Abstract
Objective
To report and analyze the causes and outcomes of malpractice litigation in ophthalmic trauma.
Methods
The Westlaw® database was reviewed for ophthalmology litigation in the United States between 1930 and 2014. All ophthalmic trauma cases were included and compared to non-traumatic ophthalmology malpractice cases.
Results
Forty-four ophthalmic trauma cases were included. Of these cases, 90.9% of ophthalmic trauma plaintiffs were male compared to 54.8% of plaintiffs in ophthalmology as a whole (P=<0.001); 34.1% of cases involved minor plaintiffs compared to 6.4% in ophthalmology as a whole (P=<0.001). Cases involving minors were more likely to be resolved in favor of the plaintiff than cases involving adult plaintiffs (53.3% vs 37.9%); however, this was not found to statistically significant (P=0.35). Overall, 54.5% of cases were resolved in favor of defendants; 40.9% of cases were resolved via jury trial with 50.0% resulting in payments to plaintiffs compared to the 29.6% rate of plaintiff verdicts in ophthalmology as a whole. Open globe injuries represented 61.4% of cases; 55.6% of these cases had intraocular foreign bodies and 37.0% developed endophthalmitis. Most cases (63.6%) alleged insufficient intervention. Of these cases, 31.8% of cases involved surgical or procedural claims, and 4.5% involved medical claims only.
Conclusion
Males and minors were overrepresented among plaintiffs in ocular trauma litigation. Most cases involved open globe injuries, often complicated by retained intraocular foreign bodies and endophthalmitis. Analysis of malpractice litigation in ophthalmic trauma calls attention to commonly litigated scenarios to improve clinical practice and to inform risk management.
Keywords: malpractice, litigation, risk, trauma, intraocular foreign body, open globe, orbital fracture, endophthalmitis
Introduction
A recent report indicates that between the years 1992 and 2014, the rate of paid malpractice claims in the United States decreased substantially; however, awards with payments greater than $1 million increased.1 Although the last two decades have seen decreasing plaintiff verdicts and tort reform,1,2 the extent to which these changes have influenced the practice of defensive medicine is unclear. Prior studies have found high rates of self-reported practice of defensive medicine and have shown that rates of physician concern about malpractice risk do not vary greatly in states with and without tort reform or with high or low litigation risk.2–4 Between 5 and 10% of ophthalmologists face a malpractice claim each year, representing a significant burden on ophthalmologists, insurers, and the public.5 Analysis of malpractice claims in ophthalmology increases physician awareness of common causes of litigation with the purpose of highlighting high-risk clinical and surgical situations, leading both to better patient care and to a deeper insight into how to avoid malpractice claims.
Ophthalmic trauma is a common cause of vision loss around the world responsible for an estimated 19 million cases of monocular blindness, representing a significant cause of loss of productivity and decreased quality of life.6 Ophthalmic trauma involves a number of potentially high-risk scenarios and opportunities for easily missed diagnoses, surgical and treatment delays, and inappropriately high patient expectations for visual recovery. Because of these factors, descriptive analysis of malpractice in ophthalmic trauma in the Westlaw® (Thompson Reuters, New York, NY) legal database was completed as a means of drawing attention to clinical scenarios that place both the patient and physician at high risk.
Materials and Methods
Westlaw® is a legal database that contains verdicts, rulings, and formal settlements in all 50 states. The jury verdict and settlements section of WestlawNext legal database collects jury verdicts that commercial vendors have deemed important either due to precedence or content. It does not contain all cases of litigation performed in the United States. As described in previous publications,7–10 the database was queried to search all US civil trials involving ophthalmologists using the search terms “ophthalmology” or “ophthalmologist” and “malpractice” anywhere in the retrieved documents. Exclusion criteria included (1) ophthalmologist named as expert witness but not defendant, and (2) filings before January 1, 1930 or after Dec 31, 2014. All search results that referenced malpractice litigation but that were not themselves malpractice lawsuits were excluded. Lawsuits with more than one Westlaw® citation were combined and represented as a single case. Record review included date of occurrence, year of suit, defendant, geography, patient age, patient sex, diagnosis, outcome, presence of disability, nature of injury, plaintiff legal allegation, indemnity, verdict, and plaintiff award. Because all data in this study are publicly available and no human subjects were involved, Institutional Review Board review and informed consent were not required.
Not all information was available for every case. Cases were also categorized by intervention (surgical/procedural, medical, or noninterventional) and by subspecialty focus by a faculty ophthalmologist. The subspecialty focus of the case was defined based on the nature of the allegation rather than the subspecialty training of the physician defendant. Cases focusing on care following globe or orbit trauma were classified as traumatic. Monetary awards were adjusted for inflation to 2015 US dollars (http://www.bls.gov/data/inflation_calculator.htm) to permit meaningful comparison.
In this analysis, all malpractice litigation involving ophthalmic trauma was identified from a database of 1063 ophthalmology litigation cases and analyzed. Results were compared to all non-trauma cases in the database. Descriptive statistics were used to report our findings, and, when appropriate, the Student’s t-test (MedCalc for Windows, Microsoft Excel for Windows) was used to compare groups.
Results
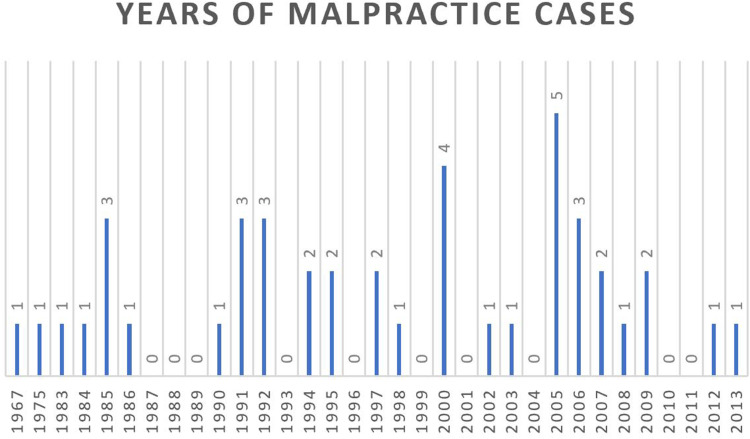
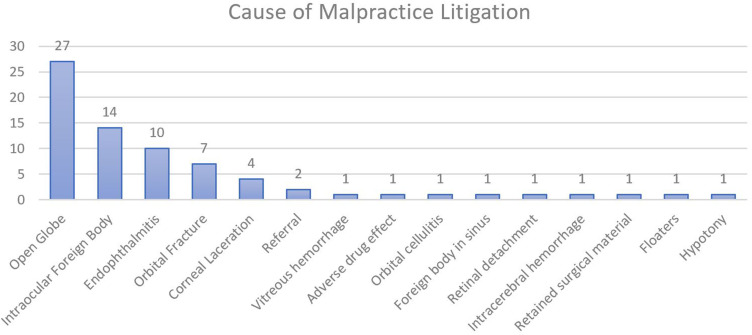
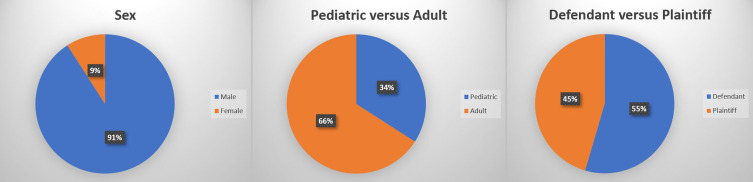
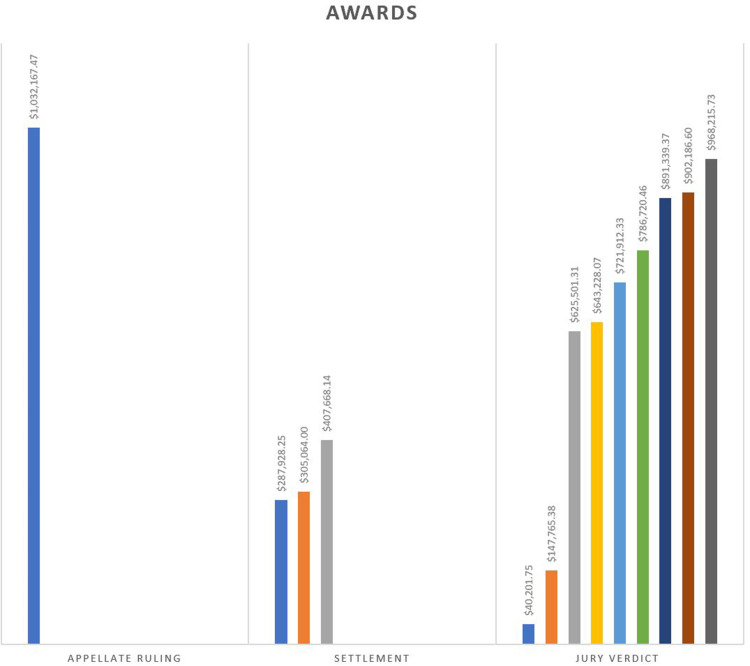
Query of the Westlaw® database yielded 1261 appellate cases and 1294 jury verdicts/settlements; 1063 cases met inclusion criteria.7–10 Forty-four ophthalmic trauma malpractice cases were identified from the database, representing 4.1% of total cases (Supplementary Table 1). The 44 ophthalmic trauma cases occurred between 1967 and 2013 (Figure 1). Figure 2 shows the causes of these malpractice cases. The majority of cases involved male plaintiffs (40 cases; 90.9%) (Figure 3). Fifteen cases (34.1%) involved pediatric plaintiffs (Figure 3). Overall, 24 cases (54.5%) were resolved in favor of the defendant (Figure 3). Eighteen cases (40.9%) were resolved by means of jury trial. Of these cases, 9 cases (50.0%) were associated with plaintiff verdicts and resulted in a mean adjusted jury award of $636,341 (range $40,202-$968,216) (Figure 4). Four cases (9.1%) resulted in settlements with mean adjusted indemnity of $333,553 (range $287,928-$407,668). Of the remaining 25 cases, 13 (29.5%) were resolved via appellate ruling with one case resulting in a payment to the plaintiff in the amount of $1,032,167, 5 cases (11.4%) were resolved via summary judgment, and 4 cases (9.1%) were resolved by pre-trial motions or post-trial relief. The
Figure 1.
Years of malpractice litigation.
Figure 2.
Cause of malpractice litigation.
Figure 3.
Demographic case information.
Figure 4.
Financial awards (inflation adjusted to 2015).
Open globe injuries were the most common clinical entity in this series, representing 61.4% of cases. Plaintiffs received awards in 40.7% of these cases. All but two payments in the series were awarded to plaintiffs with open globe injuries. Fifteen of the twenty-seven open globe cases (55.6%) specifically mention the presence of an intraocular foreign body. Seventeen open globe cases (63.0%) involved non-interventional claims only, including failure to diagnose or treat resulting in loss of vision. Ten open globe cases (37.0%) involved surgical or procedural claims, most of which involved poor outcomes after surgery, surgical delay, or claims of incomplete or poorly performed surgical interventions. Ten cases involved endophthalmitis, six of which resulted in payments to plaintiffs with mean payment of $536 268. In five of these cases, the diagnosis of penetrating trauma was missed and plaintiffs were allegedly misdiagnosed as having partial thickness lacerations only. Plaintiffs with missed diagnoses developed endophthalmitis and alleged this was a consequence of delay to accurate diagnosis and appropriate treatment. In three cases, open globe injuries were diagnosed; however, plaintiffs alleged that delay in treatment resulted in preventable endophthalmitis.
Seven cases (15.9%) involved orbital fractures, three of which resulted in payments to plaintiffs. Two of these cases involved allegations of eye movement restrictions following orbital fractures. In one, the restriction developed after extraocular muscle release surgery in a minor and resulted in a large payment to the plaintiff, and in the other, the plaintiff alleged that the restriction that developed could have been prevented had surgery been performed. In another case, the plaintiff alleged that the optic nerve had been inadvertently damaged during medial rectus release after orbital fracture. The case resulted in a payment to the plaintiff.
Minor plaintiffs were overrepresented among the ophthalmic trauma cases, with 34.1% of cases involving pediatric plaintiffs – only 6.4% of all ophthalmology cases in the database involved pediatric plaintiffs (P=<0.001).8 Among the 44 ophthalmic trauma cases, cases involving minors were more likely to be resolved in favor of the plaintiff than cases with adult plaintiffs (53.3% vs 37.9%), but this was not found to be statistically significant (P=0.35). Mean jury awards were also higher in cases involving minors than in adult cases ($687 454 vs $572 451), but again this was not found to be of statistical significance (P=0.64).
Most plaintiffs were male (90.0%) compared to the database overall, in which 54.8% of plaintiffs were male (P=<0.001). Prisoners were also overrepresented among the ocular trauma cases at 11.4% versus 3.9% of the overall database, but this was not found to be statistically significant. (P=0.13).
The majority of cases (63.6%) alleged insufficient intervention, including failure to diagnose or treat, resulting in disability or other damages. Of these cases, 32.1% resulted in payments to plaintiffs. Two of these cases involved litigation brought against defendant ophthalmologists who had never personally examined the plaintiffs. Two cases (4.5%) involved medical claims only, and neither resulted in a payment to the plaintiff.
Fourteen cases (31.8%) involved surgical or procedural claims, of which 28.6% resulted in payments to plaintiffs. The majority of these cases involve claims entirely or partially related to poor visual outcomes following open globe repair with or without removal of intraocular foreign body. The mean plaintiff payment in surgical/procedural cases was $765,564 (range $625,501-$902 187). This is higher, but not statistically significant (P=0.12), than the mean award in the non-interventional cases, which was $521,960 (range $40,202–1,032,167).
The rate of plaintiff jury verdicts was 50.0%, which was higher than the overall rate of plaintiff jury verdicts across all subspecialties of ophthalmology in this series (29.6%), but not statistically significant (P=0.11). Median plaintiff award for all of ocular trauma was $643 228, compared to $568 302 across all subspecialties.
Discussion
This review of 44 medical malpractice cases in ophthalmic trauma draws attention to commonly litigated clinical scenarios for the purpose of improving clinical management through dedicated analysis of risk. To our knowledge, this is the only review specifically analyzing malpractice cases in ophthalmic trauma, which complements existing publications on litigation in ophthalmology,7–10 while drawing special attention to many ophthalmic emergencies. The cases in this series represent some of the most common ophthalmic trauma scenarios, many of which often have poor outcomes due to the severe nature of these injuries, highlighting the importance of understanding the appropriate management of these conditions as well as the importance of documentation and expectation management.
In this analysis, ophthalmic trauma represented 4.1% of all ophthalmology cases in the database, which is similar to the 3% reported in a fifteen-year study of ophthalmology malpractice in England’s National Health Service (NHS) Litigation Authority database.11 The overwhelming majority of plaintiffs (90.9%) in this series were male, and a surprising number were minors at the time of injury (34.1%). Relative to non-trauma ophthalmology malpractice cases in the database, males were overrepresented, likely because males represent 60–90% of ophthalmic trauma patients around the world.12–17 As mentioned, minors also represented a disproportionate percentage of plaintiffs in this series compared to non-traumatic cases (P=<0.001). Importantly, ophthalmic trauma is the leading cause of unilateral non-congenital blindness in children, representing significant impact on quality of life and productivity.6,12,13,18,19
Ophthalmic trauma cases with minor plaintiffs were more likely to be resolved in favor of the plaintiffs (53.3% vs 37.9%; P=0.35) and to have higher jury awards ($687 454 vs $572 451; P=0.64) than cases with adult plaintiffs, but neither were found to be of statistical significance. We have previously reported a similar trend in ophthalmology, in which cases with pediatric plaintiffs are more likely to have plaintiff verdicts and were associated with higher monetary awards.8
The majority of cases in this analysis involved open globe injuries, representing 61.4% of cases. Open globe injuries are the most common cause of vision loss in working-aged individuals.20 Poor presenting visual acuity is associated with poor visual outcomes.20,21 Many of the cases in this series involved failure to diagnose or treat open globe injuries in a timely manner or related to poor visual outcomes following surgical repair of open globe injuries. Because of the severity of these injuries and the consequences of delayed or missed diagnoses, it is essential to err on the side of caution when treating these patients.
In this series, 55.6% of all open globe cases mentioned the presence of intraocular foreign bodies (IOFBs). The presence of an IOFB increases the risk of poor visual outcome and increases the risk of developing endophthalmitis.22 IOFBs can cause damage directly, through the compromise allowing infectious material into the eye, and through the chemical properties of the foreign body itself.22 In all cases of confirmed or suspected penetrating ocular injury, patients should be assumed to have an IOFB until proven otherwise due to the high morbidity associated with retained IOFBs. Because media opacities, hypopyon, vitritis or vitreous hemorrhage, and traumatic cataract can make it difficult to visualize IOFBs, a computed tomography scan should be considered in all cases of suspected IOFBs to avoid missing them or identifying the proper location imaging studies.22,23
Endophthalmitis complicated ten open globe cases in this series, most often secondary to alleged failure to diagnose penetrating trauma or a delay in treatment of known open globe injuries. Endophthalmitis is a serious and emergent complication of open globe injury. The diagnosis should be suspected in patients with pain or a rapid increase in pain with or without associated with hypopyon and vitritis; however, in patients who are already in extreme pain, it can be difficult to recognize.22 Whenever the diagnosis is suspected, cultures and stains for bacterial and fungal pathogens should be collected and treatment should be initiated immediately.22,24 Factors associated with the development of endophthalmitis include delay of primary repair, non-sterile wounds, and retained IOFbs.22,25 A Boston study reported that with a standardized protocol for treating these patients including repair by a dedicated eye trauma service as well as 48 hours of intravenous antibiotics, the rate of endophthalmitis was very low, at less than 1%.26
Seven cases (15.9%) involved orbital fractures. The cases were split between unfavorable surgical outcomes and allegations of poor outcomes secondary to failure to operate. Management, including whether to pursue surgical or conservative measures as well as the timing of repair of orbital fractures, depends on a number of factors and remains somewhat controversial; however, it has been reported that up to 40% of orbital fractures can have ophthalmic complications.27,28 Because management strategies vary depending on size and location of the fracture and because of the high risk of ophthalmic complications, it is recommended that ophthalmologists undertake a thorough discussion of the risks and benefits as well as a realistic discussion of prognosis with these patients.
Good clinical practice necessitates forming positive physician–patient relationships, which are often deterrents to litigation.29 A study of unsolicited complaints in ophthalmology found that ophthalmologists have significantly fewer unsolicited complaints than both non-ophthalmic surgeons and non-ophthalmic non-surgeons,30 suggesting that ophthalmologists as a whole generally are viewed favorably by patients. However, ophthalmic trauma patients often present acutely in the ED in patients with significant discomfort and distorted anatomy or other less, making it more difficult to establish a relationship with a patient and more difficult to perform a thorough evaluation.31 Although emergent trauma scenarios make building this relationship more difficult, in a review of ophthalmic malpractice with large monetary awards, Kraushar et al reported that over 43% of malpractice claims occurred less than one month following the patient’s initial encounter with the physician and 11% of cases involved ophthalmic trauma patients seen in the emergency department.31 A study that analyzed Press Ganey satisfaction scores in ophthalmology showed that perception of time spent with the practitioner was one of two main factors that significantly increased a patient’s likelihood to recommend that physician to a friend.32 These statistics reflect the results of the present analysis and serve as a reminder that time must be taken to establish rapport, especially in stressful and unfamiliar settings. Further, no review of malpractice litigation would be complete without advising careful and thorough documentation. This is especially true in settings of trauma, in which case ophthalmologists are often called as consultants. Ophthalmologists should not give advice informally over the phone and should have a low threshold to examine patients.
The majority of cases in this analysis involve suits related to either partial or complete vision loss following severe injuries to the globe or the orbit. It is always essential to have a frank and sympathetic discussion with patients about the prognosis for their conditions. In ophthalmic trauma, this discussion should be a top priority and guarded prognoses should be discussed in detail and witnessed when appropriate. While ophthalmologists may assume that patients understand the severity of their injuries, in reality, patients often have a strikingly different understanding regarding their visual prognosis. In this series, many of the poor outcomes observed were likely unavoidable consequences of severe trauma; however, it is clear from the case notes that patients often had positive expectations for their eventual outcome. When these positive outcomes do not manifest, suits may arise. As discussed above, the prognosis for open globe injuries and IOFBs is poor, and patients should be informed as such regardless of removal or foreign body or repair.23
The Westlaw® database contains settlements and verdicts from a variety of insurers, providing a global picture of ophthalmology malpractice in the United States, in contrast to many other analyses of ophthalmology malpractice litigation, which present information from a single insurer.32–37 As we have stated in other reports,7–10 limitations of the database include the fact that out-of-court settlements and dropped cases are not included. Additionally, because our database includes eighty years of cases, it is possible that changes in technology as well as patient and physician characteristics alter the applicability of some cases. The small number of cases makes statistical analysis difficult. Finally, level of detail provided about the cases varied to some degree and some data could have been lost due to classification errors. It is possible that some decisions were appealed or overturned without our knowledge.
Although ophthalmology is not among the most litigated specialties, between 5 and 10% of ophthalmologists will face a malpractice claim each year, of which 3–4% of suits are secondary to ophthalmic trauma.5,11,38 Ophthalmic trauma is a common cause of visual disability in children and adults.6,18 Not only does ophthalmic trauma often result in poor outcomes, but these patients are often seen in emergency departments or unfamiliar settings and have deforming and painful injuries, all of which make it difficult to perform a thorough and timely exam and workup. Because this population involves a higher than usual proportion of minors as well as patients who were previously healthy, it is especially important to be cognizant of potential high-risk scenarios, to set realistic prognostic expectations, to establish good communication and rapport between the provider and family members, and to document completely.
Acknowledgment
The authors would like to express appreciation to Dr. Christopher Shah for review of this manuscript.
Funding Statement
No funding was received by any author for this study.
Meeting Presentation
A portion of this work was presented at the ARVO meeting in Seattle, WA in May 2016.
Disclaimer
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the US Army Medical Department, the US Army Office of the Surgeon General, the Department of the Air Force, the Department of the Army, Department of Defense, the Uniformed Services University of the Health Sciences or any other agency of the US Government.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Disclosure
The authors declare no conflicts of interest.
References
- 1.Schaffer AC, Jena AB, Seabury SA, Singh H, Chalasani V, Kachalia A. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992–2014. JAMA Intern Med. 2017;177(5):710–718. doi: 10.1001/jamainternmed.2017.0311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assuaged by tort reforms. Health Aff. 2010;29(9):1585–1592. doi: 10.1377/hlthaff.2010.0135 [DOI] [PubMed] [Google Scholar]
- 3.Hermer LD, Brody H. Defensive medicine, cost containment, and reform. J Gen Intern Med. 2010;25(5):470–473. doi: 10.1007/s11606-010-1259-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609–2617. doi: 10.1001/jama.293.21.2609 [DOI] [PubMed] [Google Scholar]
- 5.Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629–636. doi: 10.1056/NEJMsa1012370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5(3):143–169. doi: 10.1076/opep.5.3.143.8364 [DOI] [PubMed] [Google Scholar]
- 7.Reddy AK, Engelhard SB, Shah CT, Sim AJ, Thorne JE. Medical malpractice in uveitis: a review of clinical entities and outcomes. Ocul Immunol Inflamm. 2016;1–7. [DOI] [PubMed] [Google Scholar]
- 8.Engelhard SB, Collins M, Shah CT, Sim AJ, Reddy AK. Malpractice litigation in pediatric ophthalmology. JAMA Ophthalmol. 2016;134(11):1230–1235. doi: 10.1001/jamaophthalmol.2016.3190 [DOI] [PubMed] [Google Scholar]
- 9.Engelhard SB, Aronow ME, Shah CT, Sim AJ, Reddy AK. Malpractice litigation in ocular oncology. Ocul Oncol Pathol. 2018;4(3):135–140. doi: 10.1159/000479559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Engelhard SB, Shah CT, Sim AJ, Reddy AK. Malpractice litigation in cornea and refractive surgery: a review of the westlaw database. Cornea. 2018;37(5):537–541. doi: 10.1097/ICO.0000000000001534 [DOI] [PubMed] [Google Scholar]
- 11.Mathew RG, Ferguson V, Hingorani M. Clinical negligence in ophthalmology: fifteen years of National Health Service litigation authority data. Ophthalmology. 2013;120(4):859–864. doi: 10.1016/j.ophtha.2012.01.009 [DOI] [PubMed] [Google Scholar]
- 12.Desai P, MacEwen CJ, Baines P, Minassian DC. Incidence of cases of ocular trauma admitted to hospital and incidence of blinding outcome. Br J Ophthalmol. 1996;80(7):592–596. doi: 10.1136/bjo.80.7.592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacEwen CJ, Baines PS, Desai P. Eye injuries in children: the current picture. Br J Ophthalmol. 1999;83(8):933–936. doi: 10.1136/bjo.83.8.933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacEwen CJ. Eye injuries: a prospective survey of 5671 cases. Br J Ophthalmol. 1989;73(11):888–894. doi: 10.1136/bjo.73.11.888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krishnaiah S, Nirmalan PK, Shamanna BR, Srinivas M, Rao GN, Thomas R. Ocular trauma in a rural population of southern India: the Andhra Pradesh eye disease study. Ophthalmology. 2006;113(7):1159–1164. doi: 10.1016/j.ophtha.2006.02.020 [DOI] [PubMed] [Google Scholar]
- 16.Nirmalan PK, Katz J, Tielsch JM, et al. Ocular trauma in a rural south Indian population: the Aravind comprehensive eye survey. Ophthalmology. 2004;111(9):1778–1781. doi: 10.1016/j.ophtha.2004.02.012 [DOI] [PubMed] [Google Scholar]
- 17.Wang W, Zhou Y, Zeng J, Shi M, Chen B. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in South‐Central China. Acta Ophthalmol. 2017;95(6):e503–e510. doi: 10.1111/aos.13438 [DOI] [PubMed] [Google Scholar]
- 18.Abbott J, Shah P. The epidemiology and etiology of pediatric ocular trauma. Surv Ophthalmol. 2013;58(5):476–485. doi: 10.1016/j.survophthal.2012.10.007 [DOI] [PubMed] [Google Scholar]
- 19.Minderhoud J, Nispen R, Heijthuijsen AA, et al. Epidemiology and aetiology of childhood ocular trauma in the Republic of Suriname. Acta Ophthalmol. 2016;94(5):479–484. doi: 10.1111/aos.13000 [DOI] [PubMed] [Google Scholar]
- 20.Page RD, Gupta SK, Jenkins TL, Karcioglu ZA. Risk factors for poor outcomes in patients with open-globe injuries. Clin Ophthalmol. 2016;10:1461. doi: 10.2147/OPTH.S108901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kong GY, Henderson RH, Sandhu SS, Essex RW, Allen PJ, Campbell WG. Wound‐related complications and clinical outcomes following open globe injury repair. Clin Exp Ophthalmol. 2015;43(6):508–513. doi: 10.1111/ceo.12511 [DOI] [PubMed] [Google Scholar]
- 22.Bhagat N, Nagori S, Zarbin M. Post-traumatic infectious endophthalmitis. Surv Ophthalmol. 2011;56(3):214–251. doi: 10.1016/j.survophthal.2010.09.002 [DOI] [PubMed] [Google Scholar]
- 23.Bettman JW. Seven hundred medicolegal cases in ophthalmology. Ophthalmology. 1990;97(10):1379–1384. doi: 10.1016/S0161-6420(90)32406-5 [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Zhang MN, Jiang CH, Yao Y, Zhang K. Endophthalmitis following open globe injury. Br J Ophthalmol. 2010;94(1):111–114. doi: 10.1136/bjo.2009.164913 [DOI] [PubMed] [Google Scholar]
- 25.Essex RW, Yi Q, Charles PG, Allen PJ. Post-traumatic endophthalmitis. Ophthalmology. 2004;111(11):2015–2022. doi: 10.1016/j.ophtha.2003.09.041 [DOI] [PubMed] [Google Scholar]
- 26.Andreoli CM, Andreoli MT, Kloek CE, Ahuero AE, Vavvas D, Durand ML. Low rate of endophthalmitis in a large series of open globe injuries. Am J Ophthalmol. 2009;147(4):601–608. doi: 10.1016/j.ajo.2008.10.023 [DOI] [PubMed] [Google Scholar]
- 27.Manana W, Odhiambo WA, Chindia ML, Koech K. The pattern of orbital fractures managed at two referral centers in Nairobi, Kenya. J Craniofac Surg. 2017;28(4):e338–e342. doi: 10.1097/SCS.0000000000003579 [DOI] [PubMed] [Google Scholar]
- 28.Dorafshar AH, Davidson EH, Manson PN. Controversies in the principles for management of orbital fractures in the pediatric population. Plast Reconstr Surg. 2017;139(3):804e–5e. doi: 10.1097/PRS.0000000000003122 [DOI] [PubMed] [Google Scholar]
- 29.Kraushar MF. Toward more effective risk prevention. Surv Ophthalmol. 2009;54(1):150–157. doi: 10.1016/j.survophthal.2008.10.007 [DOI] [PubMed] [Google Scholar]
- 30.Kohanim S, Sternberg P, Karrass J, Cooper WO, Pichert JW. Unsolicited patient complaints in ophthalmology: an empirical analysis from a large national database. Ophthalmology. 2016;123(2):234–241. doi: 10.1016/j.ophtha.2015.10.010 [DOI] [PubMed] [Google Scholar]
- 31.Kraushar MF, Robb JH. Ophthalmic malpractice lawsuits with large monetary awards. Arch Ophthalmol. 1996;114(3):333–337. doi: 10.1001/archopht.1996.01100130329019 [DOI] [PubMed] [Google Scholar]
- 32.Long C, Tsay EL, Jacobo SA, Popat R, Singh K, Chang RT. Factors associated with patient press ganey satisfaction scores for ophthalmology patients. Ophthalmology. 2016;123(2):242–247. doi: 10.1016/j.ophtha.2015.09.044 [DOI] [PubMed] [Google Scholar]
- 33.Abbott RL, Ou RJ, Bird M. Medical malpractice predictors and risk factors for ophthalmologists performing LASIK and photorefractive keratectomy surgery. Ophthalmology. 2003;110(11):2137–2146. doi: 10.1016/j.ophtha.2003.07.001 [DOI] [PubMed] [Google Scholar]
- 34.Day S, AM M, RL A. Retinopathy of prematurity malpractice claims: the ophthalmic mutual insurance company experience. Arch Ophthalmol. 2009;127(6):794–798. doi: 10.1001/archophthalmol.2009.97 [DOI] [PubMed] [Google Scholar]
- 35.Svider PF, Blake DM, Husain Q, et al. In the eyes of the law: malpractice litigation in oculoplastic surgery. Ophthal Plast Reconstr Surg. 2014;30(2):119–123. doi: 10.1097/IOP.0000000000000025 [DOI] [PubMed] [Google Scholar]
- 36.Kim JE, Weber P, Szabo A. Medical malpractice claims related to cataract surgery complicated by retained lens fragments (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2012;110:94. [PMC free article] [PubMed] [Google Scholar]
- 37.Fountain TR. Ophthalmic malpractice and physician gender: a claims data analysis (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2014;112. [PMC free article] [PubMed] [Google Scholar]
- 38.Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033. doi: 10.1056/NEJMsa054479 [DOI] [PubMed] [Google Scholar]