Abstract
Background
Clinical trial reports often emphasize efficacy over harms, leading to misinterpretation of the risk‐to‐benefit ratio of new therapies. Clear and sufficiently detailed reporting of methods and results is especially important in the abstracts of trial reports, as readers often base their assessment of a trial on such information. In this study, we evaluated the quality of adverse event (AE) reporting and abstract quality in phase III randomized controlled trials (RCTs) of systemic therapies in breast and colorectal cancer.
Methods
Medline, EMBASE, Cochrane Database of RCTs, and Cochrane Database of Systematic Reviews were searched from November 2005 to September 2018. Phase III RCTs evaluating systemic therapies in breast or colorectal cancer were included. Each article was independently reviewed by two investigators using a standardized data extraction form based on guidelines developed by the Consolidated Standards of Reporting Trials (CONSORT) group. Descriptive statistics, bivariate analysis, and multivariable linear regression were used to analyze data. All statistical tests were two‐sided.
Results
Of 166 RCTs identified, 99.4% reported harms in the manuscript body, and 59.6% reported harms in the abstract. Reporting was restricted to severe harms in 15.6% of RCTs. Statistical comparison of AE rates went unreported in 59.0% of studies. Information regarding AEs leading to dose reductions, treatment discontinuations, or study withdrawals went unreported in 59.3%, 18.7%, and 86.8% of studies, respectively. Recently published RCTs (P = .009) and those sponsored at least partially by for‐profit companies (P = .003) had higher abstract quality scores.
Conclusions
Breast and colorectal cancer phase III RCTs inadequately report CONSORT‐compliant AE data. Improved guideline adherence and abstract reporting is required to properly weigh benefits and harms of new oncologic therapies.
Systematic Review Registration Number
CRD42019140673.
Keywords: adverse events, breast neoplasms, colorectal neoplasms, CONSORT, drug‐related side effects and adverse reactions, harms reporting, toxicities
Clinical trial reports often emphasize efficacy rather than toxicities of investigational agents, leading to misinterpretation of the risk‐to‐benefit ratio of new therapies. Here, we evaluated the quality of adverse event reporting in phase III randomized controlled trials of systemic therapies in breast and colorectal cancer. Our results show that most studies inadequately report adverse event data.
1. INTRODUCTION
Phase III randomized controlled trials (RCTs) assess the efficacy and harms of new treatment modalities in order to stringently determine their benefits and harms to patients. Accurate reporting is a necessary part of this determination: for example, inadequate reporting of adverse events (AEs) (harms) data can lead to misinterpretation of RCT results that may bias clinical decision‐making. 1 , 2 , 3
The treatment landscape in oncology has shifted away from the cyclical use of cytotoxic chemotherapies—typically associated with episodic, severe toxicities of short duration—toward continuously administered targeted treatments that may produce chronic, lower grade, and multi‐organ system toxicities. As a result of increasingly long‐term use of therapies, stringent AEs reporting has become more necessary. In addition, increasing sample sizes in oncologic RCTs of novel therapies has allowed the detection of smaller treatment effects 4 , 5
The Consolidated Standards of Reporting Trials (CONSORT) statement was introduced in 2001 as a way to standardize reporting in RCTs. 6 The CONSORT Harms Checklist was published in November 2004 to improve the reporting of AEs in order to foster both increased transparency and consistency of harms reporting in RCTs. 7
In 2008, Hopewell et al published a CONSORT reporting checklist for RCT abstracts in the hopes of encouraging more stringent reporting of harms. 8 This checklist takes into account the following: trial title, design description, eligibility criteria, interventions, specific hypothesis, primary outcome definition, description of randomization and blinding, number of patients randomized, trial status, number of patients analyzed, primary outcome effect size and precision, harms, general interpretation of the results, trial registration number, and source of funding. Seeing as many researchers glean trial information from an abstract, a clear set of harms reporting items specifically for abstracts is a vital extension of the CONSORT statement. 8
Unfortunately, adherence to the CONSORT reporting items remains suboptimal to the present day. Pitrou et al examined the reporting of safety results from the general medical literature in 2009, finding that 27.1% of studies analyzed did not provide information on severe AEs, and 47.4% did not provide information on withdrawal of patients due to an AE. 9 In the general medical literature, multiple studies have demonstrated that only half of phase III RCT abstracts report harms in an appropriate manner. 10 , 11 , 12 This trend has been echoed in other specialties, including critical care. 13 Examining metastatic solid tumor phase III RCT abstracts, Sivendran et al showed 74% reported serious or unexpected AEs, 14 while Ghimire et al demonstrated a 77% adherence to harms reporting in oncology phase III RCT abstracts. 15
The primary aim of this study was to systematically review and evaluate the quality of AE reporting in phase III breast and colorectal cancer RCTs. We also examined whether specific trial characteristics were associated with the quality of AE reporting, and could be predicted by an abstract quality score.
2. MATERIALS AND METHODS
2.1. Data sources
Medline, EMBASE, the Cochrane Database of Randomized Controlled Trials (CCRCT), and the Cochrane Database of Systematic Reviews (CDSR) were systematically searched in duplicate from November 2005 to 14 September 2018 using subject headings and keywords to capture breast cancer, colorectal cancer, AEs, and RCT terms (Breast Neoplasms; Colorectal Neoplasms; clinical trial, phase III; adverse drug reaction). The initial time point of November 2005 was chosen to capture studies published one calendar year after the introduction of the CONSORT AE reporting guidelines in November 2004. Subject headings and keywords were modified for each database according to its unique indexing terms. The search (Data S1) was conducted by a medical information specialist and limited to humans, with English language restrictions. Grey literature and reference lists of retrieved articles were also screened for additional relevant studies.
2.2. Study selection
This review was conducted and reported according to PRISMA guidelines, 16 and the study protocol was registered with the PROSPERO International Prospective Register of Systematic Reviews (CRD42019140673). The aim of this review was to examine the quality of AEs reporting in phase III RCTs of systemic therapies in breast and colorectal cancer. Thus, all phase III RCTs evaluating drug regimens (chemotherapy, endocrine therapy, immunotherapy, and targeted agents) in breast cancer or colorectal cancer patients were included. Studies were excluded if the patient population did not include breast cancer or colorectal cancer patients; if trials were evaluating surgical or radiotherapeutic treatment modalities; or if duplicate data were reported. Phase I, II, and IV RCTs, editorials, commentaries, reviews, cohort studies, and case‐control studies were excluded. Reference lists of excluded studies were screened to identify any potentially relevant studies. One reviewer (ASK) selected potentially eligible studies by independently screening titles and abstracts of identified studies. Full texts of the studies identified were subsequently retrieved and independently assessed for eligibility by one reviewer (ASK).
2.3. Data extraction
A data extraction form (Data S2) was developed based on the CONSORT Recommendations, as well as the CONSORT Harms Checklist. 6 , 7 The form was modified from a previously published checklist used to evaluate the quality of harms reporting in the general medical literature. 9 The data extraction form was designed to capture information from the both the abstract and the entire clinical trial report, and was divided into the following sections: methodology, sponsorship, results, reporting of AEs, reporting of severity, reporting of need for treatment discontinuations (TDs) and dose reductions (DRs), and reporting of statistical tests for AEs. AE data described in appendices or supplementary files were considered to be part of the “full text” of the included studies for the purposes of this review. Data were extracted independently by two reviewers (ASK and RCP).
During data extraction, an abstract quality score was assigned to each publication that took into account the following reporting items: explanation of study rationale; brief description of participants; description of intervention; explicit statement of primary endpoint; duration of follow‐up; reporting of planned sample size; p‐value or confidence interval reporting; description of AEs or toxicities; and specification of funding source.
2.4. Risk of bias assessment
The Cochrane Risk of Bias Tool for Randomized Controlled Trials 2.0 (RoB 2.0) was deemed appropriate for use in assessing the included studies, given that the studies under systematic review were RCTs. The RoB 2.0 rates studies as “low risk”, “unclear risk”, or “high risk” of bias using preestablished criteria to evaluate both study design and applicability. 17 Risk of bias was determined by a single reviewer (ASK).
2.5. Primary and secondary outcomes
The primary outcome was the evaluation of the quality of AE reporting according to the percentage of trials including detailed information on AEs (reporting of AEs in figure/table vs only text, per treatment arm, separation of expected/unexpected AEs, and scale used for AE severity) of dose reduction and treatment discontinuations in phase III RCTs of breast and colorectal cancer treatment regimens. The secondary outcome was based on an exploratory analysis of trial characteristics, with the aim of determining whether specific trial characteristics were associated with the quality of the abstract, as represented by a numerical score assigned during data extraction (see “Materials and Methods—Data Extraction”).
2.6. Statistical analysis
Statistical analysis was performed by a biostatistician using SAS 9.4 (Cary, SAS Institute). Descriptive statistics, including mean and standard deviation, were used for continuous variables, whereas categorical variables were described with frequencies and percentages and compared using the chi‐squared test. All statistical tests were two‐sided, and statistical significance was defined as P < .05. Bivariate linear analysis was used to examine the association between the abstract quality score assigned during data extraction and selected trial characteristics. Significant covariates found during bivariate analysis were used to run the multivariable linear regression model. Multivariable linear regression analysis was thus used to identify trial characteristics associated with inadequate safety reporting. Given the lack of sufficient homogeneity between included studies with regards to participants, interventions, and outcomes, a meaningful summary statistic could not be calculated; the clinical and methodological heterogeneity obviated the use of meta‐analysis on these studies.
3. RESULTS
3.1. Study characteristics
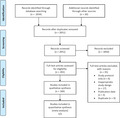
The literature search yielded 2034 abstracts; an additional 20 studies were identified through grey literature searches. After removal of duplicates and assessment by reviewers, 201 full texts were assessed for inclusion. 35 full texts were excluded from analysis, with reasoning provided in Data S3. Ultimately, 166 studies were included in this systematic review (Figure 1). 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 Characteristics of included studies are summarized in Table 1, whereas the complete set of consensus extracted data may be found in Data S4A (the data extraction set of Reviewer 1 is found in Data S4B, and the data extraction set of Reviewer 2 is found in Data S4C). All studies were published on or after November 2005, inclusive. The included studies cover each year of the date range captured by the search strategy, and represent diverse patient populations from North America, Europe, Asia, and Australia. Of the included studies, 121 (72.9%) evaluated any‐stage breast cancer, whereas 45 (27.1%) evaluated any‐stage colorectal cancer. Eighteen studies (10.8%) investigated neoadjuvant treatment regimens, whereas 51 (30.7%), 54 (32.5%), and 43 (25.9%) studies evaluated adjuvant, first‐line metastatic, and ≥second‐line metastatic treatment regimens, respectively. The median sample size of included studies was 627 patients (range: 51‐9779). A total of 138 included studies (83.1%) were at least partially funded by industry; however, only 38 studies (22.9%) explicitly stated provision of study drug by a for‐profit sponsor.
FIGURE 1.
PRISMA flow diagram
TABLE 1.
Characteristics of included studies (n = 166)
| Number of trials (n) | Percentage (%) | |
|---|---|---|
| Year of publication | ||
| 2005 | 3 | 1.81 |
| 2006 | 4 | 2.41 |
| 2007 | 9 | 5.42 |
| 2008 | 1 | 0.60 |
| 2009 | 9 | 5.42 |
| 2010 | 6 | 3.61 |
| 2011 | 8 | 4.82 |
| 2012 | 11 | 6.63 |
| 2013 | 12 | 7.23 |
| 2014 | 15 | 9.04 |
| 2015 | 10 | 6.02 |
| 2016 | 35 | 21.08 |
| 2017 | 25 | 15.06 |
| 2018 | 18 | 10.84 |
| Results of primary outcome | ||
| Positive | 100 | 60.2 |
| Negative | 65 | 39.2 |
| Lead trial region | ||
| North America | 40 | 24.1 |
| Europe | 86 | 51.8 |
| Asia | 33 | 19.9 |
| Other | 7 | 4.2 |
| Sponsorship | ||
| For profit | 100 | 60.2 |
| Non‐profit | 21 | 12.7 |
| Mixed | 38 | 22.9 |
| Not stated | 7 | 4.2 |
| Study drug provided by for profit company | ||
| Yes | 38 | 22.9 |
| No | 12 | 7.2 |
| Not reported | 116 | 69.9 |
| Tumor site | ||
| Breast | 121 | 72.9 |
| Colorectal | 45 | 27.1 |
| Line of therapy | ||
| Neoadjuvant | 18 | 10.8 |
| Adjuvant | 51 | 30.7 |
| Metastatic, first‐line | 54 | 32.5 |
| Metastatic, ≥second‐line | 43 | 25.9 |
| Primary outcome | ||
| Disease‐free survival (DFS) | 20 | 12.0 |
| Progression‐free survival (PFS) | 61 | 36.8 |
| Overall survival (OS) | 29 | 17.5 |
| Time to progression (TTP) | 8 | 4.8 |
| Other | 54 | 32.5 |
| Type of investigational therapy | ||
| Cytotoxic chemotherapy | 56 | 33.7 |
| Endocrine therapy | 19 | 11.4 |
| Targeted therapy | 19 | 11.4 |
| Combination of cytotoxic chemotherapy and endocrine therapy | 3 | 1.8 |
| Combination cytotoxic chemotherapy and targeted therapy | 49 | 29.5 |
| Other | 20 | 12.0 |
| Sample size (number of patients) | ||
| Median | 627 | |
| Mean | 1089.95 | |
| Range | 51‐9779 | |
3.2. Safety reporting
The main results of the harms reporting analysis are described in Table 2. Of the studies examined, 165 (99.4%) reported AEs in the body of the manuscript, and the majority of reports had at least one table/figure to report AEs (n = 159, 95.8%). While most (n = 162, 97.6%) manuscripts described AEs per arm, four included studies described AEs in only one arm. Severe AEs (typically greater than grade 3 on the Common Terminology Criteria for Adverse Events scale) were the sole reported type of AE in 26 studies (15.6%). Notably, a majority of studies (n = 98, 59.0%) did not perform a statistical comparison of AE rates between study arms.
TABLE 2.
Presentation of adverse events, dose reductions, and treatment discontinuation in the results section of trial publications (n = 166)
| No. of trials (n) | Percentage (%) | |
|---|---|---|
| Mode of presentation of adverse events (AEs) | ||
| Figure/Table | 159 | 95.8 |
| Text | 165 | 99.4 |
| Reported AEs per arm | 162 | 97.6 |
| Reported AEs in only one arm | 4 | 2.4 |
| Only severe AEs reported | 26 | 15.6 |
| Separation of expected/unexpected AEs | ||
| Yes | 4 | 2.4 |
| No | 162 | 97.6 |
| Statistical comparison of AE rates between study arms | ||
| Yes | 68 | 41.0 |
| No | 98 | 59.0 |
| Scale used to report AE severity | ||
| NCI CTCAE (all versions) | 143 | 86.1 |
| WHO | 6 | 3.6 |
| Other | 3 | 1.8 |
| No scale or unknown | 14 | 8.4 |
| Reporting of AEs leading to dose reductions | 67 | 40.7 |
| Reporting of AEs leading to treatment discontinuation | 135 | 81.3 |
| Reporting of AEs leading to withdrawal from study | 22 | 13.2 |
| Reporting of deaths due to AEs | 108 | 65.4 |
A scale for severity grading of AEs was identified in 91.5% (n = 152) of trials. The most commonly used scale—in 143 trials (86.1%)—was the Common Terminology Criteria for Adverse Events (CTCAE). A small number of trials (n = 14, 8.4%) omitted a severity scale or failed to report which scale was used. Notably absent from many of the included studies was information on AEs leading to dose reductions, treatment discontinuations, study withdrawal, or death. AEs leading to dose reduction or treatment discontinuation went unreported in 59.3% and 18.7% of studies, respectively. AEs leading to study withdrawal were not reported in 86.8% of studies, and no information on deaths due to AEs was reported in 34.6% of trials.
3.3. Abstract quality scoring
Linear regression of exploratory variables using abstract quality score as the dependent variable identified several significant trends outlined in Tables 3 and 4.
TABLE 3.
Results of regression analyses of trial characteristics predictive of abstract quality score
| Regression analysis | ||||||||
|---|---|---|---|---|---|---|---|---|
| Trial characteristic | Abstract quality score (0‐10) | Bivariate analysis | Multivariable analysis | |||||
| Mean | Regression coefficient estimate | t | P | Regression coefficient estimate | t | P | ||
| Year of publication, continuous | 6.8 | .09604 | 3.61 | .0004 | .08837 | 3.39 | .0013 | |
| Results of primary outcome | ||||||||
| Negative | 7.1 | −.115 | −0.58 | .5645 | Not investigated in model | |||
| Positive | 7.2 | n/a | n/a | n/a | Not investigated in model | |||
| Sponsorship | ||||||||
| Non‐industry | 6.9 | n/a | n/a | n/a | n/a | n/a | n/a | |
| Industry | 7.3 | .78786 | 3.03 | .0028 | .82252 | 3.17 | .0019 | |
| Mixed | 7.5 | .97838 | 3.23 | .0015 | .88939 | 3.01 | .0031 | |
| Intent of study therapy | ||||||||
| Curative | 7.2 | n/a | n/a | n/a | .31387 | 1.63 | .1050 | |
| Palliative | 7.1 | n/a | n/a | n/a | n/a | n/a | n/a | |
| Tumor site | ||||||||
| Breast | 7.2 | n/a | n/a | n/a | Not investigated in model | |||
| Colorectal | 7.1 | −.1107 | −0.51 | .6139 | Not investigated in model | |||
| Line of therapy | ||||||||
| Neoadjuvant | 6.9 | 7.33721 | −1.12 | .2627 | Not investigated in model | |||
| Adjuvant | 7.4 | .05495 | 0.21 | .8314 | Not investigated in model | |||
| Metastatic, first line | 6.9 | −.402 | −1.58 | .116 | Not investigated in model | |||
| Metastatic, ≥ second line | 7.3 | n/a | n/a | n/a | Not investigated in model | |||
| Type of investigational therapy | ||||||||
| Cytotoxic chemotherapy | 7.0 | −.0214 | −0.07 | .9475 | Not investigated in model | |||
| Endocrine therapy | 7.0 | −.0487 | −0.12 | .9031 | Not investigated in model | |||
| Targeted therapy | 7.8 | .76711 | 1.92 | .056 | Not investigated in model | |||
| Combination cytotoxic chemotherapy and endocrine therapy | 7.0 | −.075 | −0.1 | .9227 | Not investigated in model | |||
| Combination cytotoxic chemotherapy and targeted therapy | 7.2 | .10867 | 0.33 | .7429 | Not investigated in model | |||
| Other | 7.1 | n/a | n/a | n/a | Not investigated in model | |||
TABLE 4.
Overall P‐values for regression analyses of trial characteristics predictive of abstract quality score
| Trial characteristic | Overall P‐values | |
|---|---|---|
| Bivariate analysis | Multivariable analysis | |
| Intent of study therapy | .0034 | 0.0040 |
| Line of therapy | .1386 | Not investigated in model |
| Type of investigational therapy | .2724 | Not investigated in model |
The results of bivariate analysis demonstrated that a recent year of publication was significantly associated with a high‐abstract quality score (β = .096, t = 3.61, P = .0004). In addition, the provision of the study drug by a for‐profit sponsor was significantly associated with a high‐abstract quality score (β = .56, t = 2.48, P = .014).
The overall model fit for the final multivariable regression equation was R 2 = .14. Papers published in recent years had significantly higher abstract quality scores (P = .009). Compared with papers that received nonprofit sponsorship, those with either for‐profit (P = .002) or mixed sponsorship (P = .003) had significantly higher abstract quality scores. There was no statistically significant difference between the abstract quality scores of breast and colorectal cancer RCTs that were investigating curative vs palliative treatment regimens (P = .10).
3.4. Risk of bias
Of the included studies (n = 166), 164 were analyzed for risk of bias using the RoB 2.0 intention‐to‐treat checklist, while two papers were analyzed using the per‐protocol checklist. Of the 164 intention‐to‐treat studies, 49.4% were deemed overall to have a low risk of bias, 27.4% were deemed to have an unclear risk of bias, and 20.1% were deemed to have a high risk of bias. (Figure 2)(For the complete risk of bias data, see Data S5).
FIGURE 2.
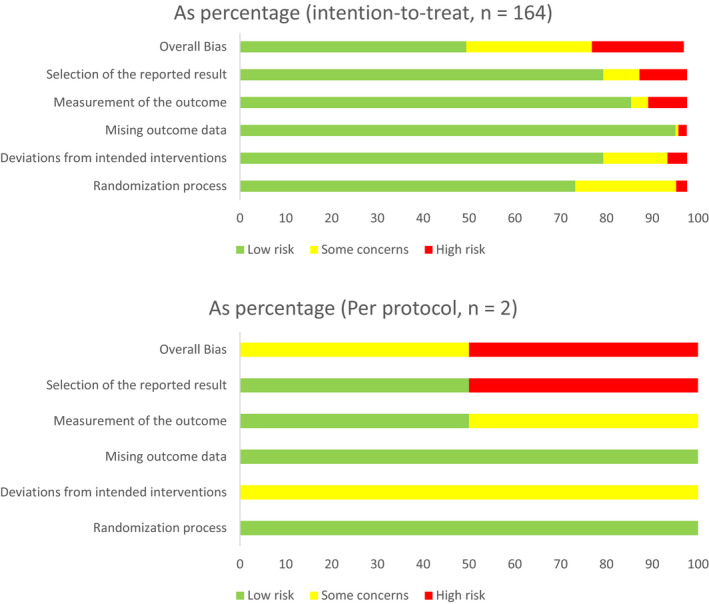
Risk of bias summary of included studies
Of the two per‐protocol studies, one had an unclear risk of bias, and one had a high risk of bias. Both studies had a low risk of bias in the “randomization process” and “missing outcome data” domains; both studies had an unclear risk of bias in the “deviation from intended interventions” domain; 50% had a low, and 50% had an unclear, risk of bias in the “outcome measurement” domain; finally, 50% had a low, and 50% had a high risk of bias in the “selection of reported result” domain.
4. DISCUSSION
In this systematic review, we evaluated the quality of AE reporting according to the CONSORT guidelines in phase III RCTs of drug regimens in breast and colorectal cancer patients between November 2005 and September 2018. Most studies do not adequately report harms as per the CONSORT guidelines. Although virtually all studies analyzed reported AEs in the main manuscript text (n = 165, 99.4%), 40.4% of reports either inadequately reported or did not include harms‐related results in the study abstract. A 2009 analysis of trial abstracts by Berwanger et al in four major medical journals found that only half reported AE data in their abstracts. 10 Another study in 2013 reiterated the finding of substandard AE reporting, with only 32% of breast cancer RCT abstracts adequately reporting harms. 184 The CONSORT authors and other groups have acknowledged the utility of stating AEs in phase III RCT abstracts: this data is important for not only establishing databases, but also retrieving appropriate information used in clinical decision‐making. 7 , 185
Severe AEs (typically greater than grade 3 on the Common Terminology Criteria for Adverse Events scale) were the sole reported type of AE in 26 studies (15.6%). Lower grade toxicities that are persistent over a prolonged period may be intolerable for patients if they have a negative impact on quality of life. For example, small molecule inhibitors—which are often offered in daily dosage regimens for some cancers—and the presence of chronic, low‐grade toxicities, may limit adherence to these treatments in routine practice. A lack of adherence to therapy would minimize the benefits observed in RCTs. Indeed, studies themselves may select for patient populations that underestimate the impact of low‐grade toxicities: eligible patients for RCTs typically have fewer comorbidities and higher performance statuses. Furthermore, the supportive care available to study patients may help mitigate the impact of low‐grade AEs on quality of life in a way that is not reproducible in routine practice. For example, clinical trial nurses, dosing diaries, structured dose modification criteria, and trial educational materials/programs all offer support outside typical practice norms. Thus, the sole reporting of severe AEs may severely limit the ability of oncologists to provide appropriate counsel to patients, mitigating their ability to provide supportive care when needed.
Among the studies we systematically reviewed, reporting of dose modification due to AEs was poor: dose reductions went unreported in 59.3%. These high figures represent a key flaw in the way most studies report their findings. Accurate reporting of dose reductions is important; it reflects whether the starting dose that is chosen for a RCT is appropriate and tolerable. An investigational agent that may be associated with few grade 3 or higher toxicities—but frequent low‐grade toxicities—may not be tolerable with prolonged administration. The recommended phase II dose (RP2D) and schedule of administration for an investigational agent is established during dose escalation phase I trials. There are a limited number of patients treated at the RP2D during phase I/II trials: these patients may not reflect the patient population enrolled in an RCT, or those who are treated outside of clinical trials in routine practice once an investigational agent has been approved by a regulatory body. Patients enrolled in phase I/II studies usually have advanced disease previously treated with multiple lines of prior therapy; they may only be treated an investigational agent for a short period of time, usually less than 6 months, and may be more willing to accept low‐grade toxicities that patients exposed to few lines of therapy, or with early stage disease treated in the adjuvant setting. In addition, phase I/II trials are usually performed by a small number of investigators who may be more experienced with toxicity management than phase III RCTs. In the adjuvant setting, patients may be less tolerable of low‐grade toxicities. Furthermore, for the palliative management of metastatic disease, the burden of harm and its often profound impact on quality of life must be balanced against improvements in disease‐related symptoms and survival.
Less than half (41.0%) of the RCTs examined included statistical comparisons of AEs between treatment arms. In addition, many studies did not identify the population used for safety analysis. Identifying the population used for safety analysis is likewise necessary, as the exclusion of any treated patients could bias the interpretation of harms‐related reporting.
Similar findings to those observed in our study of breast and colorectal cancer RCTs have been reported in other medical disciplines. In the general medical literature, Pitrou et al found that 18% of reports did not describe AEs with numerical data, and that information relating to the withdrawal of patients due to AEs was missing in 47% of papers. 9 In our study, we found that 18.7% of papers did not give information on the need to discontinue treatment due to AEs, whereas data on patient withdrawal due to AEs were missing in 86.8% of papers. Our study was also concordant with analyses in the oncology literature: for example, a 2016 paper by Maillet et al that reviewed oncology RCTs between 2007 and 2011 indicated that frequency and nature of grade 5 AEs were adequately reported in 50%, AEs leading to study withdrawal in 19%, and AEs leading to dose reduction in 13% of manuscripts. 186
Using bivariate and multivariable linear regression in an exploratory analysis, we examined whether any study characteristics were associated with the abstract quality scores we assigned during data extraction. Both bivariate and multivariable analyses showed that a recent year of publication was associated with a higher abstract quality score (P = .009, multivariable model).
We also examined whether industry‐sponsored studies had better reporting of AEs. An earlier study from the neurology literature of antiepileptic RCTs described a poor quality of AE reporting, 187 with improved safety reporting in studies sponsored by for‐profit companies, compared with studies having an academic hospital or cooperative group sponsor. Our study similarly found that industry‐sponsored studies tended to have improved AE reporting than those sponsored by nonprofit groups: those with either for‐profit (P = .002) or mixed sponsorship (P = .003) had significantly higher abstract quality scores. This may be due to the added costs of collecting detailed data on AEs, or possibly as a result of guidelines on data collection and reporting in pharmaceutical‐sponsored studies.
4.1. Limitations
A limitation of this study was that the search strategy was limited to English‐language publications; however, as there were no other restrictions and a large number of studies were included, this is unlikely to compromise this review's integrity. Overall, selection and performance biases were moderate across studies, while detection and attrition biases were generally low. The impact of selection and performance biases on the conclusions of this review is minimized by restricting the multivariable analysis to determining how well study abstracts report AEs data. A further limitation of this study is the lack of analysis of quality of life data which would allow situating our study more deeply in the patient‐centric experience.
5. CONCLUSION
Our systematic review highlights the incomplete reporting of harms in breast and colorectal cancer RCTs. A more complete description of harms is needed in order to better understand the therapeutic index of new treatments. We propose that adherence to the CONSORT AE statement should be a mandatory requirement of phase III RCT publication in medical journals, in order to ensure consistent reporting of harms data across trials. With the increasing use of immunotherapies and targeted therapies, oncologic RCTs in general may also require additional standards for the reporting of low‐grade toxicities that lead to dose interruptions, dose reductions, and treatment discontinuations. Such reporting standards may help indicate the tolerability of investigational agents administered over a long period of time and would move the RCT investigational paradigm closer to a more holistic, patient‐centered view of clinical outcomes.
CONFLICT OF INTEREST
The authors report no relevant conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception, design, collection of data, analysis, interpretation: ASK and RCP; writing, review and revision of manuscript: ASK and RCP. Funding acquisition and oncology expertise: HJM and RCP.
Supporting information
Data S1
Data S2
Data S3
Data S4A
Data S4B
Data S4C
Data S5
ACKNOWLEDGMENTS
The authors thank Xingshan Cao at the Institute for Clinical Evaluative Sciences at the University of Toronto for his expert help in statistical analysis.
Komorowski AS, MacKay HJ, Pezo RC. Quality of adverse event reporting in phase III randomized controlled trials of breast and colorectal cancer: A systematic review. Cancer Med. 2020;9:5035–5050. 10.1002/cam4.3095
DATA AVAILABILITY STATEMENT
Source data are available from the corresponding author on reasonable request.
REFERENCES
- 1. Ioannidis JP, Contopoulos‐Ioannidis DG. Reporting of safety data from randomised trials. Lancet. 1998;352:1752‐1753. [DOI] [PubMed] [Google Scholar]
- 2. Ioannidis JP, Lau J. Completeness of safety reporting in randomized trials: an evaluation of 7 medical areas. JAMA. 2001;285:437‐443. [DOI] [PubMed] [Google Scholar]
- 3. Loke YK, Derry S. Reporting of adverse drug reactions in randomised controlled trials ‐ a systematic survey. BMC Clin Pharmacol. 2001;1:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Booth CM, Cescon DW, Wang L, Tannock IF, Krzyzanowska MK. Evolution of the randomized controlled trial in oncology over three decades. J Clin Oncol. 2008;26:5458‐5464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Seruga B, Hertz PC, Wang L, et al. Absolute benefits of medical therapies in phase III clinical trials for breast and colorectal cancer. Ann Oncol. 2010;21:1411‐1418. [DOI] [PubMed] [Google Scholar]
- 6. Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomized trials. Ann Intern Med. 2001;134:657‐662. [DOI] [PubMed] [Google Scholar]
- 7. Ioannidis JP, Evans SJ, Gotzsche PC, et al. Better reporting of harms in randomized trials: an extension of the CONSORT statement. Ann Intern Med. 2004;141:781‐788. [DOI] [PubMed] [Google Scholar]
- 8. Hopewell S, Clarke M, Moher D, et al. CONSORT for reporting randomized controlled trials in journal and conference abstracts: explanation and elaboration. PLoS Med. 2008;5:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pitrou I, Boutron I, Ahmad N, Ravaud P. Reporting of safety results in published reports of randomized controlled trials. Arch Intern Med. 2009;169:1756‐1761. [DOI] [PubMed] [Google Scholar]
- 10. Berwanger O, Ribeiro RA, Finkelsztejn A, et al. The quality of reporting of trial abstracts is suboptimal: survey of major general medical journals. J Clin Epidemiol. 2009;62:387‐392. [DOI] [PubMed] [Google Scholar]
- 11. Hays M, Andrews M, Wilson R, Callender D, O'Malley PG, Douglas K. Reporting quality of randomised controlled trial abstracts among high‐impact general medical journals: a review and analysis. BMJ Open. 2016;6:e011082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ghimire S, Kyung E, Kang W, Kim E. Assessment of adherence to the CONSORT statement for quality of reports on randomized controlled trial abstracts from four high‐impact general medical journals. Trials. 2012;13:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kuriyama A, Takahashi N, Nakayama T. Reporting of critical care trial abstracts: a comparison before and after the announcement of CONSORT guideline for abstracts. Trials. 2017;18:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sivendran S, Newport K, Horst M, Albert A, Galsky MD. Reporting quality of abstracts in phase III clinical trials of systemic therapy in metastatic solid malignancies. Trials. 2015;16:341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ghimire S, Kyung E, Lee H, Kim E. Oncology trial abstracts showed suboptimal improvement in reporting: a comparative before‐and‐after evaluation using CONSORT for Abstract guidelines. J Clin Epidemiol. 2014;67:658‐666. [DOI] [PubMed] [Google Scholar]
- 16. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med. 2009;151:264‐269, w264. [DOI] [PubMed] [Google Scholar]
- 17. Higgins JPT, Savović JAC, Page MJ, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev. 2016;10(Suppl 1):.29–31. [Google Scholar]
- 18. Adjuvant Breast Cancer Trials Collaborative G . Polychemotherapy for early breast cancer: results from the international adjuvant breast cancer chemotherapy randomized trial. J Natl Cancer Inst. 2007;99:506‐515. [DOI] [PubMed] [Google Scholar]
- 19. Adjuvant Breast Cancer Trials Collaborative G . Ovarian ablation or suppression in premenopausal early breast cancer: results from the international adjuvant breast cancer ovarian ablation or suppression randomized trial. J Natl Cancer Inst. 2007;99:516‐525. [DOI] [PubMed] [Google Scholar]
- 20. Aebi SGS, Anderson S, Lang J, et al. Chemotherapy for isolated locoregional recurrence of breast cancer (CALOR): a randomised trial. The Lancet. Oncol. 2014;15:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Aihara T, Takatsuka Y, Ohsumi S, et al. Phase III randomized adjuvant study of tamoxifen alone versus sequential tamoxifen and anastrozole in Japanese postmenopausal women with hormone‐responsive breast cancer: N‐SAS BC03 study. Breast Cancer Res Treat. 2010;121:379‐387. [DOI] [PubMed] [Google Scholar]
- 22. Amadori D, Silvestrini R, De Lena M, et al. Randomized phase III trial of adjuvant epirubicin followed by cyclophosphamide, methotrexate, and 5‐fluorouracil (CMF) versus CMF followed by epirubicin in patients with node‐negative or 1–3 node‐positive rapidly proliferating breast cancer. Breast Cancer Res Treat. 2011;125:775‐784. [DOI] [PubMed] [Google Scholar]
- 23. André F, O'Regan R, Ozguroglu M, et al. Everolimus for women with trastuzumab‐resistant, HER2‐positive, advanced breast cancer (BOLERO‐3): a randomised, double‐blind, placebo‐controlled phase 3 trial. Lancet Oncol. 2014;15:580. [DOI] [PubMed] [Google Scholar]
- 24. Heinemann V, von Weikersthal LF, Decker T, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first‐line treatment for patients with metastatic colorectal cancer (FIRE‐3): a randomised, open‐label, phase 3 trial. Lancet Oncol. 2014;15:1065‐1075. [DOI] [PubMed] [Google Scholar]
- 25. Aparicio T, Lavau‐Denes S, Phelip JM, et al. Randomized phase III trial in elderly patients comparing LV5FU2 with or without irinotecan for first‐line treatment of metastatic colorectal cancer (FFCD 2001–02). Ann Oncol. 2016;27:121‐127. [DOI] [PubMed] [Google Scholar]
- 26. Awada A, Colomer R, Inoue K, et al. Neratinib plus paclitaxel vs trastuzumab plus paclitaxel in previously untreated metastatic ERBB2‐positive breast cancer: the NEfERT‐t randomized clinical trial. JAMA Oncol. 2016;2:1557‐1564. [DOI] [PubMed] [Google Scholar]
- 27. Baselga J, Bradbury I, Eidtmann H, et al. Lapatinib with trastuzumab for HER2‐positive early breast cancer (NeoALTTO): a randomised, open‐label, multicentre, phase 3 trial. Lancet. 2012;379:633‐640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Baselga J, Campone M, Piccart M, et al. Everolimus in postmenopausal hormone‐receptor‐positive advanced breast cancer. N Engl J Med. 2012;366:520‐529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Baselga J, Im SA, Iwata H, et al. Buparlisib plus fulvestrant versus placebo plus fulvestrant in postmenopausal, hormone receptor‐positive, HER2‐negative, advanced breast cancer (BELLE‐2): a randomised, double‐blind, placebo‐controlled, phase 3 trial. Lancet Oncol. 2017;18:904‐916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Baselga J, Manikhas A, Cortés J, et al. Phase III trial of nonpegylated liposomal doxorubicin in combination with trastuzumab and paclitaxel in HER2‐positive metastatic breast cancer. Ann Oncol. 2014;25:592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Baselga J, Zamagni C, Gómez P, et al. RESILIENCE: phase III randomized, double‐blind trial comparing sorafenib with capecitabine versus placebo with capecitabine in locally advanced or metastatic HER2‐negative breast cancer. Clin Breast Cancer. 2017;17:585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bear HD, Tang G, Rastogi P, et al. Bevacizumab added to neoadjuvant chemotherapy for breast cancer. N Engl J Med. 2012;366:310‐320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bergh J, Bondarenko IM, Lichinitser MR, et al. First‐line treatment of advanced breast cancer with sunitinib in combination with docetaxel versus docetaxel alone: results of a prospective, randomized phase III study. J Clin Oncol. 2012;30:921. [DOI] [PubMed] [Google Scholar]
- 34. Bergh J, Jönsson PE, Lidbrink EK, et al. FACT: an open‐label randomized phase III study of fulvestrant and anastrozole in combination compared with anastrozole alone as first‐line therapy for patients with receptor‐positive postmenopausal breast cancer. J Clin Oncol. 2012;30:1919. [DOI] [PubMed] [Google Scholar]
- 35. Big 1‐98 Collaborative Group . A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005;353:2747‐2757. [DOI] [PubMed] [Google Scholar]
- 36. Brufsky AM, Hurvitz S, Perez E, et al. RIBBON‐2: a randomized, double‐blind, placebo‐controlled, phase III trial evaluating the efficacy and safety of bevacizumab in combination with chemotherapy for second‐line treatment of human epidermal growth factor receptor 2‐negative metastatic breast cancer. J Clin Oncol. 2011;29:4286. [DOI] [PubMed] [Google Scholar]
- 37. Cameron D, Brown J, Dent R, et al. Adjuvant bevacizumab‐containing therapy in triple‐negative breast cancer (BEATRICE): primary results of a randomised, phase 3 trial. Lancet Oncol. 2013;14:933‐942. [DOI] [PubMed] [Google Scholar]
- 38. Cameron D, Morden JP, Canney P, et al. Accelerated versus standard epirubicin followed by cyclophosphamide, methotrexate, and fluorouracil or capecitabine as adjuvant therapy for breast cancer in the randomised UK TACT2 trial (CRUK/05/19): a multicentre, phase 3, open‐label, randomised, controlled trial. Lancet Oncol. 2017;18:929‐945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cascinu S, Rosati G, Nasti G, et al. Treatment sequence with either irinotecan/cetuximab followed by FOLFOX‐4 or the reverse strategy in metastatic colorectal cancer patients progressing after first‐line FOLFIRI/bevacizumab: an Italian Group for the Study of Gastrointestinal Cancer phase III, randomised trial comparing two sequences of therapy in colorectal metastatic patients. Eur J Cancer. 2017;83:106‐115. [DOI] [PubMed] [Google Scholar]
- 40. Cashin PH, Mahteme H, Spang N, et al. Cytoreductive surgery and intraperitoneal chemotherapy versus systemic chemotherapy for colorectal peritoneal metastases: a randomised trial. Eur J Cancer (Oxford, England). 2016;53:155‐162. [DOI] [PubMed] [Google Scholar]
- 41. Chan A, Delaloge S, Holmes FA, et al. Neratinib after trastuzumab‐based adjuvant therapy in patients with HER2‐positive breast cancer (ExteNET): a multicentre, randomised, double‐blind, placebo‐controlled, phase 3 trial. Lancet Oncol. 2016;17:367‐377. [DOI] [PubMed] [Google Scholar]
- 42. Chan S, Romieu G, Huober J, et al. Phase III study of gemcitabine plus docetaxel compared with capecitabine plus docetaxel for anthracycline‐pretreated patients with metastatic breast cancer. J Clin Oncol. 2009;27:1753. [DOI] [PubMed] [Google Scholar]
- 43. Chang W, Wei Y, Ren L, et al. Randomized controlled trial of intraportal chemotherapy combined with adjuvant chemotherapy (mFOLFOX6) for Stage II and III colon cancer. Ann Surg. 2016;263:434‐439. [DOI] [PubMed] [Google Scholar]
- 44. Chen J, Yao Q, Huang M, et al. A randomized Phase III trial of neoadjuvant recombinant human endostatin, docetaxel and epirubicin as first‐line therapy for patients with breast cancer (CBCRT01). Int J Cancer. 2018;142:2130‐2138. [DOI] [PubMed] [Google Scholar]
- 45. Chen X, Ye G, Zhang C, et al. Superior outcome after neoadjuvant chemotherapy with docetaxel, anthracycline, and cyclophosphamide versus docetaxel plus cyclophosphamide: results from the NATT trial in triple negative or HER2 positive breast cancer. Breast Cancer Res Treat. 2013;142:549. [DOI] [PubMed] [Google Scholar]
- 46. Cortes J, Perez‐Garcia J, Levy C, et al. Open‐label randomised phase III trial of vinflunine versus an alkylating agent in patients with heavily pretreated metastatic breast cancer. Ann Oncol. 2018;29:881‐887. [DOI] [PubMed] [Google Scholar]
- 47. Cortes J, O'Shaughnessy J, Loesch D, et al. Eribulin monotherapy versus treatment of physician's choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open‐label randomised study. Lancet (London, England). 2011;377:914. [DOI] [PubMed] [Google Scholar]
- 48. de Gramont A, Van Cutsem E, Schmoll HJ, et al. Bevacizumab plus oxaliplatin‐based chemotherapy as adjuvant treatment for colon cancer (AVANT): a phase 3 randomised controlled trial. Lancet Oncol. 2012;13:1225‐1233. [DOI] [PubMed] [Google Scholar]
- 49. Del Mastro L, Levaggi A, Michelotti A, et al. 5‐Fluorouracil, epirubicin and cyclophosphamide versus epirubicin and paclitaxel in node‐positive early breast cancer: a phase‐III randomized GONO‐MIG5 trial. Breast Cancer Res Treat. 2016;155:117‐126. [DOI] [PubMed] [Google Scholar]
- 50. Deng Y, Chi P, Lan P, et al. Modified FOLFOX6 with or without radiation versus fluorouracil and leucovorin with radiation in neoadjuvant treatment of locally advanced rectal cancer: initial results of the Chinese FOWARC multicenter, open‐label, randomized three‐arm phase iii trial. J Clin Oncol. 2016;34:3300‐3307. [DOI] [PubMed] [Google Scholar]
- 51. Di Leo A, Jerusalem G, Petruzelka L, et al. Results of the CONFIRM phase III trial comparing fulvestrant 250 mg with fulvestrant 500 mg in postmenopausal women with estrogen receptor‐positive advanced breast cancer. J Clin Oncol. 2010;28:4594‐4600. [DOI] [PubMed] [Google Scholar]
- 52. Di Leo A, Gomez HL, Aziz Z, et al. Phase III, double‐blind, randomized study comparing lapatinib plus paclitaxel with placebo plus paclitaxel as first‐line treatment for metastatic breast cancer. J Clin Oncol. 2008;26:5544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Dickler MN, Barry WT, Cirrincione CT, et al. Phase III trial evaluating letrozole as first‐line endocrine therapy with or without bevacizumab for the treatment of postmenopausal women with hormone receptor‐positive advanced‐stage breast cancer: CALGB 40503 (Alliance). J Clin Oncol. 2016;34:2602‐2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Douillard JY, Siena S, Cassidy J, et al. Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) Versus FOLFOX4 alone as first‐line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol. 2010;28:4697‐4705. [DOI] [PubMed] [Google Scholar]
- 55. Dubsky PC, Jakesz R, Mlineritsch B, et al. Tamoxifen and anastrozole as a sequencing strategy: a randomized controlled trial in postmenopausal patients with endocrine‐responsive early breast cancer from the Austrian Breast and Colorectal Cancer Study Group. J Clin Oncol. 2012;30:722. [DOI] [PubMed] [Google Scholar]
- 56. Ducreux M, Malka D, Mendiboure J, et al. Sequential versus combination chemotherapy for the treatment of advanced colorectal cancer (FFCD 2000–05): an open‐label, randomised, phase 3 trial. Lancet Oncol. 2011;12:1032‐1044. [DOI] [PubMed] [Google Scholar]
- 57. Ejlertsen B, Tuxen MK, Jakobsen EH, et al. Adjuvant cyclophosphamide and docetaxel with or without epirubicin for early top2a‐normal breast cancer: DBCG 07‐READ, an open‐label, phase III. Randomized Trial. J Clin Oncol. 2017;35:2639‐2646. [DOI] [PubMed] [Google Scholar]
- 58. Ellis P, Barrett‐Lee P, Johnson L, et al. Sequential docetaxel as adjuvant chemotherapy for early breast cancer (TACT): an open‐label, phase III, randomised controlled trial. The Lancet. 2009;373:1681‐1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Falandry C, Debled M, Bachelot T, et al. Celecoxib and exemestane versus placebo and exemestane in postmenopausal metastatic breast cancer patients: a double‐blind phase III GINECO study. Breast Cancer Res Treat. 2009;116:501‐508. [DOI] [PubMed] [Google Scholar]
- 60. Finn RS, Martin M, Rugo HS, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375:1925‐1936. [DOI] [PubMed] [Google Scholar]
- 61. Forbes JF, Sestak I, Howell A, et al. Anastrozole versus tamoxifen for the prevention of locoregional and contralateral breast cancer in postmenopausal women with locally excised ductal carcinoma in situ (IBIS‐II DCIS): a double‐blind, randomised controlled trial. Lancet (London, England). 2016;387:866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Foukakis T, von Minckwitz G, Bengtsson N‐O, et al. Effect of tailored dose‐dense chemotherapy vs standard 3‐weekly adjuvant chemotherapy on recurrence‐free survival among women with high‐risk early breast cancer: a randomized clinical trial. JAMA. 2016;316:1888‐1896. [DOI] [PubMed] [Google Scholar]
- 63. Fountzilas G, Dafni U, Papadimitriou C, et al. Dose‐dense sequential adjuvant chemotherapy followed, as indicated, by trastuzumab for one year in patients with early breast cancer: first report at 5‐year median follow‐up of a Hellenic Cooperative Oncology Group randomized phase III trial. BMC Cancer. 2014;14:515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gerard JP, Conroy T, Bonnetain F, et al. Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3–4 rectal cancers: results of FFCD 9203. J Clin Oncol. 2006;24:4620‐4625. [DOI] [PubMed] [Google Scholar]
- 65. Geyer CE, Forster J, Lindquist D, et al. Lapatinib plus capecitabine for HER2‐positive advanced breast cancer. N Engl J Med. 2006;355:2733‐2743. [DOI] [PubMed] [Google Scholar]
- 66. Gianni L, Mansutti M, Anton A, et al. Comparing neoadjuvant nab‐paclitaxel vs paclitaxel both followed by anthracycline regimens in women with ERBB2/ HER2‐negative breast cancer‐the evaluating treatment with neoadjuvant abraxane (ETNA) trial a randomized phase 3 clinical trial. JAMA Oncol. 2018;4:302‐308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Giantonio BJ, Catalano PJ, Meropol NJ, et al. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;25:1539‐1544. [DOI] [PubMed] [Google Scholar]
- 68. Gligorov J, Doval D, Bines J, et al. Maintenance capecitabine and bevacizumab versus bevacizumab alone after initial first‐line bevacizumab and docetaxel for patients with HER2‐negative metastatic breast cancer (IMELDA): a randomised, open‐label, phase 3 trial. Lancet Oncol. 2014;15:1351‐1360. [DOI] [PubMed] [Google Scholar]
- 69. Goetz MP, Toi M, Campone M, et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35:3638‐3646. [DOI] [PubMed] [Google Scholar]
- 70. Goss PE, Ingle JN, Pritchard KI, et al. Extending aromatase‐inhibitor adjuvant therapy to 10 years. N Engl J Med. 2016;375:209‐219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Goss PE, Smith IE, O'Shaughnessy J, et al. Adjuvant lapatinib for women with early‐stage HER2‐positive breast cancer: a randomised, controlled, phase 3 trial. Lancet Oncol. 2013;14:88‐96. [DOI] [PubMed] [Google Scholar]
- 72. Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo‐controlled, phase 3 trial. The Lancet. 2013;381:303‐312. [DOI] [PubMed] [Google Scholar]
- 73. Guan Z, Xu B, DeSilvio ML, et al. Randomized trial of lapatinib versus placebo added to paclitaxel in the treatment of human epidermal growth factor receptor 2‐overexpressing metastatic breast cancer. J Clin Oncol. 2013;31:1947. [DOI] [PubMed] [Google Scholar]
- 74. Guan ZZ, Xu JM, Luo RC, et al. Efficacy and safety of bevacizumab plus chemotherapy in chinese patients with metastatic colorectal cancer: a randomized phase iii artist trial. Chin J Cancer. 2011;30:682‐689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hagman H, Frodin JE, Berglund A, et al. A randomized study of KRAS‐guided maintenance therapy with bevacizumab, erlotinib or metronomic capecitabine after first‐line induction treatment of metastatic colorectal cancer: the Nordic ACT2 trial. Ann Oncol. 2016;27:140‐147. [DOI] [PubMed] [Google Scholar]
- 76. Hamaguchi T, Shimada Y, Mizusawa J, et al. Capecitabine versus S‐1 as adjuvant chemotherapy for patients with stage III colorectal cancer (JCOG0910): an open‐label, non‐inferiority, randomised, phase 3, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:47. [DOI] [PubMed] [Google Scholar]
- 77. Harbeck N, Huang CS, Hurvitz S, et al. Afatinib plus vinorelbine versus trastuzumab plus vinorelbine in patients with HER2‐overexpressing metastatic breast cancer who had progressed on one previous trastuzumab treatment (LUX‐Breast 1): an open‐label, randomised, phase 3 trial. Lancet Oncol. 2016;17:357‐366. [DOI] [PubMed] [Google Scholar]
- 78. Harbeck N, Saupe S, Jäger E, et al. A randomized phase III study evaluating pegylated liposomal doxorubicin versus capecitabine as first‐line therapy for metastatic breast cancer: results of the PELICAN study. Breast Cancer Res Treat. 2017;161:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. He K, Wang X, Guan X, et al. Vinorelbine plus gemcitabine or cisplatin as first‐line treatment of HER2‐negative advanced breast cancer. Anticancer Res. 2017;37:5647‐5653. [DOI] [PubMed] [Google Scholar]
- 80. Hecht JR, Mitchell E, Chidiac T, et al. A randomized phase IIIB trial of chemotherapy, bevacizumab, and panitumumab compared with chemotherapy and bevacizumab alone for metastatic colorectal cancer. J Clin Oncol. 2009;27:672‐680. [DOI] [PubMed] [Google Scholar]
- 81. Hickish T, Andre T, Wyrwicz L, et al. MABp1 as a novel antibody treatment for advanced colorectal cancer: a randomised, double‐blind, placebo‐controlled, phase 3 study. Lancet Oncol. 2017;18:192‐201. [DOI] [PubMed] [Google Scholar]
- 82. Hoff PM, Hochhaus A, Pestalozzi BC, et al. Cediranib plus FOLFOX/CAPOX versus placebo plus FOLFOX/CAPOX in patients with previously untreated metastatic colorectal cancer: a randomized, double‐blind, phase III study (HORIZON II). J Clin Oncol. 2012;30:3596‐3603. [DOI] [PubMed] [Google Scholar]
- 83. Hortobagyi GN, Stemmer SM, Burris HA, et al. Ribociclib as first‐line therapy for HR‐positive, advanced breast cancer. N Engl J Med. 2016;375:1738‐1748. [DOI] [PubMed] [Google Scholar]
- 84. Hu XC, Zhang J, Xu BH, et al. Cisplatin plus gemcitabine versus paclitaxel plus gemcitabine as first‐line therapy for metastatic triple‐negative breast cancer (CBCSG006): a randomised, open‐label, multicentre, phase 3 trial. Lancet Oncol. 2015;16:436. [DOI] [PubMed] [Google Scholar]
- 85. Hurvitz SA, Martin M, Symmans WF, et al. Neoadjuvant trastuzumab, pertuzumab, and chemotherapy versus trastuzumab emtansine plus pertuzumab in patients with HER2‐positive breast cancer (KRISTINE): a randomised, open‐label, multicentre, phase 3 trial. Lancet Oncol. 2018;19:115‐126. [DOI] [PubMed] [Google Scholar]
- 86. Hurvitz SA, Andre F, Jiang Z, et al. Combination of everolimus with trastuzumab plus paclitaxel as first‐line treatment for patients with HER2‐positive advanced breast cancer (BOLERO‐1): a phase 3, randomised, double‐blind, multicentre trial. Lancet Oncol. 2015;16:816. [DOI] [PubMed] [Google Scholar]
- 87. Iwamoto S, Takahashi T, Tamagawa H, et al. FOLFIRI plus bevacizumab as second‐line therapy in patients with metastatic colorectal cancer after firstline bevacizumab plus oxaliplatin‐based therapy: the randomized phase III EAGLE study. Ann Oncol. 2015;26:1427‐1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Janni W, Harbeck N, Rack B, et al. Randomised phase III trial of FEC120 vs EC‐docetaxel in patients with high‐risk node‐positive primary breast cancer: final survival analysis of the ADEBAR study. Br J Cancer. 2016;114:863‐871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Joensuu H, Kellokumpu‐Lehtinen PL, Huovinen R, et al. Adjuvant capecitabine in combination with docetaxel and cyclophosphamide plus epirubicin for breast cancer: an open‐label, randomised controlled trial. Lancet Oncol. 2009;10:1145‐1151. [DOI] [PubMed] [Google Scholar]
- 90. Johnston S, Pippen J Jr, Pivot X, et al. Lapatinib combined with letrozole versus letrozole and placebo as first‐line therapy for postmenopausal hormone receptor ‐ positive metastatic breast cancer. J Clin Oncol. 2009;27:5538‐5546. [DOI] [PubMed] [Google Scholar]
- 91. Johnston SRD, Hegg R, Im SA, et al. Phase III, Randomized study of dual human epidermal growth factor receptor 2 (HER2) blockade with lapatinib plus trastuzumab in combination with an aromatase inhibitor in postmenopausal women with HER2‐positive, hormone receptor‐positive metastatic breast cancer: ALTERNATIVE. J Clin Oncol. 2018;36:741‐748. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 92. Johnston SRD, Kilburn LS, Ellis P, et al. Fulvestrant plus anastrozole or placebo versus exemestane alone after progression on non‐steroidal aromatase inhibitors in postmenopausal patients with hormone‐receptor‐positive locally advanced or metastatic breast cancer (SoFEA): a composite, multicentre, phase 3 randomised trial. Lancet Oncol. 2013;14:989‐998. [DOI] [PubMed] [Google Scholar]
- 93. Jones SE, Savin MA, Holmes FA, et al. Phase III trial comparing doxorubicin plus cyclophosphamide with docetaxel plus cyclophosphamide as adjuvant therapy for operable breast cancer. J Clin Oncol. 2006;24:5381‐5387. [DOI] [PubMed] [Google Scholar]
- 94. Jonker DJ, Nott L, Yoshino T, et al. Napabucasin versus placebo in refractory advanced colorectal cancer: a randomised phase 3 trial. The Lancet. Gastroenterol Hepatol. 2018;3:263‐270. [DOI] [PubMed] [Google Scholar]
- 95. Kaufman B, Mackey JR, Clemens MR, et al. Trastuzumab plus anastrozole versus anastrozole alone for the treatment of postmenopausal women with human epidermal growth factor receptor 2‐positive, hormone receptor‐positive metastatic breast cancer: results from the randomized phase III TAnDEM study. J Clin Oncol. 2009;27:5529. [DOI] [PubMed] [Google Scholar]
- 96. Kaufman PA, Awada A, Twelves C, et al. Phase III open‐label randomized study of eribulin mesylate versus capecitabine in patients with locally advanced or metastatic breast cancer previously treated with an anthracycline and a taxane. J Clin Oncol. 2015;33:594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Kaufmann M, Graf E, Jonat W, et al. Tamoxifen versus control after adjuvant, risk‐adapted chemotherapy in postmenopausal, receptor‐negative patients with breast cancer: a randomized trial (GABG‐IV D‐93)–the German Adjuvant Breast Cancer Group. J Clin Oncol. 2005;23:7842‐7848. [DOI] [PubMed] [Google Scholar]
- 98. Kerr RS, Love S, Segelov E, et al. Adjuvant capecitabine plus bevacizumab versus capecitabine alone in patients with colorectal cancer (QUASAR 2): an open‐label, randomised phase 3 trial. Lancet Oncol. 2016;17:1543‐1557. [DOI] [PubMed] [Google Scholar]
- 99. Kim TW, Elme A, Kusic Z, et al. A phase 3 trial evaluating panitumumab plus best supportive care vs best supportive care in chemorefractory wild‐type KRAS or RAS metastatic colorectal cancer. Br J Cancer. 2016;115:1206‐1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kimura M, Tominaga T, Kimijima I, et al. Phase III randomized trial of toremifene versus tamoxifen for Japanese postmenopausal patients with early breast cancer. Breast Cancer. 2014;21:275‐283. [DOI] [PubMed] [Google Scholar]
- 101. Krop IE, Kim SB, Gonzalez‐Martin A, et al. Trastuzumab emtansine versus treatment of physician's choice for pretreated HER2‐positive advanced breast cancer (TH3RESA): a randomised, open‐label, phase 3 trial. Lancet Oncol. 2014;15:689‐699. [DOI] [PubMed] [Google Scholar]
- 102. Kummel S, Krocker J, Kohls A, et al. Randomised trial: survival benefit and safety of adjuvant dose‐dense chemotherapy for node‐positive breast cancer. Br J Cancer. 2006;94:1237‐1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Kwakman JJM, Simkens LHJ, van Rooijen JM, et al. Randomized phase III trial of S‐1 versus capecitabine in the first‐line treatment of metastatic colorectal cancer: SALTO study by the Dutch Colorectal Cancer Group. Ann Oncol. 2017;28:1288‐1293. [DOI] [PubMed] [Google Scholar]
- 104. Langley RE, Carmichael J, Jones AL, et al. Phase III trial of epirubicin plus paclitaxel compared with epirubicin plus cyclophosphamide as first‐line chemotherapy for metastatic breast cancer: United Kingdom National Cancer Research Institute trial AB01. J Clin Oncol. 2005;23:8322‐8330. [DOI] [PubMed] [Google Scholar]
- 105. Li J, Qin S, Xu RH, et al. Effect of fruquintinib vs placebo on overall survival in patients with previously treated metastatic colorectal cancer: the FRESCO randomized clinical trial. JAMA. 2018;319:2486‐2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Li J, Xu R, Qin S, et al. Aflibercept plus FOLFIRI in Asian patients with pretreated metastatic colorectal cancer: a randomized phase III study. Fut Oncol. 2018;14:2031‐2044. [DOI] [PubMed] [Google Scholar]
- 107. Litton JK, Rugo HS, Ettl J, et al. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med. 2018;379:753‐763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Loibl S, O'Shaughnessy J, Untch M, et al. Addition of the PARP inhibitor veliparib plus carboplatin or carboplatin alone to standard neoadjuvant chemotherapy in triple‐negative breast cancer (BrighTNess): a randomised, phase 3 trial. Lancet Oncol. 2018;19:497‐509. [DOI] [PubMed] [Google Scholar]
- 109. Lorusso V, Giotta F, Bordonaro R, et al. Non‐pegylated liposome‐encapsulated doxorubicin citrate plus cyclophosphamide or vinorelbine in metastatic breast cancer not previously treated with chemotherapy: a multicenter phase III study. Int J Oncol. 2014;45:2137. [DOI] [PubMed] [Google Scholar]
- 110. Loupakis F, Cremolini C, Masi G, et al. Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med. 2014;371:1609‐1618. [DOI] [PubMed] [Google Scholar]
- 111. Lück HJ, Du Bois A, Loibl S, et al. Capecitabine plus paclitaxel versus epirubicin plus paclitaxel as first‐line treatment for metastatic breast cancer: efficacy and safety results of a randomized, phase III trial by the AGO Breast Cancer Study Group. Breast Cancer Res Treat. 2013;139:779. [DOI] [PubMed] [Google Scholar]
- 112. Lück HJ, Lübbe K, Reinisch M, et al. Phase III study on efficacy of taxanes plus bevacizumab with or without capecitabine as first‐line chemotherapy in metastatic breast cancer. Breast Cancer Res Treat. 2015;149:141. [DOI] [PubMed] [Google Scholar]
- 113. Luo HY, Li YH, Wang W, et al. Single‐agent capecitabine as maintenance therapy after induction of XELOX (or FOLFOX) in first‐line treatment of metastatic colorectal cancer: randomized clinical trial of efficacy and safety. Ann Oncol. 2016;27:1074‐1081. [DOI] [PubMed] [Google Scholar]
- 114. Mackey R Jr, Ramos‐Vazquez M, Lipatov O, et al. Primary results of ROSE/TRIO‐12, a randomized placebo‐controlled phase III trial evaluating the addition of ramucirumab to first‐line docetaxel chemotherapy in metastatic breast cancer. J Clin Oncol. 2015;33:141. [DOI] [PubMed] [Google Scholar]
- 115. Margolese RG, Cecchini RS, Julian TB, et al. Anastrozole versus tamoxifen in postmenopausal women with ductal carcinoma in situ undergoing lumpectomy plus radiotherapy (NSABP B‐35): a randomised, double‐blind, phase 3 clinical trial. Lancet (London, England). 2016;387:849‐856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Martin M, Campone M, Bondarenko I, et al. Randomised phase III trial of vinflunine plus capecitabine versus capecitabine alone in patients with advanced breast cancer previously treated with an anthracycline and resistant to taxane. Ann Oncol. 2018;29:1195‐1202. [DOI] [PubMed] [Google Scholar]
- 117. Martin M, Ruiz A, Borrego MR, et al. Fluorouracil, doxorubicin, and cyclophosphamide (FAC) versus FAC followed by weekly paclitaxel as adjuvant therapy for high‐risk, node‐negative breast cancer: results from the GEICAM/2003‐02 study. J Clin Oncol. 2013;31:2593‐2599. [DOI] [PubMed] [Google Scholar]
- 118. Martin M, Segui MA, Anton A, et al. Adjuvant docetaxel for high‐risk, node‐negative breast cancer. N Engl J Med. 2010;363:2200‐2210. [DOI] [PubMed] [Google Scholar]
- 119. Sanofi P, Also A. Epirubicin plus cyclophosphamide followed by docetaxel versus epirubicin plus docetaxel followed by capecitabine as adjuvant therapy for node‐positive early breast cancer: results from the GEICAM/2003‐10 study. J Clin Oncol. 2015;33:3788. [DOI] [PubMed] [Google Scholar]
- 120. Masuda N, Lee S‐J, Ohtani S, et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med. 2017;376:2147‐2159. [DOI] [PubMed] [Google Scholar]
- 121. Masuda N, Sagara Y, Kinoshita T, et al. Neoadjuvant anastrozole versus tamoxifen in patients receiving goserelin for premenopausal breast cancer (STAGE): a double‐blind, randomised phase 3 trial. Lancet Oncol. 2012;13:345. [DOI] [PubMed] [Google Scholar]
- 122. Mavroudis D, Matikas A, Malamos N, et al. Dose‐dense FEC followed by docetaxel versus docetaxel plus cyclophosphamide as adjuvant chemotherapy in women with HER2‐negative, axillary lymph node‐positive early breast cancer: a multicenter randomized study by the Hellenic Oncology Research Group (HORG). Ann Oncol. 2016;27:1873‐1878. [DOI] [PubMed] [Google Scholar]
- 123. Miller K, Wang M, Gralow J, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med. 2007;357:2666‐2676. [DOI] [PubMed] [Google Scholar]
- 124. Miller KD, O'Neill A, Gradishar W, et al. Double‐blind phase III trial of adjuvant chemotherapy withand without bevacizumab in patients with lymph node‐positiveand high‐risk lymph node‐negative breast cancer (E5103). J Clin Oncol. 2018;36:2621‐2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Miyake Y, Nishimura J, Kato T, et al. Phase III trial comparing UFT + PSK to UFT + LV in stage IIB, III colorectal cancer (MCSGO‐CCTG). Surg Today. 2017;48(1):66‐72. [DOI] [PubMed] [Google Scholar]
- 126. Mobus V, von Minckwitz G, Jackisch C, et al. German Adjuvant Intergroup Node‐positive Study (GAIN): a phase III trial comparing two dose‐dense regimens (iddEPC versus ddEC‐PwX) in high‐risk early breast cancer patients. Ann Oncol. 2017;28:1803‐1810. [DOI] [PubMed] [Google Scholar]
- 127. Morales L, Canney P, Dyczka J, et al. Postoperative adjuvant chemotherapy followed by adjuvant tamoxifen versus nil for patients with operable breast cancer: a randomised phase III trial of the European Organisation for Research and Treatment of Cancer Breast Group. Eur J Cancer. 2007;43:331‐340. [DOI] [PubMed] [Google Scholar]
- 128. Oki E, Murata A, Yoshida K, et al. A randomized phase III trial comparing S‐1 versus UFT as adjuvant chemotherapy for stage II/III rectal cancer (JFMC35‐C1: ACTS‐RC). Ann Oncol. 2016;27:1266‐1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Pagani O, Regan MM, Walley BA, et al. Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. N Engl J Med. 2014;371:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Park IH, Sohn JH, Kim SB, et al. An open‐label, randomized, parallel, phase iii trial evaluating the efficacy and safety of polymeric micelle‐formulated paclitaxel compared to conventional cremophor El‐based paclitaxel for recurrent or metastatic HER2‐negative breast cancer. Cancer Res Treat. 2017;49:569‐577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Peeters M, Price TJ, Cervantes A, et al. Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second‐line treatment in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28:4706‐4713. [DOI] [PubMed] [Google Scholar]
- 132. Perez E, Awada A, O'Shaughnessy J, et al. Etirinotecan pegol (NKTR‐102) versus treatment of physician's choice in women with advanced breast cancer previously treated with an anthracycline, a taxane, and capecitabine (BEACON): a randomised, open‐label, multicentre, phase 3 trial. Lancet Oncol. 2015;16:1556. [DOI] [PubMed] [Google Scholar]
- 133. Perez EA, Barrios C, Eiermann W, et al. Trastuzumab emtansine with or without pertuzumab versus trastuzumab plus taxane for human epidermal growth factor receptor 2‐positive, advanced breast cancer: primary results from the phase III MARIANNE study. J Clin Oncol. 2017;35:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Piccart‐Gebhart M, Holmes E, Baselga J, et al. Adjuvant lapatinib and trastuzumab for early human epidermal growth factor receptor 2‐positive breast cancer: results from the randomized phase III adjuvant lapatinib and/or trastuzumab treatment optimization trial. J Clin Oncol. 2016;34:1034‐1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Pivot X, Bondarenko I, Nowecki Z, et al. Phase III, randomized, double‐blind study comparing the efficacy, safety, and immunogenicity of SB3 (trastuzumab biosimilar) and reference trastuzumab in patients treated with neoadjuvant therapy for human epidermal growth factor receptor 2‐positive early breast cancer. J Clin Oncol. 2018;36:968‐974. [DOI] [PubMed] [Google Scholar]
- 136. Price TJ, Peeters M, Kim TW, et al. Panitumumab versus cetuximab in patients with chemotherapy‐refractory wild‐type KRAS exon 2 metastatic colorectal cancer (ASPECCT): a randomised, multicentre, open‐label, non‐inferiority phase 3 study. Lancet Oncol. 2014;15:569‐579. [DOI] [PubMed] [Google Scholar]
- 137. Robertson JFR, Bondarenko IM, Trishkina E, et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor‐positive advanced breast cancer (FALCON): an international, randomised, double‐blind, phase 3 trial. The Lancet. 2016;388:2997‐3005. [DOI] [PubMed] [Google Scholar]
- 138. Robson M, Im SA, Senkus E, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377:523‐533. [DOI] [PubMed] [Google Scholar]
- 139. Rochlitz C, Bigler M, von Moos R, et al. SAKK 24/09: safety and tolerability of bevacizumab plus paclitaxel vs. bevacizumab plus metronomic cyclophosphamide and capecitabine as first‐line therapy in patients with HER2‐negative advanced stage breast cancer ‐ a multicenter, randomized phase III trial. BMC Cancer. 2016;16:780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Rugo HS, Barve A, Waller CF, et al. Effect of a proposed trastuzumab biosimilar compared with trastuzumab on overall response rate in patients With ERBB2 (HER2)‐positive metastatic breast cancer: a randomized clinical trial. JAMA. 2017;317:37‐47. [DOI] [PubMed] [Google Scholar]
- 141. Schippinger W, Samonigg H, Schaberl‐Moser R, et al. A prospective randomised phase III trial of adjuvant chemotherapy with 5‐fluorouracil and leucovorin in patients with stage II colon cancer. Br J Cancer. 2007;97:1021‐1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Schmid P, Untch M, Kosse V, et al. Leuprorelin acetate every‐3‐months depot versus cyclophosphamide, methotrexate, and fluorouracil as adjuvant treatment in premenopausal patients with node‐positive breast cancer: the TABLE study. J Clin Oncol. 2007;25:2509‐2515. [DOI] [PubMed] [Google Scholar]
- 143. Schmoll HJ, Cunningham D, Sobrero A, et al. Cediranib with mFOLFOX6 versus bevacizumab with mFOLFOX6 as first‐line treatment for patients with advanced colorectal cancer: a double‐blind, randomized phase III study (HORIZON III). J Clin Oncol. 2012;30:3588‐3595. [DOI] [PubMed] [Google Scholar]
- 144. Schwartzberg LS, Franco SX, Florance A, et al. Lapatinib plus letrozole as first‐line therapy for HER‐2+ hormone receptor‐positive metastatic breast cancer. Oncologist. 2010;15:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Seidman A, Brufsky A, Ansari RH, et al. Phase III trial of gemcitabine plus docetaxel versus capecitabine plus docetaxel with planned crossover to the alternate single agent in metastatic breast cancer. Ann Oncol. 2011;22:1094. [DOI] [PubMed] [Google Scholar]
- 146. Siu LL, Shapiro JD, Jonker DJ, et al. Phase III randomized, placebo‐controlled study of cetuximab plus brivanib alaninate versus cetuximab plus placebo in patients with metastatic, chemotherapy‐refractory, wild‐type K‐RAS colorectal carcinoma: the NCIC Clinical Trials Group and AGITG CO.20 trial. J Clin Oncol. 2013;31:2477‐2484. [DOI] [PubMed] [Google Scholar]
- 147. Sledge G, Toi M, Neven P, et al. MONARCH 2: abemaciclib in combination with fulvestrant in women with HR+/HER2− advanced breast cancer who had progressed while receiving endocrine. Therapy. 2017;35:2875‐2884. [DOI] [PubMed] [Google Scholar]
- 148. Smith I, Yardley D, Burris H, et al. Comparative efficacy and safety of adjuvant letrozole versus anastrozole in postmenopausal patients with hormone receptor‐positive, node‐positive early breast cancer: final results of the randomized phase III femara versus anastrozole clinical evaluation (FACE) trial. J Clin Oncol. 2017;35:1041‐1048. [DOI] [PubMed] [Google Scholar]
- 149. Sparano J, Makhson AN, Semiglazov VF, et al. Pegylated liposomal doxorubicin plus docetaxel significantly improves time to progression without additive cardiotoxicity compared with docetaxel monotherapy in patients with advanced breast cancer previously treated with neoadjuvant‐adjuvant anthracycline therapy: results from a randomized phase III study. J Clin Oncol. 2009;27:4522. [DOI] [PubMed] [Google Scholar]
- 150. Stebbing J, Baranau Y, Baryash V, et al. CT‐P6 compared with reference trastuzumab for HER2‐positive breast cancer: a randomised, double‐blind, active‐controlled, phase 3 equivalence trial. Lancet Oncol. 2017;18:917‐928. [DOI] [PubMed] [Google Scholar]
- 151. Steger GG, Greil R, Lang A, et al. Epirubicin and docetaxel with or without capecitabine as neoadjuvant treatment for early breast cancer: final results of a randomized phase III study (ABCSG‐24). Ann Oncol. 2014;25:366‐371. [DOI] [PubMed] [Google Scholar]
- 152. Taieb J, Tabernero J, Mini E, et al. Oxaliplatin, fluorouracil, and leucovorin with or without cetuximab in patients with resected stage III colon cancer (PETACC‐8): an open‐label, randomised phase 3 trial. Lancet Oncol. 2014;15:862. [DOI] [PubMed] [Google Scholar]
- 153. Takashima T, Mukai H, Hara F, et al. Taxanes versus S‐1 as the first‐line chemotherapy for metastatic breast cancer (SELECT BC): an open‐label, non‐inferiority, randomised phase 3 trial. Lancet Oncol. 2016;17:90. [DOI] [PubMed] [Google Scholar]
- 154. Thomas ES, Gomez HL, Li RK, et al. Ixabepilone plus capecitabine for metastatic breast cancer progressing after anthracycline and taxane treatment. J Clin Oncol. 2007;25:5210‐5217. [DOI] [PubMed] [Google Scholar]
- 155. Tol J, Koopman M, Cats A, et al. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N Engl J Med. 2009;360:563‐572. [DOI] [PubMed] [Google Scholar]
- 156. Tournigand C, Chibaudel B, Samson B, et al. Bevacizumab with or without erlotinib as maintenance therapy in patients with metastatic colorectal cancer (GERCOR DREAM; OPTIMOX3): a randomised, open‐label, phase 3 trial. Lancet Oncol. 2015;16:1493‐1505. [DOI] [PubMed] [Google Scholar]
- 157. Tredan O, Follana P, Moullet I, et al. A phase III trial of exemestane plus bevacizumab maintenance therapy in patients with metastatic breast cancer after first‐line taxane and bevacizumab: a GINECO group study. Ann Oncol. 2016;27:1020‐1029. [DOI] [PubMed] [Google Scholar]
- 158. Tripathy D, Im SA, Colleoni M, et al. Ribociclib plus endocrine therapy for premenopausal women with hormone‐receptor‐positive, advanced breast cancer (MONALEESA‐7): a randomised phase 3 trial. Lancet Oncol. 2018;19:904‐915. [DOI] [PubMed] [Google Scholar]
- 159. Turner NC, Ro J, André F, et al. Palbociclib in hormone‐receptor‐positive advanced breast cancer. N Engl J Med. 2015;373:209. [DOI] [PubMed] [Google Scholar]
- 160. Untch M, Jackisch C, Schneeweiss A, et al. Nab‐paclitaxel versus solvent‐based paclitaxel in neoadjuvant chemotherapy for early breast cancer (GeparSepto‐GBG 69): a randomised, phase 3 trial. Lancet Oncol. 2016;17:345‐356. [DOI] [PubMed] [Google Scholar]
- 161. Untch M, Loibl S, Bischoff J, et al. Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline‐taxane‐based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol. 2012;13:135. [DOI] [PubMed] [Google Scholar]
- 162. Van Cutsem E, Peeters M, Siena S, et al. Open‐label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy‐refractory metastatic colorectal cancer. J Clin Oncol. 2007;25:1658‐1664. [DOI] [PubMed] [Google Scholar]
- 163. Van De Velde CJ, Rea D, Seynaeve C, et al. Adjuvant tamoxifen and exemestane in early breast cancer (TEAM): a randomised phase 3 trial. The Lancet. 2011;377:321‐331. [DOI] [PubMed] [Google Scholar]
- 164. Van Hazel GA, Heinemann V, Sharma NK, et al. SIRFLOX: randomized phase III trial comparing first‐line mFOLFOX6 (Plus or Minus Bevacizumab) versus mFOLFOX6 (Plus or Minus Bevacizumab) plus selective internal radiation therapy in patients with metastatic colorectal cancer. J Clin Oncol. 2016;34:1723‐1731. [DOI] [PubMed] [Google Scholar]
- 165. Venook AP, Niedzwiecki D, Lenz HJ, et al. Effect of first‐line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients with KRAS wild‐type advanced or metastatic colorectal cancer: a randomized clinical trial. JAMA. 2017;317:2392‐2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. von Minckwitz G, Colleoni M, Kolberg HC, et al. Efficacy and safety of ABP 980 compared with reference trastuzumab in women with HER2‐positive early breast cancer (LILAC study): a randomised, double‐blind, phase 3 trial. Lancet Oncol. 2018;19:987‐998. [DOI] [PubMed] [Google Scholar]
- 167. von Minckwitz G, Procter M, de Azambuja E, et al. Adjuvant pertuzumab and trastuzumab in early HER2‐positive breast cancer. N Engl J Med. 2017;2017:122‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. von Minckwitz G, Puglisi F, Cortes J, et al. Bevacizumab plus chemotherapy versus chemotherapy alone as second‐line treatment for patients with HER2‐negative locally recurrent or metastatic breast cancer after first‐line treatment with bevacizumab plus chemotherapy (TANIA): an open‐label, randomised phase 3 trial. Lancet Oncol. 2014;15:1269. [DOI] [PubMed] [Google Scholar]
- 169. Welt A, Marschner N, Lerchenmueller C, et al. Capecitabine and bevacizumab with or without vinorelbine in first‐line treatment of HER2/neu‐negative metastatic or locally advanced breast cancer: final efficacy and safety data of the randomised, open‐label superiority phase 3 CARIN trial. Breast Cancer Res Treat. 2016;156:97‐107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Wolff AC, Lazar AA, Bondarenko I, et al. Randomized phase III placebo‐controlled trial of letrozole plus oral temsirolimus as first‐line endocrine therapy in postmenopausal women with locally advanced or metastatic breast cancer. J Clin Oncol. 2013;31:196‐202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Xu B, Jiang Z, Shao Z, et al. Fulvestrant 250 mg versus anastrozole for Chinese patients with advanced breast cancer: results of a multicentre, double‐blind, randomised phase III trial. Cancer Chemother Pharmacol. 2011;67:223. [DOI] [PubMed] [Google Scholar]
- 172. Xu J, Kim TW, Shen L, et al. Results of a randomized, double‐blind, placebo‐controlled, phase III trial of trifluridine/tipiracil (TAS‐102) monotherapy in Asian patients with previously treated metastatic colorectal cancer: the TERRA study. J Clin Oncol. 2018;36:350‐358. [DOI] [PubMed] [Google Scholar]
- 173. Xu RH, Muro K, Morita S, et al. Modified XELIRI (capecitabine plus irinotecan) versus FOLFIRI (leucovorin, fluorouracil, and irinotecan), both either with or without bevacizumab, as second‐line therapy for metastatic colorectal cancer (AXEPT): a multicentre, open‐label, randomised, non‐inferiority, phase 3 trial. Lancet Oncol. 2018;19:660‐671. [DOI] [PubMed] [Google Scholar]
- 174. Yalcin S, Uslu R, Dane F, et al. Bevacizumab + capecitabine as maintenance therapy after initial bevacizumab + XELOX treatment in previously untreated patients with metastatic colorectal cancer: phase III 'stop and go' study results‐A Turkish oncology group trial. Oncology (Switzerland). 2013;85:328‐335. [DOI] [PubMed] [Google Scholar]
- 175. Yamada Y, Takahari D, Matsumoto H, et al. Leucovorin, fluorouracil, and oxaliplatin plus bevacizumab versus S‐1 and oxaliplatin plus bevacizumab in patients with metastatic colorectal cancer (SOFT): an open‐label, non‐inferiority, randomised phase 3 trial. Lancet Oncol. 2013;14:1278‐1286. [DOI] [PubMed] [Google Scholar]
- 176. Yamamoto D, Sato N, Rai Y, et al. Efficacy and safety of low‐dose capecitabine plus docetaxel versus single‐agent docetaxel in patients with anthracycline‐pretreated HER2‐negative metastatic breast cancer: results from the randomized phase III JO21095 trial. Breast Cancer Res Treat. 2017;161:473‐482. [DOI] [PubMed] [Google Scholar]
- 177. Yamazaki K, Nagase M, Tamagawa H, et al. Randomized phase III study of bevacizumab plus FOLFIRI and bevacizumab plus mFOLFOX6 as first‐line treatment for patients with metastatic colorectal cancer (WJOG4407G). Ann Oncol. 2016;27:1539‐1546. [DOI] [PubMed] [Google Scholar]
- 178. Yardley DA, Arrowsmith ER, Daniel BR, et al. TITAN: phase III study of doxorubicin/cyclophosphamide followed by ixabepilone or paclitaxel in early‐stage triple‐negative breast cancer. Breast Cancer Res Treat. 2017;164:649‐658. [DOI] [PubMed] [Google Scholar]
- 179. Zdenkowski N, Forbes JF, Boyle FM, et al. Observation versus late reintroduction of letrozole as adjuvant endocrine therapy for hormone receptorpositive breast cancer (ANZ0501 LATER): an open‐label randomised, controlled trial. Ann Oncol. 2016;27:806‐812. [DOI] [PubMed] [Google Scholar]
- 180. Zhang M, Wei W, Liu J, et al. Comparison of the effectiveness and toxicity of neoadjuvant chemotherapy regimens, capecitabine/epirubicin/cyclophosphamide vs 5‐fluorouracil/epirubicin/cyclophosphamide, followed by adjuvant, capecitabine/docetaxel vs docetaxel, in patients with operable breast cancer. Onco Targets Ther. 2016;9:3443‐3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Zhang P, Sun T, Zhang Q, et al. Utidelone plus capecitabine versus capecitabine alone for heavily pretreated metastatic breast cancer refractory to anthracyclines and taxanes: a multicentre, open‐label, superiority, phase 3, randomised controlled trial. Lancet Oncol. 2017;18:371‐383. [DOI] [PubMed] [Google Scholar]
- 182. Zhou Y, Ouyang T, Xie Y, et al. A single‐center, randomized, parallel controlled study comparing the efficacy and safety aspects of three anthracycline‐based regimens as neoadjuvant chemotherapy in primary breast cancer. Breast Cancer Res Treat. 2016;157:527‐534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Zielinski C, Lang I, Inbar M, et al. Bevacizumab plus paclitaxel versus bevacizumab plus capecitabine as first‐line treatment for HER2‐negative metastatic breast cancer (TURANDOT): primary endpoint results of a randomised, open‐label, non‐inferiority, phase 3 trial. Lancet Oncol. 2016;17:1230‐1239. [DOI] [PubMed] [Google Scholar]
- 184. Vera‐Badillo FE, Shapiro R, Ocana A, Amir E, Tannock IF. Bias in reporting of end points of efficacy and toxicity in randomized, clinical trials for women with breast cancer. Ann Oncol. 2013;24:1238‐1244. [DOI] [PubMed] [Google Scholar]
- 185. Derry S, Loke YK, Aronson JK. Incomplete evidence: the inadequacy of databases in tracing published adverse drug reactions in clinical trials. BMC Med Res Methodol. 2001;1:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Maillet D, Blay JY, You B, Rachdi A, Gan HK, Peron J. The reporting of adverse events in oncology phase III trials: a comparison of the current status versus the expectations of the EORTC members. Ann Oncol. 2016;27:192‐198. [DOI] [PubMed] [Google Scholar]
- 187. Shukralla AA, Tudur‐Smith C, Powell GA, Williamson PR, Marson AG. Reporting of adverse events in randomised controlled trials of antiepileptic drugs using the CONSORT criteria for reporting harms. Epilepsy Res. 2011;97:20‐29. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Data S2
Data S3
Data S4A
Data S4B
Data S4C
Data S5
Data Availability Statement
Source data are available from the corresponding author on reasonable request.


