cases: 400 mg twice a day on Day 1, followed by 400 mg once weekly for next 3 weeks.
However, currently there is a severe dearth of firm and high-quality reproducible scientific evidence of clinical efficacy of this drug in COVID-19.[53]
Wang et al.[54] had first reported the efficacy of CQ in an in vitro study in China. Soon afterwards, the same group reported that HCQ was a safer and equally effective option as CQ.[55] An open-label nonrandomized trial of 20 COVID-19 patients given HCQ with/without azithromycin concluded that HCQ significantly reduced nasopharyngeal viral carriage 6 days after start of treatment vis-à-vis untreated controls. Azithromycin added to the efficacy of HCQ and all patients treated with the combination tested negative after 6 days.[56] However, the study had major limitations of a painfully small sample size and non-randomization.
Another study from France had contrasting results with the same treatment regimen. Of 11 patients, repeat nasopharyngeal swabs were done on 10 (1 expired) and 8 were found to be still positive at 6 days after HCQ and azithromycin.[57] A retrospective study from France reported no difference in the primary outcome (ICU transfer or death due to any cause within 1 week) between hospitalized COVID-19 patients who received HCQ and those who did not.[58]
In China too, Chen et al.[59] showed no difference between HCQ and control groups in the clinical outcome or negative conversion rate of nasopharyngeal samples.
Alhazzani et al.[60], in their guidelines on critically ill patients with COVID-19, concluded that in the absence of any randomized published trials on HCQ, there is insufficient evidence to issue a recommendation on the use of CQ or HCQ.
At present, most reports have small sample sizes (hence underpowered) and have short or no follow-ups. Only well-formulated prospective, randomized, placebo-controlled clinical studies with long follow-up periods may give more definitive results. In addition, it seems obvious that progress to unsalvageable ARDS depends more on the cytokine storm than the high viral load and moreover HCQ is not by itself a powerful antiviral agent. In fact, in some of these critically ill patients, physicians might need to stop the antimalarials in view of their ineffectiveness or potential adverse effects.[61]
There have been safety concerns with HCQ, mainly with regard to cardiac toxicity, more so when it is combined with azithromycin. HCQ may cause QT interval prolongation and ventricular arrhythmia, which may be difficult to identify and manage especially in the setting of either pre-existing cardiac disease or myocarditis due to COVID-19.
Notably recent study by ICMR on side effects of prophylactic doses of HCQ in healthcare workers observed abdominal pain in 10%, nausea in 6%, and hypoglycemia in 1.3%.
Dosage
Adults: HCQ sulfate tablets contain 200 mg HCQ sulfate, equivalent to 155 mg base, used for oral administration. Usual starting dose for HCQ is between 200 and 400 mg/day.
The minimum effective dose should be used. This dose should not exceed 6.5 mg/kg/day (calculated from ideal body weight). However, in clinical practice, a dose of HCQ at 5 mg/kg per day (unadjusted or real weight) is used.
Earlier, it was believed that irreversible retinopathy depends on whether the maximum daily dosage based on ideal body weight is exceeded or not. However, it has recently been shown that real body weight is a better predictor of risk of retinopathy than ideal body weight, perhaps because of the increasing variance of real body weight in the population and due to reduced chance of toxicity observed among thin patients. If the maximum dosages are observed, retinopathy is not a concern, even with therapy lasting for several years.[62]
Smoking leads to a decreased efficacy of HCQ and other antimalarials, possibly due to reduced absorption, enhanced metabolic turnover and by inhibiting lysosomal uptake.[63]
These effects of smoking could be additional reasons to encourage smoking cessation.
Blood levels of HCQ also determine the effects and low drug levels (<750 ng/mL) will necessitate a higher dosage to reach adequate levels and improve response in smokers.
Children: HCQ is used at a dose of 3 –5 mg/kg/day, typically to a maximum of 400 mg/day. The 200 mg tablet is therefore not suitable for use in children with an ideal body weight of less than 30 kg. To achieve this dosing in younger children using the 200-mg tablets, the drug can be dosed every other day.
Choice of Antimalarials: HCQ, CQ, or Quinacrine?
HCQ has certain advantages over CQ in the form of almost equal clinical efficacy, better tolerability, and favorable side effect profile. It has been shown to be threefold less toxic[64] than CQ, especially in terms of retinopathy. Also keratopathy is seen 40 times more frequently with high doses of CQ than with HCQ.[65] Patients who are unable to take CQ are often seen to tolerate HCQ well.
Quinacrine has certain unique adverse effects––it is contraindicated in glucose-6-phosphate dehydrogenase (G6PD)-deficient individuals due to the risk of hemolysis and is also known to cause aplastic anemia on occasion. It does not deposit in the retina and hence does not cause retinopathy but its cutaneous side effects are responsible for it not being a popular choice among dermatologists and rheumatologists. It causes deep lemon yellow pigmentation of the skin, nails, sclera, sweat, and lacrimal secretions. The typical bluish-gray pigmentation on the shins, face, and palate seen with CQ and HCQ are infrequent with quinacrine.
The equivalent doses of HCQ, CQ, and quinacrine are 400, 250, and 100 mg, respectively.
Combination of Antimalarials
Quinacrine can be added to HCQ or CQ when there is lack of or suboptimal clinical response in LE. Cavazzana et al.[66] and Tanenbaum et al.[67] have shown reduction in CLASI activity scores and initiation of response in recalcitrant cases with combination of HCQ and Quinacrine.
Workup and Monitoring
The drug is safe and in usual doses and indications nothing else is needed besides ophthamic monitoring.[68]
Ophthalmic examination
The American Academy of Ophthalmology (AAO) recommends that patients on long-term HCQ should visit an ophthalmologist within the first year of treatment for fundus examination. They have found that the risk of toxicity increases toward 1% after 5–7 years of use or a cumulative dose of 1000 g or 460 g of HCQ or CQ, respectively
The testing of the central visual field (VF) sensitivity by an automated field tester (Humphrey 10-2) is done alone with fundus examination and if normal with no risk factors, annual screening tests should start after 5 years while if there are any risk factors, they should start within 5 years. If the baseline fundus examination is abnormal screening tests should be performed annually[69]
The screening tests are automated VFs and spectral-domain optical coherence tomography (SD OCT). These should look beyond the central macula in Asian patients
Risk factors for retinopathy include dose >5 mg/kg (real body weight) per day, duration >5 years, preexisting renal disease with decreased GFR, Tamoxifen treatment, and preexisting macular disease.
Cardiac evaluation
Screen for digoxin use and history of cardiomyopathy or severe heart failure. In such cases electrocardiogram (ECG) during therapy is warranted and watch for depression of ST segment, T-wave inversion and QT interval prolongation[70]
A baseline ECG should be done if a combination with azithromycin is considered. Other drugs that may increase the QT interval (see later) should be avoided and serum electrolytes should be checked periodically
Determination of creatine kinase (CK) and lactate dehydrogenase (LDH) in blood is appropriate to screen for myopathy and cardiomyopathy and should be checked before starting the treatment and then every 3 months.
Liver studies
Aspartate transaminase (AST), alanine transaminase (ALT), and bilirubin if patient is receiving long-term treatment.
Hematological
Complete blood count (CBC) and platelets; white blood cell (WBC), red blood cell (RBC), and platelets may be decreased; if severe, product should be discontinued; assess for malaise, fever, bruising, and bleeding (rare)
G6PD levels do not need to be routinely screened, unless patient is on another drug that may cause methemoglobinemia.[71]
Cutaneous reactions
New-onset pruritus, rash, urticaria, and mucositis (acute generalized exanthematous pustulosis [AGEP] and drug reaction with eosinophilia and systemic symptoms [DRESS] can.
Ototoxicity (tinnitus, vertigo, and change in hearing)
Audiometric testing should be done before and after treatment.
Safety Profile
HCQ is a well-tolerated drug and, except for GIT side effects, discontinuation of the drug is rarely required [Box 2].
Box 2.
Overview of side effects with Antimalarial Drugs
| GIT: Nausea, vomiting, anorexia, diarrhea, cramps |
| Eye & ENT: Blurred vision (dose dependent), corneal changes, retinal changes, difficulty focusing, tinnitus, vertigo, deafness, photophobia, corneal edema |
| Blood: Thrombocytopenia, agranulocytosis, leukopenia, aplastic anemia |
| Skin: Pruritus, pigmentation changes, skin eruptions, lichenplanus-like eruptions, eczema, exfoliative dermatitis, alopecia, Stevens-Johnson syndrome, photosensitivity |
| CNS: Headache, stimulation, fatigue, irritability, seizures, bad dreams, dizziness, confusion, psychosis, decreased reflexes |
| CVS: Hypotension, heart block, asystole with syncope |
| Psychiatric: Can affect lability |
| Hypoglycemia: Hydroxychloroquine has been shown to cause severe hypoglycemia including loss of consciousness that could be life threatening in patients treated with and without antidiabetic medication |
| Neuromyotoxicity- insidious-onset proximal weakness with a normal CPK, peripheral neuropathy and cardiac myotoxicity. |
*Those underlined are commonly seen
Ocular
Melles and Marmor[62] reported that the prevalence of HCQ-induced retinopathy was 7.5% and varied with the dose (odds ratio, 5.67; for >5.0 mg/kg) and with duration of use (odds ratio, 3.22; for >10 years). At doses of 4–5 mg/kg, it was <2% within the first 10 years of use but rose to almost 20% after 20 years of use; however, even after 20 years, a patient without toxicity has only a 4% risk of converting in the subsequent year.[72]
Common: Blurring of vision due to a disturbance of accommodation is dose dependent and reversible accommodation defects are seen in those taking higher dosages >500 mg/day of CQ.
Uncommon: Retinopathy and VF defects can occur, but appear to be uncommon if the recommended daily dose (5 mg/kg/day) is not exceeded.[62,72] Retinopathy, which can lead to impaired vision, appears to be extremely rare, especially in the first 5 years of therapy. The early form of retinopathy secondary to HCQ is reversible if the drug is discontinued.[73] However if it is allowed to develop, there is risk of progression regardless of drug cessation.
Initial presentation of retinal involvement can be asymptomatic or can present as paracentral, temporal, pericentral ring type scotomas along with color vision anomalies. The pathognomonic finding is bull's eye maculopathy characterized by involvement of retinal pigment epithelial cell layer leading to depigmentation of central macula and relative sparing of the macular fovea.
However, bull's eye maculopathy is now merely a textbook term which is hardly seen clinically due to increased screening. Retinopathy starts in the inferotemporal retina (corresponding to the superonasal VF). Recent evidence has shown extramacular involvement, especially in the Asian population which can be missed during standard screening as pericentral retinopathy spares the macula.[69] Hence, screening tests (VF and OCT) should be extended in fields beyond the macula.
Corneal changes including edema and opacities have been reported. They are either asymptomatic or may cause visual disturbances such as haloes, blurring of vision, or photophobia. They may be transient and are reversible on stopping treatment.
Dermatological Effects
Pigmentation: A bluish-gray to black hyperpigmentation may occur in 10%–30% of patients treated for 4 months or longer with any of the drugs. The pigmentation typically affects the shins (resembling ecchymoses), face, palate (with a sharp line demarcating the hard and soft palate), and nailbeds (as transverse bands). The pigmentation may take months to fade after discontinuation of therapy
Progressive bleaching of the hair roots of the scalp, the face, and the body is another unusual pigmentary disturbance that may appear in as many as 10% of patients taking HCQ. This pigmentary phenomenon is also reversible. It has been suggested that taking CQ/HCQ for 3 weeks out of 4 weeks can help prevent this side effect[74]
The incidence of pruritus and various cutaneous eruptions associated with antimalarial use has been reported to be 10%–20%. Pelle and Callen[75] have reported that roughly 25% of all dermatomyositis patients experience hypersensitivity drug eruptions (mostly morbilliform, occasionally AGEP or DRESS) during antimalarial therapy
Antimalarial drugs are known to occasionally exacerbate existing psoriasis. However, psoriasis is not a contraindication for CQ therapy.
-
Uncommon side effects
- Bullous eruptions including erythema multiforme
- Drug rash with eosinophilia and systemic symptoms (DRESS syndrome)
- Stevens–Johnson syndrome and toxic epidermal necrolysis
- Photosensitivity.
Patients should be advised to use sunglasses in bright sunlight to decrease photophobia and to wear protective clothing while on HCQ.
Cardiac effects
The side effects reported include conduction disturbances, sick sinus syndrome, torsades de pointes, malignant ventricular arrhythmias, congestive heart failure, and cardiomyopathy (hypertrophic and restrictive). Immediate withdrawal of HCQ is essential if toxicity is suspected because of the early reversibility of cardiomyopathy. Cardiac toxicity due to HCQ needs to be differentiated from that due to LE/RA in patients. With regard to conduction defects, Chatre et al.[76] reported that nearly 85% patients had conduction disorders after a median of 7 years and a high cumulative dose (median 1235 g HCQ).
Myopathy
Proximal muscle myopathy may be associated with cardiac myotoxicity. Risk factors include Caucasian race and renal failure.
Haematological
G6PD screening is no longer considered essential before starting HCQ. Youngster et al.[77] concluded that there was no effect of HCQ on RBC lifespan G6PD-deficient patients. However, caution should be exercised when combining the drug with other agents with possible hemolytic effects.
Gastrointestinal
Gastrointestinal adverse effects are some of the most common causes of drug discontinuation. The most frequent symptoms are anorexia, heartburn, nausea, vomiting, diarrhea, and abdominal distention. These symptoms are usually transient and promptly disappear after the drug is stopped or the dose is lowered.
Drug Interactions
The salient interactions are listed in Table 4.
Table 4.
Drug interactions of HCQ
| Interaction | Mechanism | Drugs |
|---|---|---|
| Drugs that decrease the effect of HCQ | Antacids, kaolin, magnesium and trisilicate | |
| Drugs that increase the effect of HCQ | Cyclosporine and digoxin | |
| Drugs whose level is increased by HCQ | Inhibition of P-glycoprotein (P-gp) efflux transporter CYP2D6 inhibition by HCQ |
Cyclosporine and digoxin (substrates of P-gp) Metoprolol |
| Drugs that increase level of HCQ | CYP450 inhibition | Cimetidine |
| CYP2C8 inhibition | Gemfibrozil and clopidogrel | |
| CYP3A4/5 | Verapamil, diltiazem, azoles, macrolides, and quinolones | |
| Additive toxicity with HCQ | QT prolongation, arrhythmias | Methadone, amiodarone, quinolones, clarithromycin, azithromycin, moxifloxacin, pimozide, tricyclic antidepressants, and antiemetics (promethazine, ondansetron) |
| Seizures | Tramadol, bupropion | |
| Methemoglobinemia | Benzocaine and prilocaine | |
| Increased antibody titer | Anti-rabies vaccine | |
| Decreased effect of | live virus vaccines and botulinum toxoids |
Coadministration with azithromycin: Monitoring of the QTc interval (baseline and daily for the duration of treatment) is strongly advised, when both drugs are co-prescribed.[78] However, azithromycin is not as strong an inhibitor of CYP450 (cf. erythromycin) and thus may have less drug interactions.
Use In Special Populations
Children: Safe in children with juvenile idiopathic arthritis (JIA) and LE. However, no appropriate dosage forms of HCQ are available for children <30kg. Capsules or tablets need to be pulverized and mixed with jam, jelly, or honey to mask the bitter taste
Pregnancy and lactation: Pregnancy category C. As HCQ has a long t1/2, even discontinuation at the time of pregnancy cannot avoid fetal exposure. Although it can cross the placenta, it does not have teratogenic or fetopathic effects.[79]
There are numerous studies in rheumatology that substantiate the use of this drug in lupus in pregnancy and it has been shown that HCQ use is associated with decreased disease activity scores and lower prednisone doses at delivery,[80] whereas discontinuation is associated with disease flares. There are no reports of toxicity or developmental disabilities in the children born to mothers with a history of intake of HCQ during pregnancy or lactation.[81] Therefore, maternal HCQ use is considered safe during pregnancy and breast feeding.[82]
Conclusion
HCQ has been used for many decades in Dermatology and in the light of its varied actions and favorable safety profile; it finds wide use in Rheumatology and varied off-label indications. However, the risk of retinopathy and cardiac adverse effects should never be neglected and physicians should adhere to the prescribed guidelines at all times. Although its use has been renewed due to its purported antiviral action, it must be remembered that this has not been conclusively proven as of date and the final word on this is still awaited.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to acknowledge the expertise and help of Mrs. Kanika Mehta in the illustration used in this article.
References
- 1.Wallace DJ. The history of antimalarials. Lupus. 1996;5(Suppl 1):S2–3. [PubMed] [Google Scholar]
- 2.Van Schalkwyk DA. History of Antimalarial Agents. eLS, 1–5. 2015 doi:10.1002/9780470015902.a0003624.pub3. [Google Scholar]
- 3.Al-Bari MA. Chloroquine analogues in drug discovery: New directions of uses, mechanisms of actions and toxic manifestations from malaria to multifarious diseases. J Antimicrob Chemother. 2015;70:1608–21. doi: 10.1093/jac/dkv018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Payne J. A postgraduate lecture on lupus erythematosus. Clin J. 1894;4:223–9. [Google Scholar]
- 5.Page F. Treatment of lupus erythematosus with mepacrine. Lancet. 1951;2:755–8. doi: 10.1016/s0140-6736(51)91643-1. [DOI] [PubMed] [Google Scholar]
- 6.McChesney EW. Animal toxicity and pharmacokinetics of hydroxychloroquine sulfate. Am J Med. 1983;75:11–8. doi: 10.1016/0002-9343(83)91265-2. [DOI] [PubMed] [Google Scholar]
- 7.Fox RI. Mechanism of action of hydroxychloroquine as an antirheumatic drug. Semin Arthritis Rheum. 1993;23(2 Suppl 1):82–91. doi: 10.1016/s0049-0172(10)80012-5. [DOI] [PubMed] [Google Scholar]
- 8.Tett SE, Cutler DJ, Day RO, Brown KF. Bioavailability of hydroxychloroquine tablets in healthy volunteers. Br J Clin Pharmacol. 1989;27:771–9. doi: 10.1111/j.1365-2125.1989.tb03439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choubey V, Mittal S, Narang I, Sardana K. In: Systemic Drugs in dermatology. Sardana K, editor. New Delhi: Jaypee Publishers; 2016. pp. 691–706. [Google Scholar]
- 10.Wozniacka A, Lesiak A, Boncela J, Smolarczyk K, McCauliffe DP, Sysa-Jedrzejowska A. The influence of antimalarial treatment on IL-1beta, IL-6 and TNF-alpha mRNA expression on UVB-irradiated skin in systemic lupus erythematosus. Br J Dermatol. 2008;159:1124–30. doi: 10.1111/j.1365-2133.2008.08804.x. [DOI] [PubMed] [Google Scholar]
- 11.Theofilopoulos AN, Koundouris S, Kono DH, Lawson BR. The role of IFN-gamma in systemic lupus erythematosus: A challenge to the Th1/Th2 paradigm in autoimmunity. Arthritis Res. 2001;3:136–41. doi: 10.1186/ar290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Means TK, Latz E, Hayashi F, Murali MR, Golenbock DT, Luster AD. Human lupus autoantibody-DNA complexes activate DCs through cooperation of CD32 and TLR9. J Clin Invest. 2005;115:407–17. doi: 10.1172/JCI23025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz SJ, Russell AS. Re-evaluation of antimalarials in treating rheumatic diseases: Re-appreciation and insights into new mechanisms of action. Curr Opin Rheumatol. 2011;23:278–81. doi: 10.1097/BOR.0b013e32834456bf. [DOI] [PubMed] [Google Scholar]
- 14.Lafyatis R, York M, Marshak-Rothstein A. Antimalarial agents: Closing the gate on Toll-like receptors? Arthritis Rheum. 2006;54:3068–70. doi: 10.1002/art.22157. [DOI] [PubMed] [Google Scholar]
- 15.Sperber K, Quraishi H, Kalb TH, Panja A, Stecher V, Mayer L. Selective regulation of cytokine secretion by hydroxychloroquine: Inhibition of interleukin 1 alpha (IL-1-alpha) and IL-6 in human monocytes and T cells. J Rheumatol. 1993;20:803–8. [PubMed] [Google Scholar]
- 16.Willis R, Seif AM, McGwin G, Jr, Martinez-Martinez LA, González EB, Dang N, et al. Effect of hydroxychloroquine treatment on pro-inflammatory cytokines and disease activity in SLE patients: Data from LUMINA (LXXV), a multiethnic US cohort. Lupus. 2012;21:830–5. doi: 10.1177/0961203312437270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bondeson J, Sundler R. Antimalarial drugs inhibit phospholipase A2 activation and induction of interleukin 1beta and tumor necrosis factor alpha in macrophages: Implications for their mode of action in rheumatoid arthritis. Gen Pharmacol. 1998;30:357–6. doi: 10.1016/s0306-3623(97)00269-3. [DOI] [PubMed] [Google Scholar]
- 18.Ramakrishnan N, Kalinich JF, McClain DE. Ebselen inhibition of apoptosis by reduction of peroxides. Biochem Pharmacol. 1996;51:1443–51. doi: 10.1016/0006-2952(96)00084-6. [DOI] [PubMed] [Google Scholar]
- 19.Miyachi Y, Yoshioka A, Imamura S, Niwa Y. Antioxidant action of antimalarials. Ann Rheum Dis. 1986;45:244–8. doi: 10.1136/ard.45.3.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wozniacka A, Lesiak A, Narbutt J, Kobos J, Pavel S, Sysa-Jedrzejowska A. Chloroquine treatment reduces the number of cutaneous HLA-DR+ and CD1a+ cells in patients with systemic lupus erythematosus. Lupus. 2007;16:89–94. doi: 10.1177/0961203306075384. [DOI] [PubMed] [Google Scholar]
- 21.Rolain JM, Colson P, Raoult D. Recycling of chloroquine and its hydroxyl analogue to face bacterial, fungal and viral infections in the 21st century. Int J Antimicrob Agents. 2007;30:297–308. doi: 10.1016/j.ijantimicag.2007.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruiz-Irastorza G, Olivares N, Ruiz-Arruza I, Martinez-Berriotxoa A, Egurbide MV, Aguirre C. Predictors of major infections in systemic lupus erythematosus. Arthritis Res Ther. 2009;11:R109. doi: 10.1186/ar2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sisó A, Ramos-Casals M, Bové A, Brito-Zerón P, Soria N, Muñoz S, et al. Previous antimalarial therapy in patients diagnosed with lupus nephritis: Influence on outcomes and survival. Lupus. 2008;17:281–8. doi: 10.1177/0961203307086503. [DOI] [PubMed] [Google Scholar]
- 24.Raoult D, Houpikian P, Tissot Dupont H, Riss JM, Arditi-Djiane J, Brouqui P. Treatment of Q fever endocarditis: Comparison of 2 regimens containing doxycycline and ofloxacin or hydroxychloroquine. Arch Intern Med. 1999;159:167–73. doi: 10.1001/archinte.159.2.167. [DOI] [PubMed] [Google Scholar]
- 25.Savarino A, Di Trani L, Donatelli I, Cauda R, Cassone A. New insights into the antiviral effects of chloroquine. Lancet Infect Dis. 2006;6:67–9. doi: 10.1016/S1473-3099(06)70361-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tricou V, Minh NN, Van TP, Lee SJ, Farrar J, Wills B, et al. A randomized controlled trial of chloroquine for the treatment of dengue in Vietnamese adults. PLoS Negl Trop Dis. 2010;4:e785. doi: 10.1371/journal.pntd.0000785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Devaux CA, Rolain JM, Colson P, Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: What to expect for COVID-19? Int J Antimicrob Agents. 2020:105938. doi: 10.1016/j.ijantimicag.2020.105938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou D, Dai SM, Tong Q. COVID-19: A recommendation to examine the effect of hydroxychloroquine in preventing infection and progression? J Antimicrob Chemother. 2020:dkaa114. doi: 10.1093/jac/dkaa114. doi: 10.1093/jac/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fantini J, Di Scala C, Chahinian H, Yahi N. Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection? Int J Antimicrob Agents. 2020:105960. doi: 10.1016/j.ijantimicag.2020.105960. doi: 10.1016/j.ijantimicag.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mauthe M, Orhon I, Rocchi C, Zhou X, Luhr M, Hijlkema KJ, et al. Chloroquine inhibits autophagic flux by decreasing autophagosome-lysosome fusion. Autophagy. 2018;14:1435–55. doi: 10.1080/15548627.2018.1474314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mingo RM, Simmons JA, Shoemaker CJ, Nelson EA, Schornberg KL, D'Souza RS, et al. Ebola virus and severe acute respiratory syndrome coronavirus display late cell entry kinetics: Evidence that transport to NPC1+ endolysosomes is a rate-defining step. J Virol. 2015;89:2931–43. doi: 10.1128/JVI.03398-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R. Effects of chloroquine on viral infections: An old drug against today's diseases? Lancet Infect Dis. 2003;3:722–7. doi: 10.1016/S1473-3099(03)00806-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morris SJ, Wasko MC, Antohe JL, Sartorius JA, Kirchner HL, Dancea S, et al. Hydroxychloroquine use associated with improvement in lipid profiles in rheumatoid arthritis patients. Arthritis Care Res (Hoboken) 2011;63:530–4. doi: 10.1002/acr.20393. [DOI] [PubMed] [Google Scholar]
- 34.Mirjafari H, Al-Husain A, Bruce IN. Cardiovascular risk factors in inflammatory arthritis. Curr Opin Lipidol. 2011;22:296–301. doi: 10.1097/MOL.0b013e3283488c50. [DOI] [PubMed] [Google Scholar]
- 35.Petri M. Use of hydroxychloroquine to prevent thrombosis in systemic lupus erythematosus and in antiphospholipid antibody-positive patients. Curr Rheumatol Rep. 2011;13:77–80. doi: 10.1007/s11926-010-0141-y. [DOI] [PubMed] [Google Scholar]
- 36.Wahie S, Meggitt SJ. Long-term response to hydroxychloroquine in patients with discoid lupus erythematosus. Br J Dermatol. 2013;169:653–9. doi: 10.1111/bjd.12378. [DOI] [PubMed] [Google Scholar]
- 37.Rudnicki RD, Gresham GE, Rothfield NF. The efficacy of antimalarials in systemic lupus erythematosus. J Rheumatol. 1975;2:323–30. [PubMed] [Google Scholar]
- 38.Feldmann R, Salomon D, Saurat JH. The association of the two antimalarials chloroquine and quinacrine for treatment-resistant chronic and subacute cutaneous lupus erythematosus. Dermatol. 1994;189:425–7. doi: 10.1159/000246899. [DOI] [PubMed] [Google Scholar]
- 39.Ruiz-Irastorza G, Ramos-Casals M, Brito-Zeron P, Khamashta MA. Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: A systematic review. Ann Rheum Dis. 2010;69:20–8. doi: 10.1136/ard.2008.101766. [DOI] [PubMed] [Google Scholar]
- 40.Canadian Hydroxychloroquine Study Group. A randomized study of the effect of withdrawing hydroxychloroquine sulfate in systemic lupus erythematosus. N Engl J Med. 1991;324:150–4. doi: 10.1056/NEJM199101173240303. [DOI] [PubMed] [Google Scholar]
- 41.James JA, Kim-Howard XR, Bruner BF, Jonsson MK, McClain MT, Arbuckle MR, et al. Hydroxychloroquine sulfate treatment is associated with later onset of systemic lupus erythematosus. Lupus. 2007;16:401–9. doi: 10.1177/0961203307078579. [DOI] [PubMed] [Google Scholar]
- 42.Tutrone WD, Spann CT, Scheinfeld N, Deleo VA. Polymorphic light eruption. Dermatol Ther. 2003;16:28–39. doi: 10.1046/j.1529-8019.2003.01605.x. [DOI] [PubMed] [Google Scholar]
- 43.Murphy GM, Hawk JL, Magnus IA. Hydroxychloroquine in polymorphic light eruption: A controlled trial with drug and visual sensitivity monitoring. Br J Dermatol. 1987;116:379–86. doi: 10.1111/j.1365-2133.1987.tb05852.x. [DOI] [PubMed] [Google Scholar]
- 44.Malkinson FD, Levitt L. Hydroxychloroquine treatment of porphyria cutanea tarda. Arch Dermatol. 1980;116:1147–50. [PubMed] [Google Scholar]
- 45.Singal AK, Kormos-Hallberg C, Lee C, Sadagoparamanujam VM, Grady JJ, Freeman DH, Jr, et al. Low-dose hydroxychloroquine is as effective as phlebotomy in treatment of patients with porphyria cutanea tarda. Clin Gastroenterol Hepatol. 2012;10:1402–9. doi: 10.1016/j.cgh.2012.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stoll DM. Treatment of cutaneous pseudolymphoma with hydroxychloroquine. J Am Acad Dermatol. 1983;8:696–9. doi: 10.1016/s0190-9622(83)70082-4. [DOI] [PubMed] [Google Scholar]
- 47.Toonstra J, Wildschut A, Boer J, Smeenk G, Willemze R, van der Putte SC, et al. Jessner's lymphocytic infiltration of the skin. A clinical study of 100 patients. Arch Dermatol. 1989;125:1525–30. [PubMed] [Google Scholar]
- 48.Raghu G, Berman JS, Govender P. Treatment of sarcoidosis. Am J Respir Crit Care Med. 2018;197:P9–10. doi: 10.1164/rccm.1976P9. [DOI] [PubMed] [Google Scholar]
- 49.Cannistraci C, Lesnoni La Parola I, Falchi M, Picardo M. Treatment of generalized granuloma annulare with hydroxychloroquine. Dermatology. 2005;211:167–8. doi: 10.1159/000086452. [DOI] [PubMed] [Google Scholar]
- 50.Zhu Y, Li J, Bai Y, Wang X, Duan N, Jiang H, et al. Hydroxychloroquine decreases the upregulated frequencies of Tregs in patients with oral lichen planus. Clin Oral Investig. 2014;18:1903–11. doi: 10.1007/s00784-013-1176-z. [DOI] [PubMed] [Google Scholar]
- 51.Fazel N. Cutaneous lichen planus: A systematic review of treatments. J Dermatolog Treat. 2015;26:280–3. doi: 10.3109/09546634.2014.933167. [DOI] [PubMed] [Google Scholar]
- 52.Ramírez P, Feito M, Sendagorta E, González-Beato M, De Lucas R. Childhood actinic lichen planus: Successful treatment with antimalarials. Australas J Dermatol. 2012;53:e10–3. doi: 10.1111/j.1440-0960.2010.00695.x. [DOI] [PubMed] [Google Scholar]
- 53.Advisory on the use of Hydroxy-Chloroquine as Prophylaxis for SARS-Cov2 Infection. [Internet] Available from: https://www.mohfw.gov.in/pdf/AdvisoryontheuseofHydroxychloroquinasprophylaxisforSARSCoV2infection.pdf . Last cited on 2020 Apr 13.
- 54.Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269–71. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H, et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:16. doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label nonrandomized clinical trial. Int J Antimicrob Agents. 2020:105949. doi: 10.1016/j.ijantimicag.2020.105949. doi: 101016/jijantimicag2020105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Molina JM, Delaugerre C, Goff JL, Mela-Lima B, Ponscarme D, Goldwirt L, et al. No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine & azithromycin in patients with severe COVID-19 infection? Med Mal Infect. 2020:S0399. doi: 10.1016/j.medmal.2020.03.006. doi: 10.1016/j.medmal.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Herman AO. COVID-19: Hydroxychloroquine and Hypoxic Pneumonia/Timing of Viral Shedding and Transmission/Coinfection with Other Respiratory Pathogens [Internet] NEJM Journal Watch. Available from: wwwjwatchorg/fw116555/2020/04/15/covid-19-hydroxychloroquine-hypoxic-pneumonia-timing . Last cited on 2020 Apr 19.
- 59.Chen J, Liu D, Liu Li, Liu P, Xu Q, Xia L, et al. A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19) J Zhejiang Univ (Med Sci) 2020:49. doi: 10.3785/j.issn.1008-9292.2020.03.03. doi: 103785/jissn1008-929220200303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19) Intensive Care Med. 2020 doi: 10.1007/s00134-020-06022-5. doi: 101007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vincent JL, Taccone FS. Understanding pathways to death in patients with COVID-19? Lancet Respir Med. 2020:S2213. doi: 10.1016/S2213-2600(20)30165-X. doi: 10.1016/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Melles RB, Marmor MF. The risk of toxic retinopathy in patients on long-term hydroxychloroquine therapy. JAMA Ophthalmol. 2014;132:1453–60. doi: 10.1001/jamaophthalmol.2014.3459. [DOI] [PubMed] [Google Scholar]
- 63.Ezra N, Jorizzo J. Hydroxychloroquine and smoking in patients with cutaneous lupus erythematosus. Clin Exp Dermatol. 2012;37:327–34. doi: 10.1111/j.1365-2230.2011.04266.x. [DOI] [PubMed] [Google Scholar]
- 64.Wolf R, Wolf D, Ruocco V. Antimalarials: Unapproved uses or indications. Clin Dermatol. 2000;18:17–35. doi: 10.1016/s0738-081x(99)00092-9. [DOI] [PubMed] [Google Scholar]
- 65.Browning DJ. Toxicology of hydroxychloroquine and chloroquine and the pathology of the retinopathy they cause. In: Browning DJ, editor. Hydroxychloroquine and chloroquine retinopathy. New York: Springer Science + Business Media; 2014. pp. 65–83. [Google Scholar]
- 66.Cavazzana I, Sala R, Bazzani C, Ceribelli A, Zane C, Cattaneo R, et al. Treatment of lupus skin involvement with quinacrine and hydroxychloroquine. Lupus. 2009;18:735–9. doi: 10.1177/0961203308101714. [DOI] [PubMed] [Google Scholar]
- 67.Tanenbaum L, Tuffanelli DL. Antimalarial agents.Chloroquine, hydroxychloroquine, and quinacrine. Arch Dermatol. 1980;116:587–91. doi: 10.1001/archderm.116.5.587. [DOI] [PubMed] [Google Scholar]
- 68.Fiehn C, Ness T, Weseloh C, Specker C, Hadjiski D, Detert J, et al. Kommission Pharmakotherapie der DGRh [Safety management of the treatment with antimalarial drugs in rheumatology Interdisciplinary recommendations based on a systematic literature search] Z Rheumatol. 2020;79:186–94. doi: 10.1007/s00393-020-00751-0. [DOI] [PubMed] [Google Scholar]
- 69.Mirshahi A, Naderan M, Abrishami M. Screening for hydroxychloroquine associated retinopathy: A review. J Clin Diagn Res. 2019;13:NE01–6. [Google Scholar]
- 70.Tselios K, Gladman DD, Harvey P, Mak S, Chantal M, Butany J, et al. Hydroxychloroquine-induced cardiomyopathy in systemic lupus erythematosus. J Clin Rheumatol. 2016;22:287–8. doi: 10.1097/RHU.0000000000000400. [DOI] [PubMed] [Google Scholar]
- 71.Mohammad S, Clowse MEB, Eudy AM, Criscione-Schreiber LG. Examination of hydroxychloroquine use and hemolytic anemia in G6PDH-deficient patients. Arthritis Care Res (Hoboken) 2018;70:481–5. doi: 10.1002/acr.23296. [DOI] [PubMed] [Google Scholar]
- 72.Marmor MF, Kellner U, Lai TY, Melles RB, Mieler WF American Academy of Ophthalmology. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy (2016 Revision) Ophthalmology. 2016;123:1386–94. doi: 10.1016/j.ophtha.2016.01.058. [DOI] [PubMed] [Google Scholar]
- 73.Marmor MF, Carr RE, Easterbrook M, Farjo AA, Mieler WF American Academy of Ophthalmology. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy: A report by the American Academy of Ophthalmology. Ophthalmology. 2002;109:1377–82. doi: 10.1016/s0161-6420(02)01168-5. [DOI] [PubMed] [Google Scholar]
- 74.Ricci F, De Simone C, Del Regno L, Peris K. Drug-induced hair colour changes. Eur J Dermatol. 2016;26:531–6. doi: 10.1684/ejd.2016.2844. [DOI] [PubMed] [Google Scholar]
- 75.Pelle M, Callen JP. Adverse cutaneous reactions to hydroxychloroquine are more common in patients with dermatomyositis than in patients with cutaneous lupus erythematosus. Arch Dermatol. 2002;138:1231–3. doi: 10.1001/archderm.138.9.1231. [DOI] [PubMed] [Google Scholar]
- 76.Chatre C, Roubille F, Vernhet H, Jorgensen C, Pers YM. Cardiac complications attributed to chloroquine and hydroxychloroquine: A systematic review of the literature. Drug Saf. 2018;41:919–31. doi: 10.1007/s40264-018-0689-4. [DOI] [PubMed] [Google Scholar]
- 77.Youngster I, Arcavi L, Schechmaster R, Akayzen Y, Popliski H, Shimonov J, et al. Medications and glucose-6-phosphate dehydrogenase deficiency: An evidence-based review. Drug Saf. 2010;33:713–26. doi: 10.2165/11536520-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 78.Juurlink DN. Safety considerations with chloroquine, hydroxychloroquine and azithromycin in the management of SARS-CoV-2 infection. CMAJ. 2020 doi: 10.1503/cmaj.200528. cmaj200528 doi: 101503/cmaj200528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Abarientos C, Sperber K, Shapiro DL, Aronow WS, Chao CP, Ash JY. Hydroxychloroquine in systemic lupus erythematosus and rheumatoid arthritis and its safety in pregnancy. Expert Opin Drug Saf. 2011;10:705–14. doi: 10.1517/14740338.2011.566555. [DOI] [PubMed] [Google Scholar]
- 80.Levy RA, Vilela VS, Cataldo MJ, Ramos RC, Duarte JL, Tura BR, et al. Hydroxychloroquine (HCQ) in lupus pregnancy: Double-blind and placebo-controlled study. Lupus. 2001;10:401–4. doi: 10.1191/096120301678646137. [DOI] [PubMed] [Google Scholar]
- 81.Cortés-Hernández J, Ordi-Ros J, Paredes F, Casellas M, Castillo F, Vilardell-Tarres M. Clinical predictors of fetal and maternal outcome in systemic lupus erythematosus: A prospective study of 103 pregnancies. Rheumatology (Oxford) 2002;41:643–50. doi: 10.1093/rheumatology/41.6.643. [DOI] [PubMed] [Google Scholar]
- 82.Østensen M, Khamashta M, Lockshin M, Parke A, Brucato A, Carp H, et al. Anti-inflammatory and immunosuppressive drugs and reproduction. Arthritis Res Ther. 2006;8:209. doi: 10.1186/ar1957. [DOI] [PMC free article] [PubMed] [Google Scholar]


