Abstract
Klippel–Trenaunay syndrome (KTS) is a rare disorder characterized by triad of vascular malformations, varicose veins, and bony or soft tissue hypertrophy involving an extremity. Port wine stain is the most common vascular malformation associated with this syndrome. Various other rare vascular malformations described are angiokeratomas, angiokeratoma circumscriptum naeviformae, angiodermatitis, etc. This is the first instance, to the best of our knowledge, describing the capillary, venous, and lymphatic malformations in a same case of KTS.
Keywords: Klippel–Trenaunay syndrome, lymphangioma circumscriptum, multiple angiokeratomas, port wine stain
Introduction
Klippel–Trenaunay syndrome (KTS) is a rare disease of the vascular and lymphatic system or capillary malformation at birth associated with hypertrophy of the soft tissues/bones with an incidence of approximately 1:100,000 live births. Some authors hypothesized that embryonic mesodermal changes resulting in increased angiogenesis lead to increased vascular flow causing tissue hypertrophy and vascular changes.[1] Vascular malformations other than port wine stain that have been described in KTS are small angiokeratomas (AKs) or angiokeratoma circumscriptum naeviformae, angiodermatitis, cutaneous lymphangioma circumscriptum (CLC), and lymphoedema.[2]
Case Report
A 21-year-old female born out of nonconsanguineous marriage presented to us with hypertrophy of right lower limb with overlying reddish raised lesion since birth which gradually progressed to present size. She also complained of appearance of dark colored lesions over the pre-existing reddish lesion since 10–15 years, which initially appeared on thigh and progressed to involve right knee and upper right leg. She gave history of intermittent bleeding from the lesions.
On examination, the circumferences of right thigh (44 cm) and knee (31 cm) were greater than that of the left thigh (41 cm) and knee (29 cm) [Figure 1a]. Prominent varicosity of veins was present on dorsum of right foot [Figure 1b]. There was dark red blanchable patch suggestive of port wine stain present over right thigh, knee, and upper leg [Figure 2a]. Dermoscopy was performed using 3Gen Dermlite DL4 (CA, USA) 10× polarized mode. Dermoscopy of port wine stain showed dotted vessels and linear vessels [Figure 2b]. There were multiple brownish black hyperkeratotic papules distributed over right lower extremity [Figure 3a]. Dermoscopy of brownish black lesion showed multiple red lacunae, dark blue lacunae with few lacunae with whitish veil [Figure 3b and c], which was suggestive of AK, diagnosis of which was further confirmed on histopathology. There were multiple red–purple colored, verrucous vesicles with white to yellow secretion distributed over the right lower extremity [Figure 4a]. Dermoscopy of vesicular lesion revealed white to yellow lacunae surrounded by pale septa [Figure 4b and c] or yellow to pink lacunae alternating with dark red lacunae and few lacunae with feature of hypopyon [Figure 4d] which was suggestive of lymphangioma circumscriptum, which was confirmed further on histopathology.
Figure 1.

(a and b) The circumferences of right thigh (44 cm) and knee (31 cm) were greater than that of the left thigh (41 cm) and knee (29 cm) (a). Prominent varicosity of veins on dorsum of right foot (b)
Figure 2.
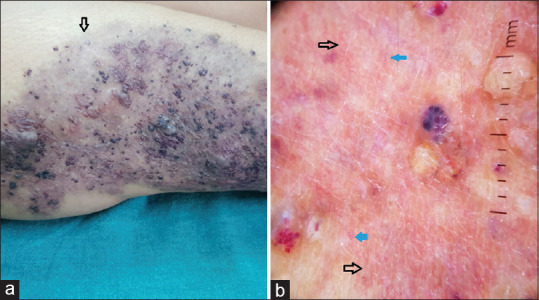
(a and b) Dark red blanchable patch suggestive of port wine present over right thigh, knee and upper leg (a). Dermoscopy (10× polarized mode) showed dotted vessels (blue arrow) and linear vessels (black arrow) (b)
Figure 3.
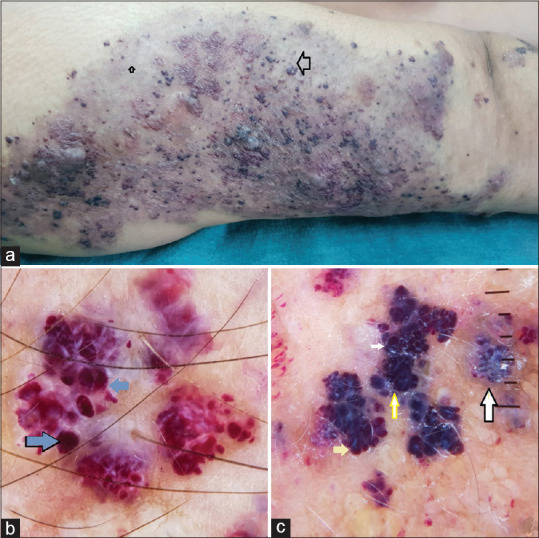
(a-c) Multiple brownish black hyperkeratotic papules distributed over right lower extremity (a). Dermoscopy (10× polarized mode) showed multiple red lacunae (blue arrow, (b), dark blue lacunae (yellow arrow) with few lacunae with whitish veil (white arrow) (c) suggestive of angiokeratoma
Figure 4.
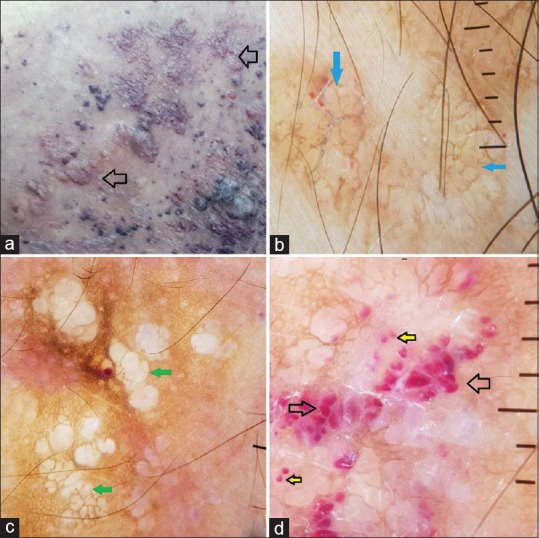
(a-d) Multiple red-purple colored, verrucous vesicles with white to yellow secretion over the right lower extremity (a). Dermoscopy (10× polarized mode) revealed white (blue arrow, (b) to yellow lacunae surrounded by pale septa (green arrow, (c), yellow to pink lacunae alternating with dark red lacunae (black arrow) and few lacunae with feature of hypopyon (yellow arrow) (d), suggestive of lymphangioma circumcriptum
Histopathalogical examination of dark hyperkeratotic lesion revealed acanthosis, hyperkeratosis, multiple blood filled ectatic, and congested thin walled blood vessels in papillary dermis with normal deep dermis and subcutaneous tissue, suggestive of AK [Figure 5a and b]. Histopathology of vesicular lesion revealed dilated lymphatic spaces lined by endothelial cells with few lymphocytes in superficial papillary dermis, suggestive of lymphangioma circumscriptum [Figure 6a and b]. General and systemic examination was normal. Routine hematological investigations were normal. Bilateral lower limb X-ray revealed diffuse soft tissue hypertrophy of right lower limb [Figure 7a] Local ultrasonography of affected limb revealed dilated vascular channels and lateral marginal vein over thigh [Figure 7b-d]. Magnetic resonance imaging (MRI) of bilateral lower limb revealed circumferential soft tissue hypertrophy and abnormal dilated vascular channels and lateral marginal vein suggestive of diffuse venolymphatic malformation of right lower limb [Figure 8a-d].
Figure 5.
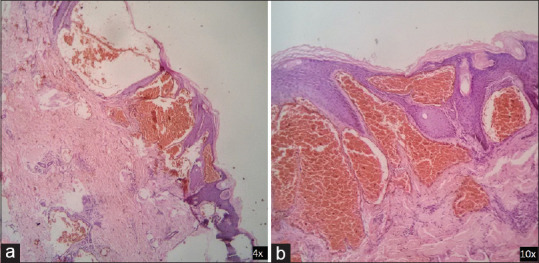
(a and b) Histopathalogical examination of dark hyperkeratotic lesion revealed acanthosis, hyperkeratosis, multiple blood-filled ectatic, and congested thin-walled blood vessels in papillary dermis with normal deep dermis and subcutaneous tissue, suggestive of angiokeratoma (Figure 5a, b H and E 4×,10×)
Figure 6.
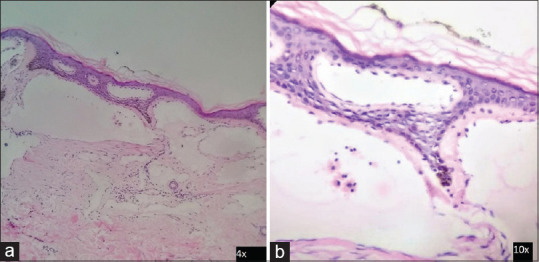
(a and b) Histopathology from vesicular lesion revealed dilated lymphatic spaces lined by endothelial cells with few lymphocytes in superficial papillary dermis, suggestive of lymphangioma circumscriptum (a and b H and E 4×,10×)
Figure 7.
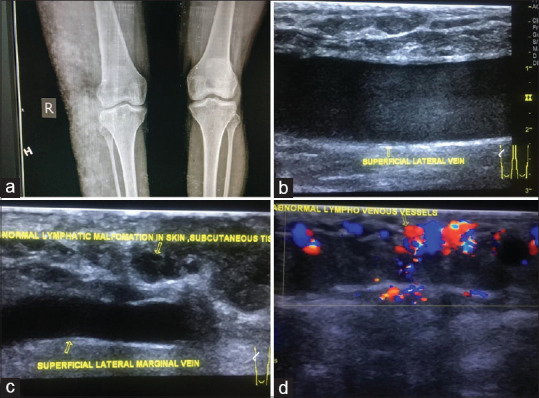
(a-d) Bilateral lower limb X-ray revealed diffuse soft tissue hypertrophy of right lower limb (a). Local ultrasonography of affected limb revealed dilated lateral marginal vein of thigh (b) abnormal dilated vascular channels and lateral marginal vein over thigh (c-d)
Figure 8.
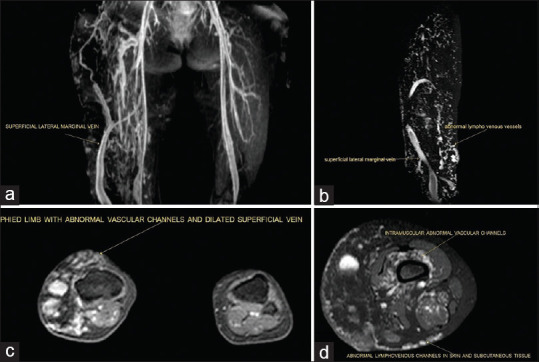
(a-d) MRI of bilateral lower limb revealed circumferential soft tissue hypertrophy and abnormal dilated vascular channels and lateral marginal vein suggestive of diffuse venolymphatic malformation of right lower limb (a-d)
On the basis of clinical examination, dermoscopy, histopathology, and radiological examination a final diagnosis of multiple angiokeratomas and lymphangioma circumscriptum associated with KTS was reached. Patient was referred to interventional radiology department for further management.
Discussion
Two French physicians Maurice Klippel and Paul Trenaunay described two patients with hemangiomatous lesions of the skin with associated bone and soft tissue hypertrophy and coined the term nevus variqueux osteohypertrophique in 1900.[3] Subsequently, Parkes Weber described arteriovenous fistulas in these patients in 1907. In 1965, Lindenauer proposed that the syndrome originally described by Klippel and Trenaunay without AV malformation be considered as a specific entity the KTS and the one associated with AV fistula be designated as Parkes Weber syndrome.[4] Most of the cases of KTS are sporadic although few reports of autosomal dominant inheritance are described. A mutation in angiogenic factor VG5Q has been proposed by Tian et al.[5] Varicosities may occur in deeper leg veins posing a risk of pulmonary embolism. Varicosities in organs like colon, urinary bladder, and brain may lead to rectal or urinary bleeding and seizures. It affects males more often than females. Jacob et al. defined KTS as the presence of any two of three features: (1) capillary malformations (CM), frequently located laterally; extension over the entire affected limb not obligatory; may be found at sites other than the hypertrophied limb; (2) soft tissue or bony hypertrophy; (3) varicose veins or venous malformations (VMs), often with persistent lateral embryologic veins. Our case had all features described by Jacob et al. 63% of patients with KTS have the manifestation of the complete triad (port-wine stain, varicose veins, and hypertrophy of soft tissues/bones).[6] Vascular malformations of KTS usually affect the capillary, venous, and lymphatic systems of the lower extremities. Rarely, these defects are seen in the upper extremities or bilateral or involve the trunk. Vascular malformations, involving the gastrointestinal and genitourinary tracts leading to bleeding, skeletal deformity, have been reported in KTS and can be a significant source of morbidity and even mortality.[7]
The characteristic dermoscopic features that have been described in literature for AK include well-demarcated round red lacunae, dark blue lacunae, and whitish veil that histologically correspond to dilated upper dermal vessels, vessel thrombosis to epidermal hyperkeratosis respectively.[8] We observed all these dermoscopic features in our case. The dermoscopic features of lymphangioma circumscriptum demonstrate two distinct patterns as yellow lacunae surrounded by pale septa without inclusion of blood (pattern 1) and yellow to pink lacunae alternating with dark red or bluish lacunae due to the inclusion of blood (pattern 2). Histopathologically, pattern 1 corresponds to dilated dermal and/or subcutaneous lymphatic vessels, which are filled with lymphatic fluid, while pattern corresponds to variable concentrations of red blood cells.[9] An additional dermoscopic feature which is typical of lymphangioma circumscriptum has recently been described as the “hypopyon-like feature.” As sedimentation of blood occurs, its corpuscles aggregate according to their density, with cellular components lying at the bottom and serum at the upper part, resulting in a color transition from dark to light in some lacunae, creating a similar effect to that seen on the eye-the hypopyon.[10] The new dermatologic metaphoric term is introduced to describe above peculiar feature as half-and-half lacuna.[11] Our case of lymphangioma circumscriptum showed all above described dermoscopic features.
There is paucity of literature describing associations of angiokeratomas and/orlymphangioma circumscriptum in KTS as depicted in Table 1. Management is largely conservative and the extent of diagnostic evaluation is determined by the planned treatment. Compression is an important part of conservative management. A multidisciplinary approach to management of KTS is warranted. Angiokeratoma and lymphangioma circumscriptum lesions can be treated with electrocoagulation, excision, cryotherapy, or laser treatment. This is the first instance, to the best of our knowledge, describing the capillary, venous and lymphatic malformations in a same case of KTS.
Table 1.
Vascular malformation associated with KTS
| Case report | Age/sex | Vascular malformations associated with KTS other than port wine stain |
|---|---|---|
| Prabhavathy et al. (1994)[12] | 5 year/F | Angiokeratomas |
| Kim et al. (2000)[13] | - | Lymphangioma circumscriptum |
| Mendiratta et al. (2004)[14] | 5 year/F | Angiokeratomatous lesion |
| Aggarwal (2009)[15] | Female infant | Angiokeratomas |
| Wankhade et al. (2014)[16] | 4 year/M | Angiokeratoma circumscriptum naeviformae |
| Sharma et al. (2015)[17] | 12 year/M | Angiokeratomas and lymphangiectatic lesions |
| Das et al. (2015)[18] | 2.5 year/M | Angiokeratoma circumscriptum naeviformae |
| Salunke et al. (2017)[19] | 13 year/F | Angiokeratomas |
| Liu et al. (2018)[20] | 31 year/F | Lymphangioma circumscriptum of vulva |
| Our case | 21 year/F | Angiokeratoma and lymphangioma circumscriptum |
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Baskerville PA, Ackroyd JS, Browse NL. The etiology of the Klippel-Trenaunay syndrome. Ann Surg. 1985;202:624–7. doi: 10.1097/00000658-198511000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Salman MM. Klippel-Trenaunay syndrome: Clinical features, complications, and management. Surg Today. 1997;27:735. doi: 10.1007/BF02384987. [DOI] [PubMed] [Google Scholar]
- 3.Klippel M, Trénaunay P. Du noevus variquex osteohypertrophiques. Arch Gen Med. 1900;3:641–72. [Google Scholar]
- 4.Lindenauer SM. The Klippel-Trenaunay syndrome: Varicosity, hypertrophy and hemangioma with no arteriovenous fistula. Ann Surg. 1965;162:303–14. doi: 10.1097/00000658-196508000-00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tian XL, Kadaba R, You SA, Liu M, Timur AA, Yang L, et al. Identification of an angiogenic factor that when mutated causes susceptibility to Klippel-Trenaunay syndrome. Nature. 2004;427:640–5. doi: 10.1038/nature02320.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacob AG, Driscoll DJ, Shaughnessy WJ, Stanson AW, Clay RP, Gloviczki P. Klippel-Trenaunay syndrome: Spectrum and management. Mayo Clin Proc. 1998;73:28–36. doi: 10.1016/S0025-6196(11)63615-X. [DOI] [PubMed] [Google Scholar]
- 7.Lee A, Driscoll D, Gloviczki P, Clay R, Shaughnessy W, Stans A. Evaluation and management of pain in patients with Klippel-Trenaunay syndrome: A review. Pediatrics. 2005;115:744–9. doi: 10.1542/peds.2004-0446. [DOI] [PubMed] [Google Scholar]
- 8.Zaballos P, Daufí C, Puig S, Argenziano G, Moreno-Ramírez D, Cabo H, et al. Dermoscopy of solitary angiokeratomas: A morphological study. Arch Dermatol. 2007;143:318–25. doi: 10.1001/archderm.143.3.318. [DOI] [PubMed] [Google Scholar]
- 9.Arpaia N, Cassano N, Vena GA. Dermoscopic features of cutaneous lymphangioma circumscriptum. Dermatol Surg. 2006;32:852–4. doi: 10.1111/j.1524-4725.2006.32174.x. [DOI] [PubMed] [Google Scholar]
- 10.Gencoglan G, Inanir I, Ermertcan AT. Hypopyon-like features: New dermoscopic criteria in the differential diagnosis of cutaneous lymphangioma circumscriptum and haemangiomas. J Eur Acad Venereol. 2012;26:1023–5. doi: 10.1111/j.1468-3083.2011.04136.x. [DOI] [PubMed] [Google Scholar]
- 11.Jha AK, Lallas A, Sonthalia S. Dermoscopy of cutaneous lymphangioma circumscriptum. Dermatol Pract Concept. 2017;7:37–8. doi: 10.5826/dpc.0702a08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prabhavathy D, Ratnavelu P, Sundraram M, Sugantha Klippel-trenaunay syndrome. Indian J Dermatol Venereol Leprol. 1994;60:161–2. [Google Scholar]
- 13.Kim JY, Lee JB, Lee SC, Won YH. A case of Klippel-Trenaunay syndrome with lymphangioma circumscriptum. Korean J Dermatol. 2000;38:1522–6. [Google Scholar]
- 14.Mendiratta V, Koranne RV, Sardana K, Hemal U, Solanki RS. Klippel trenaunay parkes-Weber syndrome. Indian J Dermatol Venereol Leprol. 2004;70:119–22. [PubMed] [Google Scholar]
- 15.Aggarwal K, Gupta S, Jain VK, Sen J, Nanda S. Klippel-Trenaunay syndrome in a newborn with multiple congenital anomalies. Indian J Dermatol Venereol Leprol. 2009;75:552. doi: 10.4103/0378-6323.55428. [DOI] [PubMed] [Google Scholar]
- 16.Wankhade V, Singh R, Sadhwani V, Kodate P, Disawal A. Angiokeratoma circumscriptum naeviforme with soft tissue hypertrophy and deep venous malformation: A variant of Klippel-Trenaunay syndrome? Indian Dermatol Online J. 2014;5:109–12. doi: 10.4103/2229-5178.146180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma D, Lamba S, Pandita A, Shastri S. Klippel-trénaunay syndrome - A very rare and interesting syndrome. Clin Med Insights Circ Respir Pulm Med. 2015;9:1–4. doi: 10.4137/CCRPM.S21645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Das D, Patil P, Tambe SA, Nayak CS. Angiokeratoma circumscriptum in a child of Klippel-Trenaunay syndrome: A rare association. Indian J Paediatr Dermatol. 2015;16:165–7. [Google Scholar]
- 19.Salunke AS, Chavan RB, Belgaumkar VA, Patil PP. A rare association of angiokeratoma circumscriptum with Klippel Trenaunay syndrome. Int J Res Dermatol. 2017;3:296–9. [Google Scholar]
- 20.Liu XY, Zhang S, Zhang H, Jia J, Cai L, Zhang JZ. Lymphangioma circumscriptum in vulva with Klippel Trenaunay syndrome. Chin Med J. 2018;131:490–1. doi: 10.4103/0366-6999.225066. [DOI] [PMC free article] [PubMed] [Google Scholar]


